Circulating Soluble CD36 is Similar in Type 1 and Type 2 Diabetes Mellitus versus Non-Diabetic Subjects
Abstract
1. Introduction
2. Experimental Section
2.1. Subjects
2.2. Determination for sCD36 by ELISA
2.3. Consistency Test of sCD36 Determination
2.4. Flow Cytometric Analysis
2.5. Real-Time PCR
2.6. Statistical Analyses
3. Results
3.1. Circulating sCD36 in the Study Groups
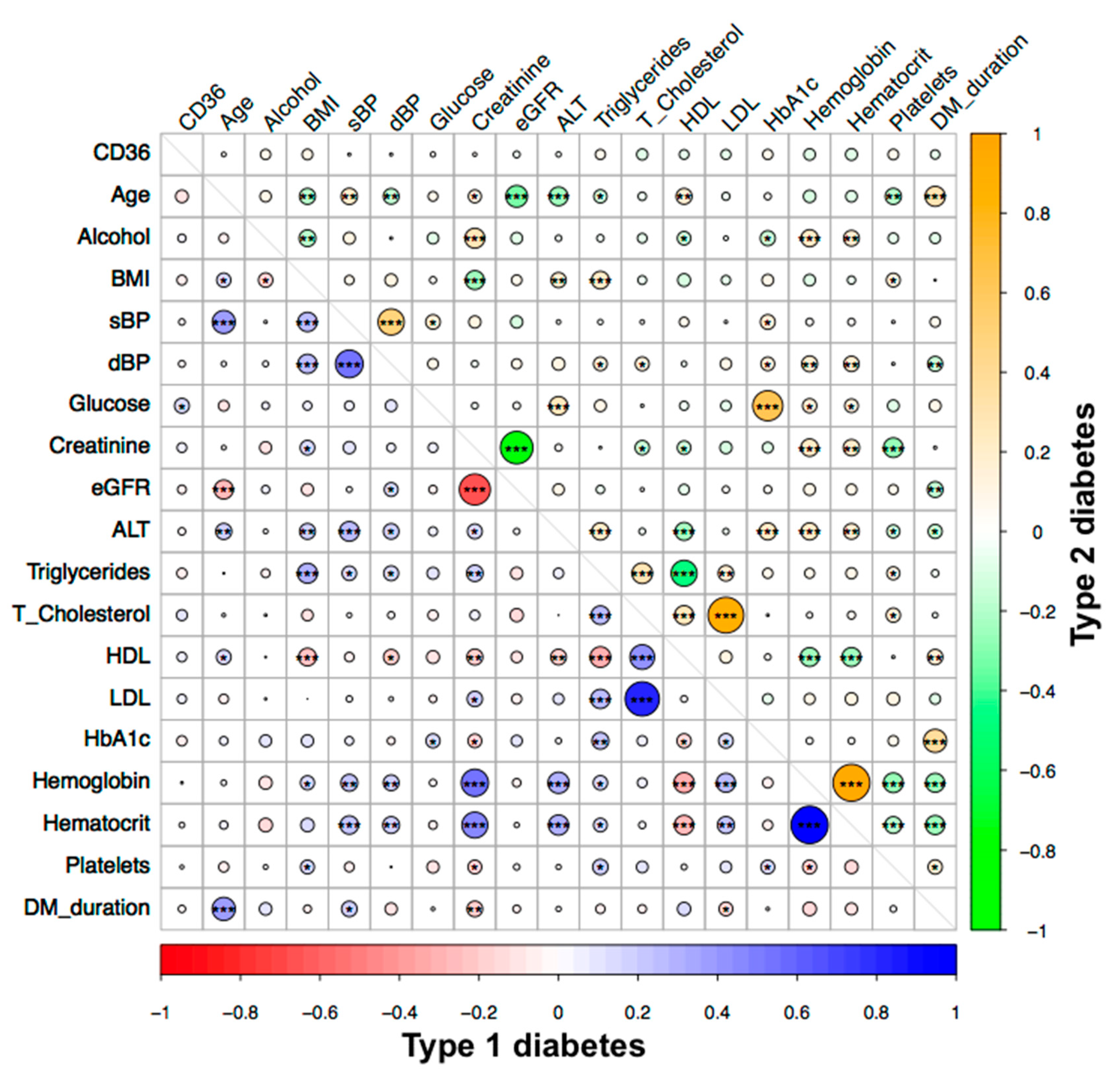
3.2. Associations of Circulating sCD36 in the Study Groups
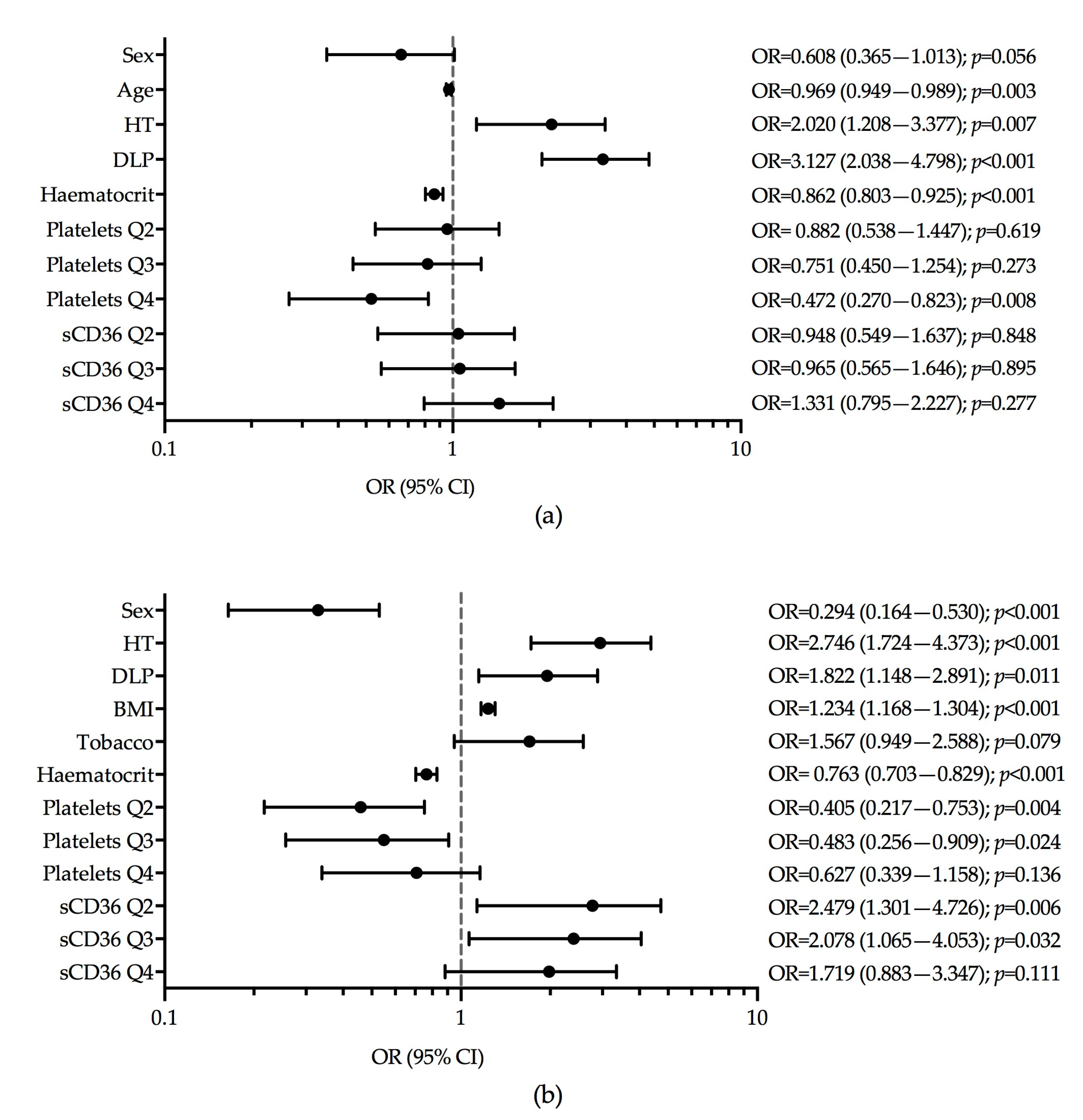
3.3. Multinomial Logistic Regression Models of sCD36
3.4. Association of sCD36 with Type 1 and Type 2 Diabetes
3.5. Flow Cytometric Analysis of CD36 and Real-Time PCR
3.6. Consistency Test in sCD36 Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Silverstein, R.L.; Febbraio, M. CD36, a Scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci. Signal. 2009, 2, re3. [Google Scholar] [CrossRef]
- Asch, A.S.; Barnwell, J.; Silverstein, R.L.; Nachman, R.L. Isolation of the thrombospondin membrane receptor. J. Clin. Investig. 1987, 79, 1054–1061. [Google Scholar] [CrossRef]
- Hoebe, K.; Georgel, P.; Rutschmann, S.; Du, X.; Mudd, S.; Crozat, K.; Sovath, S.; Shamel, L.; Hartung, T.; Zähringer, U.; et al. CD36 is a sensor of diacylglycerides. Nature 2005, 433, 523–527. [Google Scholar] [CrossRef]
- Mikołajczyk, T.P.; Skrzeczyńska-Moncznik, J.E.; Zarębski, M.A.; Marewicz, E.A.; Wiśniewska, A.M.; Dzięba, M.; Dobrucki, J.W.; Pryjma, J.R. Interaction of human peripheral blood monocytes with apoptotic polymorphonuclear cells. Immunology 2009, 128, 103–113. [Google Scholar] [CrossRef]
- Endemann, G.; Stanton, L.W.; Madden, K.S.; Bryant, C.M.; White, R.T.; Protter, A.A. CD36 is a receptor for oxidized low density lipoprotein. J. Biol. Chem. 1993, 268, 11811–11816. [Google Scholar] [PubMed]
- Ibrahimi, A.; Abumrad, N.A. Role of CD36 in membrane transport of long-chain fatty acids. Curr. Opin. Clin. Nutr. Metab. Care 2002, 5, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Coburn, C.T.; Hajri, T.; Ibrahimi, A.; Abumrad, N.A. Role of CD36 in membrane transport and utilization of long-chain fatty acids by different tissues. J. Mol. Neurosci. 2001, 16, 117–121. [Google Scholar] [CrossRef]
