The Clinical Outcomes Based on the Achievement of Low-Density Lipoprotein Cholesterol Targets after ST Elevation Myocardial Infarction
Abstract
1. Introduction
2. Materials and Methods
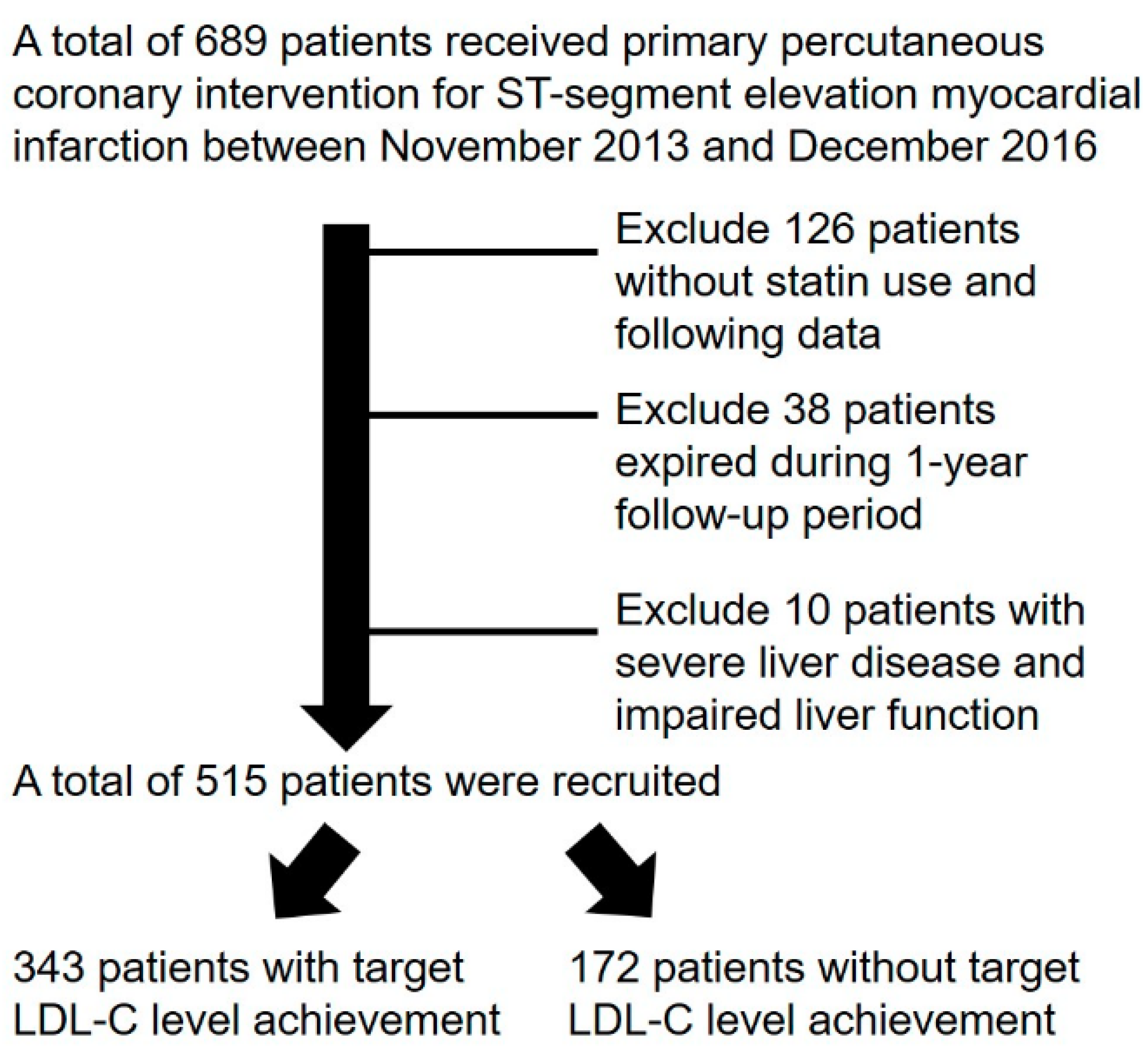
2.1. Patients and Groups
2.2. Follow-Up
2.3. Definitions
2.4. Study Endpoints
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Study Groups
3.2. Angiographic Characteristics of Study Groups
3.3. One-Year Clinical Outcomes of Study Patients
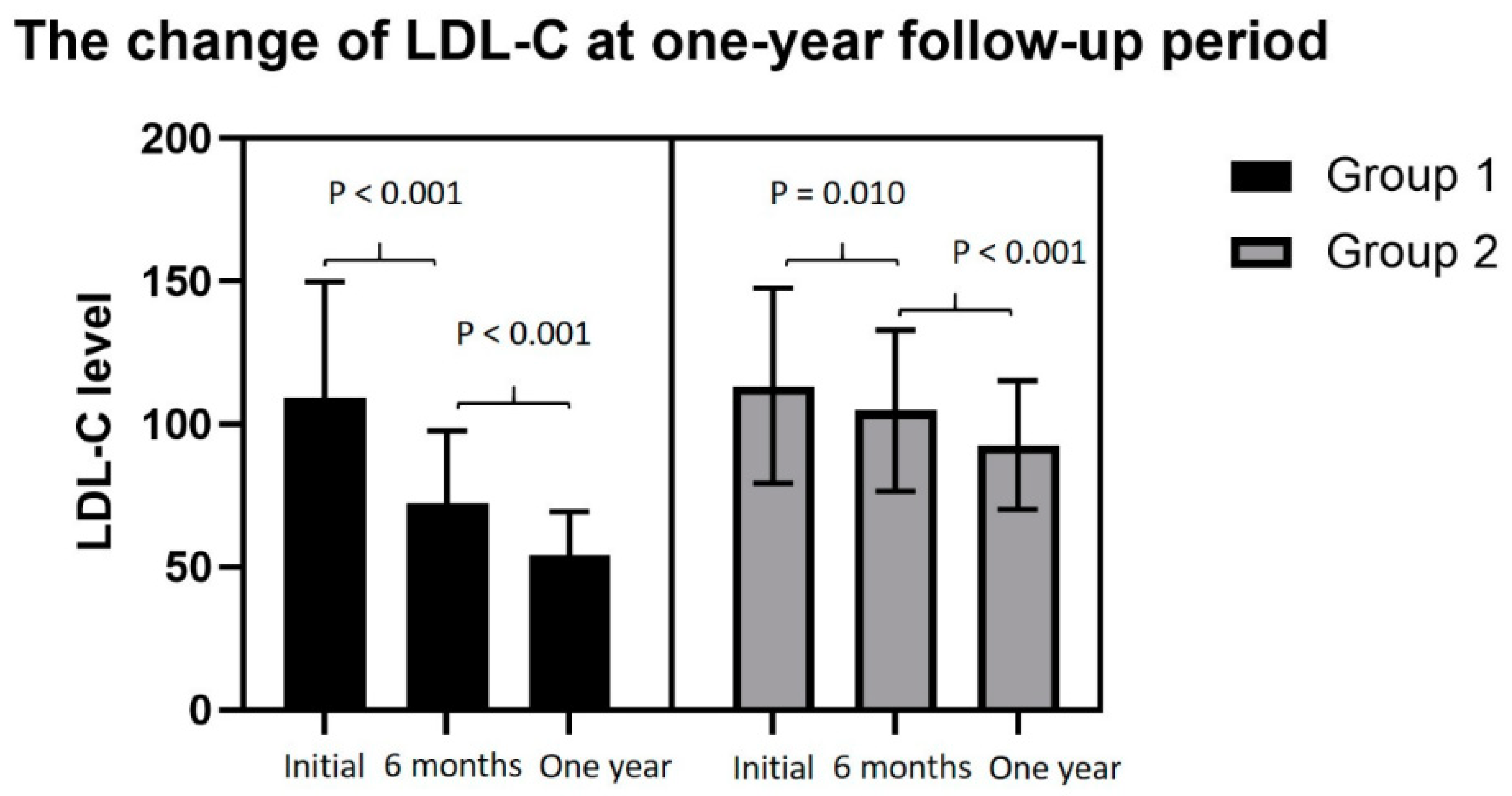
3.4. The Change in LDL-C Levels of the Study Groups at One-Year Follow-up
3.5. The Serial Changes of Lipid Profile in the Two Groups
3.6. Univariate and Multivariate Logistic Regression Analyses of Associations for Non-Achievement of LDL-C Targets
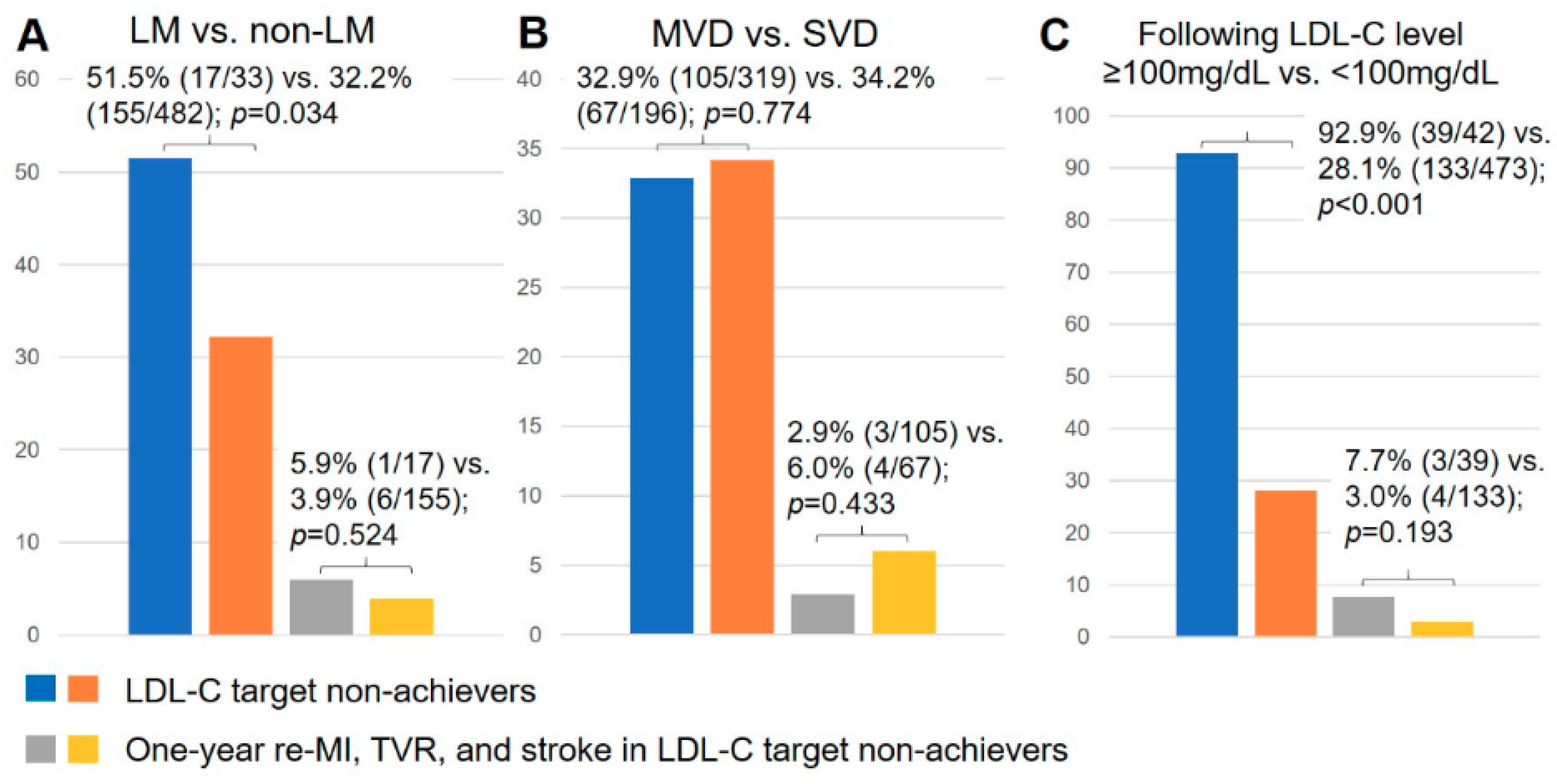
3.7. The Achieved LDL-C Target Rate and the Incidence of Re-MI, TVR, and Stroke in Different Subgroups
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Schwartz, G.G.; Olsson, A.G.; Ezekowitz, M.D.; Ganz, P.; Oliver, M.F.; Waters, D.; Zeiher, A.; Chaitman, B.R.; Leslie, S.; Stern, T. Myocardial ischemia reduction with aggressive cholesterol lowering (MIRACL) study investigators. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial. JAMA 2001, 285, 1711–1718. [Google Scholar] [CrossRef] [PubMed]
- Karthikeyan, G.; Teo, K.K.; Islam, S.; McQueen, M.J.; Pais, P.; Wang, X.; Sato, H.; Lang, C.C.; Sitthi-Amorn, C.; Pandey, M.R.; et al. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among Asians: An analysis from the INTERHEART Study. J. Am. Coll. Cardiol. 2009, 53, 244–253. [Google Scholar] [CrossRef] [PubMed]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. Circulation 2018, 73. [Google Scholar] [CrossRef]
