Association between On-Treatment Haemoglobin A1c and All-Cause Mortality in Individuals with Type 2 Diabetes: Importance of Personalized Goals and Type of Anti-Hyperglycaemic Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Subjects
2.3. All-Cause Mortality
2.4. Traditional Cardiovascular Disease (CVD) Risk Factors
2.5. Complications
2.6. Categorization of Patients
2.7. Statistical Analysis
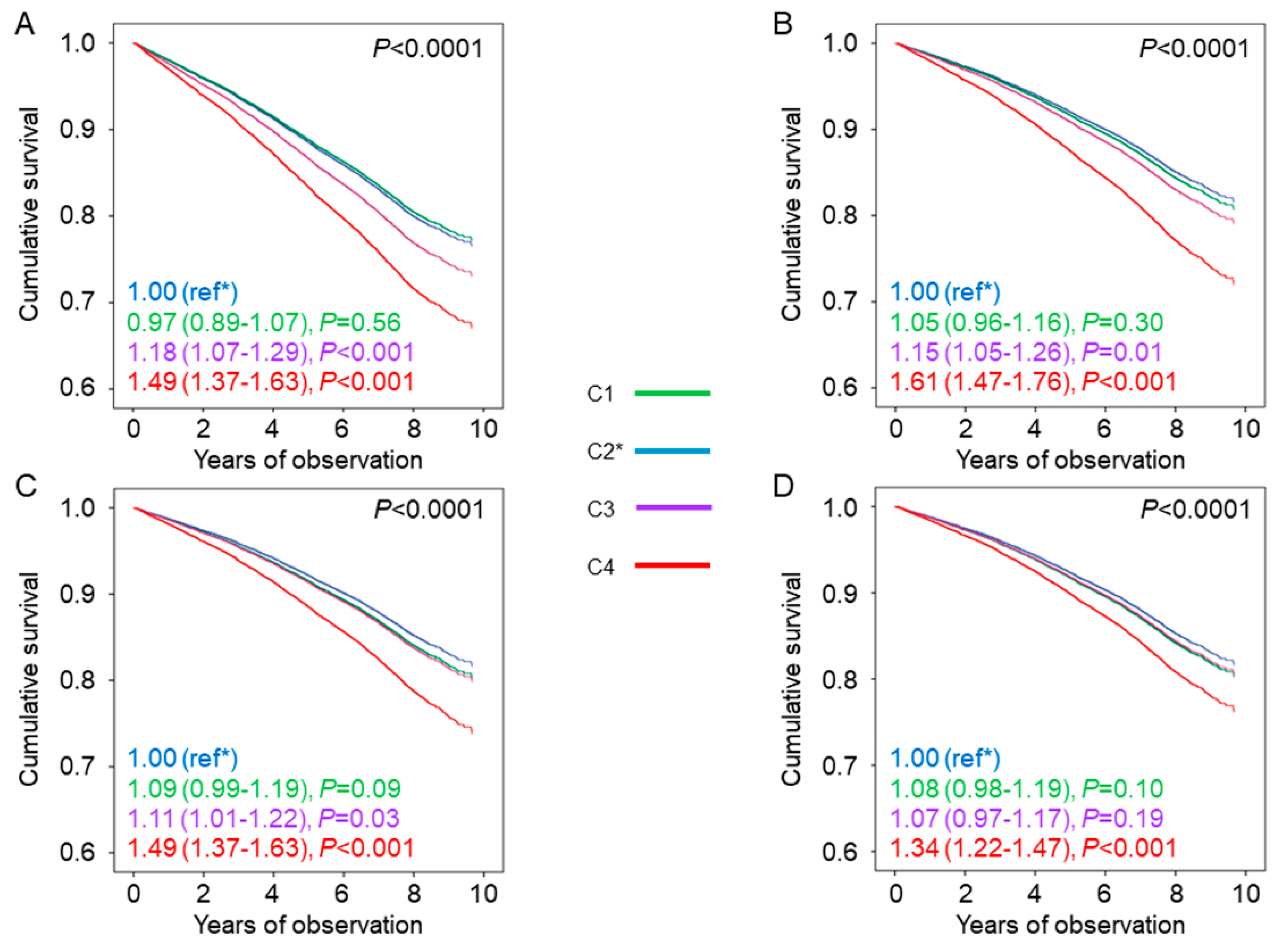
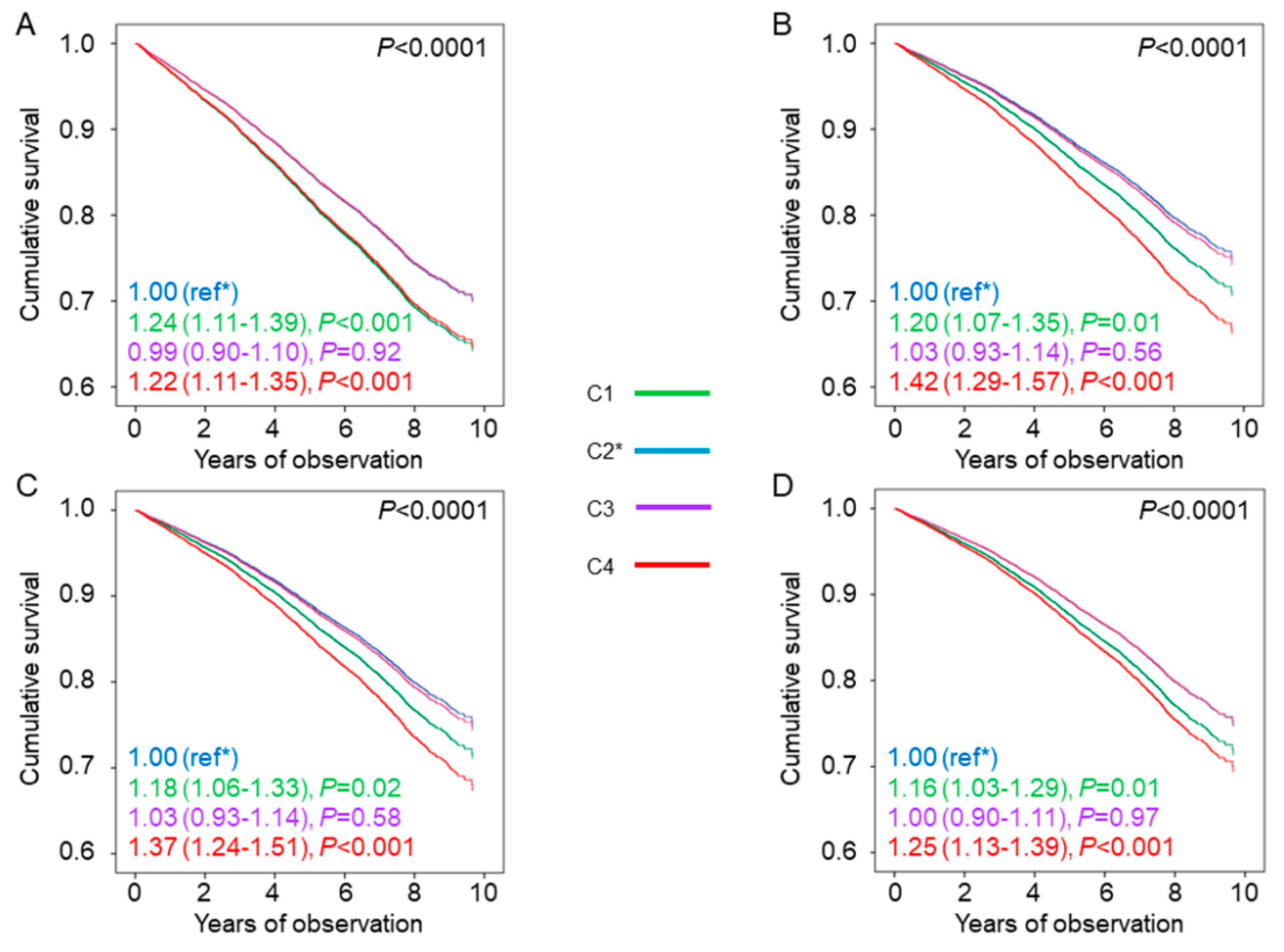
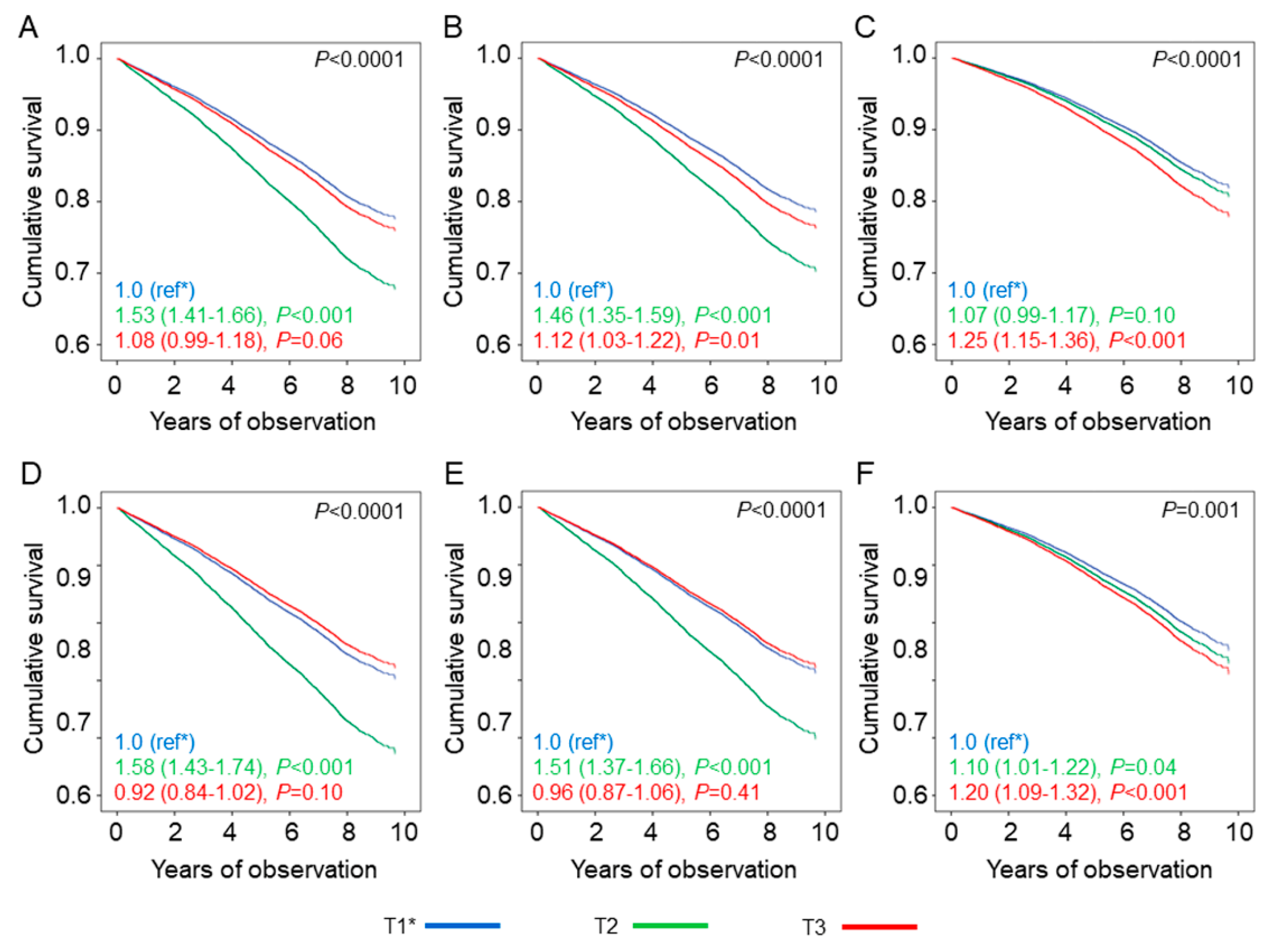
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability
Abbreviations
| CVD | cardiovascular disease |
| UKPDS | United Kingdom Prospective Diabetes Study |
| ACCORD | Action to Control Cardiovascular Risk in Diabetes |
| ADVANCE | Action in Diabetes and Vascular Disease |
| VADT | Veterans Affairs Diabetes Trial |
| HbA1c | haemoglobin A1c |
| RIACE | Renal Insufficiency And Cardiovascular Events |
| eGFR | estimated glomerular filtration rate |
| BP | blood pressure |
| BMI | body mass index |
| DCCT | Diabetes Control and Complications Trial |
| HDL | High-density lipoprotein |
| LDL | Low-density lipoprotein |
| DKD | diabetic kidney disease |
| DR | diabetic retinopathy |
| HR | hazard ratio |
| CI | Confidence interval |
| ADA | American Diabetes Association |
| NHANES | National Health And Nutrition Examination Survey |
References
- Rodriguez-Gutierrez, R.; Lipska, K.J.; McCoy, R.G. Intensive glycemic control in type 2 diabetes mellitus—A balancing act of latent benefit and avoidable harm: A teachable moment. JAMA Intern. Med. 2016, 176, 300–301. [Google Scholar] [CrossRef][Green Version]
- Holman, R.R.; Paul, S.K.; Bethel, M.A.; Matthews, D.R.; Neil, H.A. 10-year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 2008, 359, 1577–1589. [Google Scholar] [CrossRef] [PubMed]
- Action to Control Cardiovascular Risk in Diabetes Study Group; Gerstein, H.C.; Miller, M.E.; Byington, R.P.; Goff, D.C., Jr.; Bigger, J.T.; Buse, J.B.; Cushman, W.C.; Genuth, S.; Ismail-Beigi, F.; et al. Effects of intensive glucose lowering in type 2 diabetes. N. Engl. J. Med. 2008, 8, 2545–2559. [Google Scholar] [CrossRef]
- Advance Collaborative Group; Patel, A.; MacMahon, S.; Chalmers, J.; Neal, B.; Billot, L.; Woodward, M.; Marre, M.; Cooper, M.; Glasziou, P.; et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 2008, 358, 2560–2572. [Google Scholar] [CrossRef] [PubMed]
- Duckworth, W.; Abraira, C.; Moritz, T.; Reda, D.; Emanuele, N.; Reaven, P.D.; Zieve, F.J.; Marks, J.; Davis, S.N.; Hayward, R.; et al. Glucose control and vascular complications in veterans with type 2 diabetes. N. Engl. J. Med. 2009, 360, 129–139. [Google Scholar] [CrossRef]
