Diagnostic Accuracy of Stool Tests for Colorectal Cancer Surveillance in Hodgkin Lymphoma Survivors
Abstract
1. Introduction
2. Materials and Methods
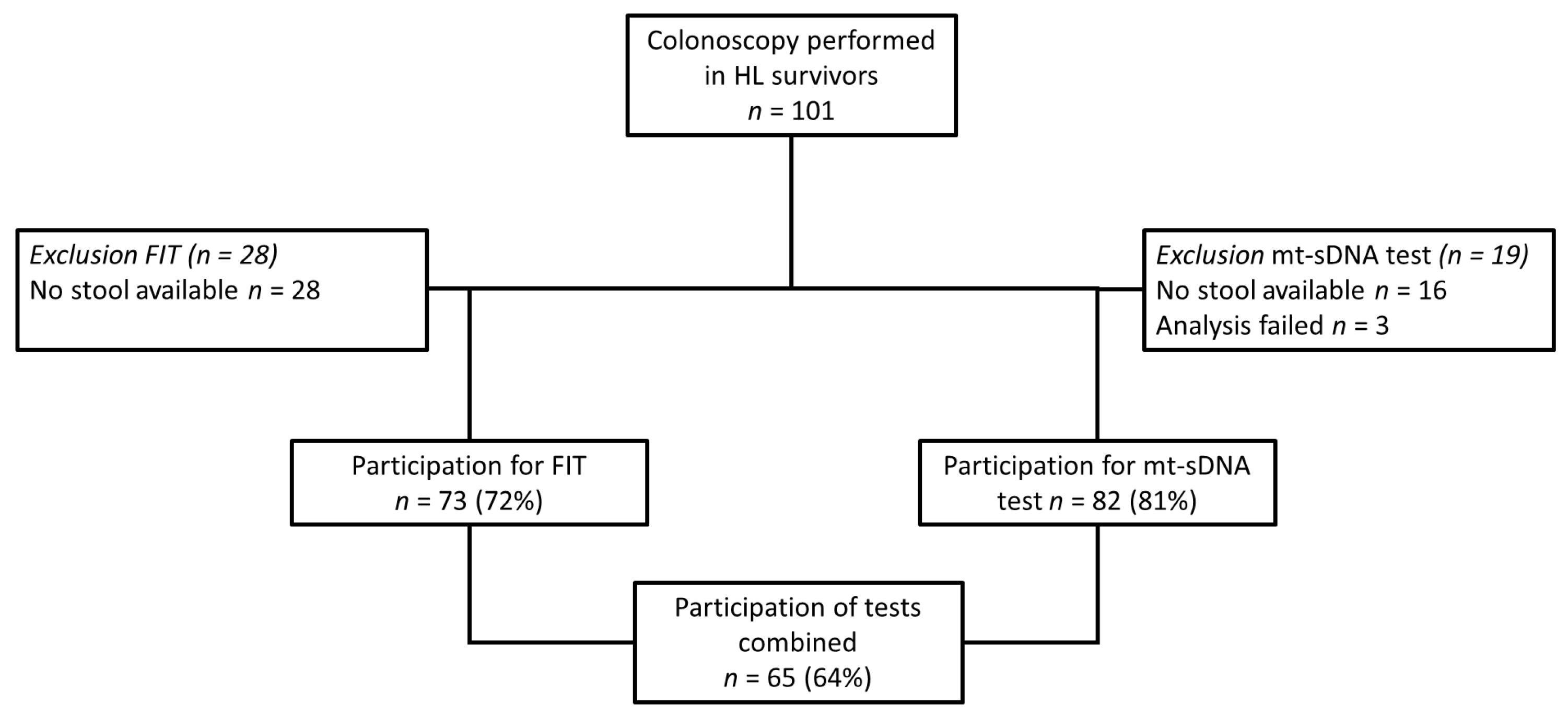
2.1. Study Population
2.2. Stool Collection
2.3. Fecal Immunochemical Test
2.4. Multi-Target Stool DNA Test
2.5. FIT and Mt-sDNA
2.6. Colonoscopy
2.7. Outcome Measures and Statistical Analysis
3. Results
3.1. Study Population
3.2. Colonoscopy Results
3.3. Fecal Immunochemical Test Results
3.4. Mt-sDNA Results
3.5. FIT10 and/or Mt-sDNA Results Combined
3.6. Diagnostic Accuracy of FIT and/or Mt-sDNA for the Most Advanced Lesion Per Participant Based on Location
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hodgson, D.C.; Gilbert, E.S.; Dores, G.M.; Schonfeld, S.J.; Lynch, C.F.; Storm, H.; Hall, P.; Langmark, F.; Pukkala, E.; Andersson, M.; et al. Long-Term Solid Cancer Risk Among 5-Year Survivors of Hodgkin’s Lymphoma. J. Clin. Oncol. 2007, 25, 1489–1497. [Google Scholar] [CrossRef] [PubMed]
- Schaapveld, M.; Aleman, B.M.; Van Eggermond, A.M.; Janus, C.P.; Krol, A.D.; Van Der Maazen, R.W.; Roesink, J.; Raemaekers, J.M.; De Boer, J.P.; Zijlstra, J.M.; et al. Second Cancer Risk Up to 40 Years after Treatment for Hodgkin’s Lymphoma. N. Engl. J. Med. 2015, 373, 2499–2511. [Google Scholar] [CrossRef] [PubMed]
- Swerdlow, A.J.; Higgins, C.D.; Smith, P.; Cunningham, D.; Hancock, B.W.; Horwich, A.; Hoskin, P.J.; Lister, T.A.; Radford, J.A.; Rohatiner, A.Z.S.; et al. Second Cancer Risk After Chemotherapy for Hodgkin’s Lymphoma: A Collaborative British Cohort Study. J. Clin. Oncol. 2011, 29, 4096–4104. [Google Scholar] [CrossRef] [PubMed]
- Nottage, K.; McFarlane, J.; Krasin, M.J.; Li, C.; Srivastava, D.; Robison, L.L.; Hudson, M.M. Secondary Colorectal Carcinoma After Childhood Cancer. J. Clin. Oncol. 2012, 30, 2552–2558. [Google Scholar] [CrossRef]
- Van Eggermond, A.M.; Schaapveld, M.; Janus, C.P.; De Boer, J.P.; Krol, A.D.; Zijlstra, J.M.; Van Der Maazen, R.W.; Kremer, L.C.; Van Leerdam, M.E.; Louwman, M.W.; et al. Infradiaphragmatic irradiation and high procarbazine doses increase colorectal cancer risk in Hodgkin lymphoma survivors. Br. J. Cancer 2017, 117, 306–314. [Google Scholar] [CrossRef]
- Henderson, T.O.; Oeffinger, K.C.; Whitton, J.; Leisenring, W.; Neglia, J.; Meadows, A.; Crotty, C.; Rubin, D.T.; Diller, L.; Inskip, P.; et al. Secondary gastrointestinal cancer in childhood cancer survivors: A cohort study. Ann. Intern. Med. 2012, 156, 757. [Google Scholar] [CrossRef]
