Enhanced Nitric Oxide (NO) and Decreased ADMA Synthesis in Pediatric ADHD and Selective Potentiation of NO Synthesis by Methylphenidate
Abstract
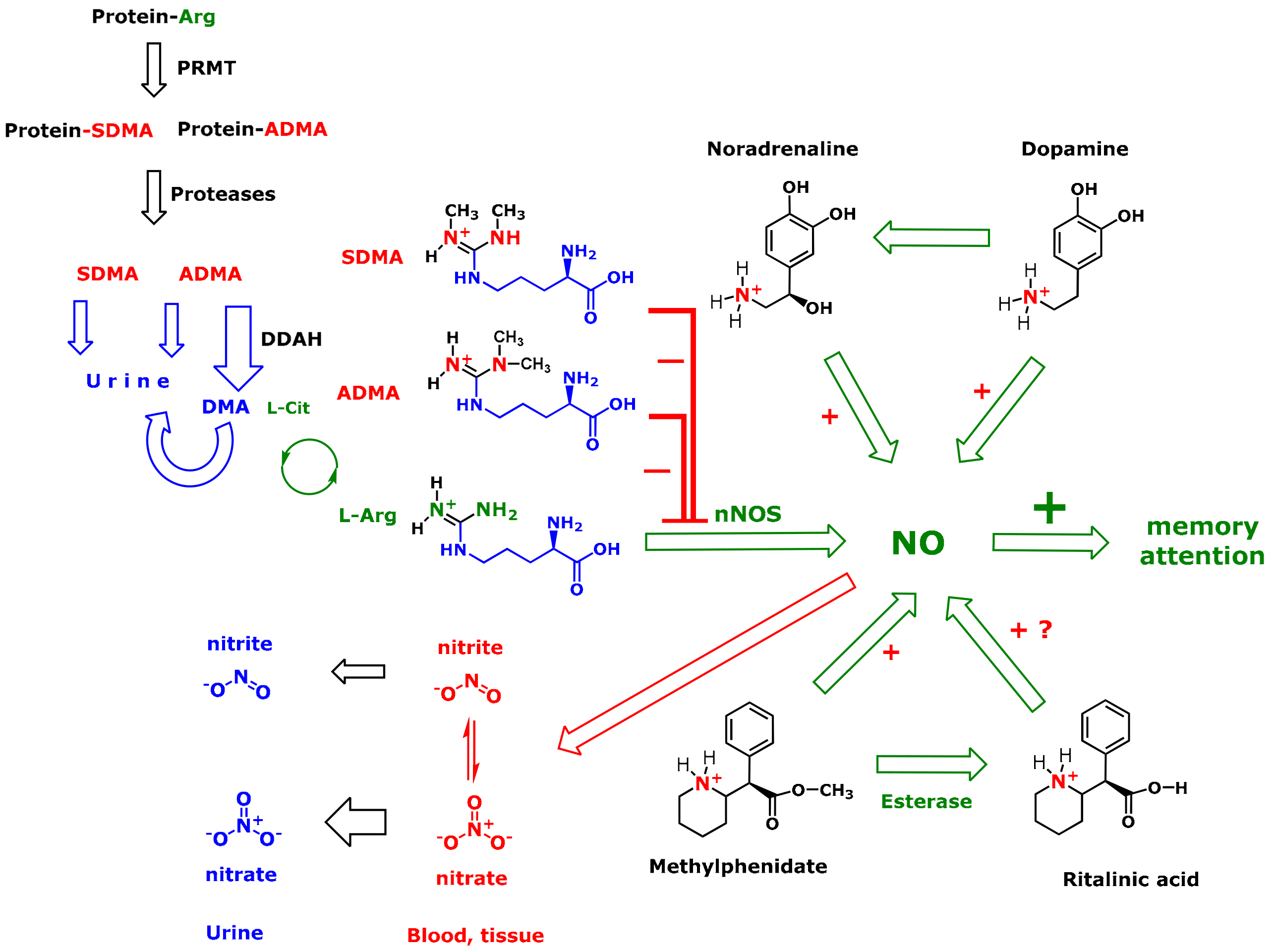
1. Introduction
2. Methods
2.1. Subjects
2.2. Sampling and Biochemical Analyses
2.3. Statistical Analyses
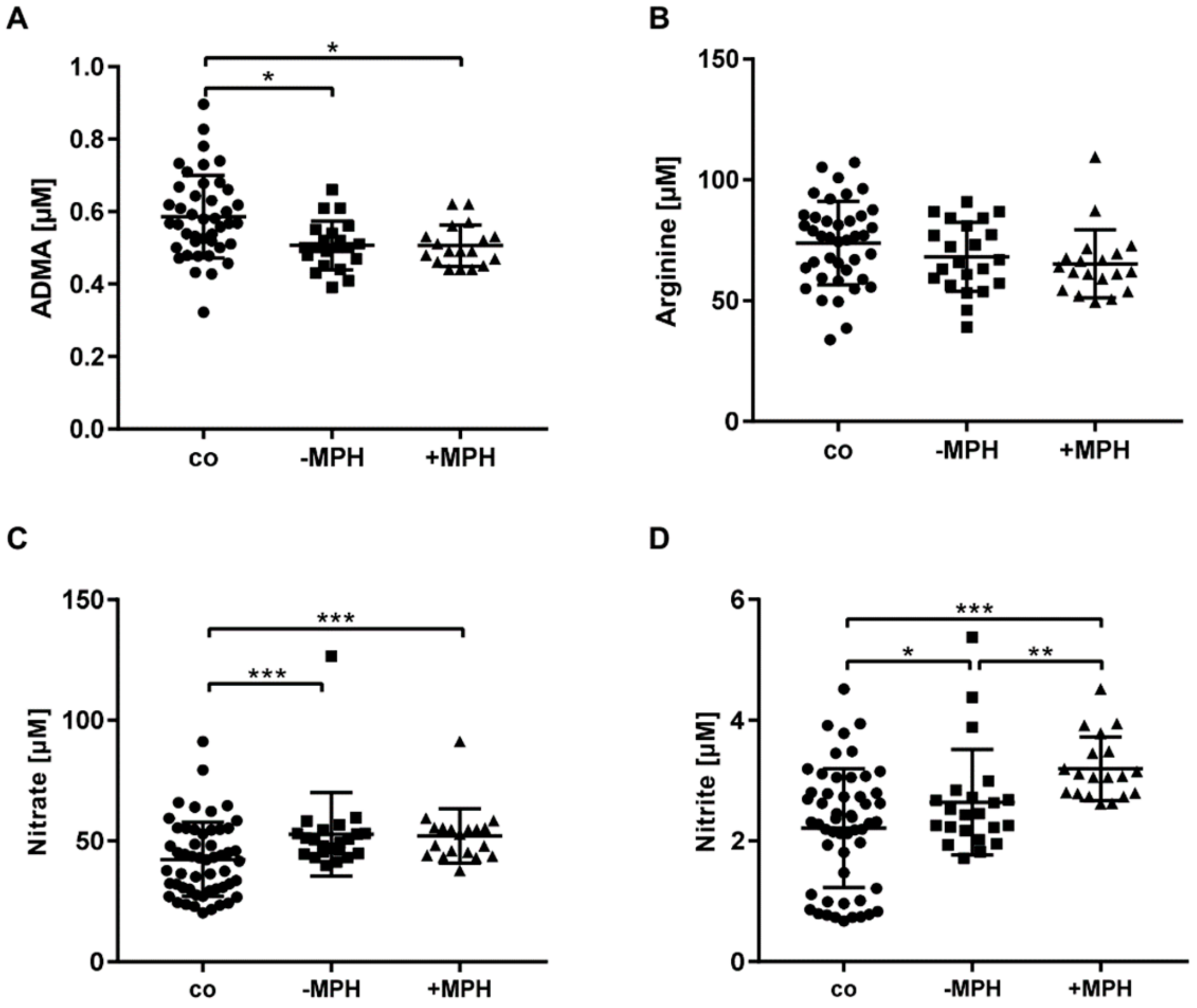
3. Results
4. Discussion
4.1. NO Synthesis is Elevated in Pediatric ADHD
4.2. ADMA Synthesis is Decreased and nNOS Inhibition by ADMA is Attenuated in Pediatric ADHD
4.3. Potential Effects of MPH on NO and ADMA Synthesis in Pediatric ADHD
4.4. Potential Effects of MPH and ADMA on Systemic Growth in ADHD
4.5. Blood Pressure in Pediatric ADHD and Potential Effects of MPH
4.6. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
References
- Sayal, K.; Prasad, V.; Daley, D.; Ford, T.; Coghill, D. ADHD in children and young people: Prevalence, care pathways, and service provision. Lancet Psychiatry 2018, 5, 175–186. [Google Scholar] [CrossRef]
- Agnew-Blais, J.C.; Polanczyk, G.V.; Danese, A.; Wertz, J.; Moffitt, T.E.; Arseneault, L. Evaluation of the persistence, remission, and emergence of Attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry 2016, 73, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Sibley, M.H.; Mitchell, J.T.; Becker, S.P. Method of adult diagnosis influences estimated persistence of childhood ADHD: A systematic review of longitudinal studies. Lancet Psychiatry 2016, 3, 1157–1165. [Google Scholar] [CrossRef]
- Prince, J. Catecholamine dysfunction in attention-deficit/hyperactivity disorder an update. J. Clin. Psychopharmacol. 2008, 28, 39–45. [Google Scholar] [CrossRef]
- Loureiro-Vieira, S.; Costa, V.M.; de Lourdes Bastos, M.; Carvalho, F.; Capela, J.P. Methylphenidate effects in the young brain: Friend or foe? Int. J. Dev. Neurosci. 2017, 60, 34–47. [Google Scholar] [CrossRef]
- Mick, E.; McManus, D.D.; Goldberg, R.J. Meta-analysis of increased heart rate and blood pressure associated with CNS stimulant treatment of ADHD in adults. Eur. Neuropsychopharmacol. 2013, 23, 534–541. [Google Scholar] [CrossRef]
- Zetterqvist, J.; Asherson, P.; Halldner, L.; Långström, N.; Larsson, H. Stimulant and non-stimulant attention deficit/hyperactivity disorder drug use: Total population study of trends and discontinuation patterns 2006–2009. Acta Psychiatr. Scand. 2013, 128, 70–77. [Google Scholar] [CrossRef]
- McCarthy, S.; Wilton, L.; Murray, M.L.; Hodgkins, P.; Asherson, P.; Wong, I.C.K. The epidemiology of pharmacologically treated attention deficit hyperactivity disorder (ADHD) in children, adolescents and adults in UK primary care. BMC Pediatr. 2012, 12, 78. [Google Scholar] [CrossRef]
