Longitudinal Substance Use and Biopsychosocial Outcomes Following Therapeutic Community Treatment for Substance Dependence
Abstract
1. Introduction
2. Method
2.1. Participants
2.2. Procedure
2.3. Therapeutic Community Treatment Program
2.4. Measures
2.5. Data Analytic Procedure
3. Results
3.1. Baseline Descriptive Statistics
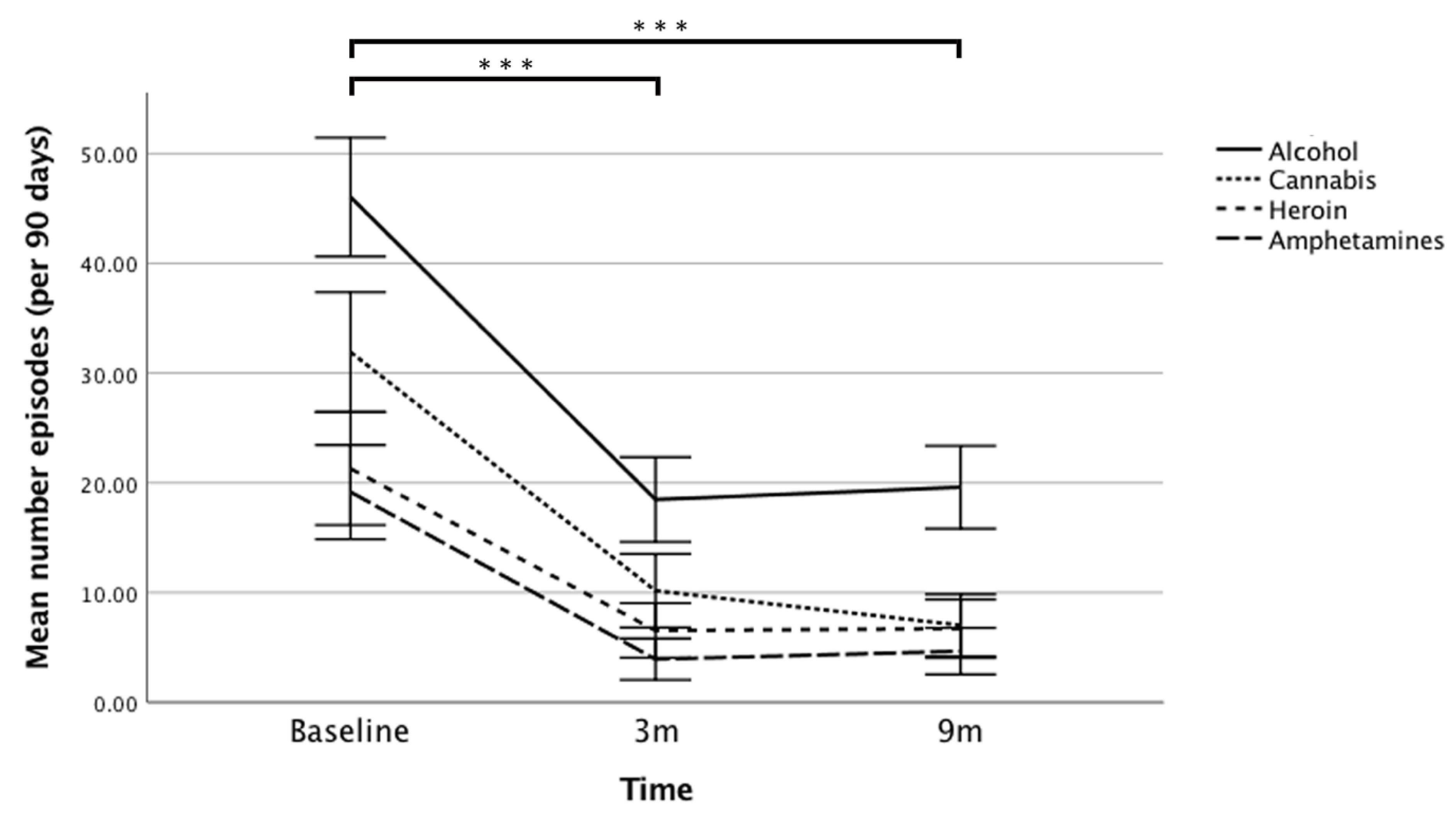
3.2. Primary Drug and Alcohol Outcomes: Use and Dependence
3.3. Secondary Outcomes: Biopsychosocial Variables at 3 Months and 9 Months Follow-Up
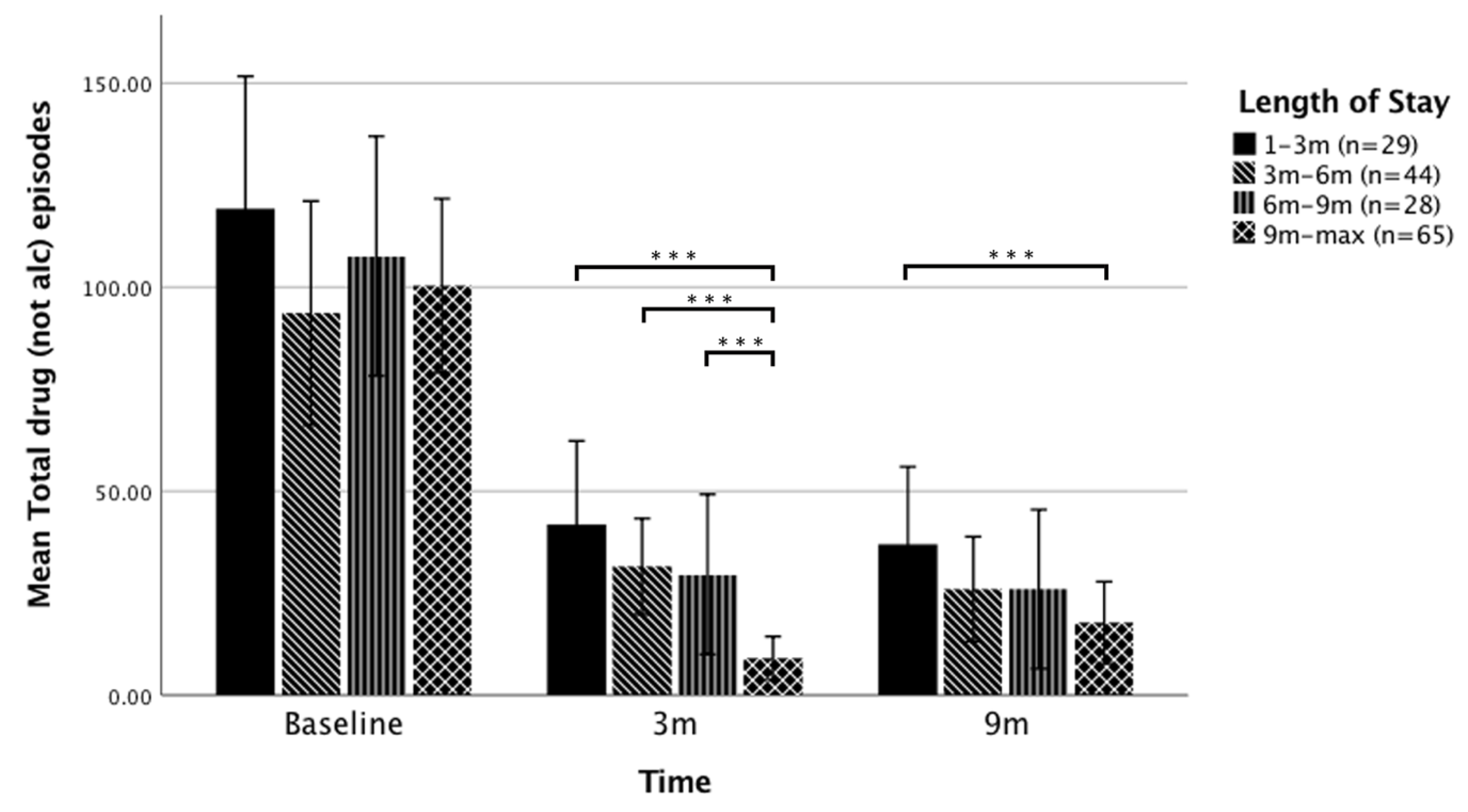
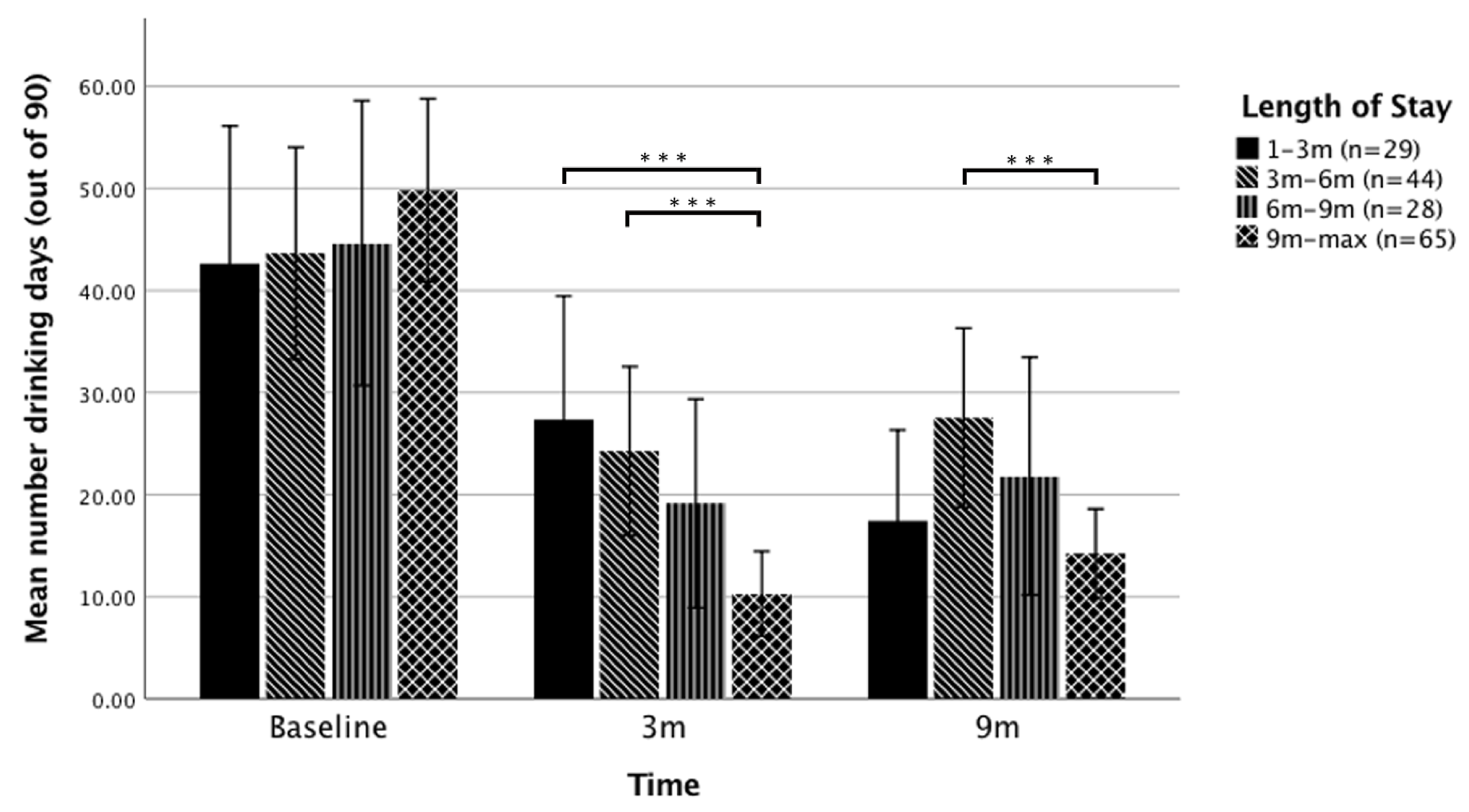
3.4. The Effect of Length of Stay (LOS) on Substance Use Outcomes
4. Discussion
4.1. Study Design Strengths and Limitations
4.2. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- O’Brien, W.B.; Biase, D.V. The therapeutic community: A current perspective. J. Psychoactive Drugs 1984, 16, 9–21. [Google Scholar] [CrossRef]
- De Leon, G. The therapeutic community: Status and evolution. Int. J. Addict. 1985, 20, 823–844. [Google Scholar] [CrossRef]
- De Leon, G. The Therapeutic Community: Theory, Model, and Method; Springer: New York, NY, USA, 2000. [Google Scholar]
- McCusker, J.; Stoddard, A.; Frost, R.; Zorn, M. Planned versus actual duration of drug abuse treatment. Reconciling observational and experimental evidence. J. Nerv. Ment. Dis. 1996, 184, 482–489. [Google Scholar] [CrossRef] [PubMed]