- Collotteixeira, S.; Martin, J.; McDermottroe, C.; Poston, R.; McGregor, J. CD36 and macrophages in atherosclerosis. Cardiovasc. Res. 2007, 75, 468–477. [Google Scholar] [CrossRef]
- Febbraio, M.; Hajjar, D.P.; Silverstein, R.L. CD36: A class B scavenger receptor involved in angiogenesis, atherosclerosis, inflammation, and lipid metabolism. J. Clin. Invest. 2001, 108, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Febbraio, M.; Silverstein, R.L. CD36: Implications in cardiovascular disease. Int. J. Biochem. Cell Biol. 2007, 39, 2012–2030. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, A.C.; Han, J.; Febbraio, M.; Silverstein, R.L.; Hajjar, D.P. Role of CD36, the Macrophage Class B Scavenger Receptor, in Atherosclerosis. Ann. N. Y. Acad. Sci. 2001, 947, 224–228. [Google Scholar] [CrossRef]
- He, J.; Lee, J.H.; Febbraio, M.; Xie, W. The emerging roles of fatty acid translocase/CD36 and the aryl hydrocarbon receptor in fatty liver disease. Exp. Biol. Med. (Maywood) 2011, 236, 1116–1121. [Google Scholar] [CrossRef]
- Kennedy, D.J.; Kashyap, S.R. Pathogenic Role of Scavenger Receptor CD36 in the Metabolic Syndrome and Diabetes. Metab. Syndr. Relat. Disord. 2011, 9, 239–245. [Google Scholar] [CrossRef]
- Aitman, T.J.; Glazier, A.M.; Wallace, C.A.; Cooper, L.D.; Norsworthy, P.J.; Wahid, F.N.; Al-Majali, K.M.; Trembling, P.M.; Mann, C.J.; Shoulders, C.C.; et al. Identification of Cd36 (Fat) as an insulin-resistance gene causing defective fatty acid and glucose metabolism in hypertensive rats. Nat. Genet. 1999, 21, 76–83. [Google Scholar] [CrossRef]
- Griffin, E.; Re, A.; Hamel, N.; Fu, C.; Bush, H.; McCaffrey, T.; Asch, A.S. A link between diabetes and atherosclerosis: Glucose regulates expression of CD36 at the level of translation. Nat. Med. 2001, 7, 840–846. [Google Scholar] [CrossRef]
- Liang, C.P.; Han, S.; Okamoto, H.; Carnemolla, R.; Tabas, I.; Accili, D.; Tall, A.R. Increased CD36 protein as a response to defective insulin signaling in macrophages. J. Clin. Investig. 2004, 113, 764–773. [Google Scholar] [CrossRef]
- Sampson, M.J.; Davies, I.R.; Braschi, S.; Ivory, K.; Hughes, D.A. Increased expression of a scavenger receptor (CD36) in monocytes from subjects with Type 2 diabetes. Atherosclerosis 2003, 167, 129–134. [Google Scholar] [CrossRef]
