Exhalative Breath Markers Do Not Offer for Diagnosis of Interstitial Lung Diseases: Data from the European IPF Registry (eurIPFreg) and Biobank
Abstract
:1. Introduction
2. Experimental Section
2.1. Clinical and Lab Data Collection
2.2. Quality of Data and Statistical Analysis
3. Results
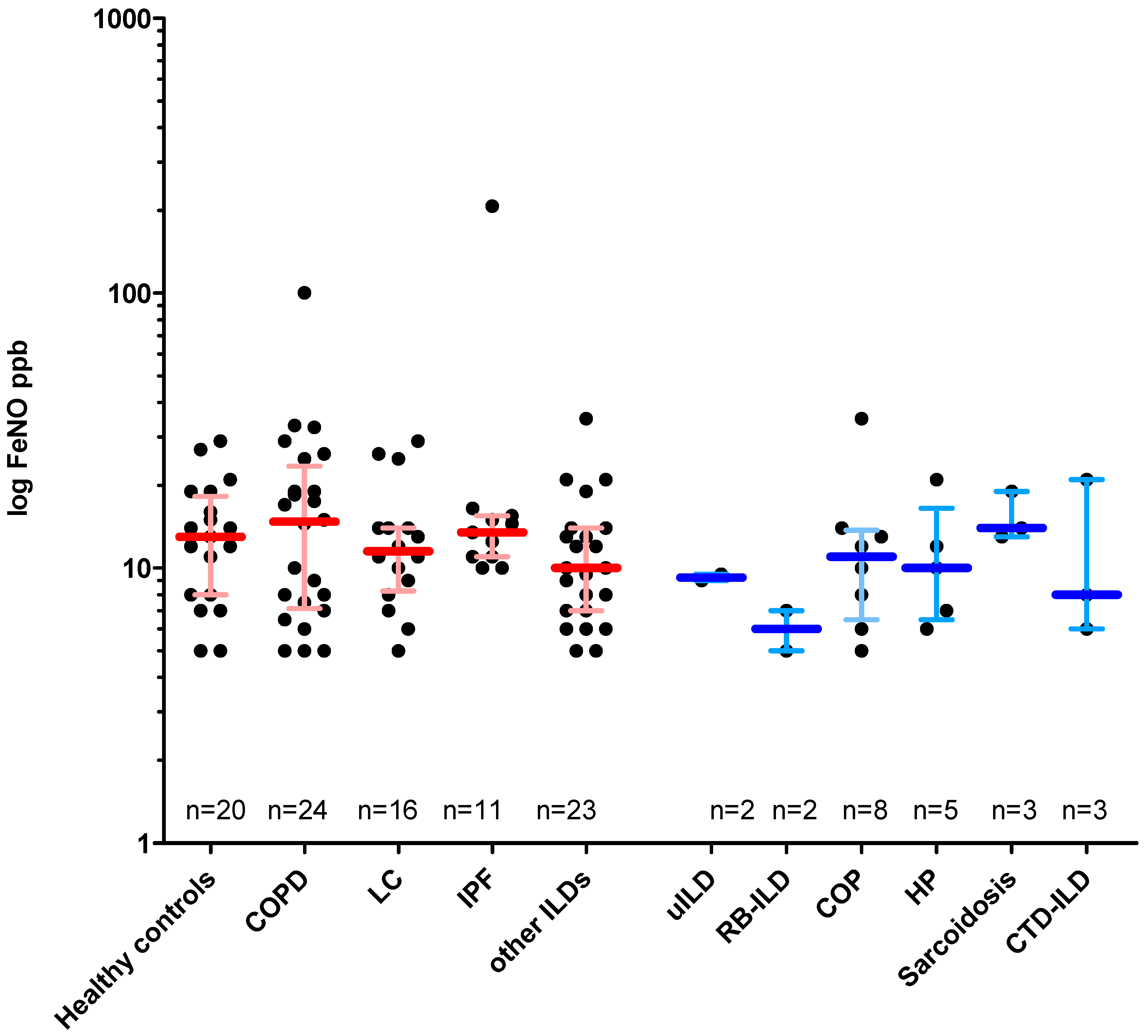
3.1. Disease-Specific FeNO Distribution and Correlation with Pulmonary Function Test (PFT) Values
3.2. Impact of Smoking Status and Medication on FeNO Measurements
3.3. Intraindividual FeNO Variability and FeNO Values in Exacerbation
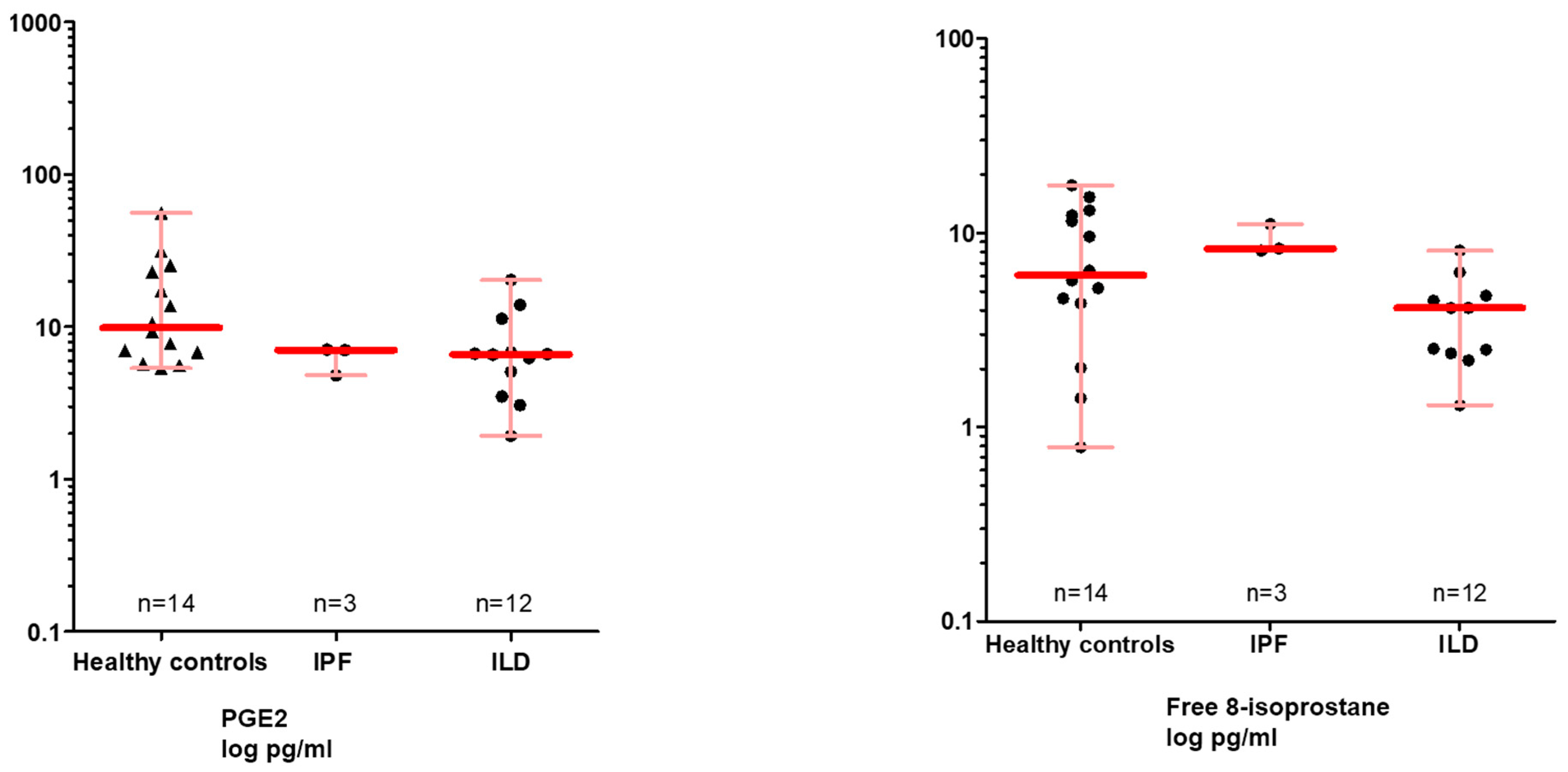
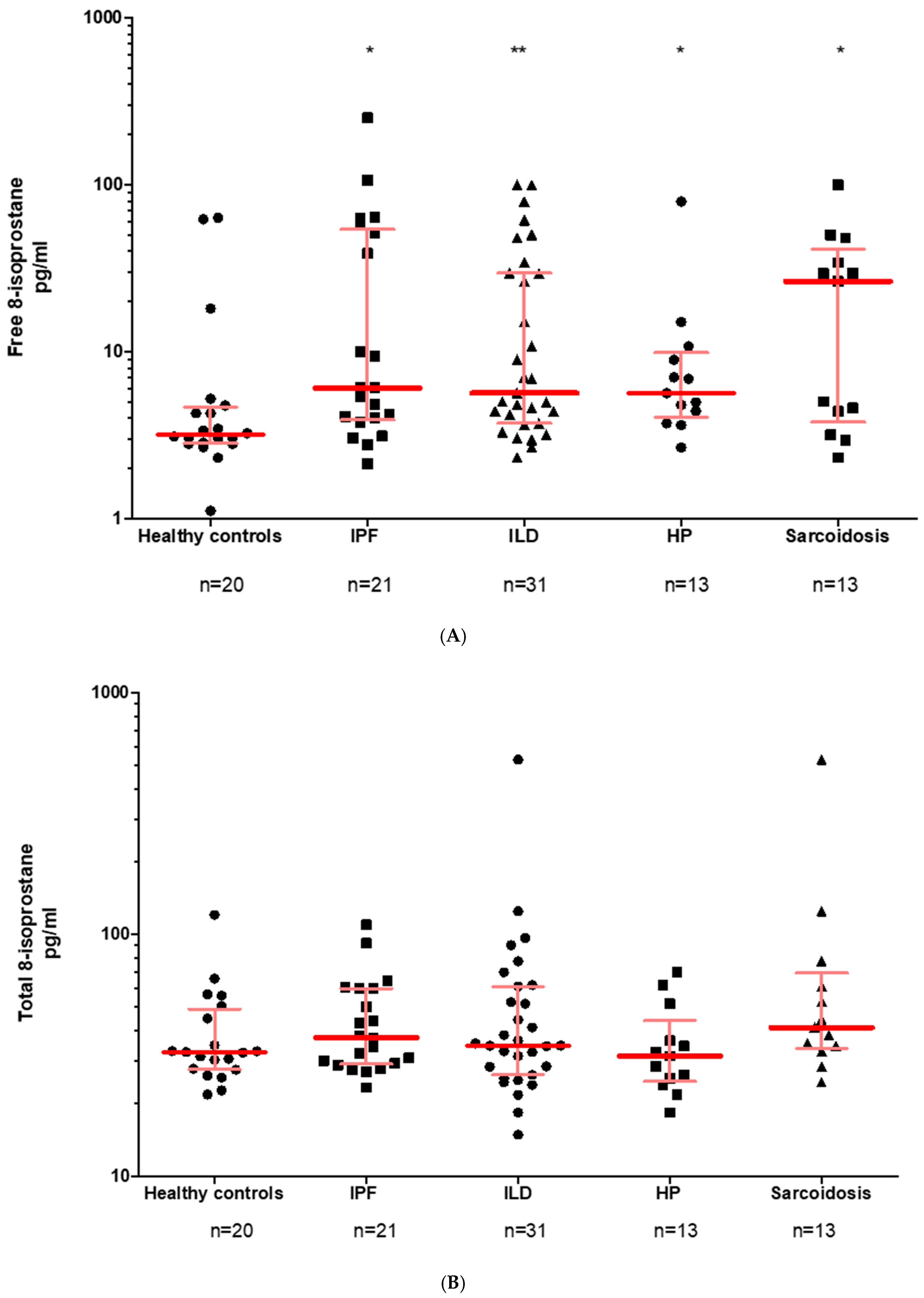
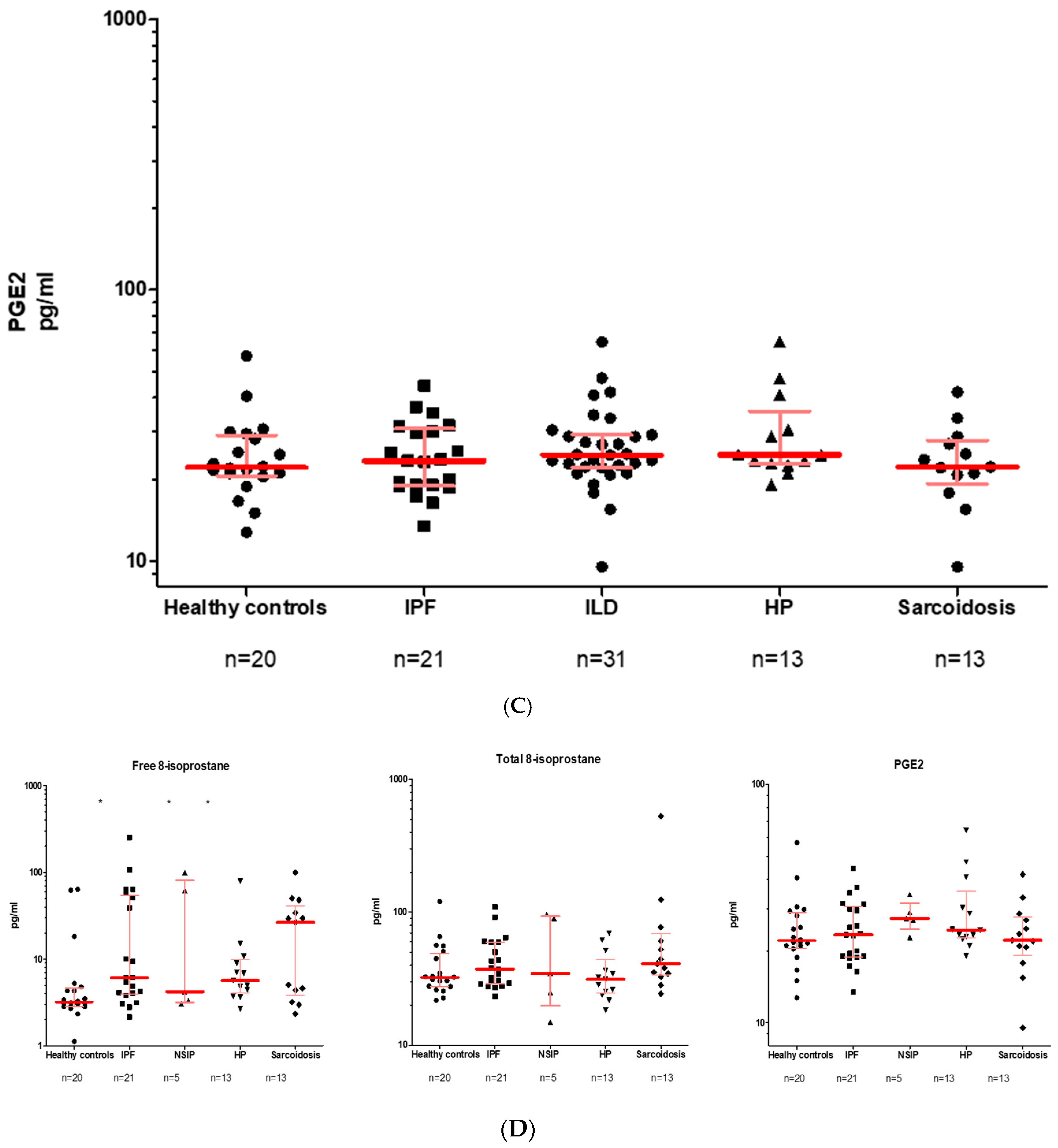
3.4. Free and Total 8-Isoprostane Values in the EBC and the BALF
3.5. PGE2 in the EBC and BALF
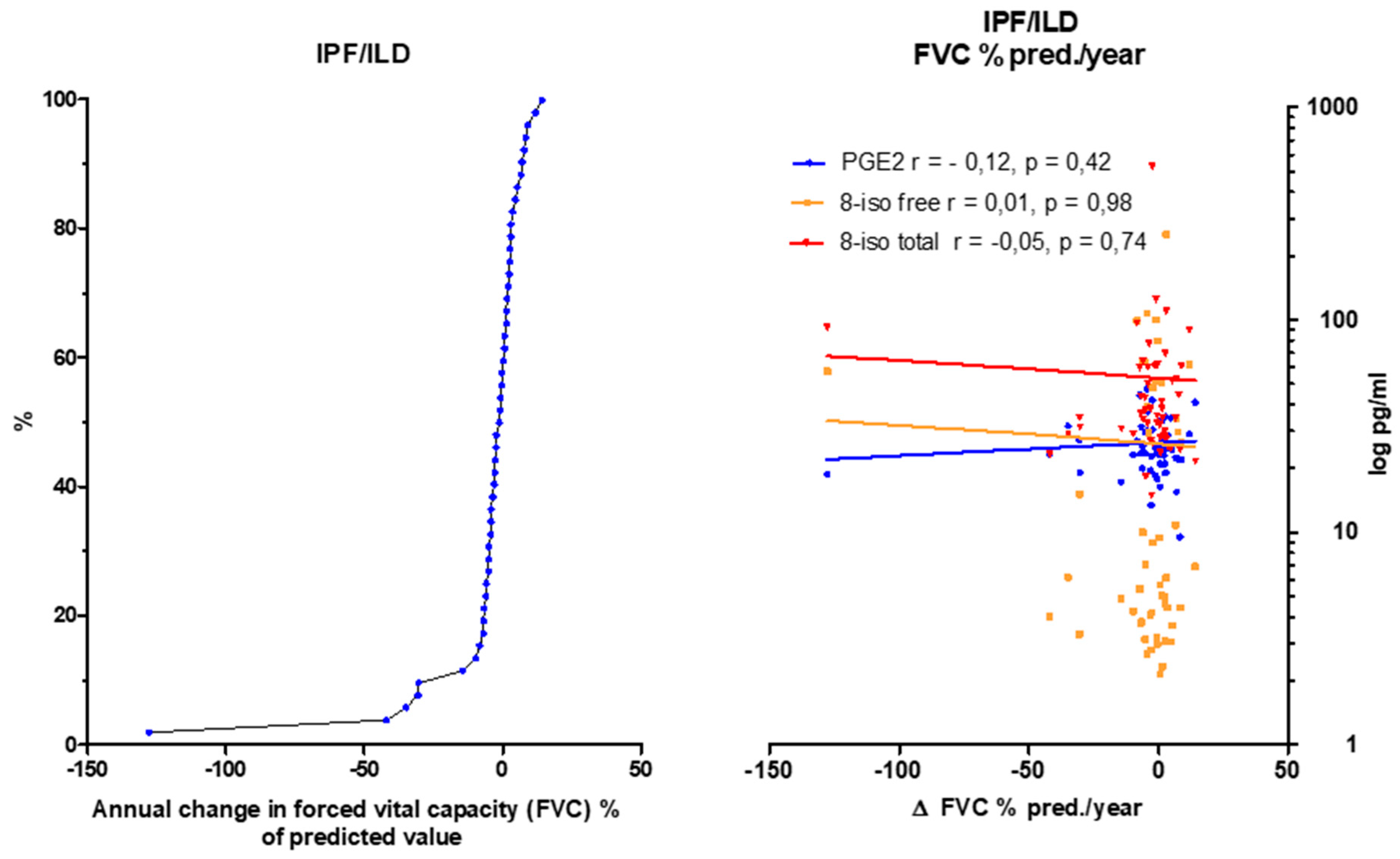
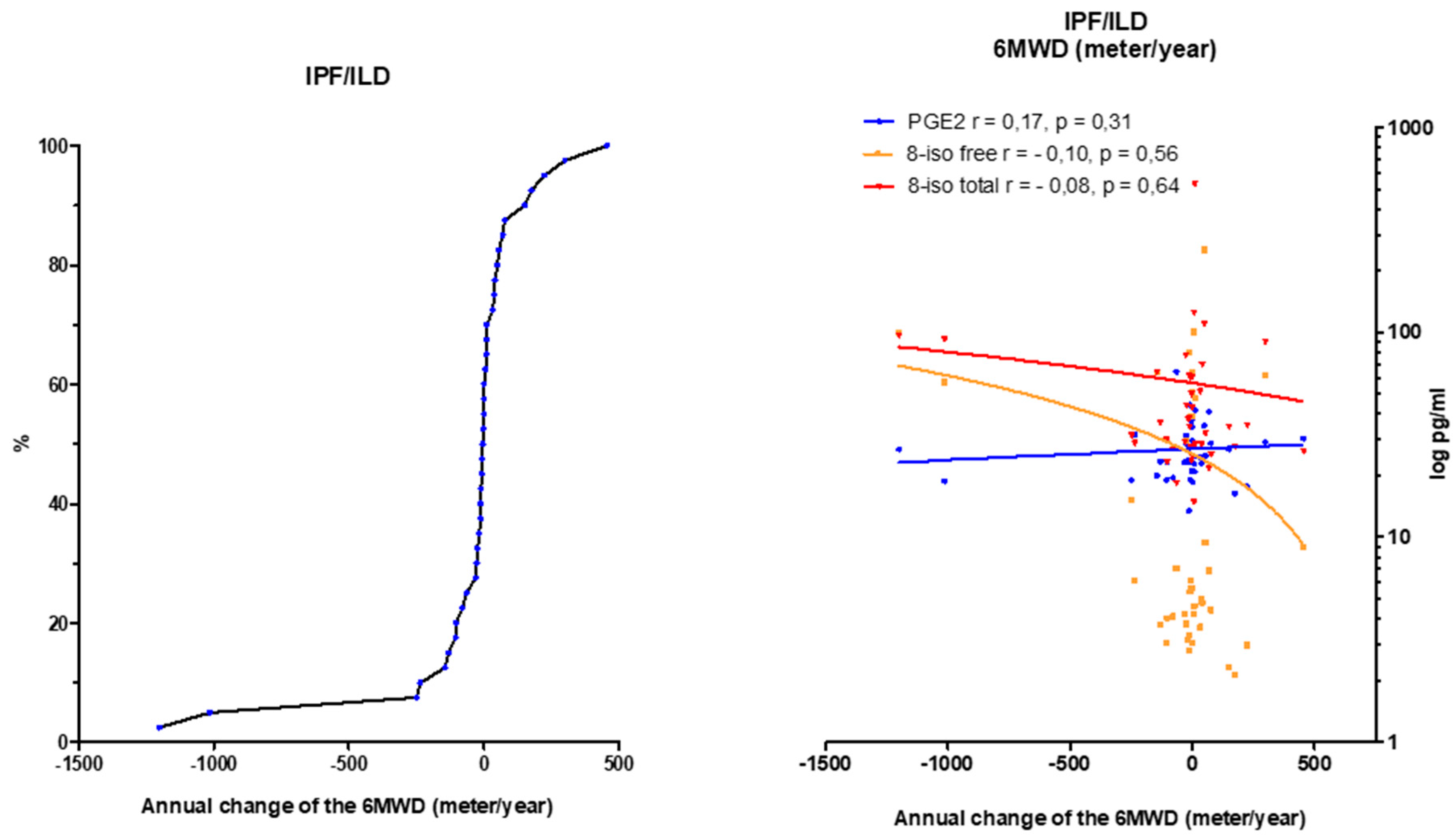
3.6. Eicosanoids Do Not Reflect Disease Progression
4. Discussion
5. Conclusions
Abbreviations
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mathai, S.K.; Schwartz, D.A. Translational research in pulmonary fibrosis. Transl. Res. J. Lab. Clin. Med. 2019, in press. [Google Scholar] [CrossRef]
- Guenther, A.; Krauss, E.; Tello, S.; Wagner, J.; Paul, B.; Kuhn, S.; Maurer, O.; Heinemann, S.; Costabel, U.; Barbero, M.A.N.; et al. The European IPF registry (eurIPFreg): Baseline characteristics and survival of patients with idiopathic pulmonary fibrosis. Respir. Res. 2018, 19, 141. [Google Scholar] [CrossRef]
- Witt, S.; Krauss, E.; Barbero, M.A.N.; Müller, V.; Bonniaud, P.; Vancheri, C.; Wells, A.U.; Vasakova, M.; Pesci, A.; Klepetko, W.; et al. Psychometric properties and minimal important differences of SF-36 in Idiopathic Pulmonary Fibrosis. Respir. Res. 2019, 20, 47. [Google Scholar] [CrossRef]
- Mahavadi, P.; Henneke, I.; Ruppert, C.; Knudsen, L.; Venkatesan, S.; Liebisch, G.; Chambers, R.C.; Ochs, M.; Schmitz, G.; Vancheri, C.; et al. Altered surfactant homeostasis and alveolar epithelial cell stress in amiodarone–induced lung fibrosis. Toxicol. Sci. 2014, 142, 285–297. [Google Scholar] [CrossRef] [PubMed]
