Incidental Finding of Strut Malapposition Is a Predictor of Late and Very Late Thrombosis in Coronary Bioresorbable Scaffolds
Abstract
1. Introduction
2. Methods
2.1. Objective of the Study
2.2. Patients
- Patients had undergone elective OCT at the end of the implantation procedure, during non-target vessel-staged procedures, or in the setting of elective invasive exams.
- In none of these patients was there evidence of ischemia in the region perfused by the vessel treated with BRS and OCTs had been performed as elective controls after implantation of these novel devices.
- An experienced interventionalist (based on current experts´ recommendations [17]) reviewed the OCT and saw no clinical indication for the re-treatment of these lesions.
2.3. Definitions
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
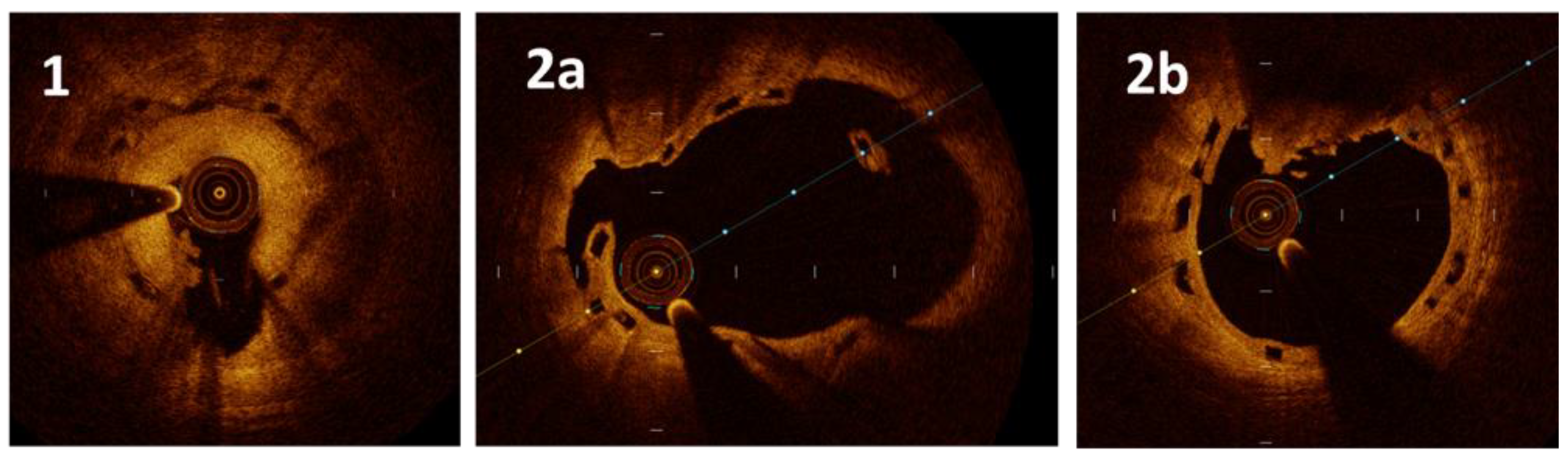
3.2. Optical Coherence Tomography (OCT) Characteristics
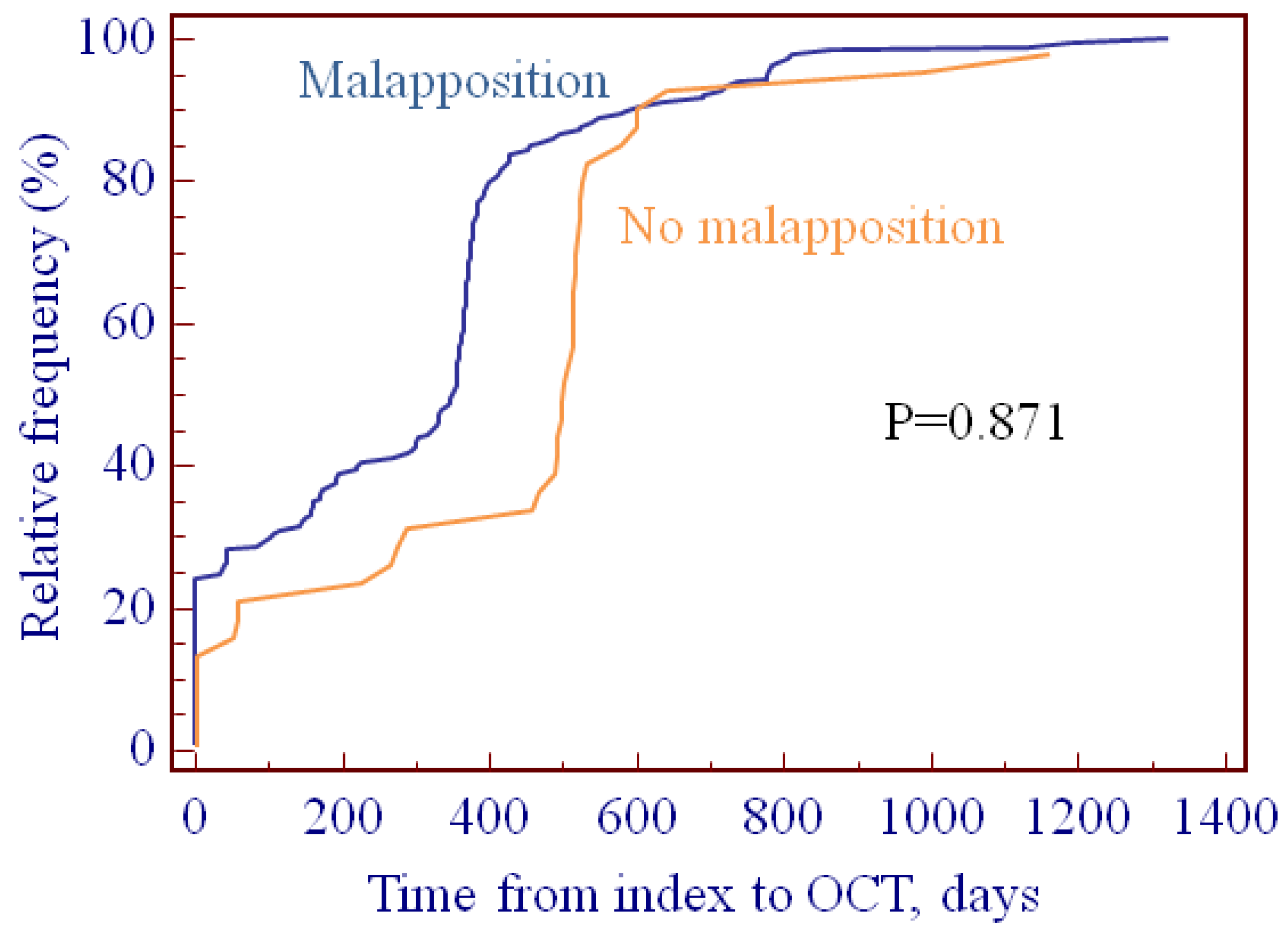
3.3. Analysis of the OCT Predictors of Scaffold Thrombosis
3.4. OCT Evidence at the Time of ScT
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
Appendix A
A.1. Retrospective Cohort: Malapposition at the Time of Scaffold Thrombosis (ScT)
A.2. Results: OCT Evidence at the Time of ScT
References
- Wiebe, J.; Nef, H.M.; Hamm, C.W. Current status of bioresorbable scaffolds in the treatment of coronary artery disease. J. Am. Coll. Cardiol. 2014, 64, 2541–2551. [Google Scholar] [CrossRef]
- Ali, Z.A.; Gao, R.; Kimura, T.; Onuma, Y.; Kereiakes, D.J.; Ellis, S.G.; Chevalier, B.; Vu, M.T.; Zhang, Z.; Simonton, C.A.; et al. Three-year outcomes with the absorb bioresorbable scaffold: individual-patient-data meta-analysis from the ABSORB randomized trials. Circulation 2018, 137, 464–479. [Google Scholar] [CrossRef]
- Arroyo, D.; Gendre, G.; Schukraft, S.; Kallinikou, Z.; Muller, O.; Baeriswyl, G.; Stauffer, J.C.; Goy, J.J.; Togni, M.; Cook, S.; et al. Comparison of everolimus- and biolimus-eluting coronary stents with everolimus-eluting bioresorbable vascular scaffolds: Two-year clinical outcomes of the EVERBIO II trial. Int. J. Cardiol. 2017, 243, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Collet, C.; Asano, T.; Miyazaki, Y.; Tenekecioglu, E.; Katagiri, Y.; Sotomi, Y.; Cavalcante, R.; de Winter, R.J.; Kimura, T.; Gao, R.; et al. Late thrombotic events after bioresorbable scaffold implantation: a systematic review and meta-analysis of randomized clinical trials. Eur. Heart J. 2017, 38, 2559–2566. [Google Scholar] [CrossRef] [PubMed]