- Kopprasch, S.; Pietzsch, J.; Kuhlisch, E.; Fuecker, K.; Temelkova-Kurktschiev, T.; Hanefeld, M.; Kühne, H.; Julius, U.; Graessler, J. In vivo evidence for increased oxidation of circulating LDL in impaired glucose tolerance. Diabetes 2002, 51, 3102–3106. [Google Scholar] [CrossRef]
- Hoogeveen, R.C.; Ballantyne, C.M.; Bang, H.; Heiss, G.; Duncan, B.B.; Folsom, A.R.; Pankow, J.S. Circulating oxidised low-density lipoprotein and intercellular adhesion molecule-1 and risk of type 2 diabetes mellitus: The Atherosclerosis Risk in Communities Study. Diabetologia 2007, 50, 36–42. [Google Scholar] [CrossRef][Green Version]
- Handberg, A.; Levin, K.; Levin, K.; Højlund, K.; Beck-Nielsen, H.; Beck-Nielsen, H. Identification of the oxidized low-density lipoprotein scavenger receptor CD36 in plasma: A novel marker of insulin resistance. Circulation 2006, 114, 1169–1176. [Google Scholar] [CrossRef]
- Handberg, A.; Lopez-Bermejo, A.; Bassols, J.; Vendrell, J.; Ricart, W.; Fernandez-Real, J.M. Circulating soluble CD36 is associated with glucose metabolism and interleukin-6 in glucose-intolerant men. Diabetes Vasc. Dis. Res. 2009, 6, 15–20. [Google Scholar] [CrossRef]
- Handberg, A.; Norberg, M.; Stenlund, H.; Hallmans, G.; Attermann, J.; Eriksson, J.W. Soluble CD36 (sCD36) Clusters with Markers of Insulin Resistance, and High sCD36 Is Associated with Increased Type 2 Diabetes Risk. J. Clin. Endocrinol. Metab. 2010, 95, 1939–1946. [Google Scholar] [CrossRef]
- Fernández-Real, J.M.; Handberg, A.; Ortega, F.; Højlund, K.; Vendrell, J.; Ricart, W. Circulating soluble CD36 is a novel marker of liver injury in subjects with altered glucose tolerance. J. Nutr. Biochem. 2009, 20, 477–484. [Google Scholar] [CrossRef]
- Alkhatatbeh, M.; Ayoub, N.; Mhaidat, N.; Saadeh, N.; Lincz, L. Soluble cluster of differentiation 36 concentrations are not associated with cardiovascular risk factors in middle-aged subjects. Biomed. Rep. 2016, 4, 1–7. [Google Scholar] [CrossRef]
- Krzystolik, A.; Dziedziejko, V.; Safranow, K.; Kurzawski, G.; Rać, M.; Sagasz-Tysiewicz, D.; Poncyljusz, W.; Jakubowska, K.; Chlubek, D.; Rać, M.E. Is plasma soluble CD36 associated with cardiovascular risk factors in early onset coronary artery disease patients? Scand. J. Clin. Lab. Investig. 2015, 75, 1–9. [Google Scholar] [CrossRef]