- Korfei, M.; Ruppert, C.; Mahavadi, P.; Henneke, I.; Markart, P.; Koch, M.; Lang, G.; Fink, L.; Bohle, R.-M.; Seeger, W.; et al. Epithelial endoplasmic reticulum stress and apoptosis in sporadic idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2008, 178, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Lynch, D.A.; Sverzellati, N.; Travis, W.D.; Brown, K.K.; Colby, T.V.; Galvin, J.R.; Goldin, J.G.; Hansell, D.M.; Inoue, Y.; Johkoh, T.; et al. Diagnostic criteria for idiopathic pulmonary fibrosis: A Fleischner Society White Paper. Lancet Respir. Med. 2018, 6, 138–153. [Google Scholar] [CrossRef]
- Loeh, B.; Brylski, L.T.; von der Beck, D.; Seeger, W.; Krauss, E.; Bonniaud, P.; Crestani, B.; Vancheri, C.; Wells, A.U.; Markart, P.; et al. Lung CT densitometry in idiopathic pulmonary fibrosis (IPF) for the prediction of natural course, severity and mortality. Chest 2019, 155, 972–981. [Google Scholar] [CrossRef]
- Ravaglia, C.; Wells, A.U.; Tomassetti, S.; Gurioli, C.; Gurioli, C.; Dubini, A.; Cavazza, A.; Colby, T.V.; Piciucchi, S.; Puglisi, S.; et al. Diagnostic yield and risk/benefit analysis of trans–bronchial lung cryobiopsy in diffuse parenchymal lung diseases: A large cohort of 699 patients. BMC Pulm. Med. 2019, 19, 16. [Google Scholar] [CrossRef] [PubMed]
- Raghu, G.; Remy–Jardin, M.; Myers, J.L.; Richeldi, L.; Ryerson, C.J.; Lederer, D.J.; Behr, J.; Cottin, V.; Danoff, S.K.; Morell, F.; et al. Diagnosis of Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2018, 198, e44–e68. [Google Scholar] [CrossRef]
- Drakopanagiotakis, F.; Wujak, L.; Wygrecka, M.; Markart, P. Biomarkers in idiopathic pulmonary fibrosis. Matrix Biol. J. Int. Soc. Matrix Biol. 2018, 68–69, 404–421. [Google Scholar] [CrossRef]
- Hayton, C.; Terrington, D.; Wilson, A.M.; Chaudhuri, N.; Leonard, C.; Fowler, S.J. Breath biomarkers in idiopathic pulmonary fibrosis: A systematic review. Respir. Res. 2019, 20, 7. [Google Scholar] [CrossRef]
- Fois, A.G.; Paliogiannis, P.; Sotgia, S.; Mangoni, A.A.; Zinellu, E.; Pirina, P.; Carru, C.; Zinellu, A. Evaluation of oxidative stress biomarkers in idiopathic pulmonary fibrosis and therapeutic applications: A systematic review. Respir. Res. 2018, 19, 51. [Google Scholar] [CrossRef]