- De Leon, G.; Schwartz, S. Therapeutic communities: What are the retention rates? Am. J. Drug Alcohol Abuse 1984, 10, 267–284. [Google Scholar] [CrossRef] [PubMed]
- De Andrade, D.; Elphinston, R.A.; Quinn, C.; Allan, J.; Hides, L.J.D.; Dependence, A. The effectiveness of residential treatment services for individuals with substance use disorders: A systematic review. Drug Alcohol Depend. 2019, 201, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Harley, M.; Pit, S.W.; Rees, T.; Thomas, S. Completion rates and psychosocial intervention effectiveness in an Australian substance use therapeutic community. Subst. Abuse Treat. Prev. Policy 2018, 13, 33. [Google Scholar] [CrossRef]
- Deane, F.P.; Kelly, P.J.; Crowe, T.P.; Coulson, J.C.; Lyons, G.C. Clinical and reliable change in an Australian residential substance use program using the addiction severity index. J. Addict. Dis. 2013, 32, 194–205. [Google Scholar] [CrossRef]
- Turner, B.; Deane, F.P. Length of stay as a predictor of reliable change in psychological recovery and well being following residential substance abuse treatment. Ther. Communities. 2016, 37, 112–120. [Google Scholar] [CrossRef]
- Malivert, M.; Fatséas, M.; Denis, C.; Langlois, E.; Auriacombe, M. Effectiveness of therapeutic communities: A systematic review. Eur. Addict. Res. 2012, 18, 1–11. [Google Scholar] [CrossRef]