- Chmielewski, M.; Bragfors-Helin, A.C.; Stenvinkel, P.; Lindholm, B.; Anderstam, B. Serum soluble CD36, assessed by a novel monoclonal antibody-based sandwich ELISA, predicts cardiovascular mortality in dialysis patients. Clin. Chim. Acta 2010, 411, 2079–2082. [Google Scholar] [CrossRef]
- Carbonell, M.; Castelblanco, E.; Valldeperas, X.; Betriu, A.; Traveset, A.; Granado-Casas, M.; Hernández, M.; Vázquez, F.; Martín, M.; Rubinat, E.; et al. Diabetic retinopathy is associated with the presence and burden of subclinical carotid atherosclerosis in type 1 diabetes. Cardiovasc. Diabetol. 2018, 17, 1–10. [Google Scholar] [CrossRef]
- Alonso, N.; Traveset, A.; Rubinat, E.; Ortega, E.; Alcubierre, N.; Sanahuja, J.; Hernández, M.; Betriu, A.; Jurjo, C.; Fernández, E.; et al. Type 2 diabetes-associated carotid plaque burden is increased in patients with retinopathy compared to those without retinopathy. Cardiovasc. Diabetol. 2015, 14, 33–39. [Google Scholar] [CrossRef]
- Vilanova, M.B.; Falguera, M.; Marsal, J.; Rubinat, E.; Alcubierre, N.; Castelblanco, E.; Granado-Casas, M.; Miró, N.; Molló, A.; Mata-Cases, M.; et al. Prevalence, clinical features and risk assessment of pre-diabetes in Spain: The prospective Mollerussa cohort study. BMJ Open 2017, 7, e015158. [Google Scholar] [CrossRef]
- Lykkeboe, S.; Larsen, A.L.; Handberg, A. Lack of consistency between two commercial ELISAs and against an in-house ELISA for the detection of CD36 in human plasma. Clin. Chem. Lab. Med. 2012, 50, 1071–1074. [Google Scholar] [CrossRef]
- Petta, S.; Handberg, A.; Marchesini, G.; Cammà, C.; Di Marco, V.; Cabibi, D.; Macaluso, F.S.; Craxì, A. High sCD36 plasma level is associated with steatosis and its severity in patients with genotype 1 chronic hepatitis C. J. Viral Hepat. 2012, 20, 174–182. [Google Scholar] [CrossRef]
- Handberg, A.; Højlund, K.; Gastaldelli, A.; Flyvbjerg, A.; Dekker, J.M.; Petrie, J.; Piatti, P.; Beck-Nielsen, H. RISC Investigators; RISC Investigators Plasma sCD36 is associated with markers of atherosclerosis, insulin resistance and fatty liver in a nondiabetic healthy population. J. Intern. Med. 2012, 271, 294–304. [Google Scholar] [CrossRef]