- Neighbors, M.; Cabanski, C.R.; Ramalingam, T.R.; Sheng, X.R.; Tew, G.W.; Gu, C.; Jia, G.; Peng, K.; Ray, J.M.; Ley, B.; et al. Prognostic and predictive biomarkers for patients with idiopathic pulmonary fibrosis treated with pirfenidone: Post-hoc assessment of the CAPACITY and ASCEND trials. Lancet Respir. Med. 2018, 6, 615–626. [Google Scholar] [CrossRef]
- Sgalla, G.; Iovene, B.; Calvello, M.; Ori, M.; Varone, F.; Richeldi, L. Idiopathic pulmonary fibrosis: Pathogenesis and management. Respir. Res. 2018, 19, 32. [Google Scholar] [CrossRef] [PubMed]
- Chiba, H.; Otsuka, M.; Takahashi, H. Significance of molecular biomarkers in idiopathic pulmonary fibrosis: A mini review. Respir. Investig. 2018, 56, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Ronan, N.; Bennett, D.M.; Khan, K.A.; McCarthy, Y.; Dahly, D.; Bourke, L.; Chelliah, A.; Cavazza, A.; O’Regan, K.; Moloney, F.; et al. Tissue and Bronchoalveolar Lavage Biomarkers in Idiopathic Pulmonary Fibrosis Patients on Pirfenidone. Lung 2018, 196, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Ghebre, Y.T.; Raghu, G. Idiopathic Pulmonary Fibrosis: Novel Concepts of Proton Pump Inhibitors as Antifibrotic Drugs. Am. J. Respir. Crit. Care Med. 2016, 193, 1345–1352. [Google Scholar] [CrossRef]
- Janssen, W.; Pullamsetti, S.S.; Cooke, J.; Weissmann, N.; Guenther, A.; Schermuly, R.T. The role of dimethylarginine dimethylaminohydrolase (DDAH) in pulmonary fibrosis. J. Pathol. 2013, 229, 242–249. [Google Scholar] [CrossRef]
- Guilleminault, L.; Saint-Hilaire, A.; Favelle, O.; Caille, A.; Boissinot, E.; Henriet, A.C.; Diot, P.; Marchand-Adam, S. Can exhaled nitric oxide differentiate causes of pulmonary fibrosis? Respir. Med. 2013, 107, 1789–1796. [Google Scholar] [CrossRef]
- Aldakheel, F.M.; Bourke, J.E.; Thomas, P.S.; Matheson, M.C.; Abramson, M.J.; Hamilton, G.S.; Lodge, C.J.; Thompson, B.R.; Walters, H.E.; Allen, K.J.; et al. NOx in exhaled breath condensate is related to allergic sensitization in young and middle-aged adults. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2018, 49, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Licari, A.; Castagnoli, R.; Brambilla, I.; Marseglia, A.; Tosca, M.A.; Marseglia, G.L.; Ciprandi, G. Asthma Endotyping and Biomarkers in Childhood Asthma. Pediatr. Allergy Immunol. Pulmonol. 2018, 31, 44–55. [Google Scholar] [CrossRef]