- McCarthy, S.; Neubert, A.; Man, K.K.C.; Banaschewski, T.; Buitelaar, J.; Carucci, S.; Coghill, D.; Danckaerts, M.; Falissard, B.; Garas, P.; et al. Effects of long-term methylphenidate use on growth and blood pressure: Results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). BMC Psychiatry 2018, 18, 327. [Google Scholar] [CrossRef]
- Caldwell, R.W.; Goldberg, L.I. An evaluation of the vasodilation produced by mephentermine and certain other sympathomimetic amines. J. Pharmacol. Exp. Ther. 1970, 172, 297–309. [Google Scholar]
- Hennissen, L.; Bakker, M.J.; Banaschewski, T.; Carucci, S.; Coghill, D.; Danckaerts, M.; Dittmann, R.W.; Hollis, C.; Kovshoff, H.; McCarthy, S.; et al. Cardiovascular Effects of Stimulant and Non-Stimulant Medication for Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Trials of Methylphenidate, Amphetamines and Atomoxetine. CNS Drugs 2017, 31, 199–215. [Google Scholar] [CrossRef] [PubMed]
- Liang, E.F.; Lim, S.Z.; Tam, W.W.; Ho, C.S.; Zhang, M.W.; McIntyre, R.S.; Ho, R.C. The effect of methylphenidate and atomoxetine on heart rate and systolic blood pressure in young people and adults with attention-deficit hyperactivity disorder (ADHD): Systematic review, meta-analysis, and meta-regression. Int. J. Environ. Res. Public Health 2018, 15, 1789. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Vodovotz, Y.; Tzeng, E.; Billiar, T.R. Nitric oxide, a protective molecule in the cardiovascular system. Nitric Oxide Biol. Chem. 2013, 35, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Cossenza, M.; Socodato, R.; Portugal, C.C.; Domith, I.C.L.; Gladulich, L.F.H.; Encarnação, T.G.; Calaza, K.C.; Mendonça, H.R.; Campello-Costa, P.; Paes-de-Carvalho, R. Nitric oxide in the nervous system. Biochemical, developmental, and neurobiological aspects. In Vitamins and Hormones; Academic Press Inc.: Cambridge, MA, USA, 2014; Volume 96, pp. 79–125. [Google Scholar]
- Farah, C.; Michel, L.Y.M.; Balligand, J.L. Nitric oxide signalling in cardiovascular health and disease. Nat. Rev. Cardiol. 2018, 15, 292–316. [Google Scholar] [CrossRef]
- Tsikas, D. Circulating and excretory nitrite and nitrate: Their value as measures of nitric oxide synthesis, bioavailability and activity is inherently limited. Nitric Oxide Biol. Chem. 2015, 45, 1–3. [Google Scholar] [CrossRef]
- Lundberg, J.O.; Weitzberg, E.; Gladwin, M.T. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat. Rev. Drug Discov. 2008, 7, 156–167. [Google Scholar] [CrossRef]
- Zhao, Y.; Vanhoutte, P.M.; Leung, S.W.S. Vascular nitric oxide: Beyond eNOS. J. Pharmacol. Sci. 2015, 129, 83–94. [Google Scholar] [CrossRef]
