Subclinical Atherosclerosis Imaging in People Living with HIV
Abstract
1. Introduction
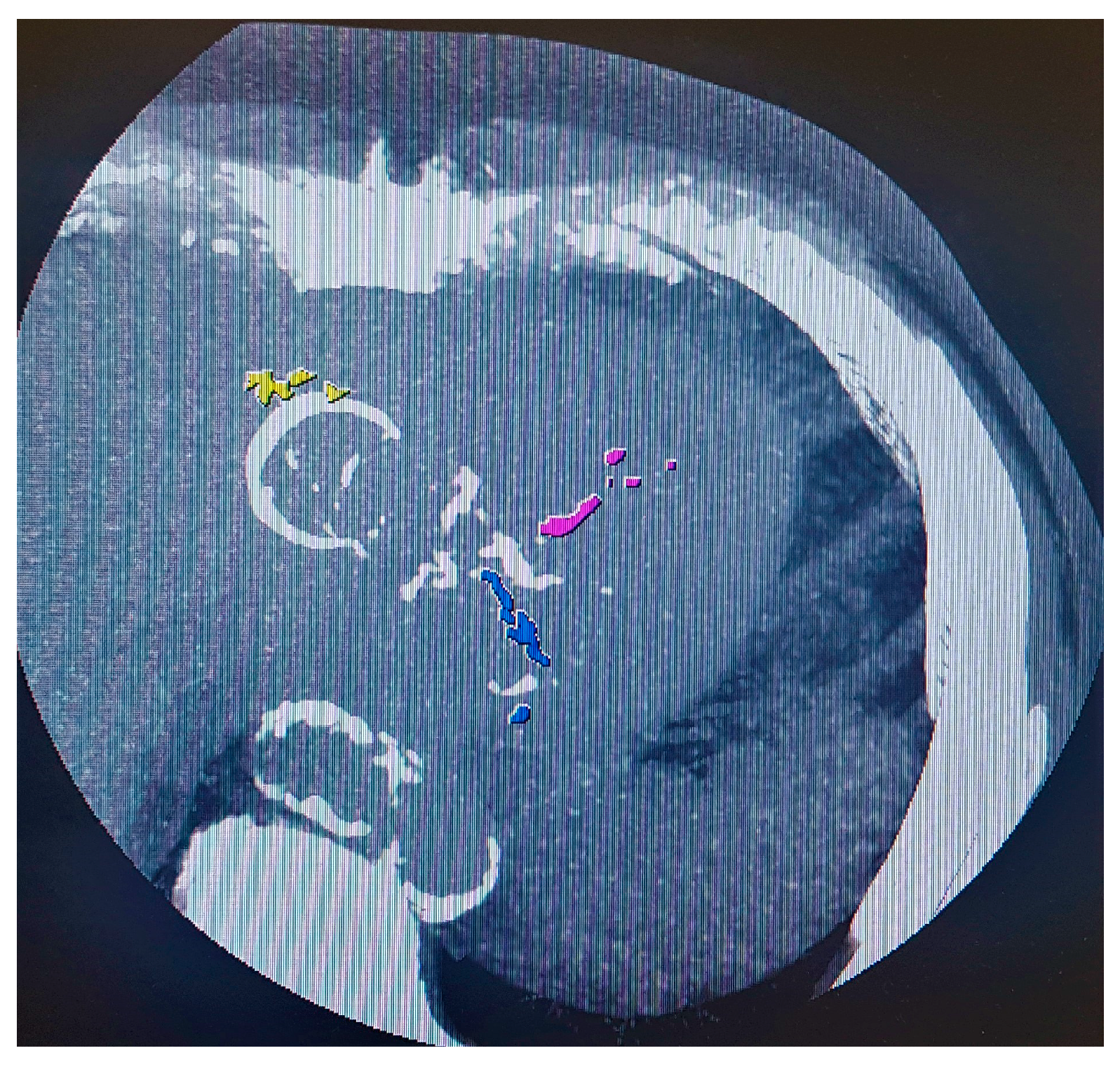
2. Carotid Artery Intima-Media Thickness (CIMT)
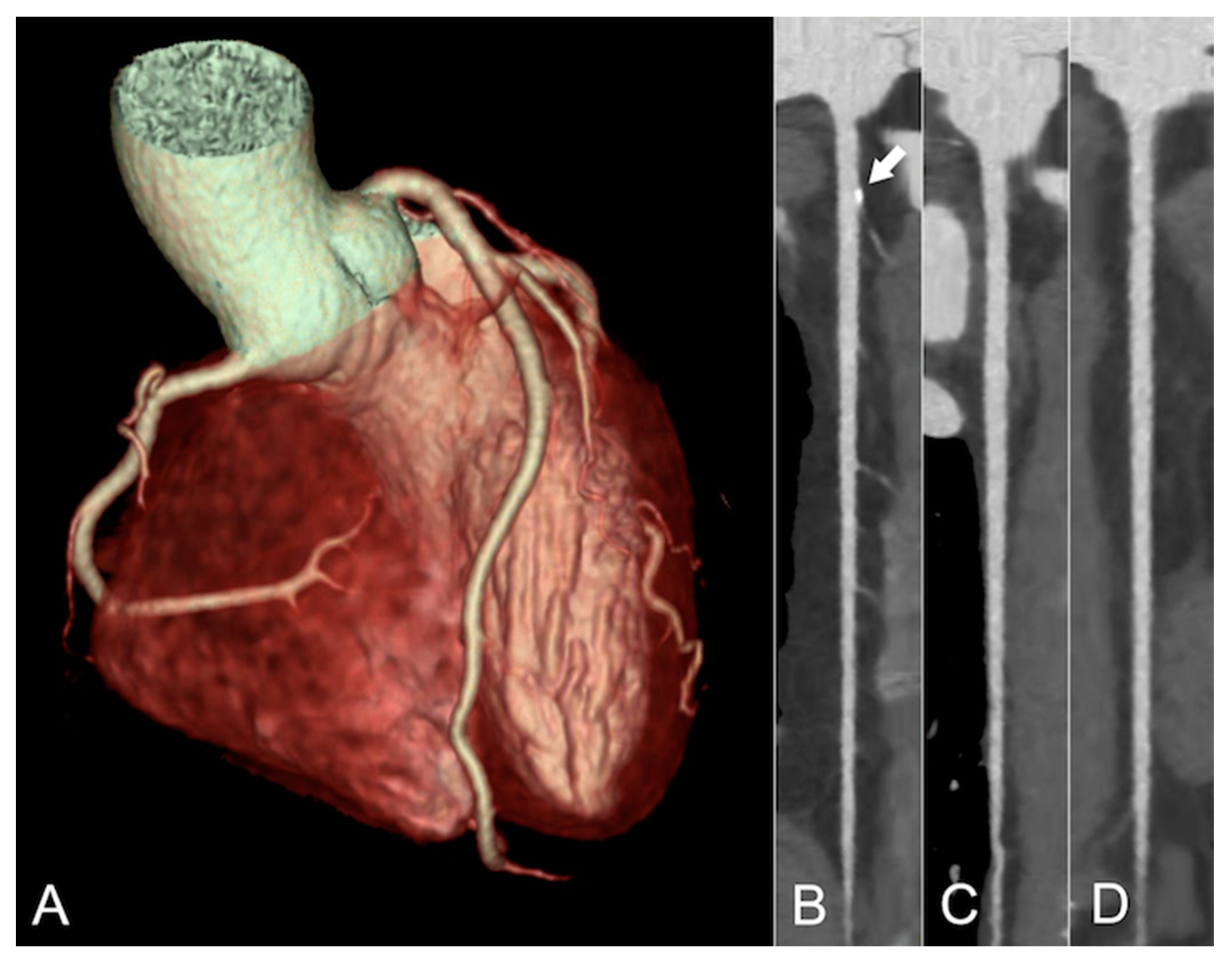
3. Coronary Artery Calcium (CAC) Scoring
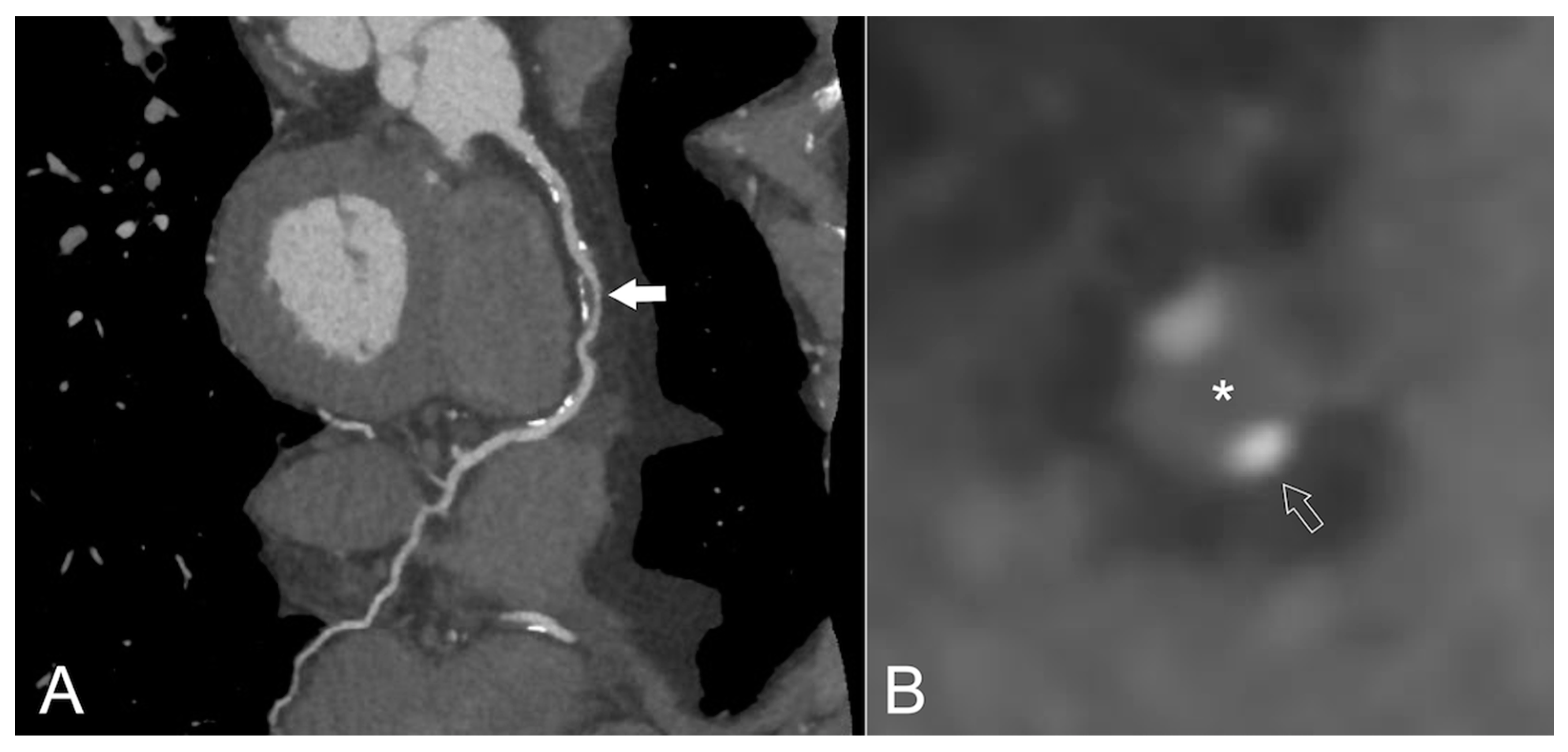
4. Coronary CT Angiography (CCTA)
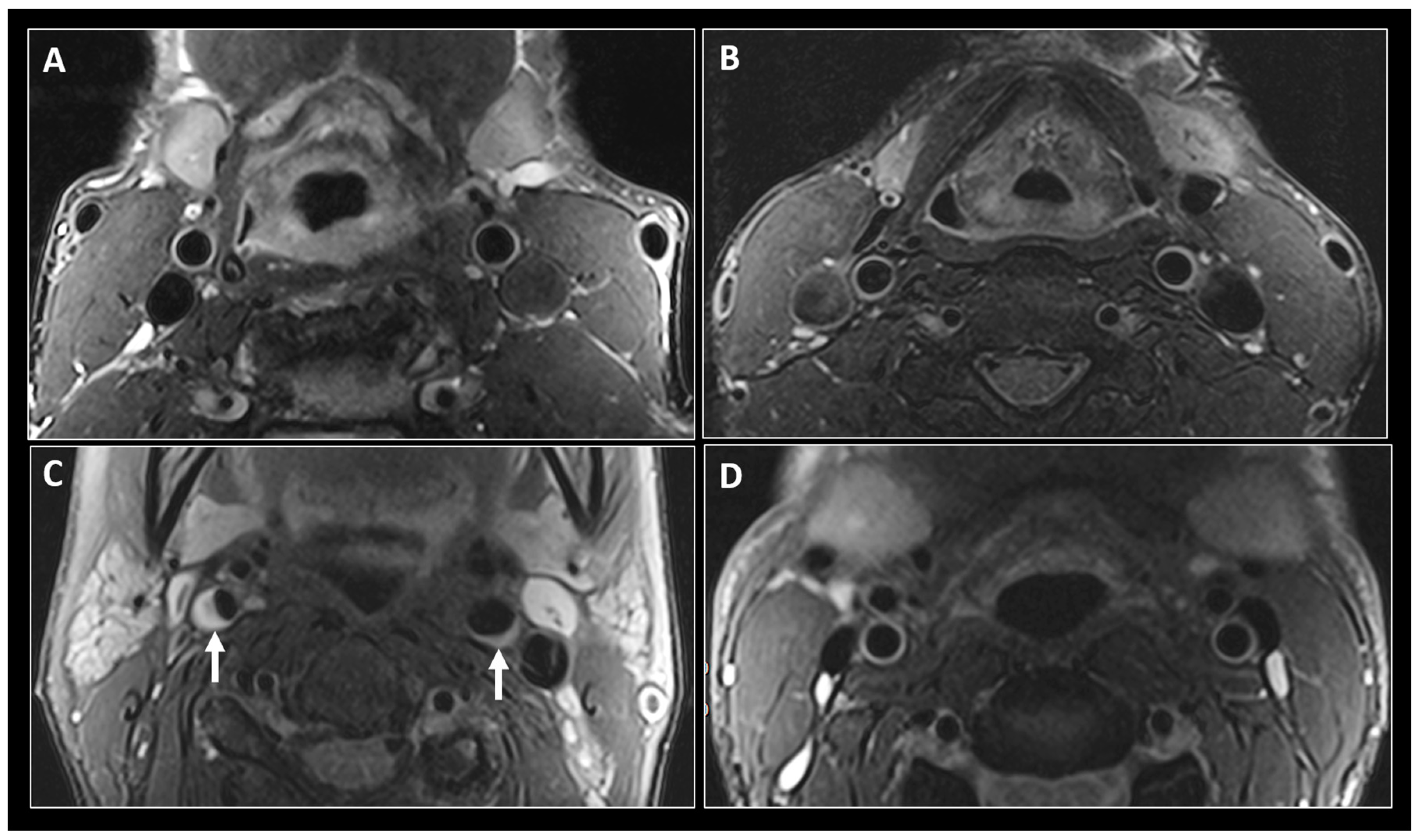
5. Magnetic Resonance Rmaging (MRI)
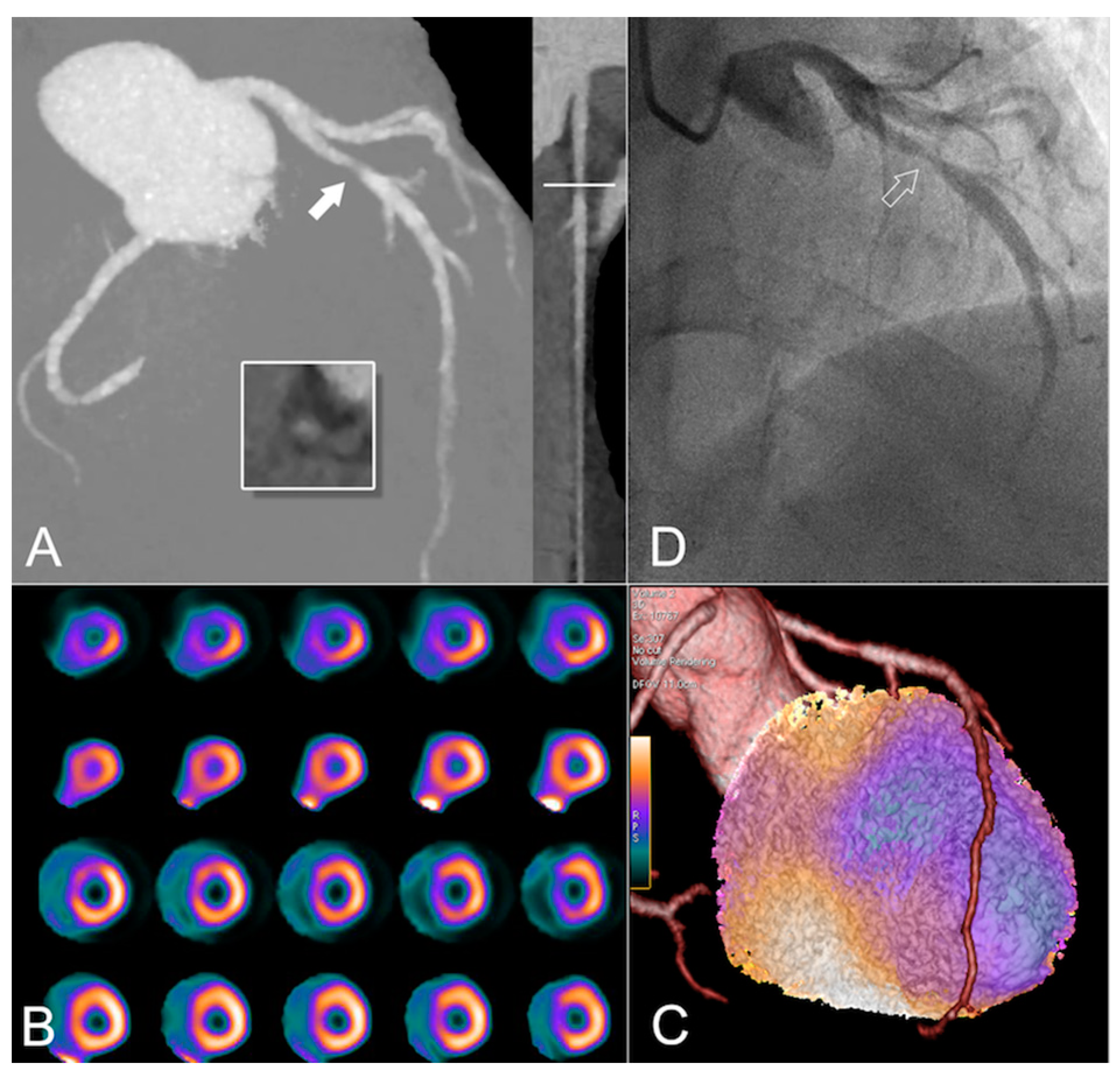
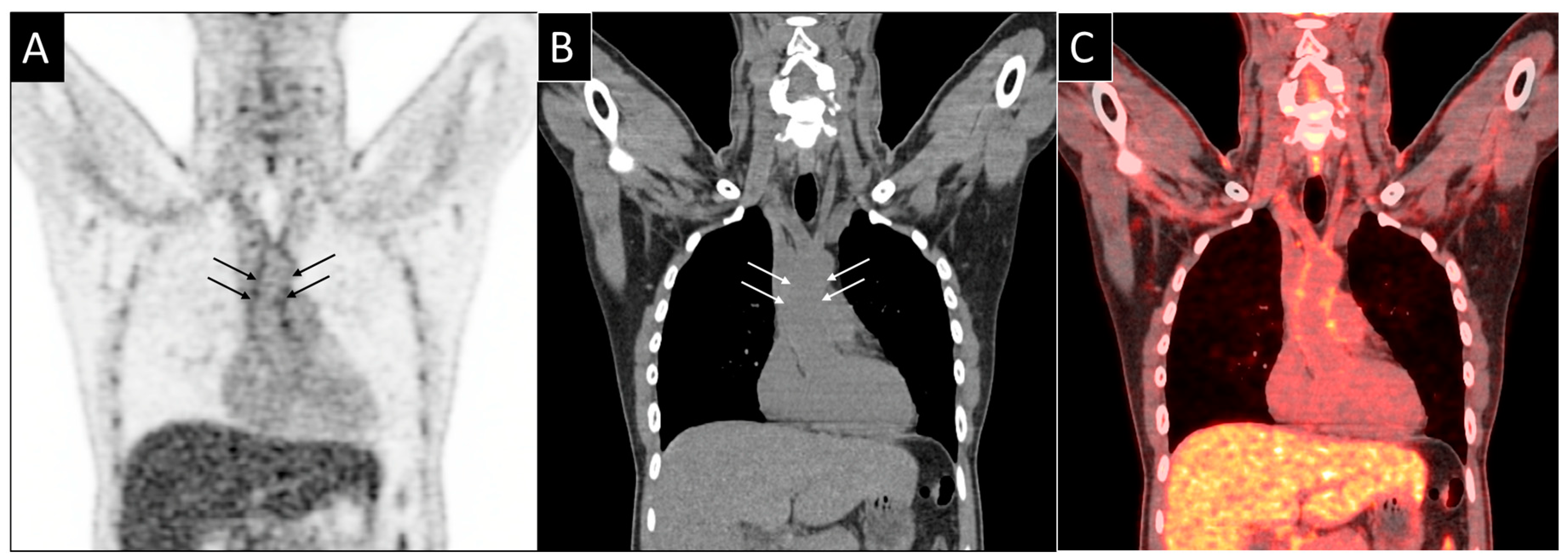
6. 18F-Fluorodeoxyglucose Positron Emission Tomography (FDG PET)
7. Outlook
Author Contributions
Funding
Conflicts of Interest
References
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation 2015, 133, 38–360. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.V.; Stelzle, D.; Lee, K.K.; Beck, E.J.; Alam, S.; Clifford, S.; Longenecker, C.T.; Strachan, F.; Bagchi, S.; Whiteley, W.; et al. Global Burden of Atherosclerotic Cardiovascular Disease in People Living With HIV. Circulation 2018, 138, 1100–1112. [Google Scholar] [CrossRef] [PubMed]
- Weber, R.; Ruppik, M.; Rickenbach, M.; Spoerri, A.; Furrer, H.; Battegay, M.; Cavassini, M.; Calmy, A.; Bernasconi, E.; Schmid, P.; et al. Decreasing mortality and changing patterns of causes of death in the Swiss HIV Cohort Study. HIV Med. 2013, 14, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.J.; Ryom, L.; Weber, R.; Morlat, P.; Pradier, C.; Reiss, P.; Kowalska, J.D.; de Wit, S.; Law, M.; el Sadr, W.; et al. Trends over time in underlying causes of death amongst HIV-positive individuals from 1999 to 2011. Lancet 2014, 384, 241–248. [Google Scholar] [CrossRef]
- Frieden, T.R.; Jaffe, M.G. Saving 100 million lives by improving global treatment of hypertension and reducing cardiovascular disease risk factors. J. Clin. Hypertens. 2018, 20, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.; Sabin, K.; Godfrey-Faussett, P. Approaches to Improve the Surveillance, Monitoring, and Management of Noncommunicable Diseases in HIV-Infected Persons: Viewpoint. JMIR Public Heal. Surveill. 2018, 4, e10989. [Google Scholar] [CrossRef] [PubMed]
- Hsue, P.Y.; Waters, D.D. Time to Recognize HIV Infection as a Major Cardiovascular Risk Factor. Circulation 2018, 138, 1113–1115. [Google Scholar] [CrossRef]
- Hasse, B.; Tarr, P.E.; Marques-Vidal, P.; Waeber, G.; Preisig, M.; Mooser, V.; Valeri, F.; Djalali, S.; Andri, R.; Bernasconie, E.; et al. Strong Impact of Smoking on Multimorbidity Immunodeficiency Virus-Infected Individuals in and Cardiovascular Risk Among Human Comparison With the General Population. Open Forum Infect. Dis. 2015. [Google Scholar] [CrossRef]
- Rasmussen, L.D.; Helleberg, M.; May, M.T.; Afzal, S.; Kronborg, G.; Larsen, C.S.; Pedersen, C.; Gerstoft, J.; Nordestgaard, B.G.; Obel, N. Myocardial infarction among danish HIV-infected individuals: Population-attributable fractions associated with smoking. Clin. Infect. Dis. 2015, 60, 1415–1423. [Google Scholar] [CrossRef]
- Engel, T.; Raffenberg, M.; Marzolini, C.; Cavassini, M.; Kovari, H.; Hasse, B.; Tarr, P.E. HIV and Aging-Perhaps Not as Dramatic as We Feared? Gerontology 2018, 64, 446–456. [Google Scholar] [CrossRef]
- Triant, V.A.; Lee, H.; Hadigan, C.; Grinspoon, S.K. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J. Clin. Endocrinol. Metab. 2007, 92, 2506–2512. [Google Scholar] [CrossRef] [PubMed]
- De Lima, L.R.; Petroski, E.L.; Moreno, Y.M.; Silva, D.A.; Trindade, E.B.; de Carvalho, A.P.; de Carlos Back, I. Dyslipidemia, chronic inflammation, and subclinical atherosclerosis in children and adolescents infected with HIV: The PositHIVe Health Study. PLoS ONE 2018, 13, 1–17. [Google Scholar]
- Mallon, P.W.G. Getting to the Heart of HIV and Myocardial Infarction. JAMA Intern. Med. 2013, 173, 622. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.D.; May, M.T.; Kronborg, G.; Larsen, C.S.; Pedersen, C.; Gerstoft, J.; Obel, N. Time trends for risk of severe age-related diseases in individuals with and without HIV infection in Denmark: A nationwide population-based cohort study. Lancet HIV 2015, 2, e288–e298. [Google Scholar] [CrossRef]
- Drozd, D.R.; Kitahata, M.M.; Althoff, K.N.; Zhang, J.; Gange, S.J.; Napravnik, S.; Burkholder, G.A.; Mathews, W.C.; Silverberg, M.J.; Sterling, T.R.; et al. Increased Risk of Myocardial Infarction in HIV-Infected Individuals in North America Compared with the General Population. J. Acquir. Immune Defic. Syndr. 2017, 75, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Freiberg, M.S.; Chang, C.C.H.; Kuller, L.H.; Skanderson, M.; Lowy, E.; Kraemer, K.L.; Butt, A.A.; Goetz, M.B.; Leaf, D.; Oursler, K.A.; et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern. Med. 2013, 173, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.B.; Leyden, W.A.; Xu, L.; Chao, C.R.; Horberg, M.A.; Towner, W.J.; Hurley, L.B.; Marcus, J.L.; Quesenberry, C.P.; Silverberg, M.J. Declining relative risk for myocardial infarction among HIV-positive compared with HIV-negative individuals with access to care. Clin. Infect. Dis. 2015, 60, 1278–1280. [Google Scholar] [CrossRef] [PubMed]
- Tarr, P.E.; Ledergerber, B.; Calmy, A.; Doco-Lecompte, T.; Marzel, A.; Weber, R.; Kaufmann, P.A.; Nkoulou, R.; Buechel, R.R.; Kovari, H. Subclinical coronary artery disease in Swiss HIV-positive and HIV-negative persons. Eur. Heart J. 2018, 39, 2147–2154. [Google Scholar] [CrossRef] [PubMed]
- Lang, S.; Mary-Krausea, M.; Cotte, L.; Gilquind, J.; Partisanie, M.; Simonf, A.; Boccarag, F.; Binghamh, A.; Dominique, C.; for the French Hospital Database on HIV-ANRS CO4. Increased risk of myocardial infarction in HIV-infected patients in France, relative to the general population. Res. Lett. 2010, 24, 1228–1230. [Google Scholar] [CrossRef]
- Boccara, F.; Lang, S.; Meuleman, C.; Ederhy, S.; Mary-Krause, M.; Costagliola, D.; Capeau, J.; Cohen, A. HIV and coronary heart disease: Time for a better understanding. J. Am. Coll. Cardiol. 2013, 61, 511–523. [Google Scholar] [CrossRef]
- Vachiat, A.; McCutcheon, K.; Tsabedze, N.; Zachariah, D.; Manga, P. HIV and Ischemic Heart Disease. J. Am. Coll. Cardiol. 2017, 69, 73–82. [Google Scholar] [CrossRef]
- Wang, X.; Chai, H.; Yao, Q.; Chen, C. Molecular Mechanisms of HIV Protease Inhibitor-Induced. J. Acquir. Immune Defic. Syndr. 2007, 44, 493–499. [Google Scholar] [CrossRef]
