Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19
Abstract
1. Introduction
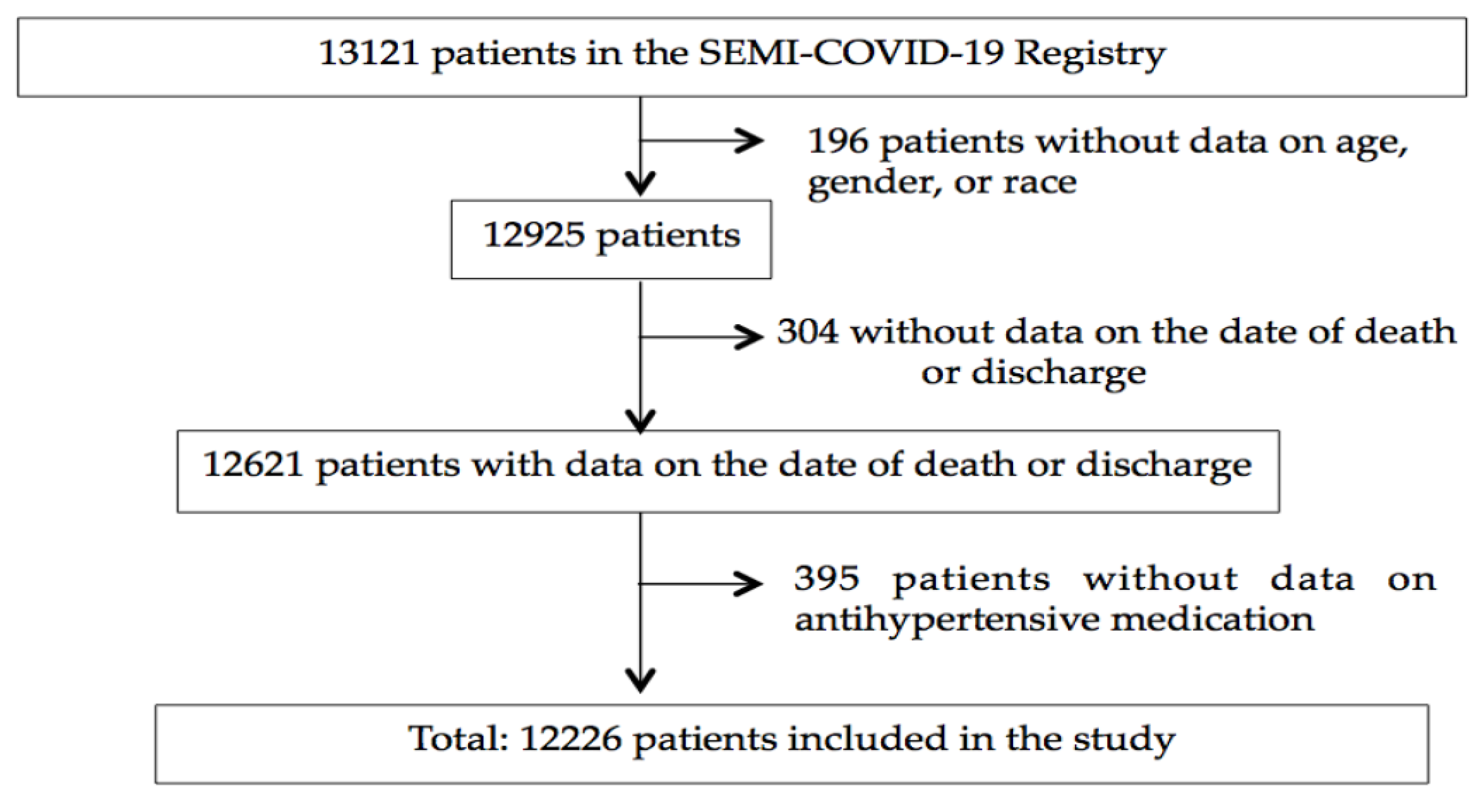
2. Subjects and Methods
3. Results
3.1. Demographic Characteristics of the Study Population
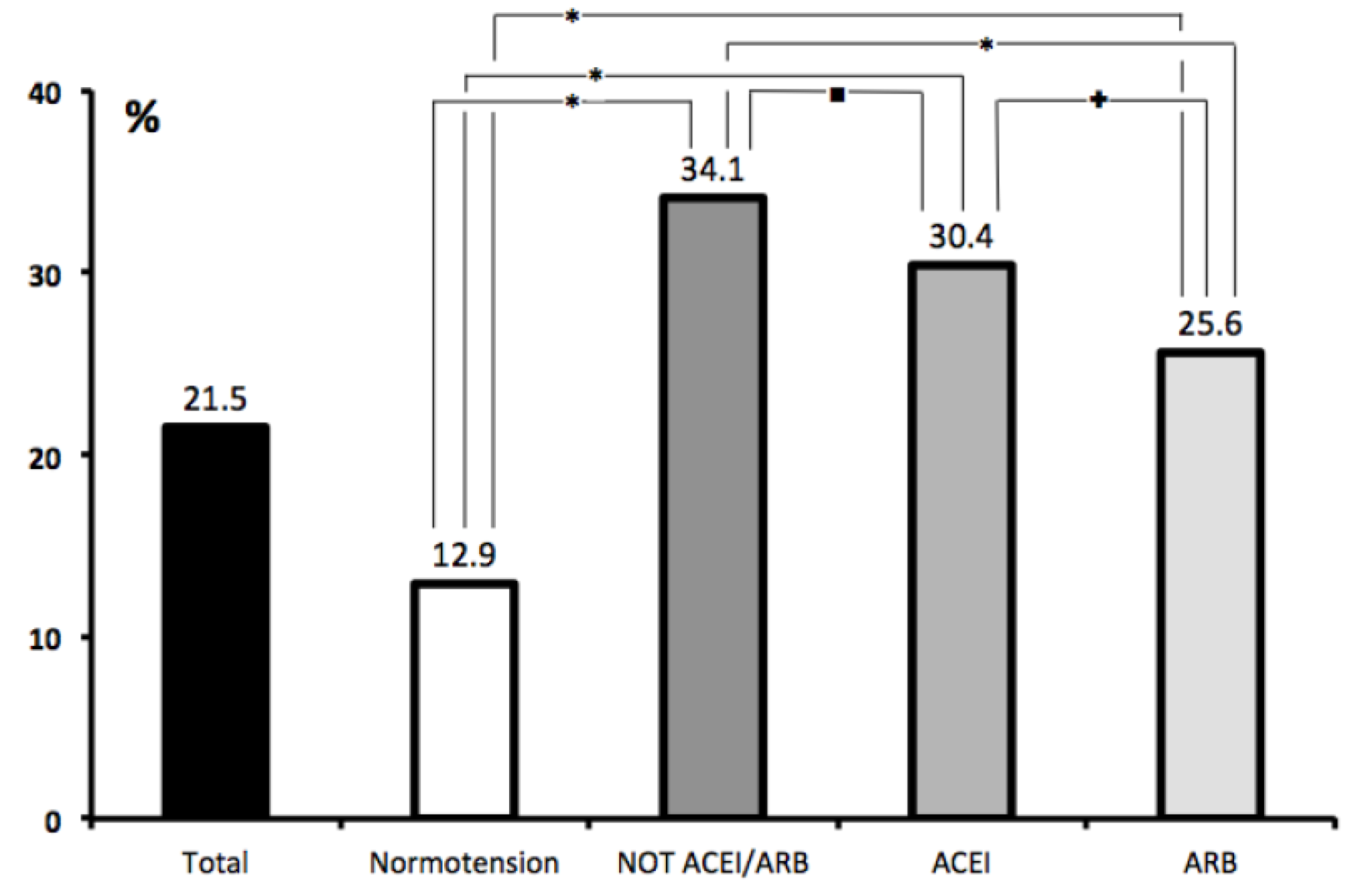
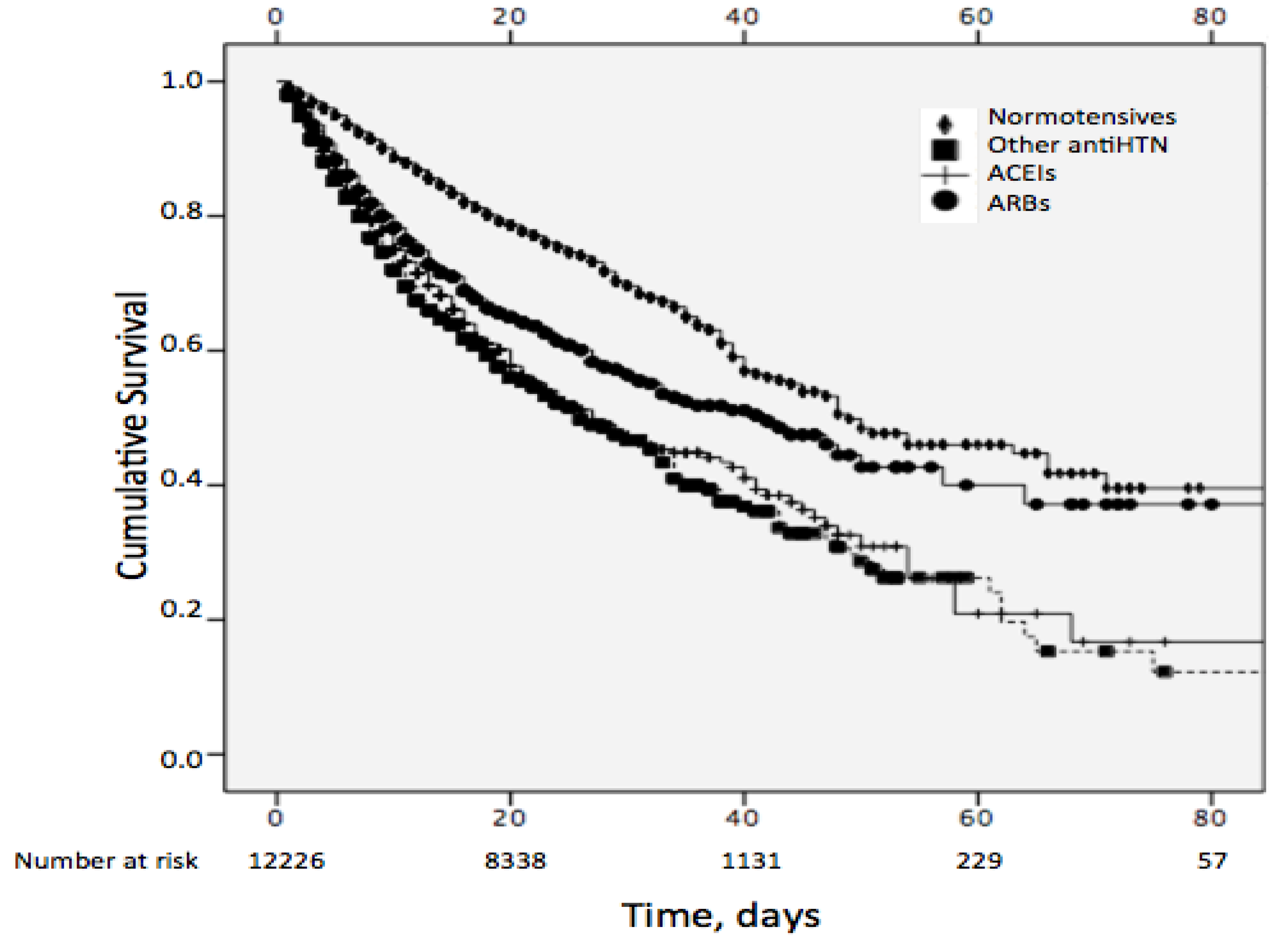
3.2. Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Johns Hopkins University Website. Available online: https://coronavirus.jhu.edu/map.html (accessed on 14 August 2020).
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, C.; Ou, J.; He, L.; Liu, H.; Shan, C.; Lei, D.S.C.; Hui, B.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Massimo, A.; Luca, C.; Antonio, C.; Danilo, C.; Antonio, C.; Giuseppe, F.; Roberto, F.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [PubMed]
- Global Atlas on Cardiovascular Disease Prevention and Control; World Health Organization: Geneva, Switzerland, 2011; ISBN 978-92-4-156437-3.