- Barnes, P.J.; Dweik, R.A.; Gelb, A.F.; Gibson, P.G.; George, S.C.; Grasemann, H.; Pavord, I.D.; Ratjen, F.; Silkoff, P.E.; Taylor, D.R.; et al. Exhaled nitric oxide in pulmonary diseases: A comprehensive review. Chest 2010, 138, 682–692. [Google Scholar] [CrossRef] [PubMed]
- Cameli, P.; Barbagli, E.; Rottoli, P. Exhaled nitric oxide is not increased in pulmonary sarcoidosis. Sarcoidosis Vasc. Diffuse Lung Dis. 2016, 33, 39–40. [Google Scholar] [PubMed]
- Speth, J.M.; Bourdonnay, E.; Penke, L.R.K.; Mancuso, P.; Moore, B.B.; Weinberg, J.B.; Peters–Golden, M. Alveolar epithelial cell–derived prostaglandin E2 serves as a request signal for macrophage secretion of suppressor of cytokine signaling 3 during innate inflammation. J. Immunol. (Baltimore Md. 1950) 2016, 196, 5112–5120. [Google Scholar] [CrossRef] [PubMed]
- Wettlaufer, S.H.; Scott, J.P.; McEachin, R.C.; Peters-Golden, M.; Huang, S.K. Reversal of the Transcriptome by Prostaglandin E2 during Myofibroblast Dedifferentiation. Am. J. Respir. Cell Mol. Biol. 2016, 54, 114–127. [Google Scholar] [CrossRef]
- Patrono, C.; FitzGerald, G.A. Isoprostanes: Potential markers of oxidant stress in atherothrombotic disease. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 2309–2315. [Google Scholar] [CrossRef] [PubMed]
- Kawikova, I.; Barnes, P.J.; Takahashi, T.; Tadjkarimi, S.; Yacoub, M.H.; Belvisi, M.G. 8-Epi-PGF2 alpha, a novel noncyclooxygenase-derived prostaglandin, constricts airways in vitro. Am. J. Respir. Crit. Care Med. 1996, 153, 590–596. [Google Scholar] [CrossRef]
- Malli, F.; Bardaka, F.; Tsilioni, I.; Karetsi, E.; Gourgoulianis, K.I.; Daniil, Z. 8–isoprostane levels in serum and bronchoalveolar lavage in idiopathic pulmonary fibrosis and sarcoidosis. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2013, 61, 160–163. [Google Scholar] [CrossRef]
