Migration of the Lag Screw after Intramedullary Treatment of AO/OTA 31.A2.1-3 Pertrochanteric Fractures Does Not Result in Higher Incidence of Cut-Outs, Regardless of Which Implant Was Used: A Comparison of Gamma Nail with and without U-Blade (RC) Lag Screw and Proximal Femur Nail Antirotation (PFNA)
Abstract
1. Introduction
2. Materials and Methods
2.1. Diagnosis, Surgical Technique and Aftercare
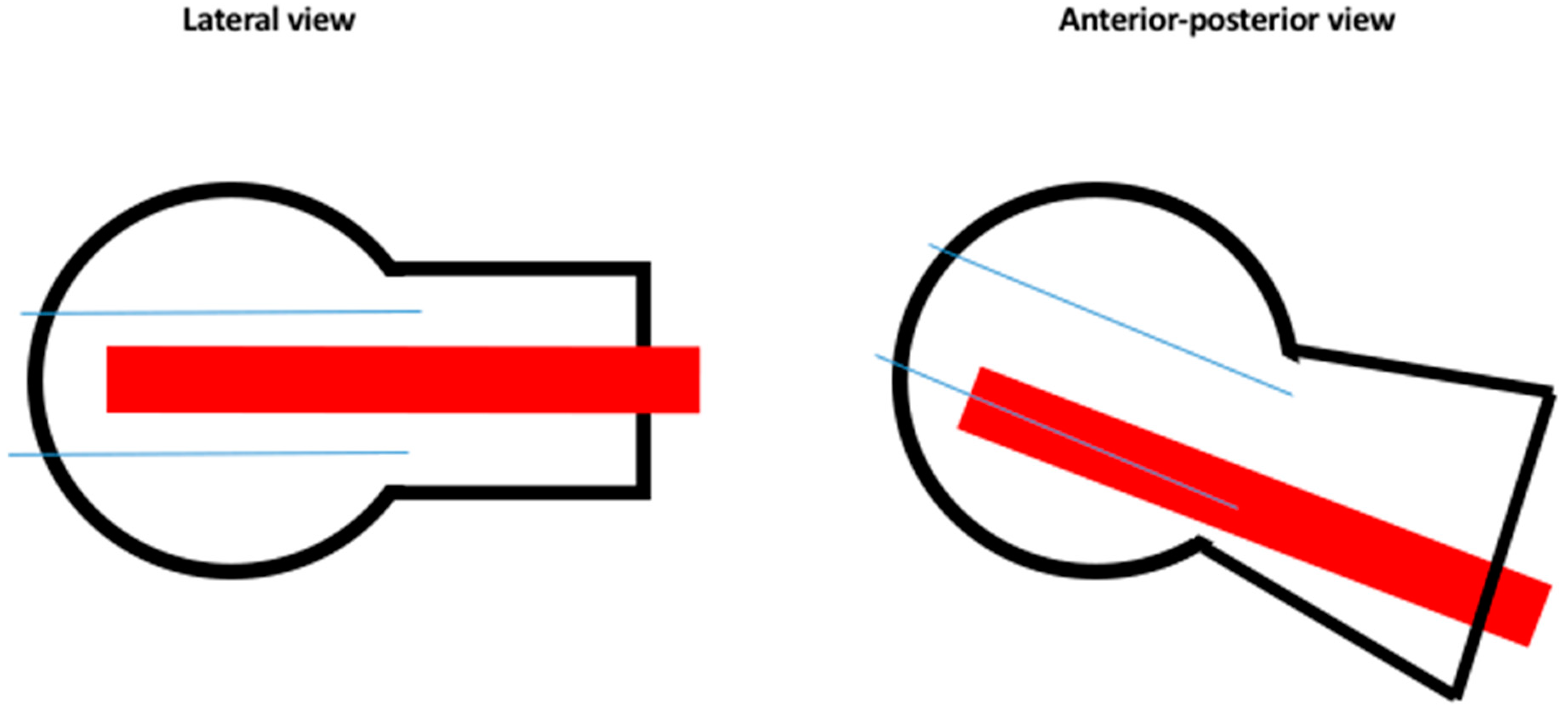
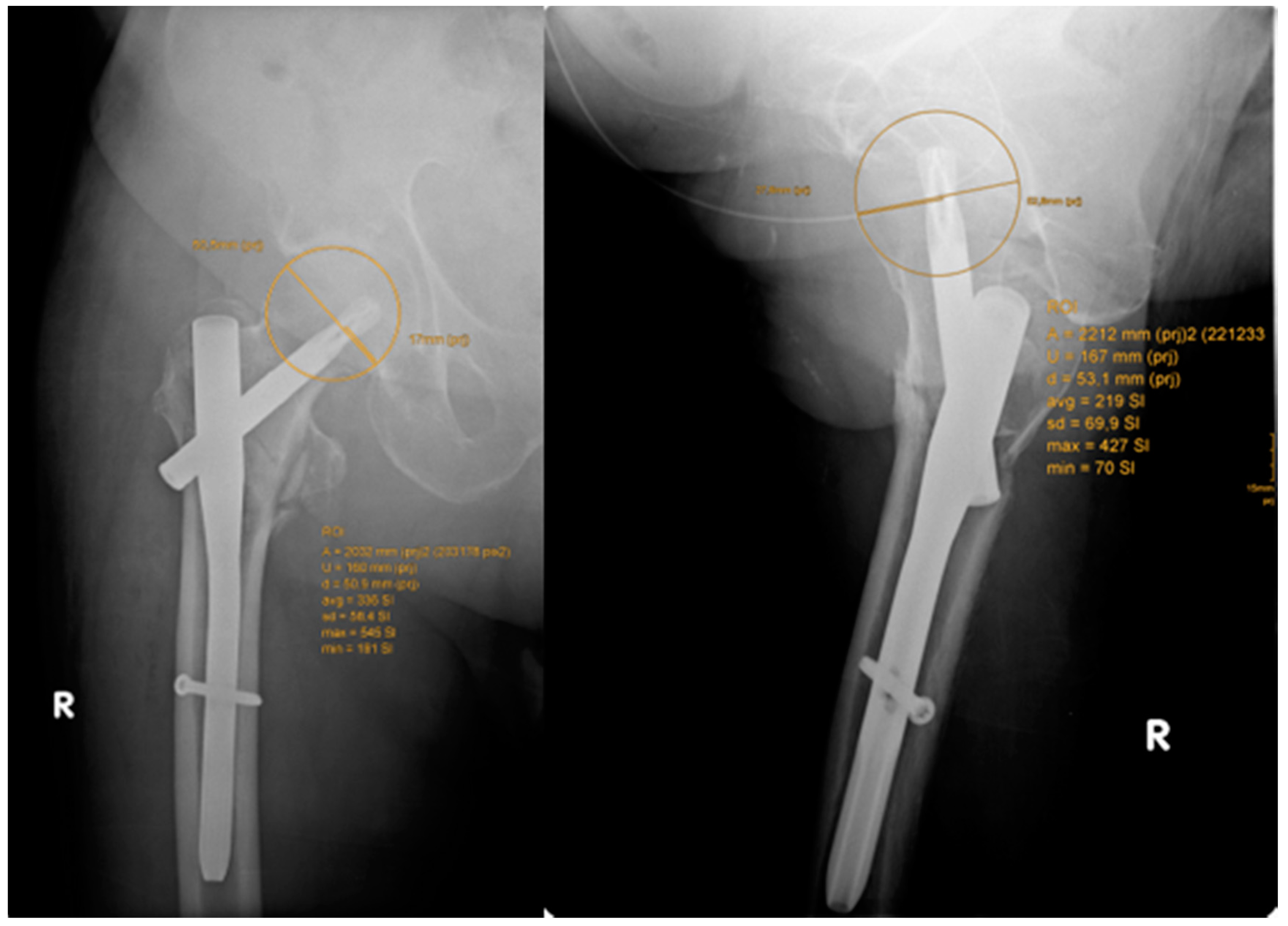
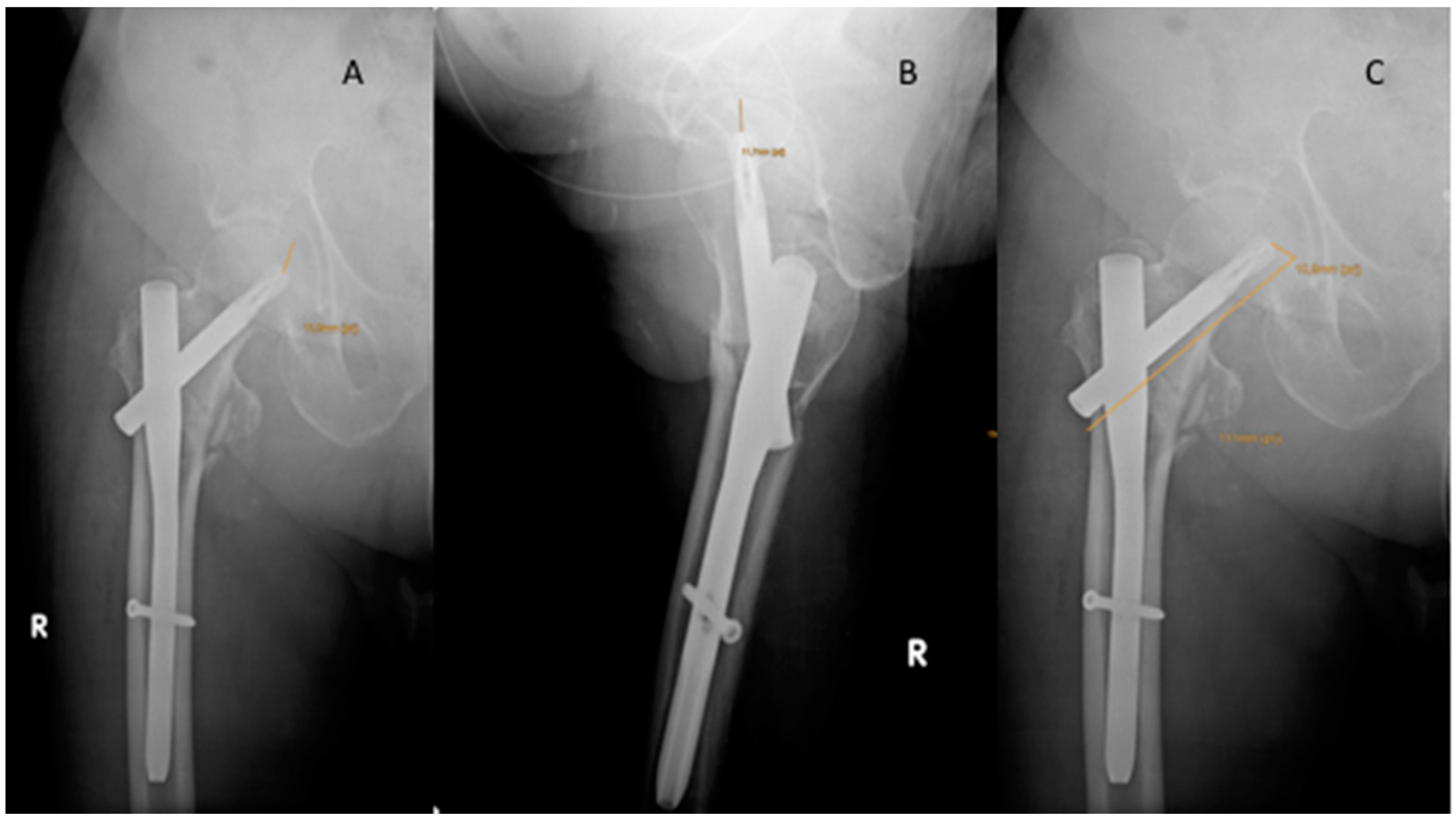
2.2. Outcome Parameters
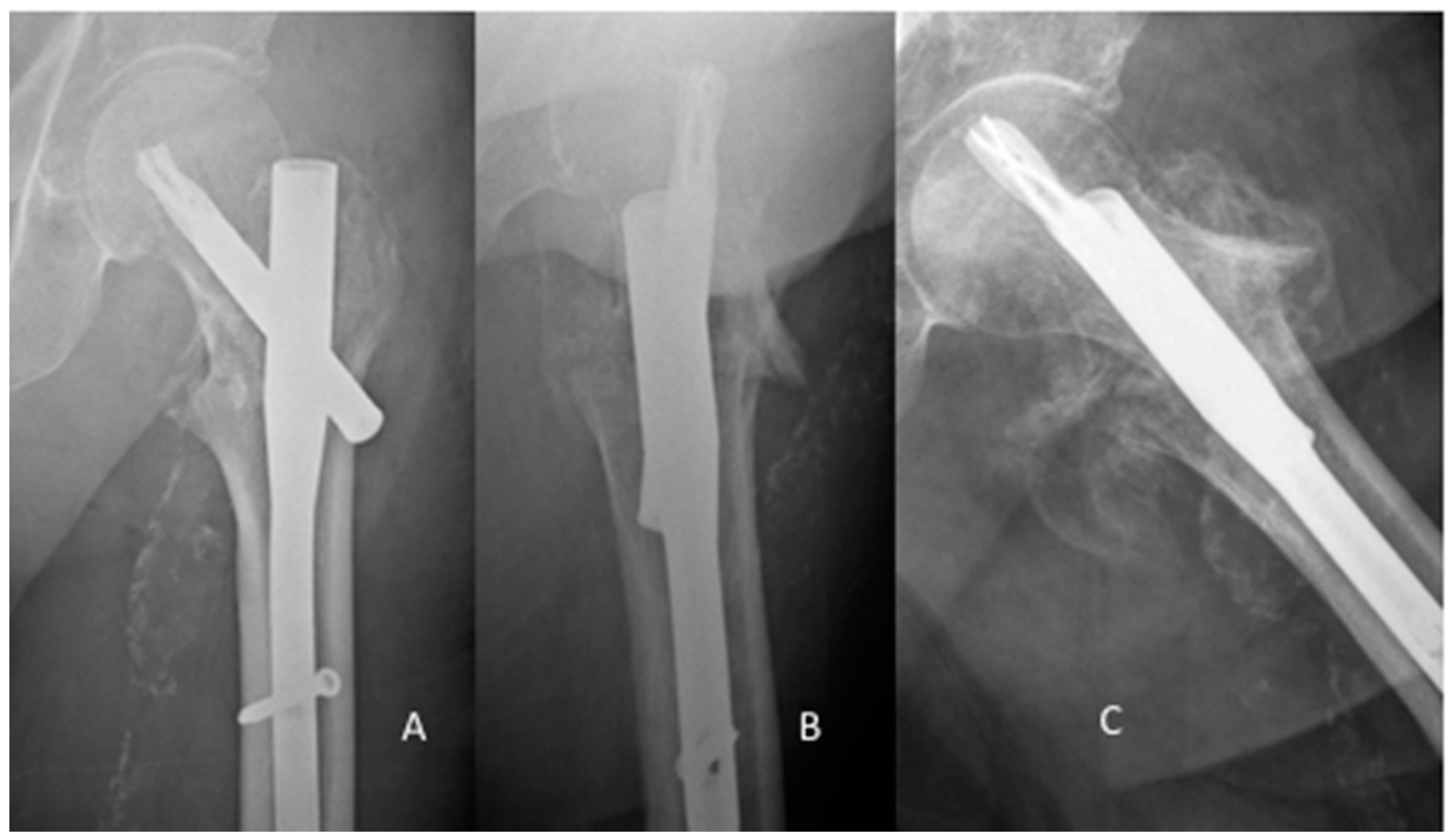
2.3. Complications
2.4. Statistical Analysis
3. Results
3.1. Time to Cut Out/Treatment
3.2. Migration of the Lag Screw/Blade
3.3. Functional Outcome
4. Discussion
Limitations
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Sandmann, G.; Biberthaler, P. Pertrochanteric femoral fractures in the elderly. Unfallchirurg 2015, 118, 447–462. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertner, M.; Socci, A.; Casemyr, N.; Leslie, M. Implant options for the treatment of intertrochanteric fractures of the hip: Rationale, evidence, and recommendations. Bone Joint J. 2017, 99, 128–133. [Google Scholar] [CrossRef]
- Jun, L.; Augusto, R.; Sousa, M.; Zamboni, C.; Durigan, J.R.; Hungria, J.S.; Mercadante, M.T.; Christian, R.W.; Hungria, J.O.S. Late postoperative analysis of the tip-apex distance (TAD) in pertrochanteric fractures: Is there an accommodation of the implant within the bone? Injury 2017, 48, 54–56. [Google Scholar] [CrossRef]