- Del Prato, S. Megatrials in type 2 diabetes. From excitement to frustration? Diabetologia 2009, 52, 1219–1226. [Google Scholar] [CrossRef]
- Hill, D.; Fisher, M. The effect of intensive glycaemic control on cardiovascular outcomes. Diabetes Obes. Metab. 2010, 12, 641–647. [Google Scholar] [CrossRef]
- Inzucchi, S.E.; Bergenstal, R.M.; Buse, J.B.; Diamant, M.; Ferrannini, E.; Nauck, M.; Peters, A.L.; Tsapas, A.; Wender, R.; Matthews, D.R.; et al. Management of hyperglycemia in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012, 35, 1364–1379. [Google Scholar] [CrossRef]
- Bonds, D.E.; Miller, M.E.; Bergenstal, R.M.; Buse, J.B.; Byington, R.P.; Cutler, J.A.; Dudl, R.J.; Ismail-Beigi, F.; Kimel, A.R.; Hoogwerf, B.; et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: Retrospective epidemiological analysis of the ACCORD study. BMJ 2010, 340, b4909. [Google Scholar] [CrossRef]
- Zoungas, S.; Patel, A.; Chalmers, J.; de Galan, B.E.; Li, Q.; Billot, L.; Woodward, M.; Ninomiya, T.; Neal, B.; MacMahon, S.; et al. Severe hypoglycemia and risks of vascular events and death. N. Engl. J. Med. 2010, 363, 1410–1418. [Google Scholar] [CrossRef]
- Davis, S.N.; Duckworth, W.; Emanuele, N.; Hayward, R.A.; Wiitala, W.L.; Thottapurathu, L.; Reda, D.J.; Reaven, P.D.; Investigators of the Veterans Affairs Diabetes Trial. Effects of severe hypoglycemia on cardiovascular outcomes and death in the Veterans Affairs Diabetes Trial. Diabetes Care 2019, 42, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Riddle, M.C.; Ambrosius, W.T.; Brillon, D.J.; Buse, J.B.; Byington, R.P.; Cohen, R.M.; Goff, D.C., Jr.; Malozowski, S.; Margolis, K.L.; Probstfield, J.L.; et al. Epidemiologic relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial. Diabetes Care 2010, 33, 983–990. [Google Scholar] [CrossRef] [PubMed]
- Penno, G.; Solini, A.; Bonora, E.; Fondelli, C.; Orsi, E.; Zerbini, G.; Trevisan, R.; Vedovato, M.; Gruden, G.; Cavalot, F.; et al. Clinical significance of nonalbuminuric renal impairment in type 2 diabetes. J. Hypertens. 2011, 29, 1802–1809. [Google Scholar] [CrossRef] [PubMed]
- Orsi, E.; Solini, A.; Bonora, E.; Fondelli, C.; Trevisan, R.; Vedovato, M.; Cavalot, F.; Gruden, G.; Morano, S.; Nicolucci, A.; et al. Haemoglobin A1c variability is a strong, independent predictor of all-cause mortality in patients with type 2 diabetes. Diabetes Obes. Metab. 2018, 20, 1885–1893. [Google Scholar] [CrossRef] [PubMed]