- Polimeni, A.; Anadol, R.; Munzel, T.; Indolfi, C.; De Rosa, S.; Gori, T. Long-term outcome of bioresorbable vascular scaffolds for the treatment of coronary artery disease: A meta-analysis of RCTs. BMC Cardiovasc. Disord. 2017, 17, 147. [Google Scholar] [CrossRef] [PubMed]
- Wykrzykowska, J.J.; Kraak, R.P.; Hofma, S.H.; van der Schaaf, R.J.; Arkenbout, E.K.; AJ, I.J.; Elias, J.; van Dongen, I.M.; Tijssen, R.Y.G.; Koch, K.T.; et al. Bioresorbable scaffolds versus metallic stents in routine PCI. N. Engl. J. Med. 2017, 376, 2319–2328. [Google Scholar] [CrossRef]
- Puricel, S.; Cuculi, F.; Weissner, M.; Schmermund, A.; Jamshidi, P.; Nyffenegger, T.; Binder, H.; Eggebrecht, H.; Munzel, T.; Cook, S.; et al. Bioresorbable coronary scaffold thrombosis: Multicenter comprehensive analysis of clinical presentation, mechanisms, and predictors. J. Am. Coll. Cardiol. 2016, 67, 921–931. [Google Scholar] [CrossRef] [PubMed]
- Ellis, S.G.; Gori, T.; Serruys, P.W.; Nef, H.; Steffenino, G.; Brugaletta, S.; Munzel, T.; Feliz, C.; Schmidt, G.; Sabate, M.; et al. Clinical, angiographic, and procedural correlates of very late absorb scaffold thrombosis: Multistudy registry results. JACC Cardiovasc. Interv. 2018, 11, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Gori, T.; Weissner, M.; Gonner, S.; Wendling, F.; Ullrich, H.; Ellis, S.; Anadol, R.; Polimeni, A.; Munzel, T. Characteristics, predictors, and mechanisms of thrombosis in coronary bioresorbable scaffolds: Differences between early and late events. JACC Cardiovasc. Interv. 2017, 10, 2363–2371. [Google Scholar] [CrossRef] [PubMed]
- Foin, N.; Gutierrez-Chico, J.L.; Nakatani, S.; Torii, R.; Bourantas, C.V.; Sen, S.; Nijjer, S.; Petraco, R.; Kousera, C.; Ghione, M.; et al. Incomplete stent apposition causes high shear flow disturbances and delay in neointimal coverage as a function of strut to wall detachment distance: Implications for the management of incomplete stent apposition. Circ. Cardiovasc. Interv. 2014, 7, 180–189. [Google Scholar] [CrossRef]