- Carulli, C.; Piacentini, F.; Paoli, T.; Civinini, R.; Innocenti, M. A comparison of two fixation methods for femoral trochanteric fractures: A new generation intramedullary system vs sliding hip screw. Clin. Cases Miner Bone Metab. 2017, 14, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Niu, E.; Ms, A.Y.; Harris, A.H.S.; Bishop, J. Which fixation device is preferred for surgical treatment of intertrochanteric hip fractures in the United States? A survey of orthopaedic surgeons. Clin. Orthop. Relat. Res. 2015, 473, 3647–3655. [Google Scholar] [CrossRef]
- Matre, K.; Ivar, L.; Gjertsen, J.; Vinje, T.; Espehaug, B.; Meling, J. Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures. A study of 2716 patients in the Norwegian Hip Fracture Register. Injury 2013, 44, 735–742. [Google Scholar] [CrossRef]
- Ozkan, K.; Eceviz, E.; Unay, K. Treatment of reverse oblique trochanteric femoral fractures with proximal femoral nail. Int. Orthop. 2011, 35, 595–598. [Google Scholar] [CrossRef]
- Kregor, P.J.; Obremskey, W.T.; Kreder, H.J.; Swiontkowski, M.F. Unstable pertrochanteric femoral fractures. J. Orthop. Trauma 2014, 28, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Radaideh, A.M.; Qudah, H.A.; Audat, Z.A.; Jahmani, R.A.; Yousef, I.R.; Saleh, A.A. Functional and radiological results of proximal femoral nail antirotation (PFNA) osteosynthesis in the treatment of unstable pertrochanteric fractures. J. Clin. Med. 2018, 7. [Google Scholar] [CrossRef]
- Hoffmann, S.; Paetzold, R.; Stephan, D.; Püschel, K.; Buehren, V.; Augat, P. Biomechanical evaluation of interlocking lag screw design in intramedullary nailing of unstable pertrochanteric fractures. J Orthop Trauma 2013, 27, 483–490. [Google Scholar] [CrossRef]
- Zhang, H.; Zhu, X.; Pei, G.; Zeng, X.; Zhang, N.; Xu, P.; Chen, D.; Yu, W.; Zhang, X. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation in the treatment of intertrochanteric fractures in elderly patients with osteoporosis: A minimum follow-up of 3 years. J. Orthop. Surg. Res. 2017, 12, 1–8. [Google Scholar] [CrossRef][Green Version]