- Penno, G.; Solini, A.; Bonora, E.; Fondelli, C.; Orsi, E.; Zerbini, G.; Trevisan, R.; Vedovato, M.; Gruden, G.; Laviola, L.; et al. Gender differences in cardiovascular disease risk factors, treatments and complications in patients with type 2 diabetes: The RIACE Italian multicentre study. J. Intern. Med. 2013, 274, 176–191. [Google Scholar] [CrossRef]
- Pugliese, G.; Solini, A.; Fondelli, C.; Trevisan, R.; Vedovato, M.; Nicolucci, A.; Penno, G.; Renal Insufficiency And Cardiovascular Events (RIACE) Study Group. Reproducibility of albuminuria in type 2 diabetic subjects. Findings from the Renal Insufficiency and Cardiovascular Events (RIACE) Study. Nephrol. Dial. Transplant. 2011, 26, 3950–3954. [Google Scholar] [CrossRef]
- Penno, G.; Solini, A.; Zoppini, G.; Orsi, E.; Zerbini, G.; Trevisan, R.; Gruden, G.; Cavalot, F.; Laviola, L.; Morano, S.; et al. Rate and determinants of association between advanced retinopathy and chronic kidney disease in patients with type 2 diabetes: The Renal Insufficiency and Cardiovascular Events (RIACE) Italian Multicenter Study. Diabetes Care 2012, 35, 2317–2323. [Google Scholar] [CrossRef]
- Solini, S.; Penno, G.; Bonora, E.; Fondelli, C.; Orsi, E.; Arosio, M.; Trevisan, R.; Vedovato, M.; Cignarelli, M.; Andreaozzi, F.; et al. Diverging association of reduced glomerular filtration rate and albuminuria with coronary and noncoronary events in patients with type 2 diabetes: The Renal Insufficiency and Cardiovascular Events (RIACE) Italian Multicentre Study. Diabetes Care 2012, 35, 143–149. [Google Scholar] [CrossRef]
- Penno, G.; Solini, A.; Orsi, E.; Bonora, E.; Fondelli, C.; Trevisan, R.; Vedovato, M.; Cavalot, F.; Lamacchia, O.; Scardapane, M.; et al. Non-albuminuric renal impairment is a strong predictor of mortality in individuals with type 2 diabetes: The Renal Insufficiency and Cardiovascular Events (RIACE) Italian multicentre study. Diabetologia 2018, 61, 2277–2289. [Google Scholar] [CrossRef]
- Bruce, D.G.; Davis, W.A.; Davis, T.M.E. Glycaemic control and mortality in older people with type 2 diabetes: The Fremantle Diabetes Study Phase II. Diabetes Obes. Metab. 2018, 20, 2852–2859. [Google Scholar] [CrossRef]
- Currie, C.J.; Peters, J.R.; Tynan, A.; Evans, M.; Heine, R.J.; Bracco, O.L.; Zagar, T.; Poole, C.D. Survival as a function of HbA(1c) in people with type 2 diabetes: A retrospective cohort study. Lancet 2010, 375, 481–489. [Google Scholar] [CrossRef]