- Catapano, A.L.; Graham, I.; De Backer, G.; Wiklund, O.; Chapman, M.J.; Drexel, H.; Hoes, A.W.; Jennings, C.S.; Landmesser, U.; Pedersen, T.R.; et al. ESC Scientific Document Group. 2016 ESC/EAS Guidelines for the management of dyslipidaemias. Eur. Heart J. 2016, 37, 2999–3058. [Google Scholar] [CrossRef]
- Boekholdt, S.M.; Hovingh, G.K.; Mora, S.; Arsenault, B.J.; Amarenco, P.; Pedersen, T.R.; LaRosa, J.C.; Waters, D.D.; DeMicco, D.A.; Simes, R.J.; et al. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: A meta-analysis of statin trials. J. Am. Coll. Cardiol. 2014, 64, 485–494. [Google Scholar] [CrossRef]
- Lee, J.H.; Yang, D.H.; Park, H.S.; Cho, Y.; Jeong, M.H.; Kim, Y.J.; Kim, K.S.; Hur, S.H.; Seong, I.W.; Hong, T.J.; et al. Korea Acute Myocardial Infarction Registry Investigators. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea acute myocardial infarction registry: Prescription rate, predictors, and prognostic value. Am. Heart J. 2010, 159, 1012–1019. [Google Scholar] [CrossRef]
- Choi, J.S.; Kim, C.S.; Bae, E.H.; Ma, S.K.; Jeong, M.H.; Kim, Y.J.; Cho, M.C.; Kim, C.J.; Kim, S.W. Suboptimal medical care of patients with ST-elevation myocardial infarction and renal insufficiency: Results from the Korea acute myocardial infarction registry. BMC Nephrol. 2012, 13, 110. [Google Scholar] [CrossRef]
- Wang, W.T.; Hellkamp, A.; Doll, J.A.; Thomas, L.; Navar, A.M.; Fonarow, G.C.; Julien, H.M.; Peterson, E.D.; Wang, T.Y. Lipid testing and statin dosing after acute myocardial infarction. J. Am. Heart Assoc. 2018, 7. [Google Scholar] [CrossRef]
- Natsuaki, M.; Furukawa, Y.; Morimoto, T.; Nakagawa, Y.; Ono, K.; Kaburagi, S.; Inada, T.; Mitsuoka, H.; Taniguchi, R.; Nakano, A.; et al. CREDO-Kyoto PCI/CABG registry cohort-2 investigators. Intensity of statin therapy, achieved low-density lipoprotein cholesterol levels and cardiovascular outcomes in Japanese patients after coronary revascularization. Perspectives from the CREDO-Kyoto registry cohort-2. Circ. J. 2012, 76, 1369–1379. [Google Scholar]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar] [PubMed]