- Rigter, L.S.; Spaander, M.C.W.; Aleman, B.M.P.; Bisseling, T.M.; Moons, L.M.; Cats, A.; Lugtenburg, P.J.; Janus, C.P.M.; Petersen, E.J.; Roesink, J.M.; et al. High prevalence of advanced colorectal neoplasia and serrated polyposis syndrome in Hodgkin lymphoma survivors. Cancer 2019, 125, 990–999. [Google Scholar] [CrossRef]
- Roos, V.H.; Mangas-Sanjuan, C.; Rodriguez-Girondo, M.; Prado, L.M.; Steyerberg, E.W.; Bossuyt, P.M.; Dekker, E.; Jover, R.; Van Leerdam, M.E. Effects of Family History on Relative and Absolute Risks for Colorectal Cancer: A Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2019, 17, 2657–2667.e9. [Google Scholar] [CrossRef]
- Atkin, W.; Dadswell, E.; Wooldrage, K.; Kralj-Hans, I.; Von Wagner, C.; Edwards, R.; Yao, G.; Kay, C.; Burling, D.; Faiz, O.; et al. Computed tomographic colonography versus colonoscopy for investigation of patients with symptoms suggestive of colorectal cancer (SIGGAR): A multicentre randomised trial. Lancet 2013, 381, 1194–1202. [Google Scholar] [CrossRef]
- Von Wagner, C.; Ghanouni, A.; Halligan, S.; Smith, S.; Dadswell, E.; Lilford, R.J.; Morton, D.; Atkin, W.; Wardle, J. Patient Acceptability and Psychologic Consequences of CT Colonography Compared with Those of Colonoscopy: Results from a Multicenter Randomized Controlled Trial of Symptomatic Patients. Radiology 2012, 263, 723–731. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, H.-S.; Park, H.J. Adverse events related to colonoscopy: Global trends and future challenges. World J. Gastroenterol. 2019, 25, 190–204. [Google Scholar] [CrossRef]
- Zauber, A.G.; Winawer, S.J.; O’Brien, M.J.; Lansdorp-Vogelaar, I.; Van Ballegooijen, M.; Hankey, B.F.; Shi, W.; Bond, J.H.; Schapiro, M.; Panish, J.F.; et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N. Engl. J. Med. 2012, 366, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Nishihara, R.; Wu, K.; Lochhead, P.; Morikawa, T.; Liao, X.; Qian, Z.R.; Inamura, K.; Kim, S.A.; Kuchiba, A.; Yamauchi, M.; et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N. Engl. J. Med. 2013, 369, 1095–1105. [Google Scholar] [CrossRef] [PubMed]
- Citarda, F.; Tomaselli, G.; Capocaccia, R.; Barcherini, S.; Crespi, M.; The Italian Multicentre Study Group. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut 2001, 48, 812–815. [Google Scholar] [CrossRef] [PubMed]