- Horváth, I.; Barnes, P.J.; Loukides, S.; Sterk, P.J.; Högman, M.; Olin, A.-C.; Amann, A.; Antus, B.; Baraldi, E.; Bikov, A.; et al. A European Respiratory Society technical standard: Exhaled biomarkers in lung disease. Eur. Respir. J. 2017, 49, 1600965. [Google Scholar] [CrossRef]
- Ferraro, V.; Carraro, S.; Bozzetto, S.; Zanconato, S.; Baraldi, E. Exhaled biomarkers in childhood asthma: Old and new approaches. Asthma Res. Pract. 2018, 4, 9. [Google Scholar] [CrossRef]
- Dweik, R.A.; Boggs, P.B.; Erzurum, S.C.; Irvin, C.G.; Leigh, M.W.; Lundberg, J.O.; Olin, A.-C.; Plummer, A.L.; Taylor, D.R. An official ATS clinical practice guideline: Interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am. J. Respir. Crit. Care Med. 2011, 184, 602–615. [Google Scholar] [CrossRef] [PubMed]
- Paredi, P.; Kharitonov, S.A.; Meah, S.; Barnes, P.J.; Usmani, O.S. A novel approach to partition central and peripheral airway nitric oxide. Chest 2014, 145, 113–119. [Google Scholar] [CrossRef]
- Balbi, B.; Pignatti, P.; Corradi, M.; Baiardi, P.; Bianchi, L.; Brunetti, G.; Radaeli, A.; Moscato, G.; Mutti, A.; Spanevello, A.; et al. Bronchoalveolar lavage, sputum and exhaled clinically relevant inflammatory markers: Values in healthy adults. Eur. Respir. J. 2007, 30, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Gelb, A.F.; George, S.C.; Camacho, F.; Fraser, C.; Flynn Taylor, C.; Shakkottai, S. Increased nitric oxide concentrations in the small airway of older normal subjects. Chest 2011, 139, 368–375. [Google Scholar] [CrossRef]
- Lu, Z.; Huang, W.; Wang, L.; Xu, N.; Ding, Q.; Cao, C. Exhaled nitric oxide in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 2695–2705. [Google Scholar] [CrossRef]
- Lehtimäki, L.; Kankaanranta, H.; Saarelainen, S.; Hahtola, P.; Järvenpää, R.; Koivula, T.; Turjanmaa, V.; Moilanen, E. Extended exhaled NO measurement differentiates between alveolar and bronchial inflammation. Am. J. Respir. Crit. Care Med. 2001, 163, 1557–1561. [Google Scholar] [CrossRef]
- Saleh, D.; Barnes, P.J.; Giaid, A. Increased production of the potent oxidant peroxynitrite in the lungs of patients with idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 1997, 155, 1763–1769. [Google Scholar] [CrossRef]