- Tsikas, D.; Böger, R.H.; Sandmann, J.; Bode-Böger, S.M.; Frölich, J.C. Endogenous nitric oxide synthase inhibitors are responsible for the L-arginine paradox. FEBS Lett. 2000, 478, 1–3. [Google Scholar] [CrossRef]
- Cooke, J.P.; Ghebremariam, Y.T. DDAH says NO to ADMA. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 1462–1464. [Google Scholar] [CrossRef]
- Blanc, R.S.; Richard, S. Arginine Methylation: The Coming of Age. Mol. Cell 2017, 65, 8–24. [Google Scholar] [CrossRef]
- Murphy, R.B.; Tommasi, S.; Lewis, B.C.; Mangoni, A.A. Inhibitors of the hydrolytic enzyme dimethylarginine dimethylaminohydrolase (DDAH): Discovery, synthesis and development. Molecules 2016, 21, 615. [Google Scholar] [CrossRef] [PubMed]
- Szuba, A.; Podgórski, M. Asymmetric dimethylarginine (ADMA) a novel cardiovascular risk factor—Evidence from epidemiological and prospective clinical trials. Pharmacol. Rep. 2006, 58, 16–20. [Google Scholar] [PubMed]
- Serg, M.; Kampus, P.; Kals, J.; Zagura, M.; Muda, P.; Tuomainen, T.P.; Zilmer, K.; Salum, E.; Zilmer, M.; Eha, J. Association between asymmetric dimethylarginine and indices of vascular function in patients with essential hypertension. Blood Press. 2011, 20, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Xia, W.; Feng, W.; Guan, M.; Yu, Y.; Li, J.; Qu, X. Increased levels of asymmetric dimethylarginine and C-reactive protein are associated with impaired vascular reactivity in essential hypertension. Clin. Exp. Hypertens. 2010, 32, 43–48. [Google Scholar] [CrossRef]
- Xia, W.; Xu, L.; Xu, W.; Wang, X.; Yao, Y. Asymmetric dimethylarginine is associated with carotid atherosclerosis in patients with essential hypertension. Clin. Exp. Hypertens. 2015, 37, 393–397. [Google Scholar] [CrossRef]
- Goonasekera, C.D.A.; Rees, D.D.; Woolard, P.; Frend, A.; Shah, V.; Dillon, M.J. Nitric oxide synthase inhibitors and hypertension in children and adolescents. J. Hypertens. 1997, 15, 901–909. [Google Scholar] [CrossRef]
- Hanff, E.; Lützow, M.; Kayacelebi, A.A.; Finkel, A.; Maassen, M.; Yanchev, G.R.; Haghikia, A.; Bavendiek, U.; Buck, A.; Lücke, T.; et al. Simultaneous GC-ECNICI-MS measurement of nitrite, nitrate and creatinine in human urine and plasma in clinical settings. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1047, 207–214. [Google Scholar] [CrossRef]
- Hanff, E.; Ruben, S.; Kreuzer, M.; Bollenbach, A.; Kayacelebi, A.A.; Das, A.M.; von Versen-Höynck, F.; von Kaisenberg, C.; Haffner, D.; Ückert, S.; et al. Development and validation of GC–MS methods for the comprehensive analysis of amino acids in plasma and urine and applications to the HELLP syndrome and pediatric kidney transplantation: Evidence of altered methylation, transamidination, and arginase acti. Amino Acids 2019, 51, 529–547. [Google Scholar] [CrossRef]