- Winawer, S.J.; Zauber, A.G.; Ho, M.N.; O’Brien, M.J.; Gottlieb, L.S.; Sternberg, S.S.; Waye, J.D.; Schapiro, M.; Bond, J.H.; Panish, J.F.; et al. Prevention of Colorectal Cancer by Colonoscopic Polypectomy. N. Engl. J. Med. 1993, 329, 1977–1981. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, D.A.; Rex, U.K.; Winawer, S.J.; Giardiello, F.M.; Johnson, D.A.; Levin, T.R. Guidelines for Colonoscopy Surveillance After Screening and Polypectomy: A Consensus Update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterol. 2012, 143, 844–857. [Google Scholar] [CrossRef] [PubMed]
- Quintero, E.; Castells, A.; Bujanda, L.; Cubiella, J.; Salas, D.; Lanas, A.; Andreu, M.; Carballo, F.; Morillas, J.D.; Hernández, C.; et al. Colonoscopy versus Fecal Immunochemical Testing in Colorectal-Cancer Screening. N. Engl. J. Med. 2012, 366, 697–706. [Google Scholar] [CrossRef]
- Kapidzic, A.; Grobbee, E.J.; Hol, L.; Van Roon, A.H.; Van Vuuren, A.J.; Spijker, W.; Izelaar, K.; Van Ballegooijen, M.; Kuipers, E.J.; Van Leerdam, M.E. Attendance and Yield Over Three Rounds of Population-Based Fecal Immunochemical Test Screening. Am. J. Gastroenterol. 2014, 109, 1257–1264. [Google Scholar] [CrossRef]
- Stegeman, I.; Van Doorn, S.; Mundt, M.; Mallant-Hent, R.; Bongers, E.; Elferink, M.; Fockens, P.; Stroobants, A.; Bossuyt, P.; Dekker, E. Participation, yield, and interval carcinomas in three rounds of biennial FIT-based colorectal cancer screening. Cancer Epidemiol. 2015, 39, 388–393. [Google Scholar] [CrossRef]
- van Roon, A.H.; Goede, S.L.; van Ballegooijen, M.; van Vuuren, A.J.; Looman, C.W.; Biermann, K.; Reijerink, J.C.; Mannetje, H.; van der Togt, A.C.; Habbema, J.D.; et al. Random comparison of repeated faecal immunochemical testing at different intervals for population-based colorectal cancer screening. Gut 2013, 62, 409–415. [Google Scholar] [CrossRef]
- Carethers, J.M. Fecal DNA Testing for Colorectal Cancer Screening. Annu. Rev. Med. 2019, 71. [Google Scholar] [CrossRef] [PubMed]
- Zhai, R.L.; Xu, F.; Zhang, P.; Zhang, W.L.; Wang, H.; Wang, J.L.; Cai, K.L.; Long, Y.P.; Lu, X.M.; Tao, K.X.; et al. The Diagnostic Performance of Stool DNA Testing for Colorectal Cancer: A Systematic Review and Meta-Analysis. Medicine 2016, 95, e2129. [Google Scholar] [CrossRef] [PubMed]
- Bosch, L.J.; Carvalho, B.; Fijneman, R.J.; Jimenez, C.R.; Pinedo, H.M.; Van Engeland, M.; Meijer, G.A. Molecular Tests for Colorectal Cancer Screening. Clin. Color. Cancer 2011, 10, 8–23. [Google Scholar] [CrossRef] [PubMed]
- Imperiale, T.F.; Ransohoff, D.F.; Itzkowitz, S.H.; Levin, T.R.; Lavin, P.; Lidgard, G.P.; Ahlquist, D.A.; Berger, B.M. Multitarget stool DNA testing for colorectal-cancer screening. N. Engl. J. Med. 2014, 370, 1287–1297. [Google Scholar] [CrossRef]