- Paredi, P.; Kharitonov, S.A.; Loukides, S.; Pantelidis, P.; Du Bois, R.M.; Barnes, P.J. Exhaled nitric oxide is increased in active fibrosing alveolitis. Chest 1999, 115, 1352–1356. [Google Scholar] [CrossRef]
- Cameli, P.; Bargagli, E.; Bergantini, L.; Refini, R.M.; Pieroni, M.; Sestini, P.; Rottoli, P. Evaluation of multiple-flows exhaled nitric oxide in idiopathic and non-idiopathic interstitial lung disease. J. Breath Res. 2019. [Google Scholar] [CrossRef]
- Schildge, J. Stickstoffmonoxyd in der Atemluft von Patienten mit interstitiellen Lungenkrankheiten. Pneumologie (Stuttg. Ger.) 2011, 65, 143–148. [Google Scholar] [CrossRef]
- Wilborn, J.; Crofford, L.J.; Burdick, M.D.; Kunkel, S.L.; Strieter, R.M.; Peters-Golden, M. Cultured lung fibroblasts isolated from patients with idiopathic pulmonary fibrosis have a diminished capacity to synthesize prostaglandin E2 and to express cyclooxygenase-2. J. Clin. Investig. 1995, 95, 1861–1868. [Google Scholar] [CrossRef] [PubMed]
- Okunishi, K.; Sisson, T.H.; Huang, S.K.; Hogaboam, C.M.; Simon, R.H.; Peters-Golden, M. Plasmin overcomes resistance to prostaglandin E2 in fibrotic lung fibroblasts by reorganizing protein kinase A signaling. J. Biol. Chem. 2011, 286, 32231–32243. [Google Scholar] [CrossRef] [PubMed]
- Maher, T.M.; Evans, I.C.; Bottoms, S.E.; Mercer, P.F.; Thorley, A.J.; Nicholson, A.G.; Laurent, G.J.; Tetley, T.D.; Chambers, R.C.; McAnulty, R.J. Diminished prostaglandin E2 contributes to the apoptosis paradox in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2010, 182, 73–82. [Google Scholar] [CrossRef]
- Psathakis, K.; Mermigkis, D.; Papatheodorou, G.; Loukides, S.; Panagou, P.; Polychronopoulos, V.; Siafakas, N.M.; Bouros, D. Exhaled markers of oxidative stress in idiopathic pulmonary fibrosis. Eur. J. Clin. Investig. 2006, 36, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Montuschi, P.; Ciabattoni, G.; Paredi, P.; Pantelidis, P.; Du Bois, R.M.; Kharitonov, S.A.; Barnes, P.J. 8-Isoprostane as a biomarker of oxidative stress in interstitial lung diseases. Am. J. Respir. Crit. Care Med. 1998, 158, 1524–1527. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Healthy Controls | IPF | ILD | COPD | Lung Cancer | Pooled Analysis | Test |