- Rać, M.; Krzystolik, A.; Rać, M.; Safranow, K.; Dziedziejko, V.; Goschorska, M.; Poncyljusz, W.; Chlubek, D. Is plasma-soluble CD36 associated with density of atheromatous plaque and ankle-brachial index in early-onset coronary artery disease patients? Kardiol. Pol. 2016, 74, 570–575. [Google Scholar]
- Liani, R.; Halvorsen, B.; Sestili, S.; Handberg, A.; Santilli, F.; Vazzana, N.; Formoso, G.; Aukrust, P.; Davì, G. Plasma levels of soluble CD36, platelet activation, inflammation, and oxidative stress are increased in type 2 diabetic patients. Free Radic. Biol. Med. 2012, 52, 1318–1324. [Google Scholar] [CrossRef]
- Handberg, A.; Skjelland, M.; Michelsen, A.E.; Sagen, E.L.; Krohg-Sørensen, K.; Russell, D.; Dahl, A.; Ueland, T.; Oie, E.; Aukrust, P.; et al. Soluble CD36 in plasma is increased in patients with symptomatic atherosclerotic carotid plaques and is related to plaque instability. Stroke 2008, 39, 3092–3095. [Google Scholar] [CrossRef]
- Vinagre, I.; Mata-Cases, M.; Hermosilla, E.; Morros, R.; Fina, F.; Rosell, M.; Castell, C.; Franch-Nadal, J.; Bolíbar, B.; Mauricio, D. Control of Glycemia and Cardiovascular Risk Factors in Patients with Type 2 Diabetes in Primary Care in Catalonia (Spain). Diabetes Care 2012, 35, 774–779. [Google Scholar] [CrossRef]
- Park, Y.M.; Febbraio, M.; Silverstein, R.L. CD36 modulates migration of mouse and human macrophages in response to oxidized LDL and may contribute to macrophage trapping in the arterial intima. J. Clin. Investig. 2009, 119, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.J.; Kuchibhotla, S.; Westfall, K.M.; Silverstein, R.L.; Morton, R.E.; Febbraio, M. A CD36-dependent pathway enhances macrophage and adipose tissue inflammation and impairs insulin signalling. Cardiovasc. Res. 2011, 89, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Bernal-Lopez, R.M.; Llorente-Cortes, V.; López-Carmona, D.; Mayas, D.M.; Gomez-Huelgas, R.; Tinahones, F.J.; Badimon, L. Modulation of human monocyte CD36 by type 2 diabetes mellitus and other atherosclerotic risk factors. Eur. J. Clin. Investig. 2011, 41, 854–862. [Google Scholar] [CrossRef] [PubMed]
- Alkhatatbeh, M.J.; Enjeti, A.K.; Acharya, S.; Thorne, R.F.; Lincz, L.F. The origin of circulating CD36 in type 2 diabetes. Nutr. Diabetes 2013, 3, e59. [Google Scholar] [CrossRef]