- Foin, N.; Lu, S.; Ng, J.; Bulluck, H.; Hausenloy, D.J.; Wong, P.E.; Virmani, R.; Joner, M. Stent malapposition and the risk of stent thrombosis: Mechanistic insights from an in vitro model. EuroIntervention 2017, 13, e1096–e1098. [Google Scholar] [CrossRef]
- Anadol, R.; Gori, T. The mechanisms of late scaffold thrombosis. Clin. Hemorheol. Microcirc. 2017, 67, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Cuculi, F.; Puricel, S.; Jamshidi, P.; Valentin, J.; Kallinikou, Z.; Toggweiler, S.; Weissner, M.; Munzel, T.; Cook, S.; Gori, T. Optical coherence tomography findings in bioresorbable vascular scaffolds thrombosis. Circ. Cardiovasc. Interv. 2015, 8, e002518. [Google Scholar] [CrossRef]
- Kraak, R.P.; Kajita, A.H.; Garcia-Garcia, H.M.; Henriques, J.P.S.; Piek, J.J.; Arkenbout, E.K.; van der Schaaf, R.J.; Tijssen, J.G.P.; de Winter, R.J.; Wykrzykowska, J.J. Scaffold thrombosis following implantation of the ABSORB Bvs. in routine clinical practice: Insight into possible mechanisms from optical coherence tomography. Catheter. Cardiovasc. Interv. 2018, 92, E106–E114. [Google Scholar] [CrossRef]
- Raber, L.; Brugaletta, S.; Yamaji, K.; O’Sullivan, C.J.; Otsuki, S.; Koppara, T.; Taniwaki, M.; Onuma, Y.; Freixa, X.; Eberli, F.R.; et al. Very late scaffold thrombosis: Intracoronary imaging and histopathological and spectroscopic findings. J. Am. Coll. Cardiol. 2015, 66, 1901–1914. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, K.; Ueki, Y.; Souteyrand, G.; Daemen, J.; Wiebe, J.; Nef, H.; Adriaenssens, T.; Loh, J.P.; Lattuca, B.; Wykrzykowska, J.J.; et al. Mechanisms of very late bioresorbable scaffold thrombosis: The INVEST registry. J. Am. Coll. Cardiol. 2017, 70, 2330–2344. [Google Scholar] [CrossRef] [PubMed]
- Tamburino, C.; Latib, A.; van Geuns, R.J.; Sabate, M.; Mehilli, J.; Gori, T.; Achenbach, S.; Alvarez, M.P.; Nef, H.; Lesiak, M.; et al. Contemporary practice and technical aspects in coronary intervention with bioresorbable scaffolds: A European perspective. EuroIntervention 2015, 11, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Gori, T.; Jansen, T.; Weissner, M.; Foin, N.; Wenzel, P.; Schulz, E.; Cook, S.; Munzel, T. Coronary evaginations and peri-scaffold aneurysms following implantation of bioresorbable scaffolds: Incidence, outcome, and optical coherence tomography analysis of possible mechanisms. Eur. Heart J. 2016, 37, 2040–2049. [Google Scholar] [CrossRef] [PubMed]
