Comparison of Bipolar Plasma Vaporization versus Standard Holmium Laser Enucleation of the Prostate: Surgical Procedures and Clinical Outcomes for Small Prostate Volumes
Abstract
:1. Introduction
2. Patients and Methods
2.1. Ethics Statement
2.2. Study Enrollment
2.3. Study Endpoints
2.4. Surgical Intervention
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Trueman, P.; Hood, S.C.; Nayak, U.S.; Mrazek, M.F. Prevalence of lower urinary tract symptoms and self-reported diagnosed’benign prostatic hyperplasia’, and their effect on quality of life in a community-based survey of men in the UK. BJU Int. 1999, 83, 410–415. [Google Scholar] [CrossRef] [PubMed]
- McVary, K.T.; Roehrborn, C.G.; Avins, A.L.; Barry, M.J.; Bruskewitz, R.C.; Donnell, R.F.; Foster, H.E., Jr.; Gonzalez, C.M.; Kaplan, S.A.; Penson, D.F.; et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J. Urol. 2011, 185, 1793–1803. [Google Scholar] [CrossRef] [PubMed]
- Oelke, M.; Bachmann, A.; Descazeaud, A.; Emberton, M.; Gravas, S.; Michel, M.C.; N’dow, J.; Nordling, J.; de la Rosette, J.J. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur. Urol. 2013, 64, 118–140. [Google Scholar] [CrossRef] [PubMed]
- Michalak, J.; Tzou, D.; Funk, J. HoLEP: The gold standard for the surgical management of BPH in the 21(st) Century. Am. J. Clin. Exp. Urol. 2015, 3, 36–42. [Google Scholar] [PubMed]
- Cornu, J.N.; Ahyai, S.; Bachmann, A.; de la Rosette, J.; Gilling, P.; Gratzke, C.; McVary, K.; Novara, G.; Woo, H.; Madersbacher, S. A Systematic Review and Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Obstruction: An Update. Eur. Urol. 2015, 67, 1066–1096. [Google Scholar] [CrossRef] [PubMed]
- Fayad, A.S.; Sheikh, M.G.; Zakaria, T.; Elfottoh, H.A.; Alsergany, R. Holmium laser enucleation versus bipolar resection of the prostate: A prospective randomized study. Which to choose? J. Endourol. 2011, 25, 1347–1352. [Google Scholar] [CrossRef] [PubMed]
- Rai, P.; Srivastava, A.; Dhayal, I.R.; Singh, S. Comparison of Safety, Efficacy and Cost Effectiveness of Photoselective Vaporization with Bipolar Vaporization of Prostate in Benign Prostatic Hyperplasia. Curr. Urol. 2018, 11, 103–109. [Google Scholar] [CrossRef]
- Cho, K.J.; Kim, H.S.; Koh, J.S.; Han, S.B.; Kim, S.H.; Kim, H.W.; Cho, S.Y.; Kim, J.C. Preoperative factors affecting postoperative early quality of life during the learning curve of holmium laser enucleation of the prostate. Int. Neurourol. J. 2013, 17, 83–89. [Google Scholar] [CrossRef]
