Systematic Review of Capnography with Mask Ventilation during Cardiopulmonary Resuscitation Maneuvers
Abstract
:1. Introduction
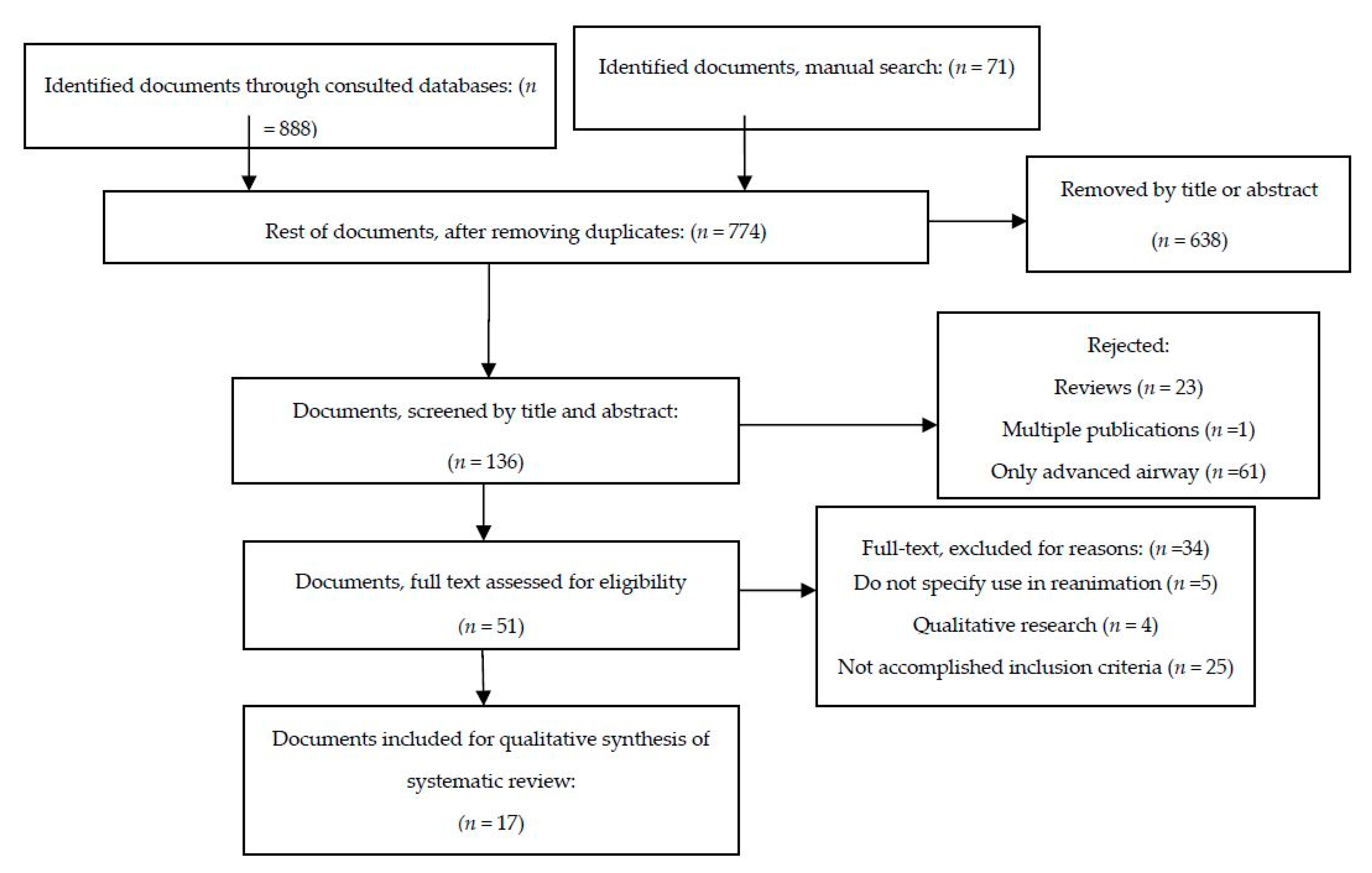
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
6. Recommendations for Practice
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Monsieurs, K.G.; Nolan, J.P.; Bossaert, L.L.; Greif, R.; Maconochie, I.K.; Nikolaou, N.I.; Perkins, G.D.; Soar, J.; Truhlář, A.; Wyllie, J.; et al. European Resuscitation Council Guidelines for Resuscitation 2015. Section 1. Executive summary. Resuscitation 2015, 95, 1–80. [Google Scholar] [CrossRef] [PubMed]
- Baskett, P.J.F.; Bossaert, L.; Carli, P.; Chamberlain, D.; Dick, W.; Nolan, J.P.; Parr, M.J.A. Guidelines for the advanced management of the airway and ventilation during resuscitation. A statement by the Airway and Ventilation Management of the Working Group of the European Resuscitation Council. Resuscitation 1996, 31, 201–230. [Google Scholar] [CrossRef]
- Deakin, C.D.; Nolan, J.P.; Soar, J.; Sunde, K.; Koster, R.W.; Smith, G.B.; Perkins, G.D. European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. Resuscitation 2010, 81, 1305–1352. [Google Scholar] [CrossRef] [PubMed]
- Callaway, C.W.; Soar, J.; Aibiki, M.; Bottiger, B.W.; Brooks, S.C.; Deakin, C.D.; Donnino, M.W.; Drajer, S.; Kloeck, W.; Morley, P.T.; et al. Part 4: Advanced Life Support: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2015, 132, S84–S145. [Google Scholar] [CrossRef] [PubMed]
- Baskett, P.J.F.; Bossaert, L.; Carli, P.; Chamberlain, D.; Dick, W.; Nolan, P.; Parr, M.J.A. Guidelines for the basic management of the airway and ventilation during resuscitation. Resuscitation 1996, 31, 187–200. [Google Scholar] [CrossRef]
- ILCOR, I.L.C. on R. Part 4: Advanced life support. Resuscitation 2005, 67, 213–247. [Google Scholar]
- Nicolás Arriaza, H.; María Mercedes Aguirre, C. Monitorización de la calidad de la reanimación cardiopulmonar. Rev. Chil. Anest. 2012, 41, 42–45. [Google Scholar]