- Gori, T.; Schulz, E.; Hink, U.; Kress, M.; Weiers, N.; Weissner, M.; Jabs, A.; Wenzel, P.; Capodanno, D.; Munzel, T. Clinical, angiographic, functional, and imaging outcomes 12 months after implantation of drug-eluting bioresorbable vascular scaffolds in acute coronary syndromes. JACC Cardiovasc. Interv. 2015, 8, 770–777. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tearney, G.J.; Regar, E.; Akasaka, T.; Adriaenssens, T.; Barlis, P.; Bezerra, H.G.; Bouma, B.; Bruining, N.; Cho, J.M.; Chowdhary, S.; et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: A report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J. Am. Coll. Cardiol. 2012, 59, 1058–1072. [Google Scholar] [CrossRef] [PubMed]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef]
- Kereiakes, D.J.; Ellis, S.G.; Metzger, C.; Caputo, R.P.; Rizik, D.G.; Teirstein, P.S.; Litt, M.R.; Kini, A.; Kabour, A.; Marx, S.O.; et al. 3-Year clinical outcomes with everolimus-eluting bioresorbable coronary scaffolds: The ABSORB III trial. J. Am. Coll. Cardiol. 2017, 70, 2852–2862. [Google Scholar] [CrossRef]
- Ellis, S.G.; Steffenino, G.; Kereiakes, D.J.; Stone, G.W.; van Geuns, R.J.; Abizaid, A.; Nef, H.; Cortese, B.; Testa, L.; Menichelli, M.; et al. Clinical, angiographic, and procedural correlates of acute, subacute, and late absorb scaffold thrombosis. JACC Cardiovasc. Interv. 2017, 10, 1809–1815. [Google Scholar] [CrossRef]
- Ortega-Paz, L.; Brugaletta, S.; Sabate, M. Impact of PSP technique on clinical outcomes following bioresorbable scaffolds implantation. J. Clin. Med. 2018, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Paz, L.; Capodanno, D.; Gori, T.; Nef, H.; Latib, A.; Caramanno, G.; Di Mario, C.; Naber, C.; Lesiak, M.; Capranzano, P.; et al. Predilation, sizing and post-dilation scoring in patients undergoing everolimus-eluting bioresorbable scaffold implantation for prediction of cardiac adverse events: Development and internal validation of the PSP score. EuroIntervention 2017, 12, 2110–2117. [Google Scholar] [CrossRef] [PubMed]
