Reliability of the Scapula Reposition Test in Subjects with Rotator Cuff Tendinopathy and Scapular Dyskinesis
Abstract
1. Introduction
2. Methods
2.1. Study Design
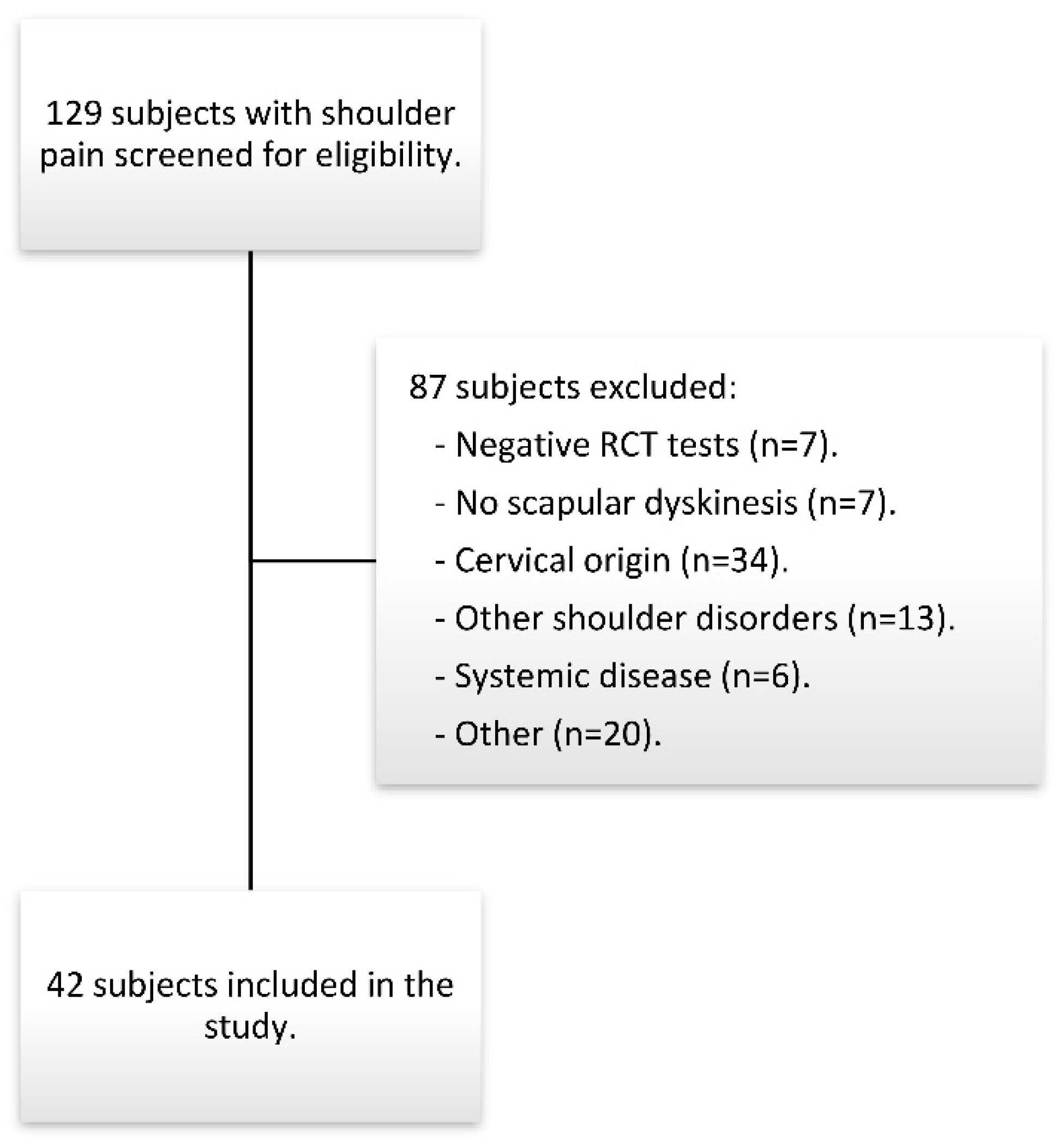
2.2. Subjects
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Raters
3. Measurements
3.1. Scapula Reposition Test
3.2. Dynamometry
3.3. Statistical Analysis
4. Results
4.1. Pairwise Comparisons of Pain Ratings at Rest
4.2. Reliability of the SRT
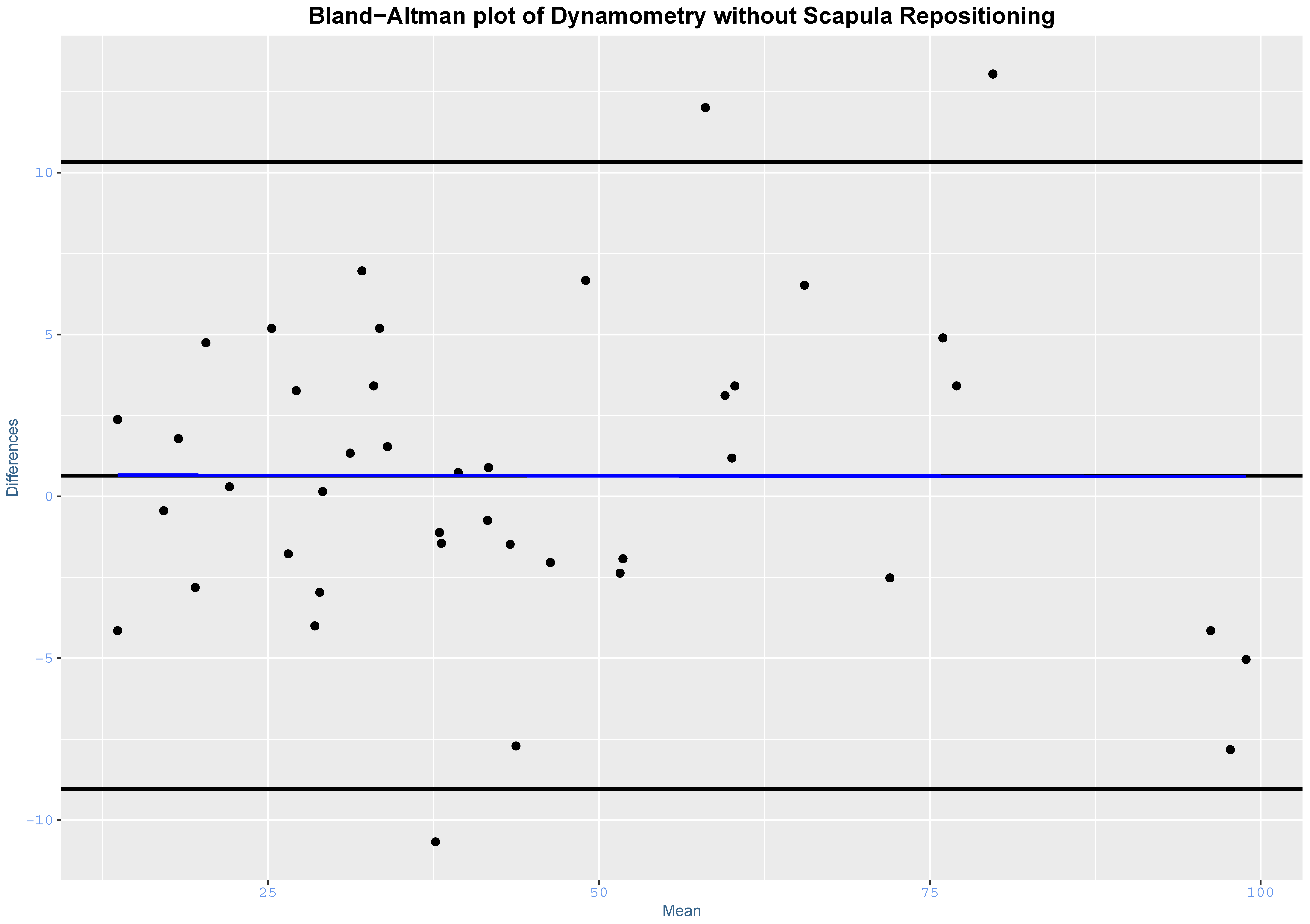
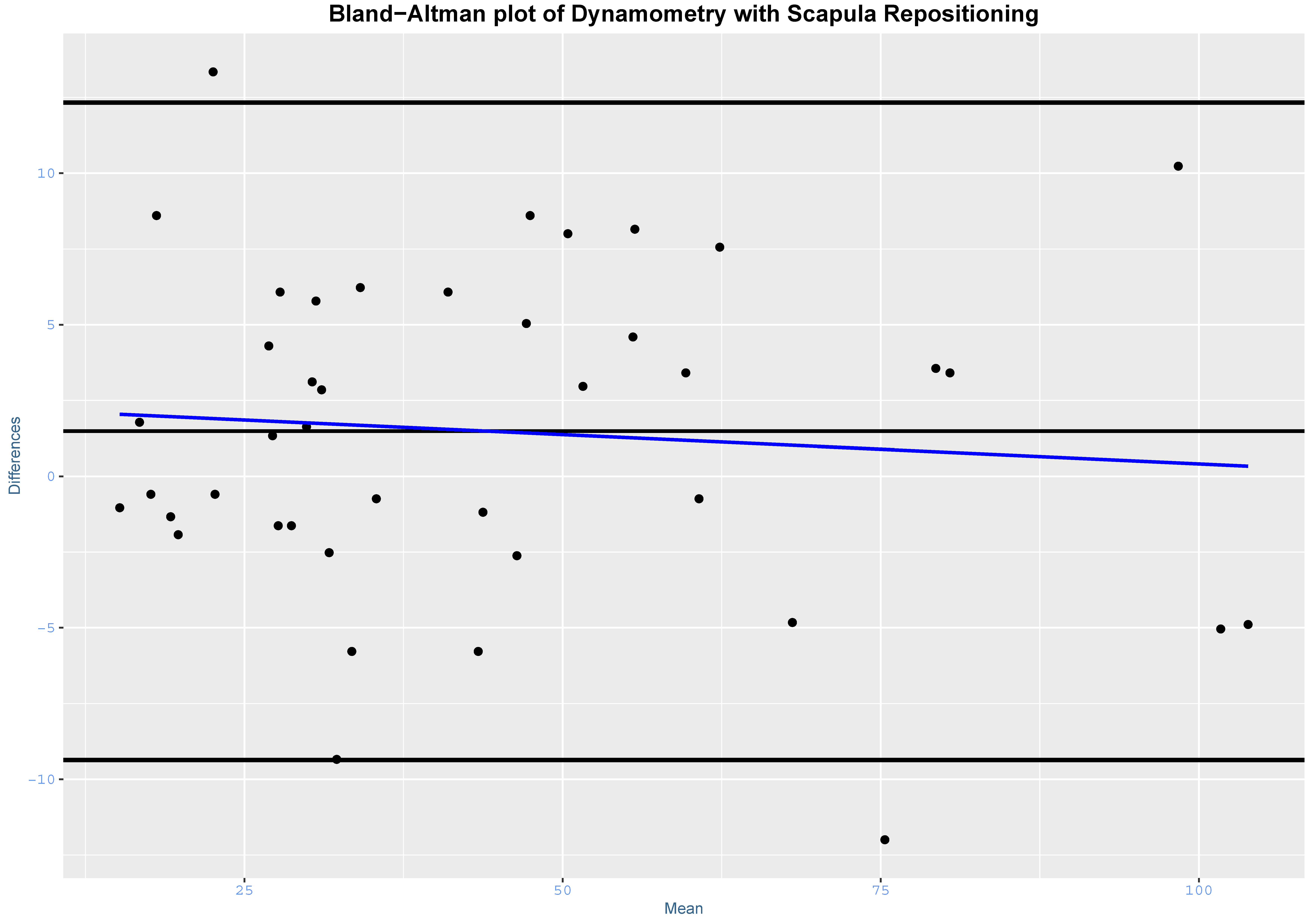
4.3. Dynamometry Reliability
4.4. Correlation Analysis
5. Discussion
5.1. Scapula Reposition Test Reliability
5.2. Manual Test and Dynamometry Correlation
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Michener, L.A.; McClure, P.W.; Karduna, A.R. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin. Biomech. 2003, 18, 369–379. [Google Scholar] [CrossRef]
- Ratcliffe, E.; Pickering, S.; McLean, S.; Lewis, J. Is there a relationship between subacromial impingement syndrome and scapular orientation? A systematic review. Br. J. Sports Med. 2014, 48, 1251–1256. [Google Scholar] [CrossRef]
- Kibler, W.B.; Ludewig, P.M.; McClure, P.W.; Michener, L.A.; Bak, K.; Sciascia, A.D. Clinical implications of scapular dyskinesis in shoulder injury: The 2013 consensus statement from the ‘Scapular Summit’. Br. J. Sports Med. 2013, 47, 877–885. [Google Scholar] [CrossRef]
- Wright, A.A.; Wassinger, C.A.; Frank, M.; Michener, L.A.; Hegedus, E.J. Diagnostic accuracy of scapular physical examination tests for shoulder disorders: A systematic review. Br. J. Sports Med. 2013, 47, 886–892. [Google Scholar] [CrossRef]