- Bollenbach, A.; Hanff, E.; Tsikas, D. Investigation of N G-hydroxy-L-arginine interference in the quantitative determination of nitrite and nitrate in human plasma and urine by GC-NICI-MS. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2018, 1100, 174–178. [Google Scholar] [CrossRef]
- Bollenbach, A.; Bakker, S.J.L.; Tsikas, D. GC–MS measurement of biological N G-hydroxy-L-arginine, a stepmotherly investigated endogenous nitric oxide synthase substrate and arginase inhibitor. Amino Acids 2019, 51, 627–640. [Google Scholar] [CrossRef]
- Tsikas, D.; Hanff, E.; Bollenbach, A.; Kruger, R.; Pham, V.V.; Chobanyan-Jürgens, K.; Wedekind, D.; Arndt, T.; Jörns, A.; Berbée, J.F.P.; et al. Results, meta-analysis and a first evaluation of UNOxR, the urinary nitrate-to-nitrite molar ratio, as a measure of nitrite reabsorption in experimental and clinical settings. Amino Acids 2018, 50, 799–821. [Google Scholar] [CrossRef] [PubMed]
- Hermenegildo, C.; Medina, P.; Peiró, M.; Segarra, G.; Vila, J.M.; Ortega, J.; Lluch, S. Plasma concentration of asymmetric dimethylarginine, an endogenous inhibitor of nitric oxide synthase, is elevated in hyperthyroid patients. J. Clin. Endocrinol. Metab. 2002, 87, 5636–5640. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, O.; Cakir, E.; Yaman, H.; Akgul, E.O.; Erturk, K.; Beyhan, Z.; Bilgi, C.; Erbil, M.K. The effects of thyroxine replacement on the levels of serum asymmetric dimethylarginine (ADMA) and other biochemical cardiovascular risk markers in patients with subclinical hypothyroidism. Clin. Endocrinol. 2005, 63, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Schulze, F.; Lenzen, H.; Hanefeld, C.; Bartling, A.; Osterziel, K.J.; Goudeva, L.; Schmidt-Lucke, C.; Kusus, M.; Maas, R.; Schwedhelm, E.; et al. Asymmetric dimethylarginine is an independent risk factor for coronary heart disease: Results from the multicenter Coronary Artery Risk Determination investigating the Influence of ADMA Concentration (CARDIAC) study. Am. Heart J. 2006, 152, e1–e493. [Google Scholar] [CrossRef] [PubMed]
- Selley, M.L. Increased concentrations of homocysteine and asymmetric dimethylarginine and decreased concentrations of nitric oxide in the plasma of patients with Alzheimer’s disease. Neurobiol. Aging 2003, 24, 903–907. [Google Scholar] [CrossRef]