- Lopez-Carmona, M.D.; Plaza-Seron, M.C.; Vargas-Candela, A.; Tinahones, F.J.; Gomez-Huelgas, R.; Bernal-Lopez, M.R. CD36 overexpression: A possible etiopathogenic mechanism of atherosclerosis in patients with prediabetes and diabetes. Diabetol. Metab. Syndr. 2017, 9, 55. [Google Scholar] [CrossRef] [PubMed]
- Alkhatatbeh, M.J.; Mhaidat, N.M.; Enjeti, A.K.; Lincz, L.F.; Thorne, R.F. The putative diabetic plasma marker, soluble CD36, is non-cleaved, non-soluble and entirely associated with microparticles. J. Thromb. Haemost. 2011, 9, 844–851. [Google Scholar] [CrossRef] [PubMed]
| Variables 1 | Control | T1D | T2D | p Value | p Control versus T1D | p Control versus T2D | p T1D versus T2D |
|---|---|---|---|---|---|---|---|
| N = 522 | N = 225 | N = 276 | |||||
| Sex, Men | 212 (40.6%) | 109 (48.4%) | 143 (51.8%) | 0.006 | 0.086 | 0.009 | 0.509 |
| Age, years | 49 (39–59) | 44 (38.0–51.0) | 59 (51–66) | <0.001 | <0.001 | <0.001 | <0.001 |
| BMI, Kg/m2 | 25.5 (23.4–28.3) | 25.6 (22.6–28.1) | 30.2 (27.9–34.7) | <0.001 | 0.557 | <0.001 | <0.001 |
| Waist, cm | 94.0 (85.0–102) | 88.0 (80.0–97.0) | 104 (97.5–112) | <0.001 | <0.001 | <0.001 | <0.001 |
| Alcohol mg/day | 2.86 (0–12.3) | 2.37 (0–7.19) | 1.53 (0–9.92) | 0.030 | 0.095 | 0.055 | 0.685 |
| Tobacco | 270 (51.7%) | 116 (51.6%) | 149 (54.0%) | 0.805 | 1.000 | 0.977 | 0.977 |
| Hypertension | 81 (16%) | 55 (24.4%) | 153 (55.4%) | <0.001 | 0.009 | <0.001 | <0.001 |
| sBP, mmHg | 121 (110–132) | 128 (116–138) | 139 (127–150) | <0.001 | <0.001 | <0.001 | <0.001 |
| dBP, mmHg | 76.0 (70–83) | 75.0 (68.5–80) | 76.0 (70–84) | 0.020 | 0.026 | 0.889 | 0.028 |
| Dyslipidaemia | 115 (22.6%) | 96 (42.7%) | 129 (46.7%) | <0.001 | <0.001 | <0.001 | 0.412 |
| Antiplatelet | - | 63 (28%) | 99 (35.9%) | <0.001 | - | - | 0.076 |
| Statins | 114 (22.4%) | 96 (42.7%) | 116 (42%) | <0.001 | <0.001 | <0.001 | 0.958 |
| Glucose, mg/dL | 90 (84–96) | 159 (107–208) | 148 (117–182) | <0.001 | <0.001 | <0.001 | 0.619 |
| HbA1c, % | 5.5 (5.2–5.8) | 7.40 (7.00–7.9) | 7.60 (6.80–8.5) | <0.001 | <0.001 | <0.001 | 0.230 |
| Creatinine mg/dL | 0.79 (0.70–0.93) | 0.78 (0.65–0.87) | 0.79 (0.68–0.93) | 0.011 | 0.009 | 0.567 | 0.046 |