- Magor-Blatch, L.E.; Ingham, L. Youth with mental illness: Attitudes towards and therapeutic benefits of residential stepped care. Community Ment. Health J. 2015, 51, 338–346. [Google Scholar] [CrossRef]
- Smith, L.A.; Gates, S.; Foxcroft, D. Therapeutic communities for substance related disorder. Cochrane Database Syst. Rev. 2006, CD005338. [Google Scholar] [CrossRef] [PubMed]
- Manning, V.; Garfield, J.B.; Best, D.; Berends, L.; Room, R.; Mugavin, J.; Larner, A.; Lam, T.; Buykx, P.; Allsop, S.; et al. Substance use outcomes following treatment: Findings from the Australian Patient Pathways Study. Aust. N. Z. J. Psychiatry 2017, 51, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Condelli, W.S.; Hubbard, R.L. Relationship between time spent in treatment and client outcomes from therapeutic communities. J. Subst. Abuse Treat. 1994, 11, 25–33. [Google Scholar] [CrossRef]
- Greenfield, L.; Burgdorf, K.; Chen, X.; Porowski, A.; Roberts, T.; Herrell, J. Effectiveness of long-term residential substance abuse treatment for women: Findings from three national studies. Am. J. Drug Alcohol Abuse 2004, 30, 537–550. [Google Scholar] [CrossRef] [PubMed]
- Teesson, M.; Mills, K.; Ross, J.; Darke, S.; Williamson, A.; Havard, A. The impact of treatment on 3 years’ outcome for heroin dependence: Findings from the Australian Treatment Outcome Study (ATOS). Addiction 2008, 103, 80–88. [Google Scholar] [CrossRef]