- Wassinger, C.A.; Williams, D.A.; Milosavljevic, S.; Hegedus, E.J. Clinical reliability and diagnostic accuracy of visual scapulohumeral movement evaluation in detecting patients with shoulder impairment. Int. J. Sports Phys. Ther. 2015, 10, 456–463. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527193/ (accessed on 20 July 2018).
- Tate, A.R.; McClure, P.W.; Kareha, S.; Irwin, D. Effect of the Scapula Reposition Test on shoulder impingement symptoms and elevation strength in overhead athletes. J. Orthop. Sports Phys. Ther. 2008, 38, 4–11. [Google Scholar] [CrossRef]
- Lange, T.; Struyf, F.; Schmitt, J.; Lützner, J.; Kopkow, C. The reliability of physical examination tests for the clinical assessment of scapular dyskinesis in subjects with shoulder complaints: A systematic review. Phys. Ther. Sport 2017, 26, 64–89. [Google Scholar] [CrossRef]
- Kottner, J.; Audigé, L.; Brorson, S.; Donner, A.; Gajewski, B.J.; Hróbjartsson, A.; Roberts, C.; Shoukri, M.; Streiner, D.L. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J. Clin. Epidemiol. 2011, 64, 96–106. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar] [CrossRef]
- Membrilla-Mesa, M.D.; Cuesta-Vargas, A.I.; Pozuelo-Calvo, R.; Tejero-Fernandez, V.; Martin-Martin, L.; Arroyo-Morales, M. Shoulder pain and disability index: Cross cultural validation and evaluation of psychometric properties of the Spanish version. Health Qual. Life Outcomes 2015, 13, 200. [Google Scholar] [CrossRef]
- Cadogan, A.; Laslett, M.; Hing, W.; McNair, P.; Williams, M. Interexaminer reliability of orthopaedic special tests used in the assessment of shoulder pain. Man. Ther. 2011, 16, 131–135. [Google Scholar] [CrossRef]