- Bradshaw, D.; Gans, C.; Jones, P.; Rizzuto, G.; Steiner, N.; Mitton, W.; Ng, J.; Koester, R.; Hartzman, R.; Hurley, C. Novel HLA-A locus alleles including A*01012, A*0306, A*0308, A*2616, A*2617, A*3009, A*3206, A*3403, A*3602 and A*6604. Tissue Antigens 2002, 59, 325–327. [Google Scholar] [CrossRef]
- CBO. Hereditary Colorectal Cancer, National Guideline. 2015. Available online: https://www.mdl.nl/sites/www.mdl.nl/files/richlijnen/Erfelijke_darmkanker_-_december_2015_def.pdf (accessed on 4 November 2019).
- Katsoula, A.; Paschos, P.; Haidich, A.-B.; Tsapas, A.; Giouleme, O. Diagnostic Accuracy of Fecal Immunochemical Test in Patients at Increased Risk for Colorectal Cancer: A Meta-analysis. JAMA Intern. Med. 2017, 177, 1110–1118. [Google Scholar] [CrossRef]
- Van Leerdam, M.E.; Roos, V.H.; Van Hooft, J.E.; Dekker, E.; Jover, R.; Kaminski, M.F.; Latchford, A.; Neumann, H.; Pellisé, M.; Saurin, J.-C.; et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2019, 51, 877–895. [Google Scholar] [CrossRef]
- Rigter, L.S.; Spaander, M.C.W.; Moons, L.M.; Bisseling, T.M.; Aleman, B.M.P.; De Boer, J.P.; Lugtenburg, P.J.; Janus, C.P.M.; Petersen, E.J.; Roesink, J.M.; et al. Colorectal cancer surveillance in Hodgkin lymphoma survivors at increased risk of therapy-related colorectal cancer: Study design. BMC Cancer 2017, 17, 112. [Google Scholar] [CrossRef]
- Cohen, J.F.; Korevaar, D.A.; Altman, U.G.; Bruns, D.E.; Gatsonis, C.A.; Hooft, L.; Irwig, L.; Levine, D.; Reitsma, J.B.; De Vet, H.C.W.; et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: Explanation and elaboration. BMJ Open 2016, 6, 012799. [Google Scholar] [CrossRef]
- Gies, A.; Bhardwaj, M.; Stock, C.; Schrotz-King, P.; Brenner, H. Quantitative fecal immunochemical tests for colorectal cancer screening. Int. J. Cancer 2018, 143, 234–244. [Google Scholar] [CrossRef]
- Toes-Zoutendijk, E.; van Leerdam, M.E.; Dekker, E.; van Hees, F.; Penning, C.; Nagtegaal, I.; van der Meulen, M.P.; van Vuuren, A.J.; Kuipers, E.J.; Bonfrer, J.M.G.; et al. Real-Time Monitoring of Results During First Year of Dutch Colorectal Cancer Screening Program and Optimization by Altering Fecal Immunochemical Test Cut-Off Levels. Gastroenterology 2017, 152, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Wilschut, J.A.; Hol, L.; Dekker, E.; Jansen, J.B.; Van Leerdam, M.E.; Lansdorp-Vogelaar, I.; Kuipers, E.J.; Habbema, J.D.F.; Van Ballegooijen, M. Cost-effectiveness Analysis of a Quantitative Immunochemical Test for Colorectal Cancer Screening. Gastroenterology 2011, 141, 1648–1655. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.-C.; Shun, C.-T.; Hsu, W.-F.; Tu, C.-H.; Tsai, P.-Y.; Lin, B.-R.; Liang, J.-T.; Wu, M.-S.; Chiu, H.-M. Fecal Immunochemical Test Detects Sessile Serrated Adenomas and Polyps With a Low Level of Sensitivity. Clin. Gastroenterol. Hepatol. 2017, 15, 872–879. [Google Scholar] [CrossRef]