- Cutcliffe, J.; Travale, R.; Richmond, M.M. Green TJIimhn. Considering the contemporary issues and unresolved challenges facing therapeutic communities for clients with alcohol and substance abuse. Issues Ment. Health Nurs. 2016, 37, 642–650. [Google Scholar] [CrossRef]
- Zhang, Z.; Friedmann, P.D.; Gerstein, D.R. Does retention matter? Treatment duration and improvement in drug use. Addiction 2003, 98, 673–684. [Google Scholar] [CrossRef]
- Gossop, M.; Marsden, J.; Stewart, D.; Rolfe, A. Treatment retention and 1 year outcomes for residential programmes in England. Drug Alcohol Depend. 1999, 57, 89–98. [Google Scholar] [CrossRef]
- Bale, R.N.; Van Stone, W.W.; Kuldau, J.M.; Engelsing, T.M.; Elashoff, R.M.; Zarcone, V.P. Therapeutic communities vs methadone maintenance: A prospective controlled study of narcotic addiction treatment: Design and one-year follow-up. Arch. Gen. Psychiatry 1980, 37, 179–193. [Google Scholar] [CrossRef]
- Hubbard, R.L.; Marsden, M.E.; Rachal, J.; Harwood, H.J.; Cavanaugh, E.R.; Ginzburg, H.M. Drug Abuse Treatment: A National Study of Effectiveness; University of North Carolina Press: Chapel Hill, NC, USA, 1989. [Google Scholar]
- Simpson, D.D.; Joe, G.W.; Fletcher, B.W.; Hubbard, R.L.; Anglin, M.D. A national evaluation of treatment outcomes for cocaine dependence. Arch. Gen. Psychiatry 1999, 56, 507–514. [Google Scholar] [CrossRef]