- Bojan, A.; Beimel, C.; Speitling, A.; Taglang, G.; Ekholm, C.; Jönsson, A. 3066 consecutive Gamma Nails. 12 years experience at a single centre. BMC Musculoskelet. Disord. 2010, 11, 1–10. [Google Scholar] [CrossRef]
- Geller, J.A.; Saifi, C.; Morrison, T.A. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int. Orthop. 2010, 34, 719–722. [Google Scholar] [CrossRef]
- Aicale, R.; Maffulli, N. Greater rate of cephalic screw mobilisation following proximal femoral nailing in hip fractures with a tip – apex distance (TAD) and a calcar referenced TAD greater than 25mm. J. Orthop. Surg. Res. 2018, 13, 1–9. [Google Scholar] [CrossRef]
- Chinzei, N.; Hiranaka, T.; Niikura, T.; Tsuji, M. Comparison of the sliding and femoral head rotation among three different femoral head fixation devices for trochanteric fractures. Clin. Orthop. Surg. 2015, 7, 291–297. [Google Scholar] [CrossRef]
- Lenich, A.; Vester, H.; Nerlich, M.; Mayr, E.; Stöckle, U.; Füchtmeier, B. Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip—Blade vs screw. Injury 2010, 41, 1292–1296. [Google Scholar] [CrossRef]
- Queally, J.; Harris, E.; Handoll, H.; Parker, M. Intramedullary nails for extracapsular hip fractures in adults. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef]
- Lang, N.W.; Arthold, C.; Joestl, J.; Gormasz, A.; Boesmueller, S.; Hajdu, S.; Sarahrudi, K. Does an additional antirotation U-Blade (RC) lag screw improve treatment of AO / OTA 31 A1-3 fractures with gamma 3 nail? Injury 2016, 47, 2733–2738. [Google Scholar] [CrossRef]