|---|---|---|---|---|---|---|---|
| n = 20 | n = 11 | n = 23 | n = 24 | n = 16 | p Value | ||
| Age | 30 (25–49) | 70 (66–73) *** | 68 (49–73) *** | 68 (61–74) | 65 (58–70) | <0.0001 | KW |
| Gender (female/male) | 19/1 | 2/9 | 10/13 | 10/14 | 3/13 | <0.0001 | KW |
| Active smoker, n (%) | 8 (40) | 1 (9) | 2 (9) | 4 (17) | 2 (13) | <0.0001 | KW |
| Never smoked, n (%) | 10 (50) | 3 (27) | 8 (35) | 4 (17) | 0 (0) | ||
| Ex smoker, n (%) | 2 (10) | 7 (64) | 13 (57) | 16 (67) | 14 (88) | ||
| CRP (mg/dl) | 0.5 (0.3–1.3) | 0.5 (0.2–1.3) | 0.7 (0.43–1.4) | 0.5 (0.15–1.08) | 0.29 | KW | |
| VC % pred. | 102 (87–112) | 75 (47–83) *** | 77 (55–92) | 68 (46–81), n = 23 | 79 (66–87) | <0.0001 | KW |
| FVC % pred. | 97 (83–110) | 68 (45–88) | 83 (47–97) ** | 57 (40–72), n = 22 *** | 76 (62–87) | <0.0001 | KW |
| TLC % pred. | 103 (94–108) | 57 (47–75) *** | 78 (62–98) ** | 87 (78–119), n = 22 | 85 (79–97) | <0.0001 | KW |
| FEV1 % pred. | 95 (87–109) | 90 (57–95) | 84 (57–109) ** | 53 (43–66), n = 23 *** | 78 (67–91) | <0.0001 | KW |
| FEV1/VC % pred. | 99 (91–106) | 112 (109–138) | 113 (104–131) *** | 83 (68–104) | 106 (92–110) | 0.0003 | KW |
| ITGV % pred. | 99 (91–112) | 64 (50–90) ** | 88 (66–109) | 113 (93–170), n = 23 | 91 (77–114) | 0.0015 | KW |
| RV % pred. | 104 (91–124) | 50 (24–80) *** | 89 (57–121) * | 140 (86–197), n = 22 | 98 (84–133) | 0.0012 | KW |
| RV/TLC % pred. | 104 (93–112) | 60 (50–142) ** | 110 (78–124) * | 147 (120–172), n = 23 ** | 112 (95–137) | 0.0008 | KW |
| R tot kPa x s/l | 0.23 (0.21–0.29) | 0.32 (0.25–0.65) | 0.34 (0.26–0.43) *** | 0.61 (0.5–0.8), n = 23 *** | 0.43 (0.33–0.54) * | <0.0001 | KW |
| DLCO % pred. | 91 (79–108) | 38 (26–54), n = 10 *** | 57 (37–74), n = 17 * | 20 (16–31), n = 7 *** | 40 (31–52), n = 6 * | <0.0001 | KW |
| KCO % pred. | 88 (77–99) | 53 (33–62), n = 10** | 67 (65–93), n = 15 | 22.5 (13–32), n = 2 * | 0.0003 | KW | |
| SaO2 in % | 97 (95–98), n =10 | 94 (94–95) | 96 (95–97)* | 94 (92–95) ** | 95 (94–96) | 0.0048 | KW |
| pO2 (mmHg) | 80 (71–89), n =10 | 73 (69–75) | 81 (74–87) | 69 (63–76.5) | 75.5 (69–83) | 0.0952 | KW |