- Scholtes, V.A.; Terwee, C.B.; Poolman, R.W. What makes a measurement instrument valid and reliable? Injury 2011, 42, 236–240. [Google Scholar] [CrossRef]
- Littlewood, C.; Bateman, M.; Brown, K.; Bury, J.; Mawson, S.; May, S.; May, J.W. A self-managed single exercise programme versus usual physiotherapy treatment for rotator cuff tendinopathy: A randomised controlled trial (the SELF study). Clin. Rehabil. 2016, 30, 686–696. [Google Scholar] [CrossRef]
- Michener, L.A.; Walsworth, M.K.; Doukas, W.C.; Murphy, K.P. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch. Phys. Med. Rehabil. 2009, 90, 1898–1903. [Google Scholar] [CrossRef]
- Watts, A.R.; Williams, B.; Kim, S.W.; Bramwell, D.C.; Krishnan, J. Shoulder impingement syndrome: A systematic review of clinical trial participant selection criteria. Shoulder Elb. 2017, 9, 31–41. [Google Scholar] [CrossRef]
- McClure, P.; Tate, A.R.; Kareha, S.; Irwin, C.; Zlupko, E. A clinical method for identifying scapular dyskinesis, part 1: Reliability. J. Athl. Train. 2009, 44, 160–164. [Google Scholar] [CrossRef]
- Tate, A.R.; McClure, P.; Kareha, S.; Irwin, D.; Barbe, M.F. A clinical method for identifying scapular dyskinesis, part 2: Validity. J. Athl. Train. 2009, 44, 165–173. [Google Scholar] [CrossRef]
- Kolber, M.J.; Fuller, C.; Marshall, J.; Wright, A.; Hanney, W.J. The reliability and concurrent validity of scapular plane shoulder elevation measurements using a digital inclinometer and goniometer. Physiother. Theory Pract. 2012, 28, 161–168. [Google Scholar] [CrossRef]
- Lewis, J.; Green, A.; Reichard, Z.; Wright, C. Scapular position: The validity of skin surface palpation. Man. Ther. 2002, 7, 26–30. [Google Scholar] [CrossRef]