- Lee, W.C.; Fang, C.Y.; Chen, H.C.; Hsueh, S.K.; Chen, C.J.; Yang, C.H.; Yip, H.K.; Hang, C.L.; Wu, C.J.; Fang, H.Y. Aspiration thrombectomy and drug-eluting stent implantation decrease the occurrence of angina pectoris one year after acute myocardial infarction. Medicine 2016, 95, e3426. [Google Scholar] [CrossRef] [PubMed]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron. Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [PubMed]
- Chinwong, D.; Patumanond, J.; Chinwong, S.; Siriwattana, K.; Gunaparn, S.; Hall, J.J.; Phrommintikul, A. Statin therapy in patients with acute coronary syndrome: Low-density lipoprotein cholesterol goal attainment and effect of statin potency. Ther. Clin. Risk Manag. 2015, 11, 127–136. [Google Scholar] [PubMed]
- Martin, S.S.; Gosch, K.; Kulkarni, K.R.; Spertus, J.A.; Mathews, R.; Ho, P.M.; Maddox, T.M.; Newby, L.K.; Alexander, K.P.; Wang, T.Y. Modifiable factors associated with failure to attain low-density lipoprotein cholesterol goal at 6 months after acute myocardial infarction. Am. Heart J. 2013, 165, 26–33.e3. [Google Scholar] [CrossRef]
- Schwartz, G.G.; Steg, P.G.; Szarek, M.; Bhatt, D.L.; Bittner, V.A.; Diaz, R.; Edelberg, J.M.; Goodman, S.G.; Hanotin, C.; Harrington, R.A.; et al. ODYSSEY OUTCOMES Committees and Investigators. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N. Engl. J. Med. 2018, 379, 2097–2107. [Google Scholar] [CrossRef]
- Liao, J.K. Safety and efficacy of statins in asians. Am. J. Cardiol. 2007, 99, 410–414. [Google Scholar] [CrossRef]
- Bitzur, R.; Cohen, H.; Kamari, Y.; Harats, D. Intolerance to statins: Mechanisms and management. Diabetes Care 2013, 36, S325–S330. [Google Scholar] [CrossRef]