| pCO2 (mmHg) | 34 (33–37), n =10 | 41 (36–46) | 39 (37–42) | 42 (40–48.25) | 39 (37–44.25) | 0.0147 | KW |
| LTOT, n (%) | 0 (0) | 3 (27) | 3 (15) | 8 (33.3) | 2 (12.5) | 0.0416 | Chi² |
| 6 MWD (meters) | 270 (120–360) | 360 (293–480), n = 10 | 360 (270–360), n = 4 | 300, n = 1 | 0.1557 | KW | |
| VO2max (ml/kg/min) | 13 (11.5–21.5), n = 5 | 19 (14–25), n = 7 | 17, n = 1 | 18 (14–22), n = 2 | 0.6404 | KW | |
| NSAID, n (%) | 0 (0) | 6 (55) | 9 (39) ** | 8 (33,3) | 8 (50) | 0.005 | KW |
| PPI, n (%) | 0 (0) | 5 (45) | 10 (43) | 14 (58) *** | 12 (75) | <0.0001 | KW |
| Systemic steroids | 0 (0) | 8 (73) | 15 (65) | 19 (79) *** | 7 (44) | <0.0001 | KW |
| Pirfenidone, n (%) | 0 (0) | 5 (45) | 0 (0) | 0 (0) | 0 (0) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krauss, E.; Froehler, M.; Degen, M.; Mahavadi, P.; Dartsch, R.C.; Korfei, M.; Ruppert, C.; Seeger, W.; Guenther, A. Exhalative Breath Markers Do Not Offer for Diagnosis of Interstitial Lung Diseases: Data from the European IPF Registry (eurIPFreg) and Biobank. J. Clin. Med. 2019, 8, 643. https://doi.org/10.3390/jcm8050643
Krauss E, Froehler M, Degen M, Mahavadi P, Dartsch RC, Korfei M, Ruppert C, Seeger W, Guenther A. Exhalative Breath Markers Do Not Offer for Diagnosis of Interstitial Lung Diseases: Data from the European IPF Registry (eurIPFreg) and Biobank. Journal of Clinical Medicine. 2019; 8(5):643. https://doi.org/10.3390/jcm8050643
Chicago/Turabian StyleKrauss, Ekaterina, Maike Froehler, Maria Degen, Poornima Mahavadi, Ruth C. Dartsch, Martina Korfei, Clemens Ruppert, Werner Seeger, and Andreas Guenther. 2019. "Exhalative Breath Markers Do Not Offer for Diagnosis of Interstitial Lung Diseases: Data from the European IPF Registry (eurIPFreg) and Biobank" Journal of Clinical Medicine 8, no. 5: 643. https://doi.org/10.3390/jcm8050643
APA StyleKrauss, E., Froehler, M., Degen, M., Mahavadi, P., Dartsch, R. C., Korfei, M., Ruppert, C., Seeger, W., & Guenther, A. (2019). Exhalative Breath Markers Do Not Offer for Diagnosis of Interstitial Lung Diseases: Data from the European IPF Registry (eurIPFreg) and Biobank. Journal of Clinical Medicine, 8(5), 643. https://doi.org/10.3390/jcm8050643