- Adriaenssens, T.; Joner, M.; Godschalk, T.C.; Malik, N.; Alfonso, F.; Xhepa, E.; De Cock, D.; Komukai, K.; Tada, T.; Cuesta, J.; et al. Optical coherence tomography findings in patients with coronary stent thrombosis: A report of the PRESTIGE consortium (Prevention of late stent thrombosis by an interdisciplinary global European effort). Circulation 2017, 136, 1007–1021. [Google Scholar] [CrossRef] [PubMed]
- Souteyrand, G.; Amabile, N.; Mangin, L.; Chabin, X.; Meneveau, N.; Cayla, G.; Vanzetto, G.; Barnay, P.; Trouillet, C.; Rioufol, G.; et al. Mechanisms of stent thrombosis analysed by optical coherence tomography: Insights from the national PESTO French registry. Eur. Heart J. 2016, 37, 1208–1216. [Google Scholar] [CrossRef]
- Chesnutt, J.K.; Han, H.C. Computational simulation of platelet interactions in the initiation of stent thrombosis due to stent malapposition. Phys. Biol. 2016, 13, 016001. [Google Scholar] [CrossRef] [PubMed]
- Poon, E.K.W.; Thondapu, V.; Hayat, U.; Barlis, P.; Yap, C.Y.; Kuo, P.H.; Wang, Q.; Ma, J.; Zhu, S.J.; Moore, S.; et al. Elevated blood viscosity and microrecirculation resulting from coronary stent malapposition. J. Biomech. Eng. 2018, 140. [Google Scholar] [CrossRef] [PubMed]
- Vorpahl, M.; Nakano, M.; Perkins, L.E.; Otsuka, F.; Jones, R.; Acampado, E.; Lane, J.P.; Rapoza, R.; Kolodgie, F.D.; Virmani, R. Vascular healing and integration of a fully bioresorbable everolimus-eluting scaffold in a rabbit iliac arterial model. EuroIntervention 2014, 10, 833–841. [Google Scholar] [CrossRef]
- Gomez-Lara, J.; Diletti, R.; Brugaletta, S.; Onuma, Y.; Farooq, V.; Thuesen, L.; McClean, D.; Koolen, J.; Ormiston, J.A.; Windecker, S.; et al. Angiographic maximal luminal diameter and appropriate deployment of the everolimus-eluting bioresorbable vascular scaffold as assessed by optical coherence tomography: An ABSORB cohort B trial sub-study. EuroIntervention 2012, 8, 214–224. [Google Scholar] [CrossRef] [PubMed]
- Harrell, F.E., Jr.; Lee, K.L.; Pollock, B.G. Regression models in clinical studies: Determining relationships between predictors and response. J. Natl. Cancer Inst. 1988, 80, 1198–1202. [Google Scholar] [CrossRef] [PubMed]
- Taniwaki, M.; Radu, M.D.; Zaugg, S.; Amabile, N.; Garcia-Garcia, H.M.; Yamaji, K.; Jorgensen, E.; Kelbaek, H.; Pilgrim, T.; Caussin, C.; et al. Mechanisms of very late drug-eluting stent thrombosis assessed by optical coherence tomography. Circulation 2016, 133, 650–660. [Google Scholar] [CrossRef] [PubMed]