- Worm, S.W.; Sabin, C.; Weber, R.; Reiss, P.; El-Sadr, W.; Dabis, F.; De Wit, S.; Law, M.; Monforte, A.D.; Friis-Møller, N.; et al. Risk of Myocardial Infarction in Patients with HIV Infection Exposed to Specific Individual Antiretroviral Drugs from the 3 Major Drug Classes: The Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) Study. J. Infect. Dis. 2009, 201, 318–330. [Google Scholar] [CrossRef]
- Subramanya, V.; McKay, H.S.; Brusca, R.M.; Palella, F.J.; Kingsley, L.A.; Witt, M.D.; Hodis, H.N.; Tracy, R.P.; Post, W.S.; Haberlen, S.A. Inflammatory biomarkers and subclinical carotid atherosclerosis in HIV-infected and HIV-uninfected men in the Multicenter AIDS Cohort Study. PLoS ONE 2019, 14, e0214735. [Google Scholar] [CrossRef]
- Tenorio, A.R.; Zheng, Y.; Bosch, R.J.; Krishnan, S.; Rodriguez, B.; Hunt, P.W.; Plants, J.; Seth, A.; Wilson, C.C.; Deeks, S.G.; et al. Soluble Markers of In flammation and Coagulation but Not T-Cell Activation Predict Non-AIDS-Defining Morbid Events During Suppressive Antiretroviral Treatment. J. Infect. Dis. 2014, 210, 1248–1259. [Google Scholar] [CrossRef]
- Kuller, L.H.; Tracy, R.; Belloso, W.; De Wit, S.; Drummond, F.; Lane, H.C.; Ledergerber, B.; Lundgren, J.; Neuhaus, J.; Nixon, D.; et al. Inflammatory and Coagulation Biomarkers and Mortality in Patients with HIV Infection. PLoS Med. 2008, 5, e203. [Google Scholar] [CrossRef]
- So-Armah, K.A.; Tate, J.P.; Chang, C.H.; Butt, A.A.; Gerschenson, M.; Gibert, C.L.; Leaf, D.; Rimland, D.; Rodriguez-barradas, M.C.; Budoff, M.J.; et al. Do Biomarkers of Inflammation, Monocyte Activation, and Altered Coagulation Explain Excess Mortality Between HIV Infected and Uninfected People? J. Acquir. Immune Defic. Syndr. 2016, 72, 206–213. [Google Scholar] [CrossRef]
- Sandler, N.G.; Wand, H.; Roque, A.; Law, M.; Nason, M.C.; Nixon, D.E.; Pedersen, C.; Ruxrungtham, K.; Lewin, S.R.; Emery, S.; et al. Plasma Levels of Soluble CD14 Independently Predict Mortality in HIV Infection. 2011, 203, 780–790. J. Infect. Dis. 2011, 203, 780–790. [Google Scholar] [CrossRef]
- Kelesidis, T.; Kendall, M.A.; Yang, O.O.; Hodis, H.N.; Currier, J.S. Biomarkers of Microbial Translocation and Macrophage Activation: Association with Progression of Subclinical Atherosclerosis in HIV-1 Infection. J. Infect. Dis. 2012, 206, 1558–1567. [Google Scholar] [CrossRef]
- Hanna, D.B.; Lin, J.; Post, W.S.; Hodis, H.N.; Xue, X.; Anastos, K.; Cohen, M.H.; Gange, S.J.; Haberlen, S.A.; Heath, S.L.; et al. Association of Macrophage Inflammation Biomarkers With Progression of Subclinical Carotid Artery Atherosclerosis in HIV-Infected Women and Men. J. Infect. Dis. 2017, 10461, 1352–1361. [Google Scholar] [CrossRef]
- Burdo, T.H.; Lo, J.; Abbara, S.; Wei, J.; Delelys, M.E.; Preffer, F.; Rosenberg, E.S.; Williams, K.C.; Grinspoon, S. Soluble CD163, a Novel Marker of Activated Macrophages, Is Elevated and Associated With Noncalcified Coronary Plaque in HIV-Infected Patients. J. Infect. Dis. 2011, 204, 1227–1236. [Google Scholar] [CrossRef]
- Eugenin, E.A.; Morgello, S.; Klotman, M.E.; Mosoian, A.; Lento, P.A.; Berman, J.W.; Schecter, A.D. Human Immunodeficiency Virus (HIV) Infects Human Arterial Smooth Muscle Cells in Vivo and in Vitro Implications for the Pathogenesis of HIV-Mediated Vascular Disease. Am. J. Pathol. 2008, 172, 1100–1111. [Google Scholar] [CrossRef]
- Tabib, A.; Mornex, C.; Leroux, J.-F.; Loire, R. Accelerated coronary atherosclerosis and arteriosclerosis in young human-immunodeficiency-virus-positive patients. Coron. Artery Dis. 2000, 11, 41–46. [Google Scholar] [CrossRef]
- Zanni, M.V.; Schouten, J.; Grinspoon, S.K.; Reiss, P. Risk of coronary heart disease in patients with HIV infection. Nat. Rev. Cardiol. 2014, 11, 728. [Google Scholar] [CrossRef]
- Wolf, K.; Tsakiris, D.A.; Weber, R.; Erb, P.; Battegay, M. Antiretroviral Therapy Reduces Markers of Endothelial and Coagulation Activation in Patients Infected with Human Immunodeficiency Virus Type 1. J. Infect. Dis. 2002, 185, 456–462. [Google Scholar] [CrossRef]
- Lang, S.; Mary-Krause, M.; Simon, A.; Partisani, M.; Gilquin, J.; Cotte, L.; Boccara, F.; Costagliola, D. HIV Replication and Immune Status Are Independent Predictors of the Risk of Myocardial Infarction in HIV-Infected Individuals. Clin. Infect. Dis. 2012, 55, 600–607. [Google Scholar] [CrossRef]
- Michael, S.; Leyden, W.A.; Xu, L.; Horberg, M.A.; Chao, C.R.; Towner, W.J.; Hurley, L.B.; Quesenberry, C.P.; Klein, D.B. Immunodeficiency and risk of myocardial infarction among HIV-positive individuals with access to care. J. Acquir. Immune Defic. Syndr. 2014, 65, 160–166. [Google Scholar]
- Rotger, M.; Glass, T.R.; Junier, T.; Lundgren, J.; Neaton, J.D.; Poloni, E.S.; Van ’T Wout, A.B.; Lubomirov, R.; Colombo, S.; Martinez, R.; et al. Contribution of genetic background, traditional risk factors, and HIV-related factors to coronary artery disease events in HIV-positive persons. Clin. Infect. Dis. 2013, 57, 112–121. [Google Scholar] [CrossRef]
- Sabin, C.A.; Ryom, L.; De Wit, S.; Mocroft, A.; Phillips, A.N.; Worm, S.W.; Weber, R.; Monforte, A.D.; Reiss, P.; Kamara, D.; et al. Associations between immune depression and cardiovascular events in HIV infection. AIDS 2013, 27, 2735–2748. [Google Scholar] [CrossRef]
- Périard, D.; Telenti, A.; Sudre, P.; Cheseaux, J.J.; Halfon, P.; Reymond, M.J.; Marcovina, S.M.; Glauser, M.P.; Nicod, P.; Darioli, R.; et al. Atherogenic dyslipidemia in HIV-infected individuals treated with protease inhibitors. Circulation 1999, 100, 700–705. [Google Scholar] [CrossRef]
- Ryom, L.; Lundgren, J.D.; El-Sadr, W.; Reiss, P.; Kirk, O.; Law, M.; Phillips, A.; Weber, R.; Fontas, E.; d’Arminio Monforte, A.; et al. Cardiovascular disease and use of contemporary protease inhibitors: The D:A:D international prospective multicohort study. Lancet HIV 2018, 5, e291–e300. [Google Scholar] [CrossRef]
- Sabin, C.A.; Worm, S.W.; Weber, R.; Reiss, P.; El-Sadr, W.; Dabis, F.; De Wit, S.; Law, M.; D’Arminio Monforte, A.; Friis-Møller, N.; et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: A multi-cohort collaboration. Lancet 2008, 371, 1417–1426. [Google Scholar]
- Lai, H.; Moore, R.; Celentano, D.D.; Gerstenblith, G.; Treisman, G.; Keruly, J.C.; Kickler, T.; Li, J.; Chen, S.; Lai, S.; et al. HIV infection itself may not be associated with subclinical coronary artery disease among African Americans without cardiovascular symptoms. J. Am. Heart Assoc. 2015, 5, 1–16. [Google Scholar] [CrossRef]