- Kopkow, C.; Lange, T.; Schmitt, J.; Kasten, P. Interrater reliability of the modified scapular assistance test with and without handheld weights. Man. Ther. 2015, 20, 868–874. [Google Scholar] [CrossRef]
- Beshay, N.; Lam, P.H.; Murrell, G.A.C. Assessing the Reliability of Shoulder Strength Measurement: Hand-Held versus Fixed Dynamometry. Shoulder Elb. 2011, 3, 244–251. [Google Scholar] [CrossRef]
- Sim, J.; Wright, C.C. The Kappa Statistic in Reliability Studies: Use, Interpretation, and Sample Size Requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Michener, L.A.; Snyder, A.R.; Leggin, B.G. Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. J. Sport Rehabil. 2011, 20, 115–128. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Atkinson, G.; Nevill, A.M. Statistical Methods for Assessing Measurement Error (Reliability) in Variables Relevant to Sports Medicine. Sports Med. 1998, 26, 217–238. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; SAGE Publications: London, UK, 2017. [Google Scholar]
- Karanicolas, P.J.; Bhandari, M.; Kreder, H.; Moroni, A.; Richardson, M.; Walter, S.; Norman, G.; Guyatt, G. Evaluating agreement: Conducting a reliability study. J. Bone Joint Surg. Am. 2009, 91, 99–106. [Google Scholar] [CrossRef]
- Carlsson, H.; Rasmussen-Barr, E. Clinical screening tests for assessing movement control in non-specific low-back pain. A systematic review of intra- and inter-observer reliability studies. Man. Ther. 2013, 18, 103–110. [Google Scholar] [CrossRef]
- Kibler, W.B.; Sciascia, A.; Dome, D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am. J. Sports Med. 2006, 34, 1643–1647. [Google Scholar] [CrossRef]