- Ma, K.; Wang, X.; Luan, F.; Xu, H.; Fang, Y.; Min, J.; Luan, H.X.; Yang, F.; Zheng, H.; He, S.J. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: A meta-analysis. Orthop. Traumatol. Surg. Res. 2014, 100, 859–866. [Google Scholar] [CrossRef]
- Mueller, M. Classification and international AO-documentation of femur fractures. Unfallheilkunde 1980, 83, 251–259. [Google Scholar]
- Maggi, S.; Siviero, P.; Wetle, T.; Besdine, R.W. A multicenter survey on profile of care for hip fracture: Predictors of mortality and disability. Osteoporos. Int. 2010, 21, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Bottle, A.; Aylin, P. Mortality associated with delay in operation after hip fracture: Observational study. BMJ 2006, 55, 947–951. [Google Scholar] [CrossRef]
- Kostuj, T.; Smektala, R.; Schulze-Raestrup, U.; Müller-Mai, C. Pertrochanteric fractures. What impact do surgical timing and implant choice have on the outcome? Unfallchirurg 2013, 116, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Smektala, R.; Endres, H.G.; Dasch, B.; Maier, C.; Trampisch, H.J.; Bonnaire, F.; Pientka, L. The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet. Disord. 2008, 9, 171. [Google Scholar] [CrossRef]
- Parker, M. Cutting-out of the dynamic hip screw related to its position. J. Bone Joint Surg. Br. 1992, 74, 625. [Google Scholar] [CrossRef]
- Cleveland, M.; Bosworth, D.M.; Thompson, F.R.; Wilson, H.J.J.; Ishizuka, T. A ten-year analysis of intertrochanteric fractures of the femur. J. Bone Jt. Surgery Am. 1959, 41, 1399–1408. [Google Scholar] [CrossRef]
- Parmar, V.; Kumar, S.; Aster, A.; Harper, W.H. Review of methods to quantify lag screw placement in hip fracture fixation. Acta Orthopædica. Belgica. 2005, 3, 260–263. [Google Scholar]