- Nichols, G.A.; Joshua-Gotlib, S.; Parasuraman, S. Glycemic control and risk of cardiovascular disease hospitalization and all-cause mortality. J. Am. Coll. Cardiol. 2013, 62, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.S.; Liu, J.Y.; Moffet, H.H.; John, P.M.; Karter, A.J. Glycemic control, complications, and death in older diabetic patients: The diabetes and aging study. Diabetes Care 2011, 34, 1329–1336. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial Research Group; Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O.; Davis, M.; Rand, L.; Siebert, C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Stratton, I.M.; Adler, A.I.; Neil, H.A.; Matthews, D.R.; Manley, S.E.; Cull, C.A.; Hadden, D.; Turner, R.C.; Holman, R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 2000, 321, 405–412. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care 2008, 31 (Suppl. 1), S12–S54. [Google Scholar] [CrossRef]
- Ali, M.K.; Bullard, K.M.; Saaddine, J.B.; Cowie, C.C.; Imperatore, G.; Gregg, E.W. Achievement of goals in U.S. diabetes care, 1999–2010. N. Engl. J. Med. 2013, 368, 1613–1624. [Google Scholar] [CrossRef]
- Carls, G.; Huynh, J.; Tuttle, E.; Yee, J.; Edelman, S.V. Achievement of glycated hemoglobin goals in the US remains unchanged through 2014. Diabetes Ther. 2017, 8, 863–873. [Google Scholar] [CrossRef]
- Lipska, K.J.; Ross, J.S.; Miao, Y.; Shah, N.D.; Lee, S.J.; Steinman, M.A. Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. JAMA Intern. Med. 2015, 175, 356–362. [Google Scholar] [CrossRef]
- Arnold, S.V.; Lipska, K.J.; Wang, J.; Seman, L.; Mehta, S.N.; Kosiborod, M. Use of intensive glycemic management in older adults with diabetes mellitus. J. Am. Geriatr Soc. 2018, 66, 1190–1194. [Google Scholar] [CrossRef]
- Sussman, J.B.; Kerr, E.A.; Saini, S.D.; Holleman, R.G.; Klamerus, M.L.; Min, L.C.; Vijan, S.; Hofer, T.P. Rates of deintensification of blood pressure and glycemic medication treatment based on levels of control and life expectancy in older patients with diabetes mellitus. JAMA Intern. Med. 2015, 175, 1942–1949. [Google Scholar] [CrossRef] [PubMed]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020, 43 (Suppl. 1), S66–S76. [Google Scholar] [CrossRef] [PubMed]
| Variables | C1 | C2 | C3 | C4 | p-Value |
|---|---|---|---|---|---|
| N (%) | 3645 (23.3) | 5081 (32.5) | 3608 (23.0) | 3322 (21.2) | |
| Deaths, n (%) | 737 (20.2) | 1049 (20.6) | 858 (23.8) | 958 (28.8) | <0.001 |
| Age, years | 65.6 ± 10.6 | 67.1 ± 9.9 | 67.1 ± 10.2 | 66.3 ± 10.8 | <0.001 |
| Male gender, n (%) | 2233 (57.1) | 2903 (55.9) | 2018 (52.6) | 1748 (56.9) | <0.001 |
| Smoking, n (%) | <0.001 | ||||
| Never | 2021 (55.4) | 2850 (56.1) | 2090 (57.9) | 1888 (56.8) | |
| Former | 1107 (30.4) | 1472 (29.0) | 960 (26.6) | 868 (26.1) | |
| Current | 517 (14.2) | 759 (14.9) | 558 (15.5) | 566 (17.0) | |
| Diabetes duration, years | 9.0 ± 8.9 | 12.5 ± 9.9 | 15.7 ± 10.1 | 16.1 ± 10.2 | <0.001 |