- Boettcher, C.E.; Ginn, K.A.; Cathers, I. The “empty can” and “full can” tests do not selectively activate supraspinatus. J. Sci. Med. Sport 2009, 12, 435–439. [Google Scholar] [CrossRef]
- Rabin, A.; Irrgang, J.J.; Fitzgerald, G.K.; Eubanks, A. The intertester reliability of the scapular assistance test. J. Orthop. Sports Phys. Ther. 2006, 36, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Nagatomi, T.; Mae, T.; Nagafuchi, T.; Yamada, S.; Nagai, K.; Yoneda, M. Shoulder manual muscle resistance test cannot fully detect muscle weakness. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2081–2088. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Average (SD) |
|---|---|
| Age, years | 53.55 (12.15) |
| Height, cm | 166.86 (9.67) |
| Weight, kg | 74.96 (17.10) |
| Body mass index | 26.17 (5.09) |
| Sex, n (%) | |
| Female | 21 (50) |
| Male | 21 (50) |
| Tested side, n (%) | |
| Right | 18 (42.90) |
| Left | 24 (57.10) |
| Dominant side, n (%) | |
| Right | 42 (100) |
| Left | 0 (0) |
| VAS pain, cm | 4.07 (1.80) |
| Pain duration, months | 22.83 (24.03) |
| SPADI, % | 43.88 (16.64) |
| Rater 1 Second Trial | Total | |||
|---|---|---|---|---|
| Negative | Positive | |||
| Rater 1 First Trial | Negative | 6 | 6 | 12 |
| Positive | 3 | 27 | 30 | |
| Total | 9 | 32 | 42 | |
| Rater 2 | Total | |||
|---|---|---|---|---|
| Negative | Positive | |||
| Rater 1 First trial | Negative | 5 | 7 | 12 |
| Positive | 10 | 20 | 30 | |
| Total | 15 | 27 | 42 | |
| Observed Agreement (%) | Cohen’s κ (95% CI) | Prevalence Index (95% CI) | Bias Index (95% CI) | PABAK (95% CI) | κmax (95% CI) | |