- Post, W.S.; Budoff, M.; Kingsley, L.; Palella, F.J.; Witt, M.D.; Li, X.; George, R.T.; Brown, T.; Jacobson, L.P. Associations between HIV Infection and Subclinical Coronary Atherosclerosis: The Multicenter AIDS Cohort Study (MACS). Ann. Intern. Med. 2014, 160, 458–467. [Google Scholar] [CrossRef]
- Stein, J.H.; Currier, J.S.; Hsue, P.Y. Arterial Disease in Patients With Human Immunodeficiency Virus Infection. JACC Cardiovasc. Imaging 2014, 7, 515–525. [Google Scholar] [CrossRef]
- Inaba, Y.; Chen, J.A.; Bergmann, S.R. Carotid Intima-Media Thickness and Cardiovascular Events. N. Engl. J. Med. 2011, 365, 1640–1642. [Google Scholar]
- Lorenz, M.W.; Polak, J.F.; Kavousi, M.; Mathiesen, E.B.; Völzke, H.; Tuomainen, T.P.; Sander, D.; Plichart, M.; Catapano, A.L.; Robertson, C.M.; et al. Carotid intima-media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): A meta-analysis of individual participant data. Lancet 2012, 379, 2053–2062. [Google Scholar] [CrossRef]
- O’Leary, D.H.; Polak, J.F.; Kronmal, R.A.; Manolio, T.A.; Burke, G.L.; Wolfson, S.K. Carotid-Artery Intima and Media Thickness as a Risk Factor for Myocardial Infarction and Stroke in Older Adults. N. Engl. J. Med. 2002, 340, 14–22. [Google Scholar] [CrossRef]
- Den Ruijter, H.M.; Peters, S.A.E.; Anderson, T.J.; Britton, A.R.; Dekker, J.M.; Eijkemans, M.J.; Engström, G.; Evans, G.W.; de Graaf, J.; Grobbee, D.E.; et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: A meta-analysis. JAMA 2012, 308, 796–803. [Google Scholar] [CrossRef]
- Hulten, E.; Mitchell, J.; Scally, J.; Gibbs, B.; Villines, T.C. HIV positivity, protease inhibitor exposure and subclinical atherosclerosis: A systematic review and meta-analysis of observational studies. Heart 2009, 95, 1826–1835. [Google Scholar] [CrossRef]
- Maggi, P.; Serio, G.; Epifani, G.; Fiorentino, G.; Saracino, A.; Fico, C.; Perilli, F.; Lillo, A.; Ferraro, S.; Gargiulo, M.; et al. Premature lesions of the carotid vessels in HIV-1-infected patients treated with protease inhibitors. AIDS 2000, 14, F123–F128. [Google Scholar] [CrossRef]
- Maggi, P.; Lillo, A.; Perilli, F.; Maserati, R.; Chirianni, A.; Epifani, G.; Fiorentino, G.; Ladisa, N.; Pastore, G.; Angiletta, D.; et al. Colour-Doppler ultrasonography of carotid vessels in patients treated with antiretroviral therapy: A comparative study. AIDS 2004, 18, 1023–1028. [Google Scholar] [CrossRef]
- Hsue, P.Y.; Lo, J.C.; Franklin, A.; Bolger, A.F.; Martin, J.N.; Deeks, S.G.; Waters, D.D. Progression of Atherosclerosis as Assessed by Carotid Intima-Media Thickness in Patients with HIV Infection. Circulation 2004, 109, 1603–1608. [Google Scholar] [CrossRef]
- Mercié, P.; Thiébaut, R.; Aurillac-Lavignolle, V.; Pellegrin, J.L.; Yvorra-Vives, M.C.; Cipriano, C.; Neau, D.; Morlat, P.; Ragnaud, J.M.; Dupon, M.; et al. Carotid intima-media thickness is slightly increased over time in HIV-1-infected patients. HIV Med. 2005, 6, 380–387. [Google Scholar] [CrossRef]
- Hsue, P.Y.; Hunt, P.W.; Sinclair, E.; Bredt, B.; Franklin, A.; Killian, M.; Hoh, R.; Martin, J.N.; McCune, J.M.; Waters, D.D.; et al. Increased carotid intima-media thickness in HIV patients is associated with increased cytomegalovirus-specific T-cell responses. AIDS 2006, 20, 2275–2283. [Google Scholar] [CrossRef]
- Thiebaut, R.; Aurillac-Lavignolleb, V.; Bonnetb, F.; Ibrahimd, N.; Ciprianoc, C.; Neauc, D.; Duponc, M.; Dabisb, F.; Mercie, P.; Groupe d’Epidemiologie Clinique du Sida en Aquitaine (GECSA). Change in atherosclerosis progression in HIV infected patients: ANRS Aquitaine Cohort, 1999–2004. AIDS 2005, 19, 729–731. [Google Scholar] [CrossRef]
- Johnsen, S.; Dolan, S.E.; Fitch, K.V.; Kanter, J.R.; Hemphill, L.C.; Connelly, J.M.; Lees, R.S.; Lee, H.; Grinspoon, S. Carotid intimal medial thickness in human immunodeficiency virus-infected women: Effects of protease inhibitor use, cardiac risk factors, and the metabolic syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 4916–4924. [Google Scholar] [CrossRef]
- Van Wijk, J.P.H.; De Koning, E.J.P.; Cabezas, M.C.; Joven, J.; Op’t Roodt, J.; Rabelink, T.J.; Hoepelman, A.M. Functional and structural markers of atherosclerosis in human immunodeficiency virus-infected patients. J. Am. Coll. Cardiol. 2006, 47, 1117–1123. [Google Scholar] [CrossRef]
- Currier, J.S.; Kendall, M.A.; Henry, W.K.; Alston-Smith, B.; Torriani, F.J.; Tebas, P.; Li, Y.; Hodis, H.N. Progression of carotid artery intima-media thickening in HIV-infected and uninfected adults. AIDS 2007, 21, 1137–1145. [Google Scholar] [CrossRef]
- Jericó, C.; Knobel, H.; Calvo, N.; Sorli, M.L.; Guelar, A.; Gimeno-Bayón, J.L.; Saballs, P.; López-Colomés, J.L.; Pedro-Botet, J. Subclinical carotid atherosclerosis in HIV-infected patients: Role of combination antiretroviral therapy. Stroke 2006, 37, 812–817. [Google Scholar] [CrossRef]
- Lorenz, M.W.; Stephan, C.; Harmjanz, A.; Staszewski, S.; Buehler, A.; Bickel, M.; von Kegler, S.; Ruhkamp, D.; Steinmetz, H.; Sitzer, M. Both long-term HIV infection and highly active antiretroviral therapy are independent risk factors for early carotid atherosclerosis. Atherosclerosis 2008, 196, 720–726. [Google Scholar] [CrossRef]
- Coll, B.; Parra, S.; Alonso-Villaverde, C.; Aragonés, G.; Montero, M.; Camps, J.; Joven, J.; Masana, L. The role of immunity and inflammation in the progression of atherosclerosis in patients with HIV infection. Stroke 2007, 38, 2477–2484. [Google Scholar] [CrossRef]
- Depairon, M.; Chessex, S.; Sudre, P.; Rodondi, N.; Doser, N.; Chave, J.P.; Riesen, W.; Nicod, P.; Darioli, R.; Telenti, A.; et al. Premature atherosclerosis in hiv-infected individuals focus on protease inhibitor therapy. AIDS 2001, 15, 329–334. [Google Scholar] [CrossRef]
- Maggi, P.; Perilli, F.; Lillo, A.; Gargiulo, M.; Ferraro, S.; Grisorio, B.; Ferrara, S.; Carito, V.; Bellacosa, C.; Pastore, G.; et al. Rapid progression of carotid lesions in HAART-treated HIV-1 patients. Atherosclerosis 2007, 192, 407–412. [Google Scholar] [CrossRef]
- Grunfeld, C.; Delaney, J.A.; Wanke, C.; Currier, J.S.; Scherzer, R.; Biggs, M.L.; Tien, P.C.; Shlipak, M.G.; Sidney, S.; Polak, J.F.; et al. Preclinical atherosclerosis due to HIV infection: Carotid intima-medial thickness measurements from the FRAM study. AIDS 2009, 23, 1841–1849. [Google Scholar] [CrossRef]