- Madersbacher, S.; Klingler, H.C.; Djavan, B.; Stulnig, T.; Schatzl, G.; Schmidbauer, C.P.; Marberger, M. Is obstruction predictable by clinical evaluation in patients with lower urinary tract symptoms? Br. J. Urol. 1997, 80, 72–77. [Google Scholar] [CrossRef]
- Rosier, P.F.; de la Rosette, J.J.; Wijkstra, H.; Van Kerrebroeck, P.E.; Debruyne, F.M. Is detrusor instability in elderly males related to the grade of obstruction? Neurourol. Urodyn. 1995, 14, 625–633. [Google Scholar] [CrossRef]
- Kaplan, S.A.; McConnell, J.D.; Roehrborn, C.G.; Meehan, A.G.; Lee, M.W.; Noble, W.R.; Kusek, J.W.; Nyberg, L.M., Jr.; Medical Therapy of Prostatic Symptoms (MTOPS) Research Group. Combination therapy with doxazosin and finasteride for benign prostatic hyperplasia in patients with lower urinary tract symptoms and a baseline total prostate volume of 25 mL or greater. J. Urol. 2006, 175, 217–220. [Google Scholar] [CrossRef]
- Seckiner, I.; Yesilli, C.; Akduman, B.; Altan, K.; Mungan, N.A. A prospective randomized study for comparing bipolar plasmakinetic resection of the prostate with standard TURP. Urol. Int. 2006, 76, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.S.; Yip, S.K.; Lim, K.B.; Fook, S.; Foo, K.T.; Cheng, C.W. A prospective randomized study comparing monopolar and bipolar transurethral resection of prostate using transurethral resection in saline (TURIS) system. Eur. Urol. 2007, 52, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Erturhan, S.; Erbagci, A.; Seckiner, I.; Yagci, F.; Ustun, A. Plasmakinetic resection of the prostate versus standard transurethral resection of the prostate: A prospective randomized trial with 1-year follow-up. Prostate Cancer Prostatic Dis. 2007, 10, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Neill, M.G.; Gilling, P.J.; Kennett, K.M.; Frampton, C.M.; Westenberg, A.M.; Fraundorfer, M.R.; Wilson, L.C. Randomized trial comparing holmium laser enucleation of prostate with plasmakinetic enucleation of prostate for treatment of benign prostatic hyperplasia. Urology 2006, 68, 1020–1024. [Google Scholar] [CrossRef] [PubMed]
- Autorino, R.; Damiano, R.; Di Lorenzo, G.; Quarto, G.; Perdonà, S.; D’Armiento, M.; De Sio, M. Four-year outcome of a prospective randomised trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Eur. Urol. 2009, 55, 922–931. [Google Scholar] [CrossRef]
- Chen, Q.; Zhang, L.; Fan, Q.L.; Zhou, J.; Peng, Y.B.; Wang, Z. Bipolar transurethral resection in saline vs. traditional monopolar resection of the prostate: Results of a randomized trial with a 2-year follow-up. BJU Int. 2010, 106, 339–343. [Google Scholar] [CrossRef]