- Böger, R.H.; Bode-Böger, S.M.; Thiele, W.; Junker, W.; Alexander, K.; Frölich, J.C. Biochemical evidence for impaired nitric oxide synthesis in patients with peripheral arterial occlusive disease. Circulation 1997, 95, 2068–2074. [Google Scholar] [CrossRef]
- Lücke, T.; Kanzelmeyer, N.; Kemper, M.J.; Tsikas, D.; Das, A.M. Developmental changes in the L-arginine/nitric oxide pathway from infancy to adulthood: Plasma asymmetric dimethylarginine levels decrease with age. Clin. Chem. Lab. Med. 2007, 45, 1525–1530. [Google Scholar] [CrossRef]
- Tsikas, D. A critical review and discussion of analytical methods in the l-arginine/nitric oxide area of basic and clinical research. Anal. Biochem. 2008, 379, 139–163. [Google Scholar] [CrossRef]
- Schmitz, F.; da Silva Scherer, E.B.; da Cunha, M.J.; da Cunha, A.A.; Lima, D.D.; Delwing, D.; Netto, C.A.; de Souza Wyse, A.T. Chronic methylphenidate administration alters antioxidant defenses and butyrylcholinesterase activity in blood of juvenile rats. Mol. Cell. Biochem. 2012, 361, 281–288. [Google Scholar] [CrossRef]
- Kleinbongard, P.; Dejam, A.; Lauer, T.; Rassaf, T.; Schindler, A.; Picker, O.; Scheeren, T.; Gödecke, A.; Schrader, J.; Schulz, R.; et al. Plasma nitrite reflects constitutive nitric oxide synthase activity in mammals. Free Radic. Biol. Med. 2003, 35, 790–796. [Google Scholar] [CrossRef]
- Niijima-Yaoita, F.; Nagasawa, Y.; Tsuchiya, M.; Arai, Y.; Tadano, T.; Tan-No, K. Effects of methylphenidate on the impairment of spontaneous alternation behavior in mice intermittently deprived of REM sleep. Neurochem. Int. 2016, 100, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Kielstein, A.; Tsikas, D.; Galloway, G.P.; Mendelson, J.E. Asymmetric dimethylarginine (ADMA)-A modulator of nociception in opiate tolerance and addiction? Nitric Oxide Biol. Chem. 2007, 17, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Tsikas, D. Does the Inhibitory Action of Asymmetric Dimethylarginine (ADMA) on the Endothelial Nitric Oxide Synthase Activity Explain Its Importance in the Cardiovascular System? The ADMA Paradox. J. Controv. Biomed. Res. 2017, 3, 16–22. [Google Scholar] [CrossRef][Green Version]
- Clements, K.M.; Devonshire, I.M.; Reynolds, J.N.J.; Overton, P.G. Enhanced visual responses in the superior colliculus in an animal model of attention-deficit hyperactivity disorder and their suppression by d-amphetamine. Neuroscience 2014, 274, 289–298. [Google Scholar] [CrossRef]
- Faraone, S.V. The pharmacology of amphetamine and methylphenidate: Relevance to the neurobiology of attention-deficit/hyperactivity disorder and other psychiatric comorbidities. Neurosci. Biobehav. Rev. 2018, 87, 255–270. [Google Scholar] [CrossRef]