- Hsue, P.Y.; Hunt, P.W.; Schnell, A.; Kalapus, S.C.; Hoh, R.; Ganz, P.; Martin, J.N.; Deeks, S.G. Role of viral replication, antiretroviral therapy, and immunodeficiency in HIV-associated atherosclerosis. AIDS 2009, 23, 1059–1067. [Google Scholar] [CrossRef]
- Cabello, C.M.; Bair, W.B.; Lamore, S.D.; Ley, S.; Alexandra, S.; Azimian, S.; Wondrak, G.T. Silencing of germline-expressed genes by DNA elimination in somatic cells. Dev. Cell 2010, 46, 220–231. [Google Scholar]
- Kaplan, R.C.; Sinclair, E.; Landay, A.L.; Lurain, N.; Sharrett, A.R.; Gange, S.J.; Xue, X.; Hunt, P.; Karim, R.; Kern, D.M.; et al. T Cell Activation and Senescence Predict Subclinical Carotid Artery Disease in HIV-Infected Women. J. Infect. Dis. 2011, 203, 452–463. [Google Scholar] [CrossRef]
- Sainz, T.; Álvarez-Fuente, M.; Navarro, M.L.; Díaz, L.; Rojo, P.; Blázquez, D.; De José, M.I.; Ramos, J.T.; Serrano-Villar, S.; Martínez, J.; et al. Subclinical atherosclerosis and markers of immune activation in hiv-infected children and adolescents: The carovih study. J. Acquir. Immune Defic. Syndr. 2014, 65, 42–49. [Google Scholar] [CrossRef]
- Hanna, D.B.; Post, W.S.; Deal, J.A.; Hodis, H.N.; Jacobson, L.P.; Mack, W.J.; Anastos, K.; Gange, S.J.; Landay, A.L.; Lazar, J.M.; et al. HIV Infection Is Associated with Progression of Subclinical Carotid Atherosclerosis. Clin. Infect. Dis. 2015, 61, 640–650. [Google Scholar] [CrossRef]
- Hsue, P.Y.; Scherzer, R.; Hunt, P.W.; Schnell, A.; Bolger, A.F.; Kalapus, S.C.; Maka, K.; Martin, J.N.; Ganz, P.; Deeks, S.G. Carotid Intima-Media Thickness Progression in HIV-Infected Adults Occurs Preferentially at the Carotid Bifurcation and Is Predicted by Inflammation. J. Am. Heart Assoc. 2012, 1, 1–12. [Google Scholar] [CrossRef]
- Bots, M.L.; Baldassarre, D.; Simon, A.; De Groot, E.; O’Leary, D.H.; Riley, W.; Kastelein, J.J.; Grobbee, D.E. Carotid intima-media thickness and coronary atherosclerosis: Weak or strong relations? Eur. Heart J. 2007, 28, 398–406. [Google Scholar] [CrossRef]
- Hodis, H.N.; Mack, W.J.; Labree, L.; Selzer, R.H. The Role of Carotid Arterial Intima-Media Thickness in Predicting Clinical Coronary Events Methods Study Design. Annals Intern. Med. 2006, 128, 262–269. [Google Scholar] [CrossRef]
- Greenland, P.; Alpert, J.S.; Beller, G.; Benjamin, E.J.; Budoff, M.J.; Fayad, Z.A.; Foster, E.; Hlatky, M.A.; Hodgson, J.M.; Kushner, F.G.; et al. 2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults. J. Am. Coll. Cardiol. 2010, 56, 50–103. [Google Scholar] [CrossRef]
- Callister, T.Q.; Cooil, B.; Raya, S.; Lippolis, N.J.; Russo, D.J.; Raggi, P. Coronary artery disease: improved reproducibility of calcium scoring with an electron-beam CT volumetric method. Radiology 2014, 208, 807–814. [Google Scholar] [CrossRef]
- Callister, T.Q.; Raggi, P.; Cooil, B.; Lippolis, N.J.; Russo, D.J. Effect of HMG-CoA Reductase Inhibitors on Coronary Artery Disease as Assessed by Electron-Beam Computed Tomography. N. Engl. J. Med. 2002, 339, 1972–1978. [Google Scholar] [CrossRef]
- Raggi, P.; Callister, T.Q.; Shaw, L.J. Progression of coronary artery calcium and risk of first myocardial infarction in patients receiving cholesterol-lowering therapy. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 1272–1277. [Google Scholar] [CrossRef]
- Raggi, P.; Davidson, M.; Callister, T.Q.; Welty, F.K.; Bachmann, G.A.; Hecht, H.; Rumberger, J.A. Aggressive Versus Moderate Lipid-Lowering Therapy in Hypercholesterolemic Postmenopausal Women. Circulation 2005, 112, 563–571. [Google Scholar] [CrossRef]
- Achenbach, S.; Ropers, D.; Pohle, K.; Leber, A.; Thilo, C.; Knez, A.; Menendez, T.; Maeffert, R.; Kusus, M.; Regenfus, M.; et al. Influence of lipid-lowering therapy on the progression of coronary artery calcification: A prospective evaluation. Circulation 2002, 106, 1077–1082. [Google Scholar] [CrossRef]
- Bonow, R.O. Should Coronary Calcium Screening Be Used in Cardiovascular Prevention Strategies? N. Engl. J. Med. 2009, 361, 990–997. [Google Scholar] [CrossRef]
- Hoffmann, U.; Brady, T.J.; Muller, J. Use of New Imaging Techniques to Screen for Coronary Artery Disease. Circulation 2003, 108, 1–4. [Google Scholar] [CrossRef]
- Polonsky, T.S.; Mcclelland, R.L.; Jorgensen, N.W.; Bild, D.E.; Burke, G.L.; Guerci, A.D.; Greenland, P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2011, 303, 1610–1616. [Google Scholar] [CrossRef]
- Schmermund, A.; Baumgart, D.; Möhlenkamp, S.; Kriener, P.; Pump, H.; Grönemeyer, D.; Seibel, R.; Erbel, R. Natural History and Topographic Pattern of Progression of Coronary Calcification in Symptomatic Patients. Arterioscler. Thromb. Vasc. Biol. 2011, 21, 421–426. [Google Scholar] [CrossRef]
- Detrano, R.; Guerci, A.D.; Carr, J.J.; Bild, D.E.; Burke, G.; Folsom, A.R.; Liu, K.; Shea, S.; Szklo, M.; Bluemke, D.A.; et al. Coronary Calcium as a Predictor of Coronary Events in Four Racial or Ethnic Groups. N. Engl. J. Med. 2008, 358, 1336–1345. [Google Scholar] [CrossRef]
- Pletcher, M.; Tice, J.; Pignone, M.; Browner, W. Using the Coronary Artery Calcium Score to Predict Coronary Heart Disease Events. Arch. Intern. Med. 2004, 164, 1285–1292. [Google Scholar] [CrossRef]
- Folsam, A.; Kronmal, R.A.; Detrano, R.; O’Leary, D.; Bild, D.E.; Bluemke, D.A.; Budoff, M.J.; Liu, K.; Shea, S.; Szklo, M.; et al. Coronary Artery Calcification Compared With Carotid Intima-Media Thickness in the Prediction of Cardiovascular Disease Incidence. Arch. Intern. Med. 2008, 168, 1333–1339. [Google Scholar] [CrossRef]
- Taylor, A.J.; Bindeman, J.; Feuerstein, I.; Cao, F.; Brazaitis, M.; O’Malley, P.G. Coronary Calcium Independently Predicts Incident Premature Coronary Heart Disease Over Measured Cardiovascular Risk Factors. J. Am. Coll. Cardiol. 2005, 46, 807–814. [Google Scholar] [CrossRef]
- Arad, Y.; Goodman, K.J.; Roth, M.; Newstein, D.; Guerci, A.D. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: The St. Francis heart study. J. Am. Coll. Cardiol. 2005, 46, 158–165. [Google Scholar] [CrossRef]
- Budoff, M.J.; Shaw, L.J.; Liu, S.T.; Weinstein, S.R.; Mosler, T.P.; Tseng, P.H.; Flores, F.R.; Callister, T.Q.; Raggi, P.; Berman, D.S. Long-Term Prognosis Associated With Coronary Calcification. Observations From a Registry of 25,253 Patients. J. Am. Coll. Cardiol. 2007, 49, 1860–1870. [Google Scholar] [CrossRef]