- Kashigar, A.; Vincent, A.; Gunton, M.J.; Safir, O.; Kuzyk, P.R.T. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Jt. J. 2014, 96, 1029–1034. [Google Scholar] [CrossRef]
- Parker, M.J.; Palmer, C.R. A new mobility score for predicting mortality after hip fractures. J. Bone Joint Surg. Br. 1993, 75, 797–798. [Google Scholar] [CrossRef]
- Georgiannos, D.; Lampridis, V.; Bisbinas, I. Complications following treatment of trochanteric fractures with the gamma3 nail: Is the latest version of gamma nail superior to its predecessor? Surg. Res. Pract. 2014, 2014, 3–8. [Google Scholar] [CrossRef]
- Andruszkow, H.; Frink, M.; Frömke, C.; Suntardjo, S.; Krettek, C.; Hildebrand, F. Tip apex distance, hip screw placement, and neck shaft angle as potential risk factors for cut-out failure of hip screws after surgical treatment of intertrochanteric fractures. Int. Orthop. 2012, 11, 2347–2354. [Google Scholar] [CrossRef]
- Murena, L.; Moretti, A.; Meo, F.; Saggioro, E.; Barbati, G.; Ratti, C. Predictors of cut-out after cephalomedullary nail fixation of pertrochanteric fractures: A retrospective study of 813 patients. Arch Orthop. Trauma Surg. 2018, 138, 351–359. [Google Scholar] [CrossRef]
- Liu, Y.; Tao, R.; Liu, F.; Wang, Y.; Zhou, Z.; Cao, Y.; Wang, H. Mid-term outcomes after intramedullary fixation of peritrochanteric femoral fractures using the new proximal femoral nail antirotation (PFNA). Injury 2010, 41, 810–817. [Google Scholar] [CrossRef]
- Simmermacher, R.K.J.; Ljungqvist, J.; Bail, H.; Hockerts, T.; Vochteloo, A.J.H.; Ochs, U.; Werken, C.v.; AO-PFNA studygroup. The new proximal femoral nail antirotation (PFNA) in daily practice: Results of a multicentre clinical study. Injury 2008, 39, 932–939. [Google Scholar] [CrossRef]