- Liang, W.; Liang, H.; Ou, L.; Chen, B.; Chen, A.; Li, C.; Li, Y.; Guan, W.; Sang, L.; Lu, J.; et al. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Int. Med. 2020, e202033. [Google Scholar] [CrossRef] [PubMed]
- Drummond, G.R.; Vinh, A.; Guzik, T.J.; Sobey, C.G. Immune mechanisms of hypertension. Nat. Rev. Immunol. 2019, 19, 517–532. [Google Scholar] [CrossRef]
- Zhang, Y.; Murugesan, P.; Huang, K.; Cai, H. NADPH oxidases and oxidase crosstalk in cardiovascular diseases: Novel therapeutic targets. Nat. Rev. Cardiol. 2020, 17, 170–194. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.J.; Hiscox, J.A.; Hooper, N.M. ACE2: From vasopeptidase to SARS virus receptor. Trends Pharmacol. Sci. 2004, 25, 291–294. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Furuhashi, M.; Moniwa, N.; Mita, T.; Fuseya, T.; Ishimura, S.; Ohno, K.; Shibata, S.; Tanaka, M.; Watanabe, Y.; Akasaka, H.; et al. Urinary angiotensin-converting enzyme 2 in hypertensive patients may be increased by olmesartan, an angiotensin II receptor blocker. Am. J. Hypertens. 2015, 28, 15–21. [Google Scholar] [CrossRef]
- Santos, R.A.S.; Sampaio, W.O.; Alzamora, A.C.; Motta-Santos, D.; Alenina, N.; Bader, M.; Campagnole-Santos, M. The ACE2/angiotensin-(1-7)/MAS axis of the renin-angiotensin system: Focus on angiotensin-(1-7). Physiol. Rev. 2018, 98, 505–553. [Google Scholar] [CrossRef]
- Fang, L.; Karakiulakis, G.; Roth, M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020, 8, e21. [Google Scholar] [CrossRef]
- Mancia, G.; Rea, F.; Ludergnani, M.; Apolone, G.; Corrao, G. Renin-Angiotensin-Aldosterone System Blockers and the Risk of Covid-19. N. Engl. J. Med. 2020, 382, 2431–2440. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, G.; Grassı, G.; Borghi, C.; Ferri, C.; Salvetti, M.; Volpe, M.; SARS-RAS Investigators; Cicero, A.F.; Minuz, P.; Muiesan, M.L.; et al. Age and Multimorbidity Predict Death Among COVID-19 Patients: Results of the SARS-RAS Study of the Italian Society of Hypertension. Hypertension 2020, 76, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef]
- Lind, L.; Sundström, J.; Ärnlöv, J.; Lampa, E. Impact of aging on the strength of cardiovascular risk factors: A longitudinal study over 40 years. J. Am. Heart Assoc. 2018, 7, e007061. [Google Scholar] [CrossRef]
- Kuba, K.; Imai, Y.; Rao, S.; Gao, H.; Guo, F.; Guan, B.; Huan, Y.; Yang, P.; Zhang, Y.; Deng, W.; et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 2005, 11, 875–879. [Google Scholar] [CrossRef]
- Saavedra, J.M. Angiotensin receptor blockers and COVID-19. Pharmacol. Res. 2020, 156, 104832. [Google Scholar] [CrossRef]
- American College of Cardiology. HFSA/ACC/AHA Statement Addresses Concerns re: Using RAAS Antagonists in COVID-19. 17 March 2020. Available online: https://www.acc.org/latestin-cardiology/articles/2020/03/17/08/59/hfsa-accahastatementaddresses-concernsreusingraasantagonists-incovid19 (accessed on 14 August 2020).
- European Society of Cardiology. Position Statement of theESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. 13 March 2020. Available online: https://www.escardio.org/Councils/Council-onHypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang (accessed on 14 August 2020).
- Casas-Rojo, J.M.; Antón-Santos, J.M.; Millán-Núñez-Cortés, J.; Lumbreras-Bermejo, C.; Ramos-Rincón, J.M.; Roy-Vallejo, E.; Artero-Mora, A.; Arnalich-Fernández, F.; García-Bruñén, J.M.; Vargas-Núñez, J.A.; et al. Características clínicas de los pacientes hospitalizados con COVID-19 en España: Resultados del Registro SEMI-COVID-19. Rev. Clínica Española 2020. [Google Scholar] [CrossRef]
- WHO. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (NCOV) Infection Is Suspected: Interim Guidance. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications (accessed on 10 July 2020).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Análisis de los casos de COVID-19 notificados a la RENAVE hasta el 10 de mayo en España, Informe COVID-19 nº 33. 29 de mayo de 2020. Informe nº 33. Análisis de los casos de COVID-19 notificados a la RENAVE hasta el 10 de mayo en España a 29 de mayo de 2020. Equipo COVID-19. RENAVE. CNE. CNM (ISCIII). Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20n%C2%BA%2033.%20An%C3%A1lisis%20de%20los%20casos%20de%20COVID-19%20hasta%20el%2010%20de%20mayo%20en%20Espa%C3%B1a%20a%2029%20de%20mayo%20de%202020.pdf (accessed on 14 August 2020).