| HbA1c, % | 5.93 ± 0.46 | 6.97 ± 0.29 | 7.93 ± 0.28 | 9.77 ± 1.31 | <0.001 |
| (mmol·mol−1) | (41.3 ± 5.0) | (52.7 ± 3.2) | (63.2 ± 3.1) | (83.3 ± 14.3) | |
| BMI, kg·m−2 | 28.6 ± 4.9 | 28.6 ± 4.9 | 29.1 ± 5.2 | 29.7 ± 5.5 | <0.001 |
| Waist circumference, cm | 101.8 ± 10.0 | 101.9 ± 10.0 | 102.7 ± 10.6 | 104.0 ± 11.1 | <0.001 |
| Triglycerides, mmol·L−1 | 1.46 ± 0.94 | 1.49 ± 0.85 | 1.56 ± 0.89 | 1.84 ± 1.27 | <0.001 |
| Total cholesterol, mmol L−1 | 4.74 ± 0.96 | 4.77 ± 0.95 | 4.75 ± 0.96 | 4.89 ± 1.09 | <0.001 |
| HDL cholesterol, mmol·L−1 | 1.31 ± 0.36 | 1.31 ± 0.35 | 1.28 ± 0.34 | 1.24 ± 0.35 | <0.001 |
| LDL cholesterol, mmol L−1 | 3.43 ± 0.92 | 3.46 ± 0.91 | 3.47 ± 0.92 | 3.65 ± 1.05 | 0.01 |
| Non-HDL cholesterol, mmol L−1 | 2.78 ± 0.84 | 2.79 ± 0.83 | 2.76 ± 0.82 | 2.83 ± 0.90 | <0.001 |
| Systolic BP, mmHg | 136.3 ± 17.5 | 137.9 ± 17.7 | 139.6 ± 18.2 | 138.6 ± 18.7 | <0.001 |
| Diastolic BP, mmHg | 79.0 ± 9.4 | 78.6 ± 9.2 | 78.9 ± 9.5 | 78.7 ± 9.7 | 0.16 |
| Pulse pressure, mmHg | 57.3 ± 15.3 | 59.3 ± 15.6 | 60.8 ± 16.0 | 60.0 ± 15.8 | <0.001 |
| Anti-hyperglycaemic treatment, n (%) | |||||
| Lifestyle | 1017 (27.9) | 762 (15.0) | 192 (5.3) | 142 (4.3) | <0.001 |
| Insulin | 440 (12.1) | 913 (18.0) | 1062 (29.4) | 1509 (45.4) | <0.001 |
| Non-insulin agents | 2188 (60.0) | 3406 (67.0) | 2354 (65.2) | 1671 (50.3) | <0.001 |
| Metformin | 1746 (47.9) | 2840 (55.9) | 2206 (61.1) | 1853 (55.8) | <0.001 |
| Pioglitazone | 87 (2.4) | 167 (3.3) | 163 (4.5) | 137 (4.1) | <0.001 |
| Acarbose | 36 (1.0) | 43 (0.8) | 47 (1.3) | 44 (1.3) | 0.09 |
| Sulfonylureas | 820 (22.5) | 1677 (33.0) | 1472 (40.8) | 1281 (38.6) | <0.001 |
| Repaglinide | 335 (9.2) | 537 (10.6) | 371 (10.3) | 282 (8.5) | 0.01 |
| Agents causing hypoglycaemia, n (%) | 1538 (42.2) | 2944 (57.9) | 2646 (73.3) | 2702 (81.3) | <0.001 |
| Lipid-lowering treatment, n (%) | 1572 (43.1) | 2389 (47.0) | 1728 (47.9) | 1549 (46.6) | <0.001 |
| Anti-hypertensive treatment, n (%) | 2509 (68.8) | 3611 (71.1) | 2601 (72.1) | 2351 (70.8) | <0.001 |
| Albuminuria, mg·day−1 | 53.8 ± 225.5 | 68.7 ± 373.2 | 74.4 ± 329.7 | 96.0 ± 293.1 | <0.001 |
| Serum creatinine, μmol·L−1 | 81.3 ± 38.0 | 80.4 ± 35.4 | 80.4 ± 31.8 | 82.2 ± 31.8 | 0.27 |
| eGFR, mL·min−1·1.73 m−2 | 81.6 ± 21.0 | 80.3 ± 20.1 | 79.9 ± 20.5 | 79.2 ± 22.6 | <0.001 |
| DKD phenotype, n (%) | <0.001 | ||||
| No DKD | 2554 (70.1) | 3385 (66.6) | 2269 (62.9) | 1776 (53.5) | |
| Albuminuric DKD with preserved eGFR | 532 (14.6) | 877 (17.3) | 691 (19.2) | 866 (26.1) | |
| Non-albuminuric DKD | 321 (8.8) | 465 (9.2) | 360 (10.0) | 330 (9.9) | |