- Mannu, G.S.; Zaman, M.J.S.; Gupta, A.; Rehman, H.U.; Myint, P.K. Evidence of lifestyle modification in the management of hypercholesterolemia. Curr. Cardiol. Rev. 2013, 9, 2–14. [Google Scholar]
- Ahn, T.; Suh, S.Y.; Lee, K.; Kang, W.C.; Han, S.H.; Ahn, Y.; Jeong, M.H. Clinical outcomes according to the achievement of target low density lipoprotein-cholesterol in patients with acute myocardial infarction. Korean Circ. J. 2017, 47, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.W.; Chau, R.Y.; Cheung, H.Y.; Yu, C.M.; Lam, Y.Y.; Yan, B.P. How low should we target the LDL goal to improve survival for acute coronary syndrome patients in Hong Kong? BMC Cardiovasc. Disord. 2015, 15, 117. [Google Scholar] [CrossRef] [PubMed]
- White, C.W.; Gobel, F.L.; Campeau, L.; Knatterud, G.L.; Forman, S.A.; Forrester, J.S.; Geller, N.L.; Herd, J.A.; Hickey, A.; Hoogwerf, B.J.; et al. Post Coronary Artery Bypass Graft Trial Investigators. Effect of an aggressive lipid-lowering strategy on progression of atherosclerosis in the left main coronary artery from patients in the post coronary artery bypass graft trial. Circulation 2001, 104, 2660–2665. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Ji, F.; Yu, X.; Wang, X. Factors associated with unattained LDL-cholesterol goals in Chinese patients with acute coronary syndrome one year after percutaneous coronary intervention. Medicine 2017, 96, e5469. [Google Scholar] [CrossRef]
| Group 1 (N = 343) | Group 2 (N = 172) | p-Value | |
|---|---|---|---|
| General demographics | |||
| Age (years) | 60 ± 12.7 | 59 ± 12.9 | 0.211 |
| Male sex (%) | 284 (82.8) | 135 (78.5) | 0.609 |
| BMI (kg/m2) | 26.20 ± 9.46 | 25.87 ± 4.04 | 0.668 |
| Comorbidities | |||