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wu- han, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Guan, W.-J.; Liang, W.-H.; Zhao, Y.; Liang, H.-R.; Chen, Z.-S.; Li, Y.-M.; Liu, X.-Q.; Chen, R.-C.; Tang, C.-L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed]
- Leiva Sisnieguez, C.E.; Espeche, W.G.; Salazar, M.R. Arterial hypertension and the risk of severity and mortality of COVID-19. Eur. Respir. J. 2020, 55, 2001148. [Google Scholar] [CrossRef]
- Fosbøl, E.L.; Butt, J.H.; Østergaard, L.; Andersson, C.; Selmer, C.; Kragholm, K.; Schou, M.; Phelps, M.; Gislason, G.H.; Gerds, T.A.; et al. Association of Angiotensin-Converting Enzyme Inhibitor or Angiotensin Receptor Blocker Use With COVID-19 Diagnosis and Mortality. JAMA 2020, 324, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. HLH Across Speciality Collaboration, UK. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Rao, C. Medical certification of cause of death for COVID 19. Bull. World Health Organ. 2020, 98, 298-A. [Google Scholar] [CrossRef]
| Variable | Total Study Population (n = 12226) | Non-Survivors (n = 2630) | Survivors (n = 9596) | p Value |
|---|---|---|---|---|
| Age, years | 67.5 ± 16.1 | 79.6 ± 10.5 | 64.1 ± 15.7 | 0.0001 |
| Women, % | 42.6 | 38.1 | 43.8 | 0.0001 |
| Hypertension, % | 50.9 | 70.6 | 45.5 | 0.0001 |
| Diabetes mellitus, % | 19.1 | 28.2 | 16.6 | 0.0001 |
| COPD, % | 7.0 | 12.5 | 5.5 | 0.0001 |
| CKD, % | 6.0 | 12.5 | 4.3 | 0.0001 |
| Coronary heart disease, % | 8.0 | 14.1 | 6.3 | 0.0001 |
| Heart failure, % | 7.1 | 15.4 | 4.9 | 0.0001 |
| Stroke, % | 7.7 | 14.2 | 6.0 | 0.0001 |
| Atrial fibrillation, % | 11.2 | 21.7 | 8.3 | 0.0001 |
| Peripheral vascular disease, % | 4.7 | 9.0 | 3.5 | 0.0001 |
| Charlson Comorbidity Index score | 3.6 ± 2.7 | 5.7 ± 2.4 | 3.1 ± 2.5 | 0.0001 |
| Variable | Normotensive Subjects (n = 6001) | Hypertensive Subjects | p Value | ||
|---|---|---|---|---|---|
| Non-ACEI/ARB (n = 1987) | ACEI (n = 1983) | ARB (n = 2255) | |||
| Death, % | 12.9 | 34.1 | 30.4 | 25.6 | 0.0001 |
| Age, years | 60.1 ± 16.1 | 76.4 ± 12.7 | 73.5 ± 12.6 | 73.9 ± 11.8 | 0.0001 |
| Women, % | 41.8 | 48.5 | 39.1 | 42.4 | 0.0001 |
| Hypertension, % | 0 | 100 | 100 | 100 | 0.0001 |
| Diabetes mellitus, % | 9.3 | 25.5 | 29.3 | 30.4 | 0.0001 |
| COPD, % | 4.6 | 10.0 | 9.2 | 9.0 | 0.0001 |
| CKD, % | 1.8 | 12.5 | 7.3 | 10.5 | 0.0001 |
| Coronary heart disease, % | 3.1 | 13.0 | 12.9 | 12.1 | 0.0001 |
| Heart failure, % | 2.6 | 14.7 | 10.6 | 9.4 | 0.0001 |
| Stroke, % | 3.9 | 12.6 | 11.2 | 10.8 | 0.0001 |
| Atrial fibrillation, % | 4.9 | 21.4 | 15.1 | 15.3 | 0.0001 |
| Peripheral vascular disease, % | 2.2 | 7.1 | 6.5 | 7.5 | 0.0001 |
| Charlson Comorbidity Index score | 2.5 ± 2.3 | 5.1 ± 2.6 | 4.5 ± 2.5 | 4.6 ± 2.5 | 0.0001 |
| Variable. | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (CI 95%) | p Value | OR (CI 95%) | p Value | |