|---|---|---|---|---|---|---|
| Intra-rater | 33/42 (78.57) | 0.43 (0.14, 0.73) | −0.50 (−0.68, −0.32) | 0.07 (−0.11, 0.26) | 0.57 (0.26, 0.79) | 0.81 (0.60, 1.00) |
| Inter-rater | 25/42 (59.52) | 0.08 (−0.22, 0.38) | −0.36 (−0.54, −0.18) | −0.07 (−0.27, 0.13) | 0.19 (−0.13, 0.49) | 0.84 (0.66, 1.00) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandez-Matias, R.; Gallardo-Zamora, P.; Sanchez-Aguilera, C.L.; Mardones-Varela, H.; Gallego-Izquierdo, T.; Pecos-Martin, D. Reliability of the Scapula Reposition Test in Subjects with Rotator Cuff Tendinopathy and Scapular Dyskinesis. J. Clin. Med. 2020, 9, 80. https://doi.org/10.3390/jcm9010080
Fernandez-Matias R, Gallardo-Zamora P, Sanchez-Aguilera CL, Mardones-Varela H, Gallego-Izquierdo T, Pecos-Martin D. Reliability of the Scapula Reposition Test in Subjects with Rotator Cuff Tendinopathy and Scapular Dyskinesis. Journal of Clinical Medicine. 2020; 9(1):80. https://doi.org/10.3390/jcm9010080
Chicago/Turabian StyleFernandez-Matias, Ruben, Pablo Gallardo-Zamora, Cristina Lorenzo Sanchez-Aguilera, Hector Mardones-Varela, Tomas Gallego-Izquierdo, and Daniel Pecos-Martin. 2020. "Reliability of the Scapula Reposition Test in Subjects with Rotator Cuff Tendinopathy and Scapular Dyskinesis" Journal of Clinical Medicine 9, no. 1: 80. https://doi.org/10.3390/jcm9010080
APA StyleFernandez-Matias, R., Gallardo-Zamora, P., Sanchez-Aguilera, C. L., Mardones-Varela, H., Gallego-Izquierdo, T., & Pecos-Martin, D. (2020). Reliability of the Scapula Reposition Test in Subjects with Rotator Cuff Tendinopathy and Scapular Dyskinesis. Journal of Clinical Medicine, 9(1), 80. https://doi.org/10.3390/jcm9010080