| Baseline Characteristic | Late or Very Late Scaffold Thrombosis ScT (n = 7) | No ScT (n = 190) | p |
|---|---|---|---|
| Age (years) | 58.3 ± 9.1 | 61.8 ± 11.9 | 0.37 |
| Male Sex (%) | 85.7 | 81.6 | 0.78 |
| Hypertension (%) | 100 | 77.9 | 0.16 |
| Diabetes mellitus (%) | 14.3 | 20.5 | 0.69 |
| Current smoker (%) | 43.9 | 36.8 | 0.74 |
| Family history (%) | 14.3 | 30.0 | 0.37 |
| Hyperlipoproteinaemia (%) | 43.9 | 47.4 | 0.81 |
| Prior revascularization (%) | 71.4 | 34.7 | 0.04 * |
| Prior bypass surgery (%) | 0 | 3.7 | 0.06 |
| Prior percutaneous intervention (%) | 71.4 | 33.2 | 0.04 * |
| Prior stroke/TIA (%) | 0 | 3.2 | 0.63 |
| eGFR (mean ± SD, ml/min) | 91.4 ± 30.8 | 85.4 ± 20.2 | 0.74 |
| Left ventricular ejection fraction (mean ± SD, %) | 54.3 ± 7.9 | 54 ± 8.2 | 0.96 |
| Acute coronary syndrome (%) | 71.4 | 51.4 | 0.30 |
| Clinical indication | |||
| - Stable angina (%) | 28.6 | 37.4 | 0.57 |
| - ST-elevation myocardial infarction (%) | 42.9 | 22.1 | 0.29 |
| - Non-ST-elevation myocardial infarction (%) | 28.6 | 24.9 | 0.82 |
| - Unstable angina (%) | 0 | 13.8 | 0.20 |
| Number of vessels treated | 1.6 ± 0.8 | 1.1 ± 0.4 | 0.01 * |
| Number of scaffolds per lesion | 1.0 ± 0 | 1.2 ± 0.5 | 0.25 |
| Number of scaffolds per patient | 1.7 ± 1.1 | 1.3 ± 0.7 | 0.23 |
| Chronic total occlusion (%) | 0 | 6.8 | 0.47 |
| Lesion type AHA/ACC classification B/C2 (%) | 85.7 | 63.5 | 0.22 |
| Dual antiplatelet therapy (DAPT) | 0.58 | ||
| - Clopidogrel (%) | 14.3 | 31.2 | |
| - Prasugrel (%) | 14.3 | 52.4 | |
| - Ticagrelor (%) | 71.4 | 16.4 |
| Optical Coherence Finding | Late or Very Late ScT (n = 7) | No ScT (n = 190) | p |
|---|---|---|---|
| Number of struts | 1080 ± 485 | 1059 ± 837 | 0.38 |
| Number of frames | 116.1 ± 84 | 120.4 ± 49 | 0.24 |
| Pullback length (mm) | 19.1 ± 8.1 | 21.1 ± 5.4 | 0.35 |
| Maximum lumen area (mm2) | 12.3 ± 2.5 | 9.1 ± 3.1 | 0.005 * |
| Minimum lumen area (mm2) | 6.3 ± 1.0 | 4.8 ± 1.9 | 0.02 * |
| Average lumen area (mm2) | 8.96 ± 1.03 | 6.6 ± 2.20 | 0.003 * |
| Maximum lumen asymmetry | 0.28 ± 0.10 | 0.27 ± 0.11 | 0.82 |
| Maximum scaffold asymmetry | 0.24 ± 0.012 | 0.24 ± 0.09 | 0.91 |