| Albuminuric DKD with reduced eGFR | 238 (6.5) | 354 (7.0) | 288 (8.0) | 350 (10.5) | |
| DR, n (%) | <0.001 | ||||
| No DR | 3178 (87.2) | 4185 (82.4) | 2658 (73.7) | 2168 (63.5) | |
| Non-advanced DR | 242 (6.6) | 503 (9.9) | 586 (16.2) | 616 (18.5) | |
| Advanced DR | 225 (6.2) | 393 (7.7) | 364 (10.1) | 538 (16.2) | |
| CVD, n (%) | |||||
| Any | 699 (19.2) | 1086 (21.4) | 906 (25.1) | 929 (28.0) | <0.001 |
| Myocardial infarction | 354 (9.7) | 514 (10.1) | 445 (12.3) | 429 (12.9) | <0.001 |
| Coronary revascularization | 295 (8.1) | 487 (9.6) | 411 (11.4) | 386 (11.6) | <0.001 |
| Stroke | 126 (3.5) | 143 (2.8) | 118 (3.3) | 126 (3.8) | 0.09 |
| Carotid revascularization | 120 (3.3) | 240 (4.7) | 235 (6.5) | 261 (7.9) | <0.001 |
| Ulcer/gangrene/amputation | 92 (2.5) | 167 (3.3) | 131 (3.6) | 166 (5.0) | <0.001 |
| Lower limb revascularization | 65 (1.8) | 135 (2.7) | 121 (3.4) | 129 (3.9) | <0.001 |
| Comorbidities, n (%) | |||||
| Any | 682 (18.7) | 872 (17.2) | 620 (17.2) | 613 (18.5) | 0.15 |
| COPD | 173 (4.7) | 201 (4.0) | 142 (3.9) | 158 (4.8) | <0.001 |
| Chronic liver disease | 299 (8.2) | 415 (8.2) | 326 (9.0) | 321 (9.7) | 0.06 |
| Cancer | 279 (7.7) | 342 (6.7) | 215 (6.0) | 195 (5.9) | <0.001 |
| HbA1c Target Categories | Unadjusted | Adjusted | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||||||||
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| C2 (ref) | 1.00 | - | <0.001 | 1.00 | - | <0.001 | 1.00 | - | <0.001 | 1.00 | - | <0.001 |
| C1 | 0.92 | 0.78–1.10 | 0.36 | 1.01 | 0.85–1.20 | 0.94 | 1.03 | 0.87–1.23 | 0.70 | 1.03 | 0.87–1.22 | 0.74 |
| C3 | 1.36 | 1.12–1.66 | 0.01 | 1.34 | 1.10–1.63 | 0.01 | 1.28 | 1.05–1.55 | 0.02 | 1.26 | 1.04–1.54 | 0.02 |
| C4 | 1.67 | 1.35–2.07 | <0.001 | 1.72 | 1.39–2.13 | <0.001 | 1.59 | 1.28–1.97 | <0.001 | 1.50 | 1.21–1.86 | <0.001 |
| Variables | T1 | T2 | T3 | p-Value |
|---|---|---|---|---|
| n (%) | 4989 (31.9) | 4621 (29.5) | 6046 (38.6) | |
| Deaths, n (%) | 991 (19.9) | 1330 (28.8) | 1281 (21.2) | <0.001 |
| Age, years | 66.7 ± 9.9 | 69.4 ± 10.1 | 64.4 ± 10.3 | <0.001 |
| Male gender, n (%) | 2833 (56.8) | 2818 (61.0) | 3251 (53.8) | <0.001 |
| Smoking, n (%) | <0.001 | |||
| Never | 2837 (56.9) | 2581 (55.9) | 3431 (56.7) | |
| Former | 1435 (28.8) | 1455 (31.5) | 1517 (25.1) | |
| Current | 717 (14.4) | 585 (12.7) | 1098 (18.2) | |
| Diabetes duration, years | 12.7 ± 10.1 | 13.3 ± 10.7 | 13.6 ± 9.8 | <0.001 |
| HbA1c, % | 7.13 ± 0.57 | 6.22 ± 0.66 | 8.90 ± 1.40 | <0.001 |
| (mmol·mol−1) | (54.4 ± 6.2) | (44.5 ± 7.2) | (73.8 ± 15.3) | |
| BMI, kg·m−2 | 28.8 ± 5.0 | 28.2 ± 4.7 | 29.7 ± 5.5 | <0.001 |