| Age, tertiles | ||||
| <60.9 | 1 | 1 | ||
| ≥60.9 and <76.3 | 5.3 (4.38–6.30) | 0.0001 | 2.0 (1.56–2.43) | 0.0001 |
| ≥76.3 | 20.3 (17.08–24.16) | 0.0001 | 4.7 (3.75–5.92) | 0.0001 |
| Blood pressure | ||||
| Normotension | 1 | 1 | ||
| Non-ACEIs/ARBs | 3.5 (3.11–3.95) | 0.0001 | 1.3 (1.08–1.43) | 0.002 |
| ACEIs | 3.0 (2.61–3.34) | 0.0001 | 1.6 (1.35–1.85) | 0.001 |
| ARBs | 2.3 (2.07–2.64) | 0.0001 | 1.2 (1.01–1.38) | 0.035 |
| Charlson Comorbidity Index, tertiles | ||||
| <2 | 1 | 1 | ||
| ≥2 and <5 | 11.2 (9.34–13.45) | 0.0001 | 4.7 (3.73–5.86) | 0.0001 |
| ≥5 | 28.2 (23.47–33.97) | 0.0001 | 8.1 (6.37–10,36) | 0.0001 |
| Gender | ||||
| Female | 1 | 1 | ||
| Male | 1.3 (1.16–1.38) | 0.0001 | 1.5 (1.39–1.71) | 0.0001 |
| ACEIs (in-hospital) | ||||
| no | 1 | 1 | ||
| yes | 1.1 (0.93–1.24) | 0.357 | 0.6 (0.45–0.66) | 0.0001 |
| ARBs (in-hospital) | ||||
| no | 1 | 1 | ||
| yes | 0.86 (0.74–0.99) | 0.046 | 0.5 (0.45–0.65) | 0.0001 |
| HF | ||||
| no | 1 | 1 | ||
| yes | 3.6 (3.08–4.09) | 0.0001 | 1.2 (1.01–1.41) | 0.037 |
| Atrial fibrillation | ||||
| no | 1 | 1 | ||
| yes | 1.3 (1.16–1.38) | 0.0001 | 1.2 (1.01–1.33) | 0.034 |
| CKD | ||||
| no | 1 | 1 | ||
| yes | 3.2 (2.75–3.73) | 0.0001 | 1.2 (0.99–1.41) | 0.068 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodilla, E.; Saura, A.; Jiménez, I.; Mendizábal, A.; Pineda-Cantero, A.; Lorenzo-Hernández, E.; Fidalgo-Montero, M.d.P.; López-Cuervo, J.F.; Gil-Sánchez, R.; Rabadán-Pejenaute, E.; et al. Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19. J. Clin. Med. 2020, 9, 3136. https://doi.org/10.3390/jcm9103136
Rodilla E, Saura A, Jiménez I, Mendizábal A, Pineda-Cantero A, Lorenzo-Hernández E, Fidalgo-Montero MdP, López-Cuervo JF, Gil-Sánchez R, Rabadán-Pejenaute E, et al. Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19. Journal of Clinical Medicine. 2020; 9(10):3136. https://doi.org/10.3390/jcm9103136
Chicago/Turabian StyleRodilla, Enrique, Alberto Saura, Iratxe Jiménez, Andrea Mendizábal, Araceli Pineda-Cantero, Elizabeth Lorenzo-Hernández, Maria del Pilar Fidalgo-Montero, Joaquín Fernandez López-Cuervo, Ricardo Gil-Sánchez, Elisa Rabadán-Pejenaute, and et al. 2020. "Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19" Journal of Clinical Medicine 9, no. 10: 3136. https://doi.org/10.3390/jcm9103136
APA StyleRodilla, E., Saura, A., Jiménez, I., Mendizábal, A., Pineda-Cantero, A., Lorenzo-Hernández, E., Fidalgo-Montero, M. d. P., López-Cuervo, J. F., Gil-Sánchez, R., Rabadán-Pejenaute, E., Abella-Vázquez, L., Giner-Galvañ, V., Solís-Marquínez, M. N., Boixeda, R., Peña-Fernández, A. d. l., Carrasco-Sánchez, F. J., González-Moraleja, J., Torres-Peña, J. D., Guisado-Espartero, M. E., ... Gómez-Huelgas, R. (2020). Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19. Journal of Clinical Medicine, 9(10), 3136. https://doi.org/10.3390/jcm9103136