| Diabetes mellitus (%) | 128 (37.3) | 53 (30.8) | 0.171 |
| Current smoker (%) | 204 (59.5) | 105 (61.0) | 0.775 |
| Hypertension (%) | 199 (58.0) | 110 (64.0) | 0.215 |
| Prior MI (%) | 13 (3.8) | 9 (5.2) | 0.491 |
| Prior stroke (%) | 17 (5.0) | 6 (3.5) | 0.506 |
| CKD stage ≥ 3 (eGFR < 60 mL/min/1.73 m2) | 45 (13.1) | 20 (11.6) | 0.675 |
| ESRD on maintenance hemodialysis (%) | 9 (2.6) | 3 (1.7) | 0.759 |
| Dyslipidemia with prior statin use (%) | 144 (42.0) | 75 (43.6) | 0.777 |
| Advanced heart failure (%) | 3 (0.9) | 1 (0.6) | 1.000 |
| The severity of MI | |||
| SBP (mmHg) | 139.82 ± 33.28 | 141.67 ± 32.90 | 0.551 |
| Killip level (%) | 0.721 | ||
| I, II | 295 (86.0) | 146 (84.9) | |
| III, IV | 48 (14.0) | 26 (15.1) | |
| Timing of primary PCI | |||
| Door-to-balloon time (min) | 69.04 ± 45.04 | 83.64 ± 46.17 | 0.094 |
| Reperfusion time (min) | 17.81 ± 7.39 | 18.82 ± 8.42 | 0.167 |
| Pain-to-reperfusion time (min) | 225.49 ± 156.17 | 208.59 ± 101.83 | 0.575 |
| Laboratory examination | |||
| White blood cell count (×103) | 11.1 ± 3.6 | 11.0 ± 3.7 | 0.788 |
| Hemoglobin (gm/dL) | 14.5 ± 2.0 | 14.6 ± 2.0 | 0.595 |
| Blood fasting sugar (mg/dL) | 180.8 ± 90.5 | 173.6 ± 82.6 | 0.421 |
| HbA1C (%) | 6.92 ± 1.85 | 6.71 ± 1.56 | 0.200 |
| Creatinine (except ESRD) (mg/dL) | 1.11 ± 0.51 | 1.08 ± 0.36 | 0.475 |
| Total cholesterol (mg/dL) | 178.96 ± 49.25 | 185.11 ± 42.27 | 0.164 |
| LDL-cholesterol (mg/dL) | 109.32 ± 40.58 | 113.49 ± 34.16 | 0.247 |
| >130 mg/dL (%) | 83 (24.2) | 55 (32.0) | 0.073 |
| HDL-cholesterol (mg/dL) | 41.11 ± 10.75 | 41.04 ± 12.33 | 0.943 |
| <40 mg/dL (%) | 173 (50.4) | 80 (46.5) | 0.455 |
| Peak troponin-I (ng/mL) | 50.93 ± 35.99 | 46.25 ± 34.12 | 0.162 |
| LVEF (%) | 57.40 ± 12.71 | 56.32 ± 12.60 | 0.366 |
| Infarcted territory (%) | 0.400 | ||
| Anterior wall | 184 (53.6) | 85 (49.4) | |