| Waist circumference, cm | 102.1 ± 10.1 | 101.1 ± 9.7 | 103.9 ± 11.0 | <0.001 |
| Triglycerides, mmol·L−1 | 1.51 ± 0.89 | 1.42 ± 0.86 | 1.74 ± 1.14 | <0.001 |
| Total cholesterol, mmol·L−1 | 4.78 ± 0.95 | 4.69 ± 0.96 | 4.86 ± 1.04 | <0.001 |
| HDL cholesterol, mmol·L−1 | 1.30 ± 0.34 | 1.32 ± 0.37 | 1.26 ± 0.35 | <0.001 |
| LDL cholesterol, mmol·L−1 | 3.47 ± 0.91 | 3.37 ± 0.91 | 3.61 ± 1.00 | <0.001 |
| Non-HDL cholesterol, mmol·L−1 | 2.79 ± 0.82 | 2.73 ± 0.83 | 2.83 ± 0.88 | <0.001 |
| Systolic BP, mmHg | 138.3 ± 17.9 | 137.5 ± 17.9 | 138.2 ± 18.2 | 0.06 |
| Diastolic BP, mmHg | 79.0 ± 9.2 | 78.3 ± 9.5 | 78.9 ± 9.6 | 0.01 |
| Pulse pressure, mmHg | 59.4 ± 15.6 | 59.2 ± 15.8 | 59.3 ± 15.7 | 0.87 |
| Anti-hyperglycaemic treatment, n (%) | ||||
| Lifestyle | 810 (16.2) | 927 (20.1) | 376 (6.2) | <0.001 |
| Insulin | 972 (19.5) | 860 (18.6) | 2092 (34.6) | <0.001 |
| Non-insulin agents | 3207 (64.3) | 2834 (61.3) | 3578 (59.2) | <0.001 |
| Metformin | 2784 (55.8) | 2195 (47.5) | 3666 (60.6) | <0.001 |
| Pioglitazone | 181 (3.6) | 92 (2.0) | 281 (4.6) | <0.001 |
| Acarbose | 49 (1.0) | 47 (1.0) | 74 (1.2) | 0.41 |
| Sulfonylureas | 1610 (32.3) | 1314 (28.4) | 2326 (38.5) | <0.001 |
| Repaglinide | 461 (9.2) | 510 (11.0) | 554 (9.2) | 0.01 |
| Agents causing hypoglycaemia, n (%) | 2835 (56.8) | 2557 (55.3) | 4438 (73.4) | <0.001 |
| Lipid-lowering treatment, n (%) | 2314 (46.4) | 2148 (46.5) | 2776 (45.9) | 0.82 |
| Anti-hypertensive treatment, n (%) | 3504 (70.2) | 3449 (74.6) | 4119 (68.1) | <0.001 |
| Albuminuria, mg·day−1 | 64.1 ± 285.4 | 80.3 ± 377.0 | 73.0 ± 290.3 | 0.04 |
| Serum creatinine, μmol·L−1 | 79.6 ± 31.8 | 85.7±42.4 | 78.7±29.2 | <0.001 |
| eGFR, mL·min−1·1.73 m−2 | 81.0±19.7 | 76.6±21.7 | 82.5±21.0 | <0.001 |
| DKD phenotype, n (%) | <0.001 | |||
| No DKD | 3348 (67.1) | 2859 (61.9) | 3777 (62.5) | |
| Albuminuric DKD with preserved eGFR | 863 (17.3) | 767 (16.6) | 1336 (22.1) | |
| Non-albuminuric DKD | 461 (9.2) | 523 (11.3) | 492 (8.1) | |
| Albuminuric DKD with reduced eGFR | 317 (6.4) | 472 (10.2) | 441 (7.3) | |
| DR, n (%) | <0.001 | |||
| No DR | 4064 (81.5) | 3695 (80.0) | 4430 (73.3) | |
| Non-advanced DR | 529 (10.6) | 444 (9.6) | 974 (16.1) | |
| Advanced DR | 396 (7.9) | 482 (10.4) | 642 (10.6) | |
| CVD, n (%) | ||||
| Any | 1004 (20.1) | 1457 (31.5) | 1159 (19.2) | <0.001 |
| Myocardial infarction | 480 (9.6) | 703 (15.2) | 559 (9.2) | <0.001 |
| Coronary revascularization | 447 (9.0 | 617 (13.4) | 515 (8.5) | <0.001 |
| Stroke | 137 (2.7) | 231 (5.0) | 145 (2.4) | <0.001 |
| Carotid revascularization | 250 (5.0) | 308 (6.7) | 298 (4.9) | <0.001 |