- Zorzi, M.; Senore, C.; Da Re, F.; Barca, A.; Bonelli, L.A.; Cannizzaro, R.; De Pretis, G.; Di Furia, L.; Di Giulio, E.; Mantellini, P.; et al. Detection rate and predictive factors of sessile serrated polyps in an organised colorectal cancer screening programme with immunochemical faecal occult blood test: The EQuIPE study (Evaluating Quality Indicators of the Performance of Endoscopy). Gut 2016, 66, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Cock, C.; Anwar, S.; Byrne, S.E.; Meng, R.; Pedersen, S.; Fraser, R.J.L.; Young, G.P.; Symonds, E.L. Low Sensitivity of Fecal Immunochemical Tests and Blood-Based Markers of DNA Hypermethylation for Detection of Sessile Serrated Adenomas/Polyps. Dig. Dis. Sci. 2019, 64, 2555–2562. [Google Scholar] [CrossRef] [PubMed]
- Van Lanschot, M.C.J.; Carvalho, B.; Coupé, V.M.H.; Van Engeland, M.; Dekker, E.; Meijer, G.A. Molecular stool testing as an alternative for surveillance colonoscopy: A cross-sectional cohort study. BMC Cancer 2017, 17, 116. [Google Scholar] [CrossRef]
- Naber, S.K.; Knudsen, A.B.; Zauber, A.G.; Rutter, C.M.; Fischer, S.E.; Pabiniak, C.J.; Soto, B.; Kuntz, K.M.; Lansdorp-Vogelaar, I. Cost-effectiveness of a multitarget stool DNA test for colorectal cancer screening of Medicare beneficiaries. PLoS ONE 2019, 14, e0220234. [Google Scholar] [CrossRef]
- Heigh, R.I.; Yab, T.C.; Taylor, W.R.; Hussain, F.T.N.; Smyrk, T.C.; Mahoney, U.W.; Domanico, M.J.; Berger, B.M.; Lidgard, G.P.; Ahlquist, D.A. Detection of Colorectal Serrated Polyps by Stool DNA Testing: Comparison with Fecal Immunochemical Testing for Occult Blood (FIT). PLoS ONE 2014, 9, e85659. [Google Scholar] [CrossRef]
- De Wijkerslooth, T.R.; Stoop, E.M.; Bossuyt, P.M.; Meijer, G.A.; Van Ballegooijen, M.; Van Roon, A.H.C.; Stegeman, I.; Kraaijenhagen, R.A.; Fockens, P.; Van Leerdam, M.E.; et al. Immunochemical Fecal Occult Blood Testing Is Equally Sensitive for Proximal and Distal Advanced Neoplasia. Am. J. Gastroenterol. 2012, 107, 1570–1578. [Google Scholar] [CrossRef]
- Van Leeuwen, F.E.; Ng, A.K. Late sequelae in Hodgkin lymphoma survivors. Hematol. Oncol. 2017, 35, 60–66. [Google Scholar] [CrossRef]