| Non-anterior wall | 159 (46.4) | 87 (50.6) | |
| Characteristics of coronary artery disease | |||
| Single or multiple vessel disease (%) | 0.983 | ||
| Single vessel disease | 129 (37.6) | 67 (39.0) | |
| Multiple vessel disease | 214 (62.4) | 105 (61.0) | |
| Non-culprit lesion stenosis ≥ 70% (%) | 144 (67.3) | 76 (72.4) | 0.210 |
| Left main coronary artery disease (%) | 16 (4.7) | 17 (9.9) | 0.034 |
| Post-MI Medications | |||
| ACEI/ARBs (%) | 314 (94.3) | 153 (91.1) | 0.190 |
| Beta-blockers (%) | 298 (89.5) | 148 (88.1) | 0.328 |
| Kept the same brand of statin therapy | 316 (92.1) | 151 (87.8) | 0.147 |
| The change of lipid-lower strategy | |||
| Increasement of the statin dose (%) | 55 (16.0) | 53 (30.8) | < 0.001 |
| Add ezetimibe (%) | 9 (2.6) | 22 (12.8) | < 0.001 |
| Group 1 (N = 343) | Group 2 (N = 172) | p-Value | |
|---|---|---|---|
| Primary PCI angiography | |||
| Culprit vessel | |||
| Pre-PCI TIMI flow | 0.192 | ||
| ≥2 (%) | 79 (23.6) | 49 (29.3) | |
| ≤1 (%) | 264 (76.4) | 123 (70.7) | |
| Pre-PCI stenosis (%) | 95.15 ± 8.35 | 93.46 ± 9.82 | 0.046 |
| Pre-PCI MLD (mm) | 0.14 ± 0.05 | 0.23 ± 0.12 | 0.005 |
| Pre-PCI RLD (mm) | 3.20 ± 0.57 | 3.25 ± 0.60 | 0.380 |
| Post-PCI TIMI flow | 0.668 | ||
| ≥2 (%) | 340 (99.1) | 170 (98.8) | |
| ≤1 (%) | 3 (0.9) | 2 (1.2) | |
| Post-PCI stenosis (%) | 12.62 ± 10.31 | 12.46 ± 7.23 | 0.856 |
| Post-PCI MLD (mm) | 2.86 ± 0.56 | 2.84 ± 0.50 | 0.708 |
| Post-PCI RLD (mm) | 3.34 ± 0.52 | 3.35 ± 0.58 | 0.856 |
| Distal embolization (%) | 12 (3.5) | 6 (3.5) | 1.000 |
| Method of perfusion | 0.442 | ||
| Balloon angioplasty alone (%) | 15 (4.4) | 12 (7.0) | |
| Bare-metal stents (%) | 123 (35.9) | 58 (33.7) | |
| Drug-eluting stents (%) | 205 (59.8) | 102 (59.3) | |
| Procedural device | |||
| IABP (%) | 49 (14.3) | 22 (12.8) | 0.686 |