- Kraus, M.; Krischak, G.; Wiedmann, K.; Riepl, C.; Gebhard, F.; Jöckel, J.A.; Scola, A. Clinical evaluation of PFNA® and relationship between the tip-apex distance and mechanical failure. Unfallchirurg 2011, 114, 470–478. [Google Scholar] [CrossRef]
- Kammerlander, C.; Gebhard, F.; Meier, C.; Lenich, A.; Linhart, W.; Clasbrummel, B.; Neubauer-Gartzke, T.; Garcia-Alonso, M.; Pavelka, T.; Blauth, M. Standardised cement augmentation of the PFNA using a perforated blade: A new technique and preliminary clinical results. A prospective multicentre trial. Injury 2011, 42, 1484–1490. [Google Scholar] [CrossRef]
- Iwakura, T.; Niikura, T.; Lee, S.Y.; Sakai, Y.; Nishida, K.; Kuroda, R.; Kurosaka, M. Case report breakage of a third generation gamma nail: A case report and review of the literature. Case Rep. Orthop. 2013, 2013, 1–5. [Google Scholar] [CrossRef]
- Bojan, A.J.; Beimel, C.; Taglang, G.; Collin, D.; Ekholm, C.; Jönsson, A. Critical factors in cut-out complication after gamma nail treatment of proximal femoral fractures. BMC Musculoskelet. Disord. 2013, 14, 1–9. [Google Scholar] [CrossRef]
- Morvan, A.; Boddaert, J.; Cohen-Bittan, J.; Picard, H.; Pascal-Mousselard, H.; Khiami, F. Risk factors for cut-out after internal fixation of trochanteric fractures in elderly subjects. Orthop. Traumatol. Surg. Res. 2018, 104, 1183–1187. [Google Scholar] [CrossRef]
| PFNA | Gamma | U-Blade | Total | |
|---|---|---|---|---|
| (n = 86) | (n = 82) | (n = 69) | (n = 237) | |
| Male/Female | 15/71 | 19/63 | 11/58 | 45/192 |
| Age (years) | 80.7±11.7 | 82.0 ± 10.0 | 83.2 ± 9.6 | 81.9 ± 10.5 |
| BMI (kg/m2) | 23.4 ± 3.8 | 23.9 ± 4.6 | 24.6 ± 4.0 | 24.0 ± 4.1 |