- Salum, C.; Schmidt, F.; Michel, P.P.; Del-Bel, E.; Raisman-Vozari, R. Signaling Mechanisms in the Nitric Oxide Donor- and Amphetamine-Induced Dopamine Release in Mesencephalic Primary Cultured Neurons. Neurotox. Res. 2016, 29, 92–104. [Google Scholar] [CrossRef]
- Volz, T.J.; Bjorklund, N.L.; Schenk, J.O. Methylphenidate analogs with behavioral differences interact differently with arginine residues on the dopamine transporter in rat striatum. Synapse 2005, 57, 175–178. [Google Scholar] [CrossRef]
- Ueda, S.; Kato, S.; Matsuoka, H.; Kimoto, M.; Okuda, S.; Morimatsu, M.; Imaizumi, T. Regulation of cytokine-induced nitric oxide synthesis by asymmetric dimethylarginine: Role of dimethylarginine dimethylaminohydrolase. Circ. Res. 2003, 92, 226–233. [Google Scholar] [CrossRef]
- Verlaet, A.A.J.; Breynaert, A.; Ceulemans, B.; De Bruyne, T.; Fransen, E.; Pieters, L.; Savelkoul, H.F.J.; Hermans, N. Oxidative stress and immune aberrancies in attention-deficit/hyperactivity disorder (ADHD): A case–control comparison. Eur. Child Adolesc. Psychiatry 2019, 28, 719–729. [Google Scholar] [CrossRef]
- Gruber, H.J.; Mayer, C.; Meinitzer, A.; Almer, G.; Horejsi, R.; Möller, R.; Pilz, S.; März, W.; Gasser, R.; Truschnig-Wilders, M.; et al. Asymmetric dimethylarginine (ADMA) is tightly correlated with growth in juveniles without correlations to obesity related disorders. Exp. Clin. Endocrinol. Diabetes 2008, 116, 520–524. [Google Scholar] [CrossRef]
- Langen, J.; Kayacelebi, A.A.; Beckmann, B.; Weigt-Usinger, K.; Carmann, C.; Hörster, I.; Lilienthal, E.; Richter-Unruh, A.; Tsikas, D.; Lücke, T. Homoarginine (hArg) and asymmetric dimethylarginine (ADMA) in short stature children without and with growth hormone deficiency: hArg and ADMA are involved differently in growth in the childhood. Amino Acids 2015, 47, 1875–1883. [Google Scholar] [CrossRef] [PubMed]
- Gross, M.D. Growth of hyperkinetic children taking methylphenidate, dextroamphetamine, or imipramine/desipramine. Pediatrics 1976, 58, 423–431. [Google Scholar] [PubMed]
- Sharma, R.P.; Javaid, J.I.; Pandey, G.N.; Easton, M.; Davis, J.M. Pharmacological effects of methylphenidate on plasma homovanillic acid and growth hormone. Psychiatry Res. 1990, 32, 9–17. [Google Scholar] [CrossRef]
- Faraone, S.V.; Lecendreux, M.; Konofal, E. Growth Dysregulation and ADHD: An Epidemiologic Study of Children in France. J. Atten. Disord. 2012, 16, 572–578. [Google Scholar] [CrossRef]
- Traicu, A.; Grizenko, N.; Fortier, M.-È.; Fageera, W.; Sengupta, S.M.; Joober, R. Acute blood pressure change with methylphenidate is associated with improvement in attention performance in children with ADHD. Prog. Neuropsychopharmacol. Biol. Psychiatry 2020, 96, 109732. [Google Scholar] [CrossRef]