| ECMO (%) | 4 (1.2) | 2 (1.2) | 1.000 |
| Post PCI acute kidney injury (%) | 30 (8.7) | 11 (6.4) | 0.393 |
| Group 1 (N = 343) | Group 2 (N = 172) | p-Value | |
|---|---|---|---|
| Recurrent angina (%) | 30 (8.7) | 16 (9.3) | 0.870 |
| Target-vessel revascularization (%) | 8 (2.3) | 6 (3.5) | 0.566 |
| Recurrent myocardial infarction (%) | 5 (1.5) | 2 (1.2) | 1.000 |
| Stroke (%) | 1 (0.3) | 0 (0) | 1.000 |
| Group 1 (N = 343) | Group 2 (N = 172) | p-Value | |
|---|---|---|---|
| LDL-C level (mg/dL) | 54.24 ± 15.18 | 92.73 ± 22.48 | < 0.001 |
| LDL-C < 70 mg/dL (%) | 323 (94.2) | 0 (0) | < 0.001 |
| The change of reduction > 50% (%) | 172 (50.1) | 0 (0) | < 0.001 |
| The average reduction of LDL-C (mg/dL) | −55.08 ± 36.86 | −20.77 ± 36.78 | < 0.001 |
| The average percentage of LDL-C reduction (%) | −44.61 ± 25.12 | −6.79 ± 32.86 | < 0.001 |
| Variables | Univariate Analyses | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Male | 0.812 | 0.404–1.634 | 0.560 | |||
| Age | 1.009 | 0.995–1.024 | 0.211 | |||
| BMI | 1.006 | 0.980–1.032 | 0.671 | |||
| Diabetes mellitus | 0.748 | 0.506–1.106 | 0.145 | 0.651 | 0.435–0.991 | 0.045 |
| Current smoker | 1.068 | 0.734–1.553 | 0.731 | |||
| Hypertension | 1.284 | 0.880–1.874 | 0.195 | 1.461 | 0.975–2.985 | 0.066 |
| Prior MI | 1.402 | 0.587–3.347 | 0.447 | |||
| Prior stroke | 0.693 | 0.268–1.791 | 0.449 | |||
| CKD stage ≥ 3 (eGFR < 60 mL/min/1.73 m2) | 0.871 | 0.497–1.528 | 0.631 | |||
| Dyslipidemia with prior statin use | 1.069 | 0.738–1.547 | 0.725 | |||
| Blood fasting sugar (mg/dL) | 1.001 | 0.999–1.003 | 0.420 | |||
| HbA1C (%) | 1.074 | 0.963–1.199 | 0.201 | 1.049 | 0.910–1.209 | 0.510 |
| Total cholesterol (mg/dL) | 0.997 | 0.993–1.001 | 0.165 | 0.999 | 0.993–1.004 | 0.620 |
| LDL-cholesterol (mg/dL) | 0.997 | 0.993–1.002 | 0.248 | |||