| Operation (min) | 56.5 ± 22.4 | 57.1 ± 25.3 | 67.8 ± 23.8 * | 60.5 ± 23.8 |
| Lateralization | 3 | 5 | 10 | 22 |
| Cut-out | 1 | 3 | 2 | 6 |
| Infection (superficial) | 2 | 2 | 0 | 4 |
| Complications requiring surgery | 4 (4.7%) | 12 (14.6%) | 4 (5.7%) | 8.4% |
| PFNA | Gamma | U-Blade | Total | |
|---|---|---|---|---|
| Parker’s ratio AP | 45.1 ± 8.0 | 43.2 ± 8.1 | 47.8 ± 6.6 | 45.3 ± 7.8 |
| Parker’s ratio AP f/u | 54.6 ± 8.7 * | 45.1 ± 8.3 | 49.2 ± 7.7 | 49.8 ± 8.9 |
| Parker’s ratio LAT | 54.3 ± 7.7 | 55.2 ± 8.0 | 50.8 ± 7.2 | 53.6 ± 7.8 |
| Parker’s ratio LAT f/u | 53.7 ± 8.4 | 55.9 ± 7.1 | 49.3 ± 6.4 | 53.0 ± 7.9 |
| CalTAD | 12.6 ± 2.9 | 12.5 ± 2.9 | 14.2 ± 3.6 | 13.3 ± 3.3 |
| TAD | 20.4 ± 5.0 | 18.2 ± 4.8 | 16.5 ± 3.9 | 18.5 ± 4.8 |
| Lateral overhang | 14% | 8% | 8% | 10% |
| PFNA | Gamma | U-Blade | Total | |
|---|---|---|---|---|
| Number | 1 | 3 | 2 | 6 |
| Parker’s ratio AP | 39 | 48.7 ± 5.6 | 50.5 ± 3.5 | 47.9 ± 5.8 |
| Parker’s ratio LAT | 67 | 58.3 ± 7.6 | 60.5 ± 4.9 | 56.6 ± 11.6 |
| CalTAD | 18.7 | 14.6 ± 1.4 | 15.0 ± 1.4 | 15.3 ± 1.9 |
| TAD | 32.8 * | 18.3 ± 5.9 | 17.1 ± 4.3 | 20.0 ± 7.3 |
| Lateral overhang | 6% | 11% | 7% | 9% |
| PFNA | Gamma | U-Blade | Total | |
|---|---|---|---|---|
| Implant breakage | 3 | 3 | ||
| lateralization | 1 | 2 | 3 | |
| Wound infection | 1 * | 1 * | 2 | |
| Secondary femur fracture | 1 | 1 | 2 | |
| Non-union | 1 | 1 | ||
| Overall % | 2.3% | 8.5% | 2.9% | 4.6% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lang, N.W.; Breuer, R.; Beiglboeck, H.; Munteanu, A.; Hajdu, S.; Windhager, R.; Widhalm, H.K. Migration of the Lag Screw after Intramedullary Treatment of AO/OTA 31.A2.1-3 Pertrochanteric Fractures Does Not Result in Higher Incidence of Cut-Outs, Regardless of Which Implant Was Used: A Comparison of Gamma Nail with and without U-Blade (RC) Lag Screw and Proximal Femur Nail Antirotation (PFNA). J. Clin. Med. 2019, 8, 615. https://doi.org/10.3390/jcm8050615