- Brenner, H.; Stock, C.; Hoffmeister, M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: Systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ 2014, 348, g2467. [Google Scholar] [CrossRef] [PubMed]
- Järvinen, H.J.; Aarnio, M.; Mustonen, H.; Aktan-Collan, K.; Aaltonen, L.A.; Peltomäki, P.; De La Chapelle, A.; Mecklin, J. Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 2000, 118, 829–834. [Google Scholar] [CrossRef]
- Cross, A.J.; Wooldrage, K.; Robbins, E.C.; Kralj-Hans, I.; MacRae, E.; Piggott, C.; Stenson, I.; Prendergast, A.; Patel, B.; Pack, K.; et al. Faecal immunochemical tests (FIT) versus colonoscopy for surveillance after screening and polypectomy: A diagnostic accuracy and cost-effectiveness study. Gut 2019, 68, 1642–1652. [Google Scholar] [CrossRef] [PubMed]
- Steele, R.J.; McClements, P.; Watling, C.; Libby, G.; Weller, D.; Brewster, D.H.; Black, R.; Carey, F.A.; Fraser, C.G. Interval cancers in a FOBT-based colorectal cancer population screening programme: Implications for stage, gender and tumour site. Gut 2012, 61, 576–581. [Google Scholar] [CrossRef]
- Van Rijn, J.C.; Reitsma, J.B.; Stoker, J.; Bossuyt, P.M.; Van Deventer, S.J.; Dekker, E. Polyp Miss Rate Determined by Tandem Colonoscopy: A Systematic Review. Am. J. Gastroenterol. 2006, 101, 343–350. [Google Scholar] [CrossRef]
- Lansdorp-Vogelaar, I.; Goede, S.L.; Bosch, L.J.; Melotte, V.; Carvalho, B.; Van Engeland, M.; Meijer, G.A.; De Koning, H.J.; Van Ballegooijen, M. Cost-effectiveness of High-performance Biomarker Tests vs Fecal Immunochemical Test for Noninvasive Colorectal Cancer Screening. Clin. Gastroenterol. Hepatol. 2018, 16, 504–512. [Google Scholar] [CrossRef]
- Gini, A.; Meester, R.G.S.; Keshavarz, H.; Oeffinger, K.C.; Ahmed, S.; Hodgson, D.C.; Lansdorp-Vogelaar, I. Cost-Effectiveness of Colonoscopy-Based Colorectal Cancer Screening in Childhood Cancer Survivors. J. Natl. Cancer Inst. 2019, 111, 1161–1169. [Google Scholar] [CrossRef]
| Characteristic | FIT Participants (n = 73) | Mt-sDNA Participants (n = 82) | FIT and Mt-sDNA Participants (n = 65) |
|---|---|---|---|
| Male gender, n (%) | 44 (60%) | 45 (55%) | 40 (62%) |
| HL treatment category, % | |||
| Abdominal RT + procarbazine Procarbazine Abdominal RT | 25 (34%) 35 (48%) 13 (18%) | 29 (36%) 38 (46%) 15 (18%) | 24 (37%) 28 (43%) 13 (20%) |
| Time between HL treatment and colonoscopy, median (range), y | 23 (12–40) | 23 (12–40) | 23 (12–40) |
| Age at colonoscopy, median (range), y | 51 (32–73) | 51 (32–73) | 50 (32–73) |
| Neoplastic lesions in cohorts | |||
| No. per patient, median (range) | 2 (0–21) | 2 (0–28) | 2 (0–21) |