- Tefekli, A.; Muslumanoglu, A.Y.; Baykal, M.; Binbay, M.; Tas, A.; Altunrende, F. A hybrid technique using bipolar energy in transurethral prostate surgery: A prospective, randomized comparison. J. Urol. 2005, 174, 1339–1343. [Google Scholar] [CrossRef]
- Fagerström, T.; Nyman, C.R.; Hahn, R.G. Bipolar transurethral resection of the prostate causes less bleeding than the monopolar technique: A single-centre randomized trial of 202 patients. BJU Int. 2010, 105, 1560–1564. [Google Scholar] [CrossRef]
- Reich, O.; Schlenker, B.; Gratzke, C.; Tilki, D.; Riecken, M.; Stief, C.; Seitz, M.; Bachmann, A. Plasma vaporisation of the prostate: Initial clinical results. Eur. Urol. 2010, 57, 693–698. [Google Scholar] [CrossRef]
- Botto, H.; Lebret, T.; Barré, P.; Orsoni, J.L.; Hervé, J.M.; Lugagne, P.M. Electrovaporization of the prostate with the Gyrus device. J. Endourol. 2001, 15, 313–316. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.H.; Tsai, T.H.; Lee, S.S.; Kuo, Y.H.; Hsieh, T. Maximum Urine Flow Rate of Less than 15mL/Sec Increasing Risk of Urine Retention and Prostate Surgery among Patients with Alpha-1 Blockers: A 10-Year Follow Up Study. PLoS ONE 2016, 11, e0160689. [Google Scholar] [CrossRef] [PubMed]
| BPVP (n = 31) | HoLEP (n = 32) | p-Value | |
|---|---|---|---|
| Age | 69.81 ± 7.54 | 70.23 ± 5.61 | 0.803 |
| Prostate size (g) | 37.04 ± 29.41 | 36.01 ± 25.78 | 0.481 |
| Transitional zone volume (mL) | 12.3 ± 15.37 | 13.62 ± 18.22 | 0.497 |
| PSA (ng/mL) | 2.11 ± 6.38 | 2.18 ± 6.13 | 0.965 |
| Total IPSS | 20.7 ± 8.1 | 21.8 ± 8.5 | 0.241 |
| Voiding IPSS | 12.7 ± 4.9 | 14.3 ± 5.7 | 0.057 |
| Storage IPSS | 8.5 ± 4.4 | 9.0 ± 5.3 | 0.941 |
| IPSS QoL | 4.5 ± 2.8 | 5.1 ± 1.8 | 0.641 |
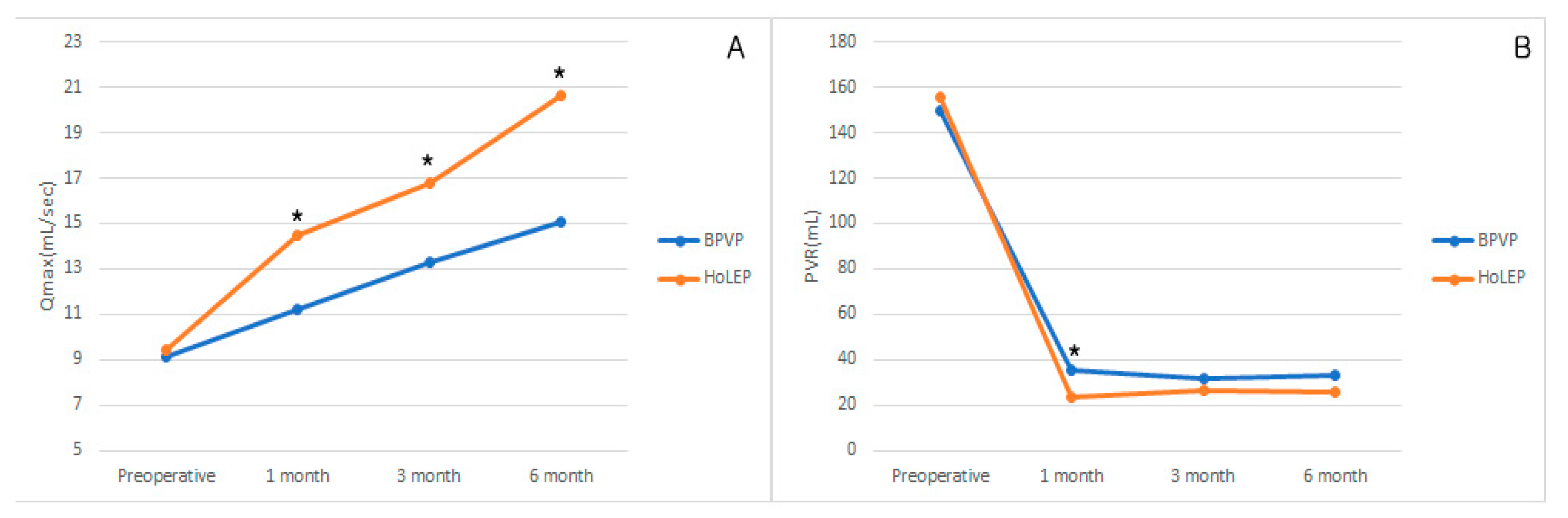
| Qmax (mL/s) | 9.09 ± 2.37 | 9.45 ± 3.59 | 0.447 |
| PVR (mL) | 149.8 ± 68.1 | 155.7 ± 104.9 | 0.119 |
| BPVP (n = 31) | HoLEP (n = 32) | p-Value | |
|---|---|---|---|
| Operation time (min) | 69.81 ± 7.54 | 70.23 ± 5.61 | 0.803 |
| Hemoglobin change | 47.04 ± 29.41 | 52.01 ± 25.78 | 0.481 |
| Vaporization/Enucleation time (min) | 22.3 ± 15.37 | 28.62 ± 18.22 | 0.497 |
| Morcellation time (min) | 3.18 ± 6.13 | ||
| Enucleation weight (g) | 11.8 ± 8.5 | ||
| Capsular perforation (case) | 1 (3.2%) | 4 (12.5%) | 0.173 |
| Hospital stay (day) | 2.1 ± 1.9 | 4.1 ± 1.3 | 0.001 * |
| Catheterization period (h) | 25.7 ± 2.1 | 51.1 ± 1.4 | 0.001 * |