| Maximum lumen eccentricity | 0.62 ± 0.11 | 0.66 ± 0.10 | 0.29 |
| Maximum scaffold eccentricity | 0.66 ± 0.10 | 0.72 ± 0.08 | 0.07 |
| Peri-strut low intensity area (PSLIA) (%) | 20.0 | 5.4 | 0.18 |
| Microvessels (%) | 42.9 | 31.0 | 0.51 |
| Fractures (%) | 57.1 | 33.5 | 0.20 |
| Uncovered scaffold struts (%) | 42.9 | 5.8 | <0.001 * |
| Malapposition (>30% in one frame, without side) (%) | 71.4 | 15.3 | <0.001 * |
| Any malapposition per patient (%) | 85.7 | 20.1 | <0.001 * |
| Malapposition length (mm) | 2.33 ± 1.5 | 2.76 ± 1.8 | 0.67 |
| Malapposition maximum area (mm2) | 1.56 ± 0.69 | 2.3 ± 1.9 | 0.64 |
| Number of malapposed segments | 1.83 ± 1.17 | 1.7 ± 0.99 | 0.88 |
| Malapposition distance (mm) | 0.52 ± 0.25 | 0.89 ± 0.77 | 0.22 |
| Evagination (%) | 57.1 | 27.5 | 0.08 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boeder, N.F.; Weissner, M.; Blachutzik, F.; Ullrich, H.; Anadol, R.; Tröbs, M.; Münzel, T.; Hamm, C.W.; Dijkstra, J.; Achenbach, S.; et al. Incidental Finding of Strut Malapposition Is a Predictor of Late and Very Late Thrombosis in Coronary Bioresorbable Scaffolds. J. Clin. Med. 2019, 8, 580. https://doi.org/10.3390/jcm8050580
Boeder NF, Weissner M, Blachutzik F, Ullrich H, Anadol R, Tröbs M, Münzel T, Hamm CW, Dijkstra J, Achenbach S, et al. Incidental Finding of Strut Malapposition Is a Predictor of Late and Very Late Thrombosis in Coronary Bioresorbable Scaffolds. Journal of Clinical Medicine. 2019; 8(5):580. https://doi.org/10.3390/jcm8050580
Chicago/Turabian StyleBoeder, Niklas F., Melissa Weissner, Florian Blachutzik, Helen Ullrich, Remzi Anadol, Monique Tröbs, Thomas Münzel, Christian W. Hamm, Jouke Dijkstra, Stephan Achenbach, and et al. 2019. "Incidental Finding of Strut Malapposition Is a Predictor of Late and Very Late Thrombosis in Coronary Bioresorbable Scaffolds" Journal of Clinical Medicine 8, no. 5: 580. https://doi.org/10.3390/jcm8050580
APA StyleBoeder, N. F., Weissner, M., Blachutzik, F., Ullrich, H., Anadol, R., Tröbs, M., Münzel, T., Hamm, C. W., Dijkstra, J., Achenbach, S., Nef, H. M., & Gori, T. (2019). Incidental Finding of Strut Malapposition Is a Predictor of Late and Very Late Thrombosis in Coronary Bioresorbable Scaffolds. Journal of Clinical Medicine, 8(5), 580. https://doi.org/10.3390/jcm8050580