| No. per patient, % | |||
| 0 ≥1 | 21 (29%) 52 (71%) | 26 (32%) 56 (68%) | 21 (32%) 44 (68%) |
| Neoplasia detection per patient, % | |||
| Adenomas | |||
| ≥1 adenoma ≥1 advanced adenoma | 43 (59%) 13 (18%) | 44 (54%) 13 (16%) | 36 (55%) 12 (19%) |
| Serrated polyps | |||
| ≥1 serrated polyps ≥1 advanced serrated lesion Advanced neoplasia | 32 (44%) 7 (10%) 19 (26%) | 35 (43%) 10 (12%) 22 (27%) | 26 (40%) 7 (11%) 18 (28%) |
| Number of Events/Total | Sensitivity | Specificity | PPV | NPV | LR+ | LR− | |
|---|---|---|---|---|---|---|---|
| (%, 95% CI) | (%, 95% CI) | (%, 95% CI) | (%, 95% CI) | (95% CI) | (95% CI) | ||
| FIT10 | |||||||
| Any polyp | 52/73 | 17 (8–30) | 86 (64–97) | 75 (47–91) | 30 (25–34) | 1.21 (0.36–4.04) | 0.96 (0.78–1.20) |
| AA | 13/73 | 31 (9–61) | 87 (75–94) | 33 (15–59) | 85 (80–89) | 2.31 (0.82–6.53) | 0.80 (0.55–1.16) |
| ASL | 7/73 | 43 (10–82) | 86 (76–94) | 25 (10–49) | 93 (88–96) | 3.14 (1.10–8.97) | 0.66 (0.35–1.27) |
| AN | 19/73 | 37 (16–62) | 91 (80–97) | 58 (34–80) | 80 (74–85) | 3.98 (1.43–11.05) | 0.70 (0.49–0.99) |
| FIT15 | |||||||
| Any polyp | 52/73 | 14 (6–26) | 86 (64–97) | 70 (40–89) | 29 (25–33) | 0.94 (0.27–3.30) | 1.01 (0.82–1.24) |
| AA | 13/73 | 31 (9–61) | 90 (70–96) | 40 (18–67) | 86 (81–90) | 3.08 (1.01–9.37) | 0.77 (0.53–1.12) |
| ASL | 7/73 | 29 (4–71) | 88 (78–95) | 20 (6–49) | 92 (88–95) | 2.36 (0.62–9.00) | 0.81 (0.50–1.31) |
| AN | 19/73 | 32 (13–57) | 93 (82–98) | 60 (32–83) | 79 (74–84) | 4.26 (1.35–13.49) | 0.74 (0.54–1.01) |
| FIT20 | |||||||
| Any polyp | 52/73 | 12 (4–23) | 91 (70–99) | 75 (40–93) | 29 (26–33) | 1.21 (0.27–5.53) | 0.98 (0.82–1.16) |
| AA | 13/73 | 23 (5–54) | 92 (82–97) | 38 (14–69) | 85 (81–88) | 2.77 (0.75–10.16) | 0.84 (0.62–1.14) |
| ASL | 7/73 | 29 (4–71) | 91 (81–97) | 25 (8–57) | 92 (88–95) | 3.14 (0.78–12.72) | 0.79 (0.49–1.26) |
| AN | 19/73 | 26 (9–51) | 94 (85–99) | 63 (31–86) | 79 (73–83) | 4.74 (1.25–17.95) | 0.78 (0.59–1.03) |
| Number of Events/Total | Sensitivity | Specificity | PPV | NPV | LR+ | LR− | |
|---|---|---|---|---|---|---|---|
| (%, 95% CI) | (%, 95% CI) | (%, 95% CI) | (%, 95% CI) | (95% CI) | (95% CI) | ||
| Mt-sDNA | |||||||
| Any polyp | 56/82 | 50 (36–67) | 81 (61–93) | 85 (71–93) | 43 (35–51) | 2.60 (1.13–5.96) | 0.62 (0.45–0.85) |
| AA | 13/82 | 54 (25–81) | 62 (50–74) | 21 (13–33) | 88 (79–93) | 1.43 (0.79–2.57) | 0.74 (0.40–1.37) |
| ASL | 10/82 | 90 (56–98) | 67 (55–67) | 27 (20–36) | 98 (88–100) | 2.70 (1.83–3.97) | 0.15 (0.02–0.97) |
| AN | 22/82 | 68 (45–86) | 70 (57–81) | 46 (34–57) | 86 (76–92) | 2.27 (1.41–3.67) | 0.45 (0.24–0.86) |