- Patterson, T.; Macleod, E.; Hobbs, L.; Egan, R.; Cameron, C.; Gross, J. Measuring both primary and secondary outcomes when evaluating treatment effectiveness in alcohol and drug treatment programmes. Clin. Psychol. (Aust. Psychol. Soc.) 2019, 23, 152–164. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Staiger, P.K.; Liknaitzky, P.; Lake, A.J.; Manning, M.; Gruenert, S.; Marlatt, G.A. Can a brief skill-based alcohol intervention embedded within a Therapeutic Community Treatment reduce alcohol consumption and relapse in recovering drug dependent individuals? Work in preparation. 2019. [Google Scholar]
- Best, D.; Beckwith, M.; Haslam, C.; Alexander Haslam, S.; Jetten, J.; Mawson, E.; Lubman, D.I. Overcoming alcohol and other drug addiction as a process of social identity transition: The social identity model of recovery (SIMOR). Addict. Res. Theory 2016, 24, 111–123. [Google Scholar] [CrossRef]
- Sobell, L.C.; Sobell, M.B.; Leo, G.I.; Cancilla, A. Reliability of a timeline method: Assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. Br. J. Addict. 1988, 83, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Dawe, S.; Mattick, R.P. Review of Diagnostic Screening Instruments for Alcohol and Other Drug Use and Other Psychiatric Disorders; Australian Government Publishing Service: Canberra, ACT, Australia, 1997.