- Raggi, P.; Cooil, B.; Shaw, L.J.; Aboulhson, J.; Takasu, J.; Budoff, M.; Callister, T.Q. Progression of coronary calcium on serial electron beam tomographic scanning is greater in patients with future myocardial infarction. Am. J. Cardiol. 2003, 92, 827–829. [Google Scholar] [CrossRef]
- Newman, A.B.; Naydeck, B.; Ives, D.; Boudreau, R.; Sutton-Tyrrell, K.; O’Leary, D.H.; Kuller, L.H. Coronary Artery Calcium, Carotid Artery Wall Thickness and Cardiovascular Disease Outcomes in Adults 70 to 99 Years Old. Am. J. Cardiol. 2010, 46, 220–231. [Google Scholar] [CrossRef]
- Vliegenthart, R.; Oudkerk, M.; Hofman, A.; Oei, H.-H.; van Dijck, W.; Van Rooij, F.J.A.; Witteman, J.C.M. Coronary Calcification Improves Cardiovascular Risk Prediction in the Elderly. Circulation 2005, 572–577. [Google Scholar] [CrossRef]
- Jain, A.; McClelland, R.L.; Polak, J.F.; Shea, S.; Burke, G.L.; Bild, D.E.; Watson, K.E.; Budoff, M.J.; Liu, K.; Post, W.S.; et al. Cardiovascular imaging for assessing cardiovascular risk in asymptomatic men versus women the Multi-Ethnic Study of Atherosclerosis (MESA). Circ. Cardiovasc. Imaging 2011, 4, 8–15. [Google Scholar] [CrossRef]
- Yeboah, J.; Mcclelland, R.L.; Polonsky, T.S.; Burke, G.L.; Sibley, C.T.; O’Leary, D.H.; Carr, J.J.; Goff, D.C.; Greenland, P.; Herrington, D.M. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012, 308, 788–795. [Google Scholar] [CrossRef]
- Guaraldi, G.; Zona, S.; Alexopoulos, N.; Orlando, G.; Carli, F.; Ligabue, G.; Fiocchi, F.; Lattanzi, A.; Rossi, R.; Modena, M.G.; et al. Coronary Aging in HIV-Infected Patients. Clin. Infect. Dis. 2009, 49, 1756–1762. [Google Scholar] [CrossRef]
- Kingsley, L.A.; Cuervo-Rojas, J.; Muñoz, A.; Palella, F.J.; Post, W.; Witt, M.D.; Budoff, M.; Kuller, L. Subclinical coronary atherosclerosis, HIV infection and antiretroviral therapy: Multicenter AIDS Cohort Study. AIDS 2008, 22, 1589–1599. [Google Scholar] [CrossRef]
- Motoyama, S.; Ito, H.; Sarai, M.; Kondo, T.; Kawai, H.; Nagahara, Y.; Harigaya, H.; Kan, S.; Anno, H.; Takahashi, H.; et al. Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J. Am. Coll. Cardiol. 2015, 66, 337–346. [Google Scholar] [CrossRef]
- Giannopoulos, A.A.; Benz, D.C.; Gräni, C.; Buechel, R.R. Imaging the event-prone coronary artery plaque. J. Nucl. Cardiol. 2019, 26, 141–153. [Google Scholar] [CrossRef]
- Monroe, A.K.; Haberlen, S.A.; Post, W.S.; Palella, F.; Kingsley, L.A.; Witts, M.D.; Budoff, M.; Jacobson, L.; Brown, T.T. Cardiovascular Disease Risk Scores’ Relationship to Subclinical Cardiovascular Disease Among HIV-Infected and HIV-Uninfected Men. AIDS 2015, 155, 1683–1695. [Google Scholar] [CrossRef]
- Ascenzo, F.D.; Cerrato, E.; Calcagno, A.; Grossomarra, W.; Montefusco, A.; Veglia, S.; Barbero, U.; Gili, S.; Cannillo, M.; Pianelli, M.; et al. High prevalence at computed coronary tomography of non-calcified plaques in asymptomatic HIV patients treated with HAART: A meta-analysis. Atherosclerosis 2015, 240, 197–204. [Google Scholar] [CrossRef]
- Schoeni-Affolter, F.; Ledergerber, B.; Rickenbach, M.; Rudin, C.; Günthard, H.F.; Telenti, A.; Furrer, H.; Yerly, S.; Francioli, P. Cohort profile: The Swiss HIV cohort study. Int. J. Epidemiol. 2010, 39, 1179–1189. [Google Scholar]
- Min, J.K.; Shaw, L.J.; Devereux, R.B.; Okin, P.M.; Weinsaft, J.W.; Russo, D.J.; Lippolis, N.J.; Berman, D.S.; Callister, T.Q. Prognostic Value of Multidetector Coronary Computed Tomographic Angiography for Prediction of All-Cause Mortality. J. Am. Coll. Cardiol. 2007, 50, 1161–1170. [Google Scholar] [CrossRef]
- Abd-Elmoniem, K.Z.; Unsal, A.B.; Eshera, S.; Matta, J.R.; Muldoon, N.; McAreavey, D.; Purdy, J.B.; Hazra, R.; Hadigan, C.; Gharib, A.M. Increased coronary vessel wall thickness in HIV-infected young adults. Clin. Infect. Dis. 2014, 59, 1779–1786. [Google Scholar] [CrossRef]
- Husmann, L.; Valenta, I.; Gaemperli, O.; Adda, O.; Treyer, V.; Wyss, C.A.; Veit-haibach, P.; Tatsugami, F.; Von Schulthess, G.K.; Kaufmann, P.A. Feasibility of low-dose coronary CT angiography: First experience with prospective. Eur. Heart J. 2008, 29, 191–197. [Google Scholar] [CrossRef]
- Buechel, R.R.; Husmann, L.; Herzog, B.A.; Pazhenkottil, A.P.; Nkoulou, R.; Ghadri, J.R.; Treyer, V.; Von Schulthess, P.; Kaufmann, P.A. Low-dose computed tomography coronary angiography with prospective electrocardiogram triggering: Feasibility in a large population. J. Am. Coll. Cardiol. 2011, 57, 332–336. [Google Scholar] [CrossRef]
- Kaufmann, P.A. Low-Dose Computed Tomography Coronary Angiography With Prospective Triggering. A Promise for the Future. J. Am. Coll. Cardiol. 2008, 52, 1456–1457. [Google Scholar] [CrossRef][Green Version]
- Min, J.K.; Dunning, A.; Lin, F.Y.; Achenbach, S.; Al-Mallah, M.; Budoff, M.J.; Cademartiri, F.; Callister, T.Q.; Chang, H.J.; Cheng, V.; et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings: Results from the international multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multice. J. Am. Coll. Cardiol. 2011, 58, 849–860. [Google Scholar] [CrossRef]
- Hadamitzky, M.; Freißmuth, B.; Meyer, T.; Hein, F.; Kastrati, A.; Martinoff, S.; Schömig, A.; Hausleiter, J. Prognostic Value of Coronary Computed Tomographic Angiography for Prediction of Cardiac Events in Patients With Suspected Coronary Artery Disease. JACC Cardiovasc. Imaging 2009, 2, 404–411. [Google Scholar] [CrossRef]
- McEvoy, J.W.; Blaha, M.J.; Nasir, K.; Yoon, Y.E.; Choi, E.K.; Cho, I.S.; Chun, E.J.; Choi, S.I.; Rivera, J.J.; Blumenthal, R.S.; et al. Impact of coronary computed tomographic angiography results on patient and physician behavior in a low-risk population. Arch. Intern. Med. 2011, 171, 1260–1268. [Google Scholar] [CrossRef]
- Herzog, B.A.; Wyss, C.A.; Husmann, L.; Gaemperli, O.; Valenta, I.; Treyer, V.; Landmesser, U.; Kaufmann, P.A. First head-to-head comparison of effective radiation dose from low-dose 64-slice CT with prospective ECG-triggering versus invasive coronary angiography. Heart 2009, 95, 1656–1661. [Google Scholar] [CrossRef]