| Number of Events/ Total | Sensitivity (%, 95% CI) | Specificity (%, 95% CI) | PPV (%, 95% CI) | NPV (%, 95% CI) | LR+ (95% CI) | LR− (95% CI) | |
|---|---|---|---|---|---|---|---|
| Combined stool test | |||||||
| Any polyp | 24/65 | 50 (35–65) | 66 (43–85) | 76 (62–86) | 39 (29–49) | 1.50 (0.77–2.94) | 0.75 (0.49–1.14) |
| AA | 12/65 | 50 (21–79) | 57 (42–70) | 21 (12–33) | 83 (73–90) | 1.15 (0.61–2.19) | 0.88 (0.48–1.63) |
| ASL | 7/65 | 100 (59–100) | 62 (48–75) | 24 (19–31) | 100 * | 2.64 (1.90–3.66) | 0 |
| AN | 18/65 | 67 (41–87) | 64 (49–77) | 41 (30–54) | 83 (72–91) | 1.84 (1.12–3.04) | 0.52 (0.26–1.04) |
| Sensitivity (%, 95% CI) | Specificity (%, 95% CI) | |
|---|---|---|
| Proximal neoplasia * | ||
| FIT10 | 13 (4–31) | 77 (55–92) |
| Mt-sDNA | 56 (38–74) | 58 (37–78) |
| FIT10 and mt-sDNA | 54 (33–73) | 56 (31–78) |
| Distal neoplasia * | ||
| FIT10 | 23 (8–45) | 87 (69–96) |
| Mt-sDNA | 42 (22–63) | 44 (26–62) |
| FIT10 and mt-sDNA | 44 (22–69) | 46 (27–67) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ykema, B.; Rigter, L.; Spaander, M.; Moons, L.; Bisseling, T.; Aleman, B.; de Boer, J.P.; Lugtenburg, P.; Janus, C.; Petersen, E.; et al. Diagnostic Accuracy of Stool Tests for Colorectal Cancer Surveillance in Hodgkin Lymphoma Survivors. J. Clin. Med. 2020, 9, 190. https://doi.org/10.3390/jcm9010190
Ykema B, Rigter L, Spaander M, Moons L, Bisseling T, Aleman B, de Boer JP, Lugtenburg P, Janus C, Petersen E, et al. Diagnostic Accuracy of Stool Tests for Colorectal Cancer Surveillance in Hodgkin Lymphoma Survivors. Journal of Clinical Medicine. 2020; 9(1):190. https://doi.org/10.3390/jcm9010190
Chicago/Turabian StyleYkema, Berbel, Lisanne Rigter, Manon Spaander, Leon Moons, Tanya Bisseling, Berthe Aleman, Jan Paul de Boer, Pieternella Lugtenburg, Cecile Janus, Eefke Petersen, and et al. 2020. "Diagnostic Accuracy of Stool Tests for Colorectal Cancer Surveillance in Hodgkin Lymphoma Survivors" Journal of Clinical Medicine 9, no. 1: 190. https://doi.org/10.3390/jcm9010190
APA StyleYkema, B., Rigter, L., Spaander, M., Moons, L., Bisseling, T., Aleman, B., de Boer, J. P., Lugtenburg, P., Janus, C., Petersen, E., Roesink, J., Raemaekers, J., van der Maazen, R., Lansdorp-Vogelaar, I., Gini, A., Verbeek, W., Lemmens, M., Meijer, G., van Leeuwen, F., ... van Leerdam, M. (2020). Diagnostic Accuracy of Stool Tests for Colorectal Cancer Surveillance in Hodgkin Lymphoma Survivors. Journal of Clinical Medicine, 9(1), 190. https://doi.org/10.3390/jcm9010190