- Gossop, M.; Darke, S.; Griffiths, P.; Hando, J.; Powis, B.; Hall, W.; Strang, J. The Severity of Dependence Scale (SDS): Psychometric properties of the SDS in English, Australian samples of heroin, cocaine and amphetamine users. Addiction 1995, 90, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Iraurgi Castillo, I.; González Saiz, F.; Lozano Rojas, O.; Landabaso Vázquez, M.A.; Jiménez Lerma, J.M. Estimation of cutoff for the Severity of Dependence Scale (SDS) for opiate dependence by ROC analysis. Actas. Esp. Psiquiatr. 2010, 38, 270–277. [Google Scholar]
- Topp, L.; Mattick, R.P. Choosing a cut-off on the Severity of Dependence Scale (SDS) for amphetamine users. Addiction 1997, 92, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Kaye, S.; Darke, S. Determining a diagnostic cut-off on the Severity of Dependence Scale (SDS) for cocaine dependence. Addiction 2002, 97, 727–731. [Google Scholar] [CrossRef]
- Stockwell, T.; Sitharthan, T.; McGrath, D.; Lang, E. The measurement of alcohol dependence and impaired control in community samples. Addiction 1994, 89, 167–184. [Google Scholar] [CrossRef]
- Stockwell, T.; Murphy, D.; Hodgson, R. The severity of alcohol dependence questionnaire: Its use, reliability and validity. Br. J. Addict. 1983, 78, 145–155. [Google Scholar] [CrossRef]
- Darke, S.; Ward, J.; Hall, W.; Heather, N.; Wodak, A. The Opiate Treatment Index (oti) Manual; Technical Report 11; National Drug and Alcohol Research: Sydney, Australia, 1991. [Google Scholar]
- Adelekan, M.; Green, A.; DasGupta, N.; Tallack, F.; Stimson, G.V.; Wells, B. Reliability and validity of the Opiate Treatment Index among a sample of opioid users in the United Kingdom. Drug Alcohol. Rev. 1996, 15, 261–270. [Google Scholar] [CrossRef]
- Darke, S.; Hall, W.; Wodaki, A.; Heather, N.; Ward, J. Development and validation of a multidimensional instrument for assessing outcome of treatment among opiate users: The Opiate Treatment Index. Br. J. Addict. 1992, 87, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Cummins, R.A.; Eckersley, R.; Pallant, J.; Van Vugt, J.; Misajon, R. Developing a national index of subjective wellbeing: The Australian Unity Wellbeing Index. Soc. Indic. Res. 2003, 64, 159–190. [Google Scholar] [CrossRef]
- Lau, A.L.; Cummins, R.A.; Mcpherson, W. An investigation into the cross-cultural equivalence of the Personal Wellbeing Index. Soc. Indic. Res. 2005, 72, 403–430. [Google Scholar] [CrossRef]
- McLellan, A.T.; Kushner, H.; Metzger, D.; Peters, R.; Smith, I.; Grissom, G.; Pettinati, H.; Argeriou, M. The fifth edition of the Addiction Severity Index. J. Subst. Abuse Treat. 1992, 9, 199–213. [Google Scholar] [CrossRef]
- McLellan, A.T.; Luborsky, L.; Cacciola, J.; Griffith, J.; Evans, F.; Barr, H.L.; O’Brien, C.P. New data from the Addiction Severity Index: Reliability and validity in three centers. J. Nerv. Ment. Dis. 1985, 173, 412–423. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: Hoboken, NJ, USA, 2004. [Google Scholar]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R Stat. Soc. Series B (Methodol.) 1995, 57, 289–300. [Google Scholar] [CrossRef]