Lang NW, Breuer R, Beiglboeck H, Munteanu A, Hajdu S, Windhager R, Widhalm HK. Migration of the Lag Screw after Intramedullary Treatment of AO/OTA 31.A2.1-3 Pertrochanteric Fractures Does Not Result in Higher Incidence of Cut-Outs, Regardless of Which Implant Was Used: A Comparison of Gamma Nail with and without U-Blade (RC) Lag Screw and Proximal Femur Nail Antirotation (PFNA). Journal of Clinical Medicine. 2019; 8(5):615. https://doi.org/10.3390/jcm8050615
Chicago/Turabian StyleLang, Nikolaus Wilhelm, Robert Breuer, Hannes Beiglboeck, Alexandru Munteanu, Stefan Hajdu, Reinhard Windhager, and Harald Kurt Widhalm. 2019. "Migration of the Lag Screw after Intramedullary Treatment of AO/OTA 31.A2.1-3 Pertrochanteric Fractures Does Not Result in Higher Incidence of Cut-Outs, Regardless of Which Implant Was Used: A Comparison of Gamma Nail with and without U-Blade (RC) Lag Screw and Proximal Femur Nail Antirotation (PFNA)" Journal of Clinical Medicine 8, no. 5: 615. https://doi.org/10.3390/jcm8050615
APA StyleLang, N. W., Breuer, R., Beiglboeck, H., Munteanu, A., Hajdu, S., Windhager, R., & Widhalm, H. K. (2019). Migration of the Lag Screw after Intramedullary Treatment of AO/OTA 31.A2.1-3 Pertrochanteric Fractures Does Not Result in Higher Incidence of Cut-Outs, Regardless of Which Implant Was Used: A Comparison of Gamma Nail with and without U-Blade (RC) Lag Screw and Proximal Femur Nail Antirotation (PFNA). Journal of Clinical Medicine, 8(5), 615. https://doi.org/10.3390/jcm8050615