| Initial LDL-C >130 mg/dL | 1.473 | 0.983–2.207 | 0.061 | 1.583 | 1.038–2.415 | 0.033 |
| HDL-cholesterol (mg/dL) | 1.001 | 0.984–1.017 | 0.943 | |||
| Initial HDL-C < 40 mg/dL | 0.854 | 0.592–1.233 | 0.401 | |||
| Multiple vessel coronary disease | 1.023 | 0.829–1.262 | 0.831 | |||
| Left main coronary artery disease | 2.242 | 1.103–4.554 | 0.026 | 2.376 | 1.149–4.915 | 0.020 |
| One-year post-MI angina | 1.070 | 0.566–2.022 | 0.835 | |||
| One-year TVR | 1.514 | 0.517–4.433 | 0.450 | |||
| One-year recurrent MI | 0.795 | 0.153–4.142 | 0.786 | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.-C.; Fang, C.-Y.; Chen, C.-J.; Yang, C.-H.; Wu, C.-J.; Fang, H.-Y. The Clinical Outcomes Based on the Achievement of Low-Density Lipoprotein Cholesterol Targets after ST Elevation Myocardial Infarction. J. Clin. Med. 2020, 9, 79. https://doi.org/10.3390/jcm9010079
Lee W-C, Fang C-Y, Chen C-J, Yang C-H, Wu C-J, Fang H-Y. The Clinical Outcomes Based on the Achievement of Low-Density Lipoprotein Cholesterol Targets after ST Elevation Myocardial Infarction. Journal of Clinical Medicine. 2020; 9(1):79. https://doi.org/10.3390/jcm9010079
Chicago/Turabian StyleLee, Wei-Chieh, Chih-Yuan Fang, Chien-Jen Chen, Cheng-Hsu Yang, Chiung-Jen Wu, and Hsiu-Yu Fang. 2020. "The Clinical Outcomes Based on the Achievement of Low-Density Lipoprotein Cholesterol Targets after ST Elevation Myocardial Infarction" Journal of Clinical Medicine 9, no. 1: 79. https://doi.org/10.3390/jcm9010079
APA StyleLee, W.-C., Fang, C.-Y., Chen, C.-J., Yang, C.-H., Wu, C.-J., & Fang, H.-Y. (2020). The Clinical Outcomes Based on the Achievement of Low-Density Lipoprotein Cholesterol Targets after ST Elevation Myocardial Infarction. Journal of Clinical Medicine, 9(1), 79. https://doi.org/10.3390/jcm9010079