- Benz, D.C.; Gräni, C.; Hirt Moch, B.; Mikulicic, F.; Vontobel, J.; Fuchs, T.; Stehli, J.; Clerc, O.; Possner, M.; Pazhenkottil, A.; et al. A low-dose and an ultra-low-dose contrast agent protocol for coronary CT angiography in a clinical setting: Quantitative and qualitative comparison to a standard dose protocol. Br. J. Radiolody 2017, 90, 1–10. [Google Scholar] [CrossRef]
- Litt, H.; Gatsonis, C.; Snyder, B.; Singh, H.; Miller, C.; Entrikin, D.; Leaming, J.; Gavin, L.; Pacella, C.; Hollander, J. CT Angiography for Safe Discharge of Patients with Possible Acute Coronary Syndromes. N. Engl. J. Med. 2012, 366, 1393–1403. [Google Scholar] [CrossRef]
- Wyler von Ballmoos, M.; Haring, B.; Juillerat, P.; Alkadhi, H. Meta-analysis: Diagnostic Performance of Low-Radiation-Dose Coronary Computed Tomography Angiography. Ann. Intern. Med. 2011, 154, 413–420. [Google Scholar] [CrossRef]
- Goldstein, J.A.; Chinnaiyan, K.M.; Abidov, A.; Achenbach, S.; Berman, D.S.; Hayes, S.W.; Hoffmann, U.; Lesser, J.R.; Mikati, I.A.; Neil, B.J.O.; et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) Trial. J. Am. Coll. Cardiol. 2011, 58, 1414–1422. [Google Scholar] [CrossRef]
- Hachamovitch, R.; Hayes, S.W.; Friedman, J.D.; Cohen, I.; Berman, D.S. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003, 107, 2900–2906. [Google Scholar] [CrossRef]
- Petoumenos, K.; Law, M. Comment HIV-infection and comorbidities: A complex mix. Lancet HIV 2015, 2, e265–e266. [Google Scholar] [CrossRef]
- Gharib, A.M.; Abd-Elmoniem, K.Z.; Pettigrew, R.I.; Hadigan, C. Noninvasive Coronary Imaging for Atherosclerosis in Human Immunodeficiency Virus Infection. Curr. Probl. Diagn. Radiol. 2011, 40, 262–267. [Google Scholar] [CrossRef][Green Version]
- Van Velzen, J.E.; Schuijf, J.D.; De Graaf, F.R.; Boersma, E.; Pundziute, G.; Spanó, F.; Boogers, M.J.; Schalij, M.J.; Kroft, L.J.; De Roos, A.; et al. Diagnostic performance of non-invasive multidetector computed tomography coronary angiography to detect coronary artery disease using different endpoints: Detection of significant stenosis vs. detection of atherosclerosis. Eur. Heart J. 2011, 32, 637–645. [Google Scholar] [CrossRef]
- Wijns, W.; Kolh, P.; Danchin, N.; Di Mario, C.; Falk, V.; Folliguet, T.; Garg, S.; Huber, K.; James, S.; Knuuti, J.; et al. Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2010, 31, 2501–2555. [Google Scholar]
- Lin, F.Y.; Shaw, L.J.; Dunning, A.M.; Labounty, T.M.; Choi, J.; Weinsaft, J.W.; Koduru, S.; Gomez, M.J.; Delago, A.J.; Callister, T.Q.; et al. Mortality Risk in Symptomatic Patients with Nonobstructive Coronary Artery Disease. J. Am. Coll. Cardiol. 2011, 58, 510–519. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Kofoed, K.F.; Khl, J.T.; Nielsen, W.B.; Nielsen, M.B.; Kelbæk, H. Prognostic implications of nonobstructive coronary plaques in patients with NonST-segment elevation myocardial infarction: A multidetector computed tomography study. J. Am. Coll. Cardiol. 2011, 58, 502–509. [Google Scholar] [CrossRef]
- Fitch, K.V.; Lo, J.; Abbara, S.; Ghoshhajra, B.; Shturman, L.; Soni, A.; Sacks, R.; Wei, J.; Grinspoon, S. Increased coronary artery calcium score and noncalcified plaque among HIV-infected men: Relationship to metabolic syndrome and cardiac risk parameters. J. Acquir. Immune Defic. Syndr. 2010, 55, 495–499. [Google Scholar] [CrossRef]
- Lai, S.; Bartlett, J.; Lai, H.; Moore, R.; Cofrancesco, J.; Pannu, H.; Tong, W.; Meng, W.; Sun, H.; Fishman, E.K. Long-Term Combination Antiretroviral Therapy Is Associated with the Risk of Coronary Plaques in African Americans with HIV Infection. AIDS Patient Care STDS 2009, 23, 815–824. [Google Scholar] [CrossRef]
- Loa, J.; Abbarab, S.; Shturmanc, L.; Sonic, A.; Weia, J.; Rocha-Filhoc, J.; Nasirc, K.; Grinspoona, S.K. Increased prevalence of subclinical coronary atherosclerosis detected by coronary computed tomography angiography in HIV-infected men. AIDS 2010, 24, 243–253. [Google Scholar] [CrossRef]
- Duarte, H.; Matta, J.R.; Muldoon, N.; Masur, H.; Hadigan, C.; Gharib, A.M. Non-calcified coronary plaque volume inversely related to CD4(+)T-cell count in HIV infection. Antivir. Ther. 2012, 17, 763–767. [Google Scholar] [CrossRef]
- Post, W.S.; Haberlen, S.A.; Zhang, L. HIV infection is associated with progression of high risk coronary plaques in the MACS. In Proceedings of the Conference on Retroviruses and Opportunistic Infections, Boston, MA, USA, 4–7 March 2018. [Google Scholar]
- Ma, G.S.; Cotter, B.R. HIV and cardiovascular disease: much ado about nothing? Eur. Heart J. 2018, 39, 2155–2157. [Google Scholar] [CrossRef]
- Tunstall-Pedoe, H.; Kuulasmaa, K.; Amouyel, P.; Arveiler, D.; Rajakangas, A.M.; Pajak, A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation 1994, 90, 583–612. [Google Scholar] [CrossRef]
- Piepoli, M.; Hoes, A.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.; Cooney, M.-T.; Corra, U.; Verschuren, W.M.M. New European guidelines for cardiovascular disease prevention in clinical practice. Clin. Chem. Lab. Med. 2009, 47, 2315–2381. [Google Scholar]
- Huber, M.; Ledergerber, B.; Sauter, R.; Young, J.; Fehr, J.; Cusini, A.; Battegay, M.; Calmy, A.; Orasch, C.; Nicca, D.; et al. Outcome of smoking cessation counselling of HIV-positive persons by HIV care physicians. HIV Med. 2012, 13, 387–397. [Google Scholar] [CrossRef]
- Guajira, T.P.; Xiuhong, L.; Post, W.S.; Jacobson, L.P.; Witt, M.D.; Brown, T.T.; Kingsley, L.A.; Phair, J.P.; Palella, F.J. Associations between antiretroviral use and subclinical coronary atherosclerosis. AIDS 2016, 30, 2477–2486. [Google Scholar]
- Kovari, H.; Calmy, A.; Doco-Lecompte, T.; Nkoulou, R.; Marzel, A.; Weber, R.; Kaufmann, P.A.; Buechel, R.R.; Ledergerber, B.; Tarr, P.E. Antiretroviral Drugs Associated with Subclinical Coronary Artery Disease in the Swiss HIV Cohort Study. Clin. Infect. Dis. 2019, 30, 9. [Google Scholar]
- Duprez, D.A.; Neuhaus, J.; Kuller, L.H.; Tracy, R.; Belloso, W.; De Wit, S.; Drummond, F.; Lane, H.C.; Ledergerber, B.; Lundgren, J.; et al. Inflammation, coagulation and cardiovascular disease in HIV-infected individuals. PLoS ONE 2012, 7, e44454. [Google Scholar] [CrossRef]
- Calmy, A.; Gayet-Ageron, A.; Montecucco, F.; Nguyen, A.; Mach, F.; Burger, F.; Ubolyam, S.; Carr, A.; Ruxungtham, K.; Hirschel, B.; et al. HIV increases markers of cardiovascular risk: Results from a randomized, treatment interruption trial. AIDS 2009, 23, 929–939. [Google Scholar] [CrossRef]