- Hartman, C.A.; Rommelse, N.; van der Klugt, C.L.; Wanders, R.B.K.; Timmerman, M.E. Stress Exposure and the Course of ADHD from Childhood to Young Adulthood: Comorbid Severe Emotion Dysregulation or Mood and Anxiety Problems. J. Clin. Med. 2019, 8, 1824. [Google Scholar] [CrossRef]
- Ferrer-Sueta, G.; Campolo, N.; Trujillo, M.; Bartesaghi, S.; Carballal, S.; Romero, N.; Alvarez, B.; Radi, R. Biochemistry of Peroxynitrite and Protein Tyrosine Nitration. Chem. Rev. 2018, 118, 1338–1408. [Google Scholar] [CrossRef]
- Liaudet, L.; Rosenblatt-Velin, N.; Pacher, P. Role of peroxynitrite in the cardiovascular dysfunction of septic shock. Curr. Vasc. Pharmacol. 2013, 11, 196–207. [Google Scholar]
- Comim, C.M.; Gomes, K.M.; Réus, G.Z.; Petronilho, F.; Ferreira, G.K.; Streck, E.L.; Dal-Pizzol, F.; Quevedo, J. Methylphenidate treatment causes oxidative stress and alters energetic metabolism in an animal model of attention-deficit hyperactivity disorder. Acta Neuropsychiatr. 2014, 26, 96–103. [Google Scholar] [CrossRef]
- Motaghinejad, M.; Motevalian, M.; Shabab, B.; Fatima, S. Effects of acute doses of methylphenidate on inflammation and oxidative stress in isolated hippocampus and cerebral cortex of adult rats. J. Neural Transm. 2017, 124, 121–131. [Google Scholar] [CrossRef]
- Guney, E.; Cetin, F.H.; Alisik, M.; Tunca, H.; Tas Torun, Y.; Iseri, E.; Isik Taner, Y.; Cayci, B.; Erel, O. Attention Deficit Hyperactivity Disorder and oxidative stress: A short term follow up study. Psychiatry Res. 2015, 229, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Förstermann, U. Endothelial NO synthase as a source of NO and superoxide. Eur. J. Clin. Pharmacol. 2006, 62, 5–12. [Google Scholar] [CrossRef]
| −MPH | +MPH | p | |
|---|---|---|---|
| Number (n) | 23 | 19 | - |
| Age (years) | 9.12 ± 2.40 | 9.67 ± 1.83 | 0.43 |
| Female [n (%)] | 5 (21.7%) | 4 (21.1%) | 0.96 |
| Age at diagnosis (years) | 7.93 (7.41–9.20) | 8.67 (7.12–11.2) | 0.57 |
| Stature (cm) | 134 (130–141) | 135 (128–151) | 0.70 |
| Head circumference (cm) | 53.8 ± 1.54 | 52.9 ± 1.13 | 0.047 |
| Weight (kg) | 31.0 (27.0–43.8) | 32.7 (25.7–46.7) | 0.94 |
| BMI (kg/m2) | 16.6 (15.6–21.2) | 17.8 (15.6–20.6) | 0.73 |
| DBP (percentile) | 60.4 ± 23.3 | 62.3 ± 19.6 | 0.77 |
| SBP (percentile) | 59.5 ± 26.6 | 76.8 ± 19.0 | 0.03 |
| MAP (mmHg) | 78.0 ± 7.36 | 80.2 ± 6.69 | 0.33 |
| Heart rate (beats/min) | 79.0 ± 13.8 | 79.6 ± 13.4 | 0.90 |
| Control | −MPH | +MPH | p | |
|---|---|---|---|---|
| ADMA (µM/mM) | 7.3 (5.3–8.9) | 6.2 (5.6–6.9) | 5.6 (5.4–6.9) | 0.07 |