- International Wellbeing Group. Personal Wellbeing Index, 5th ed.; Australian Centre on Quality of Life, Deakin University: Geelong, VIC, Australia, 2013. [Google Scholar]
- Tait, R.J. Comparison of subjective wellbeing in substance users and the parents or partners of substance users. Drug Alcohol Rev. 2018, 37, S415–S419. [Google Scholar] [CrossRef]
- Manning, V.; Gomez, B.; Guo, S.; Low, Y.D.; Koh, P.K.; Wong, K.E. An exploration of quality of life and its predictors in patients with addictive disorders: Gambling, alcohol and drugs. Int. J. Ment. Health Addict. 2012, 10, 551–562. [Google Scholar] [CrossRef]
- Dietze, P.; Stoové, M.; Miller, P.; Kinner, S.; Bruno, R.; Alati, R.; Burns, L. The self-reported personal wellbeing of a sample of Australian injecting drug users. Addiction 2010, 105, 2141–2148. [Google Scholar] [CrossRef]
- López-Goñi, J.J.; Fernández-Montalvo, J.; Menéndez, J.C.; Yudego, F.; García, A.R.; Esarte, S. Group and individual change in the treatment of drug addictions: A follow-up study in therapeutic communities. Span. J. Psychol. 2010, 13, 906–913. [Google Scholar] [CrossRef][Green Version]
- Graffam, J.; Shinkfield, A.J.; Lavelle, B. Recidivism among participants of an employment assistance program for prisoners and offenders. Int. J. Offender. Ther. Comp. Criminol. 2014, 58, 348–363. [Google Scholar] [CrossRef] [PubMed]
- McLellan, A.T.; Cacciola, J.C.; Alterman, A.I.; Rikoon, S.H.; Carise, C. The Addiction Severity Index at 25: Origins, contributions and transitions. Am. J. Psychiatry 2006, 15, 113–124. [Google Scholar]
- De Leon, G. Therapeutic communities. In The American Psychiatric Publishing Textbook of Substance Abuse Treatment, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2008. [Google Scholar]
- Pedersen, M.U.; Hesse, M. Residential treatment in Denmark: Client characteristics and Retention. Ther. Communities 2007, 28, 206–217. [Google Scholar]
- Andersson, H.W.; Wenaas, M.; Nordfjærn, T. Relapse after inpatient substance use treatment: A prospective cohort study among users of illicit substances. Addict. Behav. 2019, 90, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Dingle, G.A.; Haslam, C.; Best, D.; Chan, G.; Staiger, P.K.; Savic, M.; Beckwith, M.; Mackenzie, J.; Bathish, R.; Lubman, D.I. Social identity differentiation predicts commitment to sobriety and wellbeing in residents of therapeutic communities. Soc. Sci. Med. 2019, 237, 112459. [Google Scholar] [CrossRef] [PubMed]
| Variable | % (n) |
|---|---|
| Age, Mean (SD) | 33.3 (7.70) |
| Women | 35.5 (59) |
| Single/Separated | 76.5 (127) |
| Born in Australia | 83.7 (139) |
| Highest level of education | |
| Up to High School | 70.4 (117) |
| Certificate/Trade | 22.3 (37) |
| Tertiary | 7.2 (12) |
| Unemployed | 51.8 (86) |
| Government Benefit recipient | 97.0 (161) |
| Place of Residence | |
| Owned house | 9.0 (15) |
| Rental/Social Housing | 73.4 (122) |
| Homeless/No fixed address | 6.6 (11) |
| Primary Drug of Choice | |
| Cannabis | 18.7 (31) |
| Amphetamines | 25.9 (43) |
| Cocaine | 0.6 (1) |
| Sedatives/Tranquilisers | 4.8 (8) |
| Heroin | 31.9 (53) |