| BPVP (n = 31) | HoLEP (n = 32) | p-Value | |
|---|---|---|---|
| Grade 1 | |||
| Clot retention | 0 | 4 | 0.113 |
| Mild to moderate dysuria | 4 | 2 | 0.164 |
| Re-catheterization | 1 | 3 | 0.317 |
| Grade 2 | |||
| Blood transfusion | 0 | 2 | 0.157 |
| Febrile UTI | 1 | 1 | 0.982 |
| Grade 3 | |||
| Bleeding requiring surgery | 0 | 2 | 0.157 |
| Preoperative | Postoperative | ||||
|---|---|---|---|---|---|
| 1 month | 3 months | 6 months | |||
| IPSS total | BPVP | 20.7 ± 8.1 | 11.6 ± 8.3 | 9.8 ± 4.1 | 8.1 ± 3.5 |
| HoLEP | 21.8 ± 8.5 | 11.5 ± 7.2 | 9.3 ± 5.1 | 8.4 ± 5.4 | |
| p-value | 0.241 | 0.098 | 0.184 | 0.217 | |
| IPSS voiding | BPVP | 12.7 ± 4.9 | 4.6 ± 4.3 | 4.0 ± 4.1 | 3.8 ± 3.5 |
| HoLEP | 14.3 ± 5.7 | 4.8 ± 4.9 | 3.8 ± 3.2 | 3.5 ± 3.3 | |
| p-value | 0.057 | 0.083 | 0.126 | 0.159 | |
| IPSS storage | BPVP | 8.5 ± 4.4 | 6.4 ± 3.1 | 5.8 ± 4.1 | 4.1 ± 3.5 |
| HoLEP | 9.0 ± 5.3 | 6.6 ± 3.2 | 5.7 ± 4.4 | 4.3 ± 3.4 | |
| p-value | 0.941 | 0.541 | 0.499 | 0.287 | |
| QoL score | BPVP | 4.5 ± 2.8 | 2.6 ± 1.7 | 2.3 ± 1.6 | 2.1 ± 1.5 |
| HoLEP | 5.1 ± 1.8 | 2.7 ± 1.4 | 2.4 ± 1.4 | 2.3 ± 1.5 | |
| p-value | 0.641 | 0.241 | 0.497 | 0.481 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.S.; Lee, S.H.; Cho, H.J.; Suh, H.J.; Lee, D.H.; Choi, Y.S. Comparison of Bipolar Plasma Vaporization versus Standard Holmium Laser Enucleation of the Prostate: Surgical Procedures and Clinical Outcomes for Small Prostate Volumes. J. Clin. Med. 2019, 8, 1007. https://doi.org/10.3390/jcm8071007
Kim KS, Lee SH, Cho HJ, Suh HJ, Lee DH, Choi YS. Comparison of Bipolar Plasma Vaporization versus Standard Holmium Laser Enucleation of the Prostate: Surgical Procedures and Clinical Outcomes for Small Prostate Volumes. Journal of Clinical Medicine. 2019; 8(7):1007. https://doi.org/10.3390/jcm8071007
Chicago/Turabian StyleKim, Kang Sup, Sung Hyun Lee, Hyuk Jin Cho, Hong Jin Suh, Dong Hwan Lee, and Yong Sun Choi. 2019. "Comparison of Bipolar Plasma Vaporization versus Standard Holmium Laser Enucleation of the Prostate: Surgical Procedures and Clinical Outcomes for Small Prostate Volumes" Journal of Clinical Medicine 8, no. 7: 1007. https://doi.org/10.3390/jcm8071007
APA StyleKim, K. S., Lee, S. H., Cho, H. J., Suh, H. J., Lee, D. H., & Choi, Y. S. (2019). Comparison of Bipolar Plasma Vaporization versus Standard Holmium Laser Enucleation of the Prostate: Surgical Procedures and Clinical Outcomes for Small Prostate Volumes. Journal of Clinical Medicine, 8(7), 1007. https://doi.org/10.3390/jcm8071007