- Polak, J.F.; Leary, D.H.O. Carotid Intima-Media Thickness as Surrogate for and Predictor of CVD. Glob. Heart 2016, 11, 295–312. [Google Scholar] [CrossRef]
- Du, J.; Wasserman, A.; Tong, W. Cholesterol Is Associated with the Presence of a Lipid Core in Carotid Plaque of Asymptomatic, Young-to-Middle-Aged African Americans with and without HIV Infection and Cocaine Use Residing in Inner-City Baltimore, Md., USA. Cerebrovasc. Dis. 2012, 21287, 295–301. [Google Scholar] [CrossRef]
- Labounty, T.M.; Hardy, W.D.; Fan, Z.; Yumul, R.; Li, D.; Dharmakumar, R.; Conte, A.H. Carotid artery thickness is associated with chronic use of highly active antiretroviral therapy in patients infected with human immunode fi ciency virus: A 3.0 Tesla magnetic resonance imaging study. Br. HIV Assoc. 2016, 17, 516–523. [Google Scholar]
- Mee, T.C.; Aepfelbacher, J.; Krakora, R.; Chairez, C.; Kvaratskhelia, N.; Smith, B.; Sandfort, V.; Hadigan, C.; Morse, C.; Hammoud, D.A. Carotid magnetic resonance imaging in persons living with HIV and 10-year atherosclerotic cardiovascular disease risk score Short communication Carotid magnetic resonance imaging in persons living with HIV and 10-year atherosclerotic cardiovascular diseas. Antivir. Ther. 2018, 23, 695–698. [Google Scholar] [CrossRef]
- Rose, K.A.M.; Vera, J.H.; Drivas, P.; Banya, W.; Pennell, D.J.; Winston, A. Europe PMC Funders Group Atherosclerosis is evident in treated HIV-infected subjects with low cardiovascular risk by carotid cardiovascular magnetic resonance. J. Acquir. Immune Defic. Syndr. 2016, 71, 514–521. [Google Scholar] [CrossRef]
- Wasserman, B.A. Advanced Contrast-Enhanced MRI for Looking Beyond the Lumen to Predict Stroke Building a Risk Profile for Carotid Plaque. Stroke 2010, 41, 12–16. [Google Scholar] [CrossRef]
- Wasserman, B.A.; Wityk, R.J.; Iii, H.H.T.; Virmani, R. Low-Grade Carotid Stenosis Looking Beyond the Lumen With MRI. Stroke 2005, 36, 2504–2513. [Google Scholar] [CrossRef]
- Fayad, Z.A.; Fuster, V.; Fallon, J.T.; Jayasundera, T.; Worthley, S.G.; Helft, G.; Aguinaldo, J.G.; Badimon, J.J.; Sharma, S.K. Noninvasive In Vivo Human Coronary Artery Lumen and Wall Imaging Using Black-Blood Magnetic Resonance Imaging. Circulation 2000, 102, 506–510. [Google Scholar] [CrossRef]
- U-king-im, J.M.; Trivedi, R.A.; Sala, E.; Graves, M.J.; Higgins, N.J.; Cross, J.C.; Hollingworth, W.; Coulden, R.A.; Kirkpatrick, P.J.; Antoun, N.M.; et al. Evaluation of carotid stenosis with axial high-resolution black-blood MR imaging. Eur. Radiol. 2004, 14, 1154–1161. [Google Scholar] [CrossRef]
- Krishnamurthy, R.; Cheong, B.; Muthupillai, R. Tools for cardiovascular magnetic resonance imaging. Cardiovasc. Dis. Ther. 2014, 4, 104–125. [Google Scholar]
- Saam, T.; Habs, M.; Buchholz, M.; Schindler, A.; Bayer-karpinska, A.; Cyran, C.C.; Yuan, C.; Reiser, M.; Helck, A. Expansive arterial remodeling of the carotid arteries and its effect on atherosclerotic plaque composition and vulnerability: An in-vivo black-blood 3T CMR study in symptomatic stroke patients. J. Cardiovasc. Magn. Reson. 2016, 18, 11. [Google Scholar] [CrossRef]
- Al-Smadi, A.S.; Abdalla, R.N.; Elmokadem, A.H.; Shaibani, A.; Hurley, M.C.; Potts, M.B.; Jahromi, B.S.; Carroll, T.J.; Ansari, S.A. Diagnostic Accuracy of High-Resolution Black-Blood MRI in the Evaluation of Intracranial Large-Vessel Arterial Occlusions. Am. J. Neuroradiol. 2019, 40, 1–6. [Google Scholar] [CrossRef]
- Ripa, R.S.; Knudsen, A.; Hag, A.M.F.; Lebech, A.; Loft, A.; Sune, H. Feasibility of simultaneous PET/MR of the carotid artery: first clinical experience and comparison to PET/CT. Am. J. Nucl. Med. Mol. Imaging 2013, 3, 361–371. [Google Scholar]
- Floris-moore, M.A.; Fayad, Z.A.; Berman, J.W.; Schoenbaum, E.E.; Klein, R.S.; Weinshelbaum, K.B.; Fuster, V.; Howard, A.A.; Lo, Y.; Schecter, D. Association of HIV Viral Load with Monocyte Chemoattractant Protein-1 and Atherosclerosis Burden Measured by Magnetic Resonance Imaging. AIDS 2010, 23, 941–949. [Google Scholar] [CrossRef]
- Bai, X.; Lv, P.; Liu, K.; Li, Q.; Ding, J.; Qu, J.; Lin, J. 3D Black-Blood Luminal Angiography Derived from High-Resolution MR Vessel Wall Imaging in Detecting MCA Stenosis: A Preliminary Study. Am. J. Neuroradiol. 2018, 39, 1827–1832. [Google Scholar] [CrossRef]
- Eiden, S.; Beck, C.; Venhoff, N.; Elsheikh, S.; Id, G.I.; Urbach, H.; Id, S.M. High-resolution contrast-enhanced vessel wall imaging in patients with suspected cerebral vasculitis: Prospective comparison of whole-brain 3D T1 SPACE versus 2D T1 black blood MRI at 3 Tesla. PLoS Med. 2019, 14, 1–14. [Google Scholar] [CrossRef]
- Takano, K.; Hida, K.; Iwaasa, M. Three-Dimensional Spin-Echo-Based Black-Blood MRA in the Detection of Vasospasm Following Subarachnoid Hemorrhage. J. Magn. Reson. Imging 2018, 49, 800–887. [Google Scholar] [CrossRef]
- Suri, M.; Qiao, Y.; Ma, X.; Guallar, E.; Zhou, J.; Zhang, Y.; Liu, L.; Chu, H.; Qureshi, A.I.; Alonso, A.; et al. Prevalence of Intracranial Atherosclerotic Stenosis Using High-Resolution Magnetic Resonance Angiography in the General Population The Atherosclerosis Risk in Communities Study. Stroke 2016, 47, 1187–1193. [Google Scholar] [CrossRef]
- Dearborn, J.L.; Zhang, Y.; Qiao, Y.; Suri, M.F.; Liu, L.; Gottesman, R.F.; Rawlings, A.M.; Mosley, T.H.; Alonso, A.; Knopman, D.S.; et al. Intracranial atherosclerosis and dementia The Atherosclerosis Risk in Communities ( ARIC ) Study. Neurology 2017, 88, 1556–1563. [Google Scholar] [CrossRef]
- Jiemy, F.W.; Heeringa, P.; Kamps, J.A.A.M.; van der Laken, C.J.; Slart, R.H.J.A.; Brouwer, E. Positron emission tomography (PET) and single photon emission computed tomography (SPECT) imaging of macrophages in large vessel vasculitis: Current status and future prospects. Autoimmun. Rev. 2018, 17, 715–726. [Google Scholar] [CrossRef]
- Longenecker, C.T.; Sullivan, C.E.; Morrison, J.; Hileman, C.O.; Zidar, D.A.; Gilkeson, R.; O’Donnell, J.; Mc Comsey, G.A. The effects of HIV and smoking on aortic and splenic inflammation. AIDS 2019, 32, 89–94. [Google Scholar] [CrossRef]
- Lawal, I.O.; Ankrah, A.O.; Popoola, G.O. Arterial inflammation in young patients with human immunodeficiency virus infection: A cross-sectional study using F-18 FDG PET/CT. J. Nucl. Cardiol. 2018. [Google Scholar] [CrossRef]