| Other opioids/analgesics | 4.80 (8) |
| Alcohol | 18.1 (30) |
| SDS baseline score, Mean (SD) (whole sample) | 9.0 (5.3) |
| SADQ baseline score, Mean (SD) (subsample a) | 34.9 (14.4) |
| Polydrug user b | 97.6 (162) |
| Days in TC at exit, Median (IQR) | 206.5 (104.7–370.0) |
| Variable | Baseline n = 166 | 3 Months Follow-Up n = 157 | 9 Months Follow-Up n = 150 | Effect Size at 9 Months (Cohen’s d) |
|---|---|---|---|---|
| Drug consumption | ||||
| Number drug episodes over 90 days, Mean (SD) | 103.1 (85.2) | 24.2 (40.5) *** | 24.7 (44.5) *** | −0.79 |
| Abstinent from drug use over past 90 days, % (n) | 12.0 (20) b | 49.4% (82) *** | 57.1% (95) *** | 1.54 |
| Proportion sample over 50% reduction in drug frequency, % (n) a | N/A | 77.5% (110) | 81.7% (116) | N/A |
| Alcohol Consumption | ||||
| Number drinking days over 90 days, Mean (SD) | 46.4 (35.3) | 18.5 (25.2) *** | 19.6 (24.7) *** | −0.47 |
| Number Standard Drinks/drinking day, Mean (SD) | 13.6 (11.6) | 7.0 (8.9) *** | 6.4 (8.2) *** | −0.42 |
| Abstinent from alcohol use over past 90 days, % (n) | 10.2 (17) | 31.9% (53) *** | 31.9% (53) *** | 0.86 |
| Proportion sample over 50% reduction in alcohol frequency, % (n) a | N/A | 63.1% (94) | 63.8% (95) | N/A |
| Dependence | ||||
| Substance Dependence Scale, Mean (SD) | 9.0 (5.3) | 4.0 (5.1) *** | 3.2 (4.8) *** | −0.56 |
| Severity of Alcohol Dependence Questionnaire, Mean (SD) | 19.4 (16.8) | 7.5 (9.8) *** | 7.3 (9.5) *** | −0.53 |
| Variable | Baseline M (SD) | 3 Months Follow-Up M (SD) | 9 Months Follow-Up M (SD) | Effect Size at 9 Months (d) |
|---|---|---|---|---|
| Wellbeing b,^ | 25.18 (18.09) | 53.28 (23.45) *** | 58.86 (24.70) *** | 0.47 |
| Social Function a,# | 19.99 (7.73) | 14.98 (7.77) *** | 13.22 (7.18) *** | −0.23 |
| Psychiatric Status c,# | 0.57 (0.22) | 0.38 (0.24) *** | 0.32 (0.24) *** | −0.32 |
| Employment Status c,# | 0.68 (0.29) | 0.59 (0.29) ** | 0.55 (0.31) *** | −0.19 |
| Medical Status c,# | 0.18 (0.30) | 0.14 (0.27) | 0.17 (0.30) | −0.03 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Staiger, P.K.; Liknaitzky, P.; Lake, A.J.; Gruenert, S. Longitudinal Substance Use and Biopsychosocial Outcomes Following Therapeutic Community Treatment for Substance Dependence. J. Clin. Med. 2020, 9, 118. https://doi.org/10.3390/jcm9010118
Staiger PK, Liknaitzky P, Lake AJ, Gruenert S. Longitudinal Substance Use and Biopsychosocial Outcomes Following Therapeutic Community Treatment for Substance Dependence. Journal of Clinical Medicine. 2020; 9(1):118. https://doi.org/10.3390/jcm9010118
Chicago/Turabian StyleStaiger, Petra K., Paul Liknaitzky, Amelia J. Lake, and Stefan Gruenert. 2020. "Longitudinal Substance Use and Biopsychosocial Outcomes Following Therapeutic Community Treatment for Substance Dependence" Journal of Clinical Medicine 9, no. 1: 118. https://doi.org/10.3390/jcm9010118
APA StyleStaiger, P. K., Liknaitzky, P., Lake, A. J., & Gruenert, S. (2020). Longitudinal Substance Use and Biopsychosocial Outcomes Following Therapeutic Community Treatment for Substance Dependence. Journal of Clinical Medicine, 9(1), 118. https://doi.org/10.3390/jcm9010118