| eGFR | 86.2 (77.4–97.6) | 95.2 (82.7–108) | 86.8 (77.5–100) | <0.001 | <0.001 | 0.383 | <0.001 |
| ALT U/L | 17 (13–23) | 17 (13.8–21) | 19 (16–28) | <0.001 | 0.719 | <0.001 | <0.001 |
| Triglycerides, mg/dL | 87 (67.0–125) | 65 (53–86) | 118 (84.8–166) | <0.001 | <0.001 | <0.001 | <0.001 |
| Total-C, mg/dL | 196 (175–226) | 180 (164–201) | 184 (163–206) | <0.001 | <0.001 | <0.001 | 0.180 |
| HDL, mg/dL | 57 (48–68) | 62.5 (53–74) | 48 (40–58) | <0.001 | <0.001 | <0.001 | <0.001 |
| LDL, mg/dL | 119 (100–142) | 101 (84.5–116) | 108 (88.4–129) | <0.001 | <0.001 | <0.001 | 0.003 |
| Haemoglobin, g/dL | 14.2 (13.3–15.2) | 14 (13.1–14.9) | 13.7 (12.9–14.7) | <0.001 | 0.031 | <0.001 | 0.098 |
| Haematocrit, % | 42.4 (3.58) | 41.5 (3.51) | 41.1 (3.54) | <0.001 | 0.003 | <0.001 | 0.545 |
| Platelets, 109/L | 233 (203–273) | 223 (197–256) | 226 (188–274) | 0.019 | 0.027 | 0.078 | 0.759 |
| Diabetes duration, years | - | 21 (15–29) | 8 (4–13.5) | <0.001 | - | - | <0.001 |
| sCD36, ng/mL | 2.84 (0.56–9.06) | 3.66 (0.69–18.7) | 2.62 (0.66–7.57) | 0.144 | 0.180 | 0.583 | 0.151 |
| sCD36 Quartiles 2 | 0.062 | 0.259 | 0.259 | 0.036 | |||
| (<−0.562) | 134 (25.7%) | 53 (23.6%) | 64 (23.2%) | ||||
| (−0.562,1.05) | 127 (24.3%) | 49 (21.8%) | 80 (29%) | ||||
| (1.05,2.24) | 133 (25.5%) | 51 (22.7%) | 77 (27.9%) | ||||
| (>2.24) | 128 (24.5%) | 72 (32.0%) | 55 (19.9%) |
| Variables | Whole Group | Control | T1D | T2D | |||||
|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | p-Value | Median (IQR) | p-Value | Median (IQR) | p-Value | Median (IQR) | p-Value | ||
| Sex | Men | 2.59 (0.48–8.51) | 0.089 | 2.36 (0.36–8.06) | 0.047 | 3.58 (0.69–27.9) | 0.812 | 2.15 (0.65–6.29) | 0.374 |
| Women | 3.37 (0.75–9.99) | 3.40 (0.74–10.3) | 3.69 (0.71–15.1) | 2.99 (0.82–8.28) | |||||
| Hypertension | No | 3.17 (0.69–10.9) | 0.024 | 3.23 (0.73–9.93) | 0.001 | 3.57 (0.70–20.7) | 0.751 | 2.29 (0.64–8.39) | 0.875 |
| Yes | 2.65 (0.48–7.17) | 1.04 (0.17–5.10) | 3.72 (0.68–8.79) | 2.83 (0.79–6.14) | |||||
| Dyslipidaemia | No | 3.09 (0.66–10.3) | 0.274 | 3.15 (0.69–10.0) | 0.044 | 4.53 (0.85–28.5) | 0.090 | 1.80 (0.48–6.95) | 0.048 |
| Yes | 2.79 (0.51–8.33) | 2.04 (0.26–7.80) | 2.75 (0.44–9.89) | 3.53 (1.01–7.95) | |||||