| SDMA (µM/mM) | Not available | 8.1 (6.5–9.6) | 8.0 (7.3–8.9) | 0.88 |
| DMA (µM/mM) | Not available | 45.7 (40.5–59.6) | 43.3 (27.1–68.8) | 0.61 |
| ADMA+DMA+SDMA (µM/mM) | Not available | 60.7 (54.8–76.7) | 60.7 (41.5–81.8) | 0.54 |
| (ADMA+DMA)/SDMA | Not available | 7.3 (5.7–8.2) | 5.2 (4.1–9.9) | 0.32 |
| Arg (µM/mM) | Not available | 3.3 (2.7–3.7) | 2.3 (2.7–3.7) | 0.12 |
| Nitrate (µM/mM) | 117 (86.3–154) | 124 (91.6–150) | 131 (87.9–162) | 0.77 |
| Nitrite (µM/mM) | 0.23 (0.11–0.45) | 0.19 (0.14–0.48) | 0.24 (0.12–0.31) | 0.97 |
| Control | −MPH | +MPH | p | |
|---|---|---|---|---|
| PNOxR | 19.9 (11.9–40.4) | 20.9 (16.0–24.8) | 16.0 (13.0–19.8) | 0.14 |
| UNOxR | 877 ± 357 | 669 ± 372 | 689 ± 368 | 0.35 |
| UNO3/PNO3 | 27.9 (8.5–36.9) | 21.8 (17.8–28.1) | 20.0 (15.5–24.0) | 0.25 |
| UNO2/PNO2 | 1.3 (0.8–1.4) | 0.6 (0.5–0.9) | 0.5 (0.4–0.7) | 0.002 |
| UNOxR/PNOxR | 24.5 (11.6–29.2) | 30.6 (19.0–60.7) | 40.6 (27.5–54.2) | 0.05 |
| FENO3 (%) | Not available | 15.8 ± 4.5 | 14.2 ± 3.5 | 0.22 |
| FENO2 (%) | Not available | 0.6 (0.2–1.2) | 0.4 (0.2–0.6) | 0.26 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jansen, K.; Hanusch, B.; Pross, S.; Hanff, E.; Drabert, K.; Bollenbach, A.; Dugave, I.; Carmann, C.; Siefen, R.G.; Emons, B.; et al. Enhanced Nitric Oxide (NO) and Decreased ADMA Synthesis in Pediatric ADHD and Selective Potentiation of NO Synthesis by Methylphenidate. J. Clin. Med. 2020, 9, 175. https://doi.org/10.3390/jcm9010175
Jansen K, Hanusch B, Pross S, Hanff E, Drabert K, Bollenbach A, Dugave I, Carmann C, Siefen RG, Emons B, et al. Enhanced Nitric Oxide (NO) and Decreased ADMA Synthesis in Pediatric ADHD and Selective Potentiation of NO Synthesis by Methylphenidate. Journal of Clinical Medicine. 2020; 9(1):175. https://doi.org/10.3390/jcm9010175
Chicago/Turabian StyleJansen, Kathrin, Beatrice Hanusch, Saskia Pross, Erik Hanff, Kathrin Drabert, Alexander Bollenbach, Irina Dugave, Christina Carmann, Rainer Georg Siefen, Barbara Emons, and et al. 2020. "Enhanced Nitric Oxide (NO) and Decreased ADMA Synthesis in Pediatric ADHD and Selective Potentiation of NO Synthesis by Methylphenidate" Journal of Clinical Medicine 9, no. 1: 175. https://doi.org/10.3390/jcm9010175
APA StyleJansen, K., Hanusch, B., Pross, S., Hanff, E., Drabert, K., Bollenbach, A., Dugave, I., Carmann, C., Siefen, R. G., Emons, B., Juckel, G., Legenbauer, T., Tsikas, D., & Lücke, T. (2020). Enhanced Nitric Oxide (NO) and Decreased ADMA Synthesis in Pediatric ADHD and Selective Potentiation of NO Synthesis by Methylphenidate. Journal of Clinical Medicine, 9(1), 175. https://doi.org/10.3390/jcm9010175