- Zanni, M.V.; Toribio, M.; Robbins, G.K.; Burdo, T.H.; Lu, M.T.; Ishai, A.E.; Feldpausch, M.N.; Martin, A.; Melbourne, K.; Triant, V.A.; et al. Effects of Antiretroviral Therapy on Immune Function and Arterial Inflammation in Treatment-Naive Patients With Human Immunodeficiency Virus Infection. JAMA Cardiol. 2016, 1, 474–480. [Google Scholar] [CrossRef]
- Lo, J.; Lu, M.T.; Ihenachor, E.J.; Wei, J.; Looby, S.E.; Fitch, K.V.; Oh, J.; Zimmerman, C.O.; Hwang, J.; Abbara, S.; et al. Effects of Statin Therapy on Coronary Artery Plaque Volume and High Risk Plaque Morphology in HIV-Infected Patients with Subclinical Atherosclerosis: a Randomized Double-Blind Placebo-Controlled Trial. Lancet HIV 2016, 2, e52–e63. [Google Scholar] [CrossRef]
- Knudsen, A.; Fisker, M.; Loft, A.; Lebech, A.; Ripa, S. HIV infection and arterial inflammation assessed by 18 F-fluorodeoxyglucose (FDG) positron emission tomography (PET): A prospective cross-sectional study. J. Nucl. Cardiol. 2015, 22, 372–380. [Google Scholar] [CrossRef]
- Tawakol, A.; Lo, J.; Zanni, M.; Marmarelis, E.; Ihenachor, E.; MacNabb, M.; Wai, B.; Hoffmann, U.; Abbara, S.; Grinspoon, S. Increased Arterial Inflammation Relates to High-risk Coronary Plaque Morphology in HIV-Infected Patients. J. Acquir. Immune Defic. Syndr. 2015, 66, 164–171. [Google Scholar] [CrossRef]
- Yarasheski, K.E.; Laciny, E.; Overton, E.T.; Reeds, D.N.; Harrod, M.; Baldwin, S.; Dávila-román, V.G. 18FDG PET-CT PET-CT imaging detects arterial inflammation and early atherosclerosis in HIV-infected adults with cardiovascular disease risk factors. J. Inflamm. 2012, 9, 1–9. [Google Scholar] [CrossRef]
- Subramanian, S.; Tawakol, A.; Burdo, T.H.; Wei, J.; Corsini, E.; Hoffmann, U.; Williams, K.C.; Lo, J.; Grinspoon, S.K. Arterial Inflammation in Patients With HIV. JAMA 2012, 308, 379–386. [Google Scholar] [CrossRef]
- Mhlanga, J.C.; Durand, D.; Tsai, H.-L.; Durand, C.M.; Leal, J.P.; Wang, H.; Moore, R.; Wahl, R.L. Differentiation of HIV-associated lymphoma from HIV-associated reactive adenopathy using quantitative FDG PET and symmetry. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 596–604. [Google Scholar] [CrossRef]
- Esmail, H.; Lai, R.P.; Lesosky, M.; Wilkinson, K.A.; Graham, C.M.; Coussens, A.K.; Oni, T. Europe PMC Funders Group Characterization of progressive HIV-associated tuberculosis using 2-deoxy-2-[18F] fluoro-D-glucose positron emission and computed tomography. Nat. Med. 2017, 22, 1090–1093. [Google Scholar] [CrossRef]
- Hammoud, D.A.; Boulougoura, A.; Papadakis, G.Z.; Wang, J.; Dodd, L.E.; Rupert, A.; Higgins, J.; Roby, G.; Metzger, D.; Laidlaw, E.; et al. Increased Metabolic Activity on 18 F-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography in Human Immunodeficiency Virus-Associated Immune Reconstitution Inflammatory Syndrome. Clin. Infect. Dis. 2019, 68, 229–238. [Google Scholar] [CrossRef]
- Hammoud, D.A.; Sinharay, S.; Steinbach, S.; Wakim, P.G. Global and regional brain hypometabolism on FDG-PET in treated HIV-infected individuals. Neurology 2018, 91, 1–12. [Google Scholar] [CrossRef]
- Schreiber-stainthorp, W.; Sinharay, S.; Srinivasula, S.; Shah, S.; Wang, J.; Dodd, L.; Lane, H.C.; Di Mascio, M.; Hammoud, D.A. Brain 18F-FDG PET of SIV-infected macaques after treatment interruption or initiation. J. Neuroinflammation 2018, 15, 1–9. [Google Scholar] [CrossRef]
- Obel, N.; Omland, L.H.; Kronborg, G.; Larsen, C.S.; Pedersen, C.; Pedersen, G.; Sørensen, H.T.; Gerstoft, J. Impact of Non-HIV and HIV risk factors on survival in HIV-Infected patients on HAART: A Population-Based nationwide cohort study. PLoS ONE 2011, 6, 5–10. [Google Scholar] [CrossRef]
- Gueler, A.; Moser, A.; Calmy, A.; Günthard, H.F.; Bernasconi, E.; Furrer, H.; Fux, C.A.; Battegay, M.; Cavassini, M.; Vernazza, P.; et al. Life expectancy in HIV-positive persons in Switzerland: Matched comparison with general population. AIDS 2017, 31, 427–436. [Google Scholar] [CrossRef]
- Mangili, A.; Gerrior, J.; Tang, A.M.; Leary, D.H.O.; Polak, J.K.; Schaefer, E.J.; Gorbach, S.L.; Wanke, C.A. Risk of Cardiovascular Disease in a Cohort of HIV-Infected Adults: A Study Using Carotid Intima-Media Thickness and Coronary Artery Calcium Score. Clin. Infect. Dis. 2006, 43, 1482–1489. [Google Scholar] [CrossRef]
- Hsue, P.Y.; Ordovas, K.; Lee, T.; Reddy, G.; Gotway, M.; Schnell, A.; Ho, J.E.; Selby, V.; Madden, E.; Martin, J.N.; et al. Carotid Intima-Media Thickness Among Human Immunodeficiency Virus-Infected Patients Without Coronary Calcium. Am. J. Cardiol. 2012, 109, 742–747. [Google Scholar] [CrossRef]
- Andreini, D. Screening CT Angiography in Asymptomatic Diabetes Mellitus? JACC Cardiovasc. Imaging 2016, 9, 1301–1303. [Google Scholar] [CrossRef]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. [2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC)]. Eur. Heart J. 2016, 37, 267–315. [Google Scholar]
- The SCOT Heart Investigators Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N. Engl. J. Med. 2018, 379, 924–933. [CrossRef]
- Hoffmann, U.; Udelson, J.E. Imaging Coronary Anatomy and Reducing Myocardial Infarction. N. Engl. J. Med. 2018, 379, 977–978. [Google Scholar] [CrossRef]
- Ryan, T.; Affandi, J.S.; Gahungu, N.; Dwivedi, G. Noninvasive Cardiovascular Imaging: Emergence of a Powerful Tool for Early Identification of Cardiovascular Risk in People Living With HIV. Can. J. Cardiol. 2019, 35, 260–269. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schoepf, I.C.; Buechel, R.R.; Kovari, H.; Hammoud, D.A.; Tarr, P.E. Subclinical Atherosclerosis Imaging in People Living with HIV. J. Clin. Med. 2019, 8, 1125. https://doi.org/10.3390/jcm8081125
Schoepf IC, Buechel RR, Kovari H, Hammoud DA, Tarr PE. Subclinical Atherosclerosis Imaging in People Living with HIV. Journal of Clinical Medicine. 2019; 8(8):1125. https://doi.org/10.3390/jcm8081125
Chicago/Turabian StyleSchoepf, Isabella C., Ronny R. Buechel, Helen Kovari, Dima A. Hammoud, and Philip E. Tarr. 2019. "Subclinical Atherosclerosis Imaging in People Living with HIV" Journal of Clinical Medicine 8, no. 8: 1125. https://doi.org/10.3390/jcm8081125
APA StyleSchoepf, I. C., Buechel, R. R., Kovari, H., Hammoud, D. A., & Tarr, P. E. (2019). Subclinical Atherosclerosis Imaging in People Living with HIV. Journal of Clinical Medicine, 8(8), 1125. https://doi.org/10.3390/jcm8081125