| Statins | No | 3.09 (0.66–10.1) | 0.247 | 3.15 (0.69–9.93) | 0.035 | 4.53 (0.84–23.7) | 0.145 | 1.88 (0.48–6.88) | 0.084 |
| Yes | 2.74 (0.48–8.32) | 2.01 (0.26–7.64) | 2.70 (0.42–13.1) | 3.54 (1.02–8.03) | |||||
| Obesity | No | 3.15 (0.65–10.2) | 0.130 | 3.12 (0.69–9.59) | 0.030 | 3.58 (0.65–24.4) | 0.644 | 2.51 (0.65–7.08) | 0.546 |
| Yes | 2.43 (0.53–7.59) | 1.70 (0.26–5.91) | 3.81 (0.84–10.4) | 2.73 (0.81–7.86) | |||||
| Tobacco | No | 3.68 (0.82–10.5) | 0.003 | 2.92 (0.64–9.58) | 0.321 | 6.38 (1.16–25.2) | 0.005 | 3.24 (0.94–8.58) | 0.176 |
| Yes | 2.55 (0.48–7.94) | 2.60 (0.48–8.17) | 2.37 (0.05–10.9) | 2.14 (0.65–6.38) | |||||
| Anti-platelet | No | 2.86 (0.56–9.55) | 0.393 | - | - | 4.29 (0.68–19.2) | 0.410 | 1.98 (0.48–6.81) | 0.039 |
| Yes | 3.27 (0.88–8.42) | - | 2.66 (0.73–17.8) | 3.59 (1.07–8.06) | |||||
| Diabetes | No | 2.84 (0.56–9.06) | 0.597 | - | - | - | - | - | - |
| Yes | 2.99 (0.67–9.52) | - | - | - | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castelblanco, E.; Sanjurjo, L.; Falguera, M.; Hernández, M.; Fernandez-Real, J.-M.; Sarrias, M.-R.; Alonso, N.; Mauricio, D. Circulating Soluble CD36 is Similar in Type 1 and Type 2 Diabetes Mellitus versus Non-Diabetic Subjects. J. Clin. Med. 2019, 8, 710. https://doi.org/10.3390/jcm8050710
Castelblanco E, Sanjurjo L, Falguera M, Hernández M, Fernandez-Real J-M, Sarrias M-R, Alonso N, Mauricio D. Circulating Soluble CD36 is Similar in Type 1 and Type 2 Diabetes Mellitus versus Non-Diabetic Subjects. Journal of Clinical Medicine. 2019; 8(5):710. https://doi.org/10.3390/jcm8050710
Chicago/Turabian StyleCastelblanco, Esmeralda, Lucía Sanjurjo, Mireia Falguera, Marta Hernández, José-Manuel Fernandez-Real, Maria-Rosa Sarrias, Nuria Alonso, and Didac Mauricio. 2019. "Circulating Soluble CD36 is Similar in Type 1 and Type 2 Diabetes Mellitus versus Non-Diabetic Subjects" Journal of Clinical Medicine 8, no. 5: 710. https://doi.org/10.3390/jcm8050710
APA StyleCastelblanco, E., Sanjurjo, L., Falguera, M., Hernández, M., Fernandez-Real, J.-M., Sarrias, M.-R., Alonso, N., & Mauricio, D. (2019). Circulating Soluble CD36 is Similar in Type 1 and Type 2 Diabetes Mellitus versus Non-Diabetic Subjects. Journal of Clinical Medicine, 8(5), 710. https://doi.org/10.3390/jcm8050710