| Ulcer/gangrene/amputation | 158 (3.2) | 217 (4.7) | 181 (3.0) | <0.001 |
| Lower limb revascularization | 122 (2.4) | 171 (3.7) | 157 (2.6) | <0.001 |
| Comorbidities n (%) | ||||
| Any | 756 (15.2) | 1261 (27.3) | 770 (12.7) | <0.001 |
| COPD | 167 (3.3) | 322 (7.0) | 185 (3.1) | <0.001 |
| Chronic liver disease | 385 (7.7) | 570 (12.3) | 406 (6.7) | <0.001 |
| Cancer | 276 (5.5) | 504 (10.9) | 251 (4.2) | <0.001 |
| HbA1c Target Categories | Unadjusted | Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | ||||||||
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| T1 (ref) | 1.00 | - | <0.001 | 1.00 | - | <0.001 | 1.00 | - | <0.001 |
| T2 | 1.54 | 1.31–1.82 | <0.001 | 1.49 | 1.26–1.75 | <0.001 | 1.08 | 0.92–1.28 | 0.34 |
| T3 | 1.11 | 0.92–1.33 | 0.290 | 1.14 | 0.94–1.37 | 0.19 | 1.21 | 1.01–1.46 | 0.04 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orsi, E.; Bonora, E.; Solini, A.; Fondelli, C.; Trevisan, R.; Vedovato, M.; Cavalot, F.; Zerbini, G.; Morano, S.; Nicolucci, A.; et al. Association between On-Treatment Haemoglobin A1c and All-Cause Mortality in Individuals with Type 2 Diabetes: Importance of Personalized Goals and Type of Anti-Hyperglycaemic Treatment. J. Clin. Med. 2020, 9, 246. https://doi.org/10.3390/jcm9010246
Orsi E, Bonora E, Solini A, Fondelli C, Trevisan R, Vedovato M, Cavalot F, Zerbini G, Morano S, Nicolucci A, et al. Association between On-Treatment Haemoglobin A1c and All-Cause Mortality in Individuals with Type 2 Diabetes: Importance of Personalized Goals and Type of Anti-Hyperglycaemic Treatment. Journal of Clinical Medicine. 2020; 9(1):246. https://doi.org/10.3390/jcm9010246
Chicago/Turabian StyleOrsi, Emanuela, Enzo Bonora, Anna Solini, Cecilia Fondelli, Roberto Trevisan, Monica Vedovato, Franco Cavalot, Gianpaolo Zerbini, Susanna Morano, Antonio Nicolucci, and et al. 2020. "Association between On-Treatment Haemoglobin A1c and All-Cause Mortality in Individuals with Type 2 Diabetes: Importance of Personalized Goals and Type of Anti-Hyperglycaemic Treatment" Journal of Clinical Medicine 9, no. 1: 246. https://doi.org/10.3390/jcm9010246
APA StyleOrsi, E., Bonora, E., Solini, A., Fondelli, C., Trevisan, R., Vedovato, M., Cavalot, F., Zerbini, G., Morano, S., Nicolucci, A., Penno, G., & Pugliese, G., for the Renal Insufficiency and Cardiovascular Events (RIACE) Study Group. (2020). Association between On-Treatment Haemoglobin A1c and All-Cause Mortality in Individuals with Type 2 Diabetes: Importance of Personalized Goals and Type of Anti-Hyperglycaemic Treatment. Journal of Clinical Medicine, 9(1), 246. https://doi.org/10.3390/jcm9010246