- Davis, D.P. Quantitative capnometry as a critical resuscitation tool. J. Trauma Nurs. Off. J. Soc. Trauma Nurses 2005, 12, 40–42. [Google Scholar] [CrossRef]
- Díez-Picazo, L.D.; Barrado-Muñoz, L.; Blanco-Hermo, P.; Barroso-Matilla, S.; Espinosa Ramírez, S. La capnografía en los servicios de emergencia médica. Semer. Med. Fam. 2009, 35, 138–143. [Google Scholar] [CrossRef]
- Soleimanpour, H.; Gholipouri, C.; Golzari, S.E.; Rahmani, F.; Sabahi, M. Capnography in the Emergency Department. Available online: http://www.omicsgroup.org/journals/capnography-in-the-emergency-department -2165-7548.1000e123.pdf (accessed on 14 February 2016).
- Hawkes, G.A.; Kelleher, J.; Ryan, C.A.; Dempsey, E.M. A review of carbon dioxide monitoring in preterm newborns in the delivery room. Resuscitation 2014, 85, 1315–1319. [Google Scholar] [CrossRef]
- Bhende, M.S.; LaCovey, D.C. End-tidal carbon dioxide monitoring in the prehospital setting. Prehospital Emerg. Care Off. J. Natl. Assoc. EMS Physicians Natl. Assoc. State EMS Dir. 2001, 5, 208–213. [Google Scholar]
- Kodali, B.S.; Urman, R.D. Capnography during cardiopulmonary resuscitation: Current evidence and future directions. J. Emerg. Trauma. Shock 2014, 7, 332–340. [Google Scholar]
- Pearce, A.K.; Davis, D.P.; Minokadeh, A.; Sell, R.E. Initial end-tidal carbon dioxide as a prognostic indicator for inpatient PEA arrest. Resuscitation 2015, 92, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Soar, J.; Nolan, J.P.; Böttiger, B.W.; Perkins, G.D.; Lott, C.; Carli, P.; Pellis, T.; Sandroni, C.; Skrifvars, M.B.; Smith, G.B.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015, 95, 100–147. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group, P.-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López de Argumedo, M.; Reviriego, E.; Andrío, E.; Rico, R.; Sobradillo, N.; Hurtado de Saracho, I. Revisión externa y validación de instrumentos metodológicos para la Lectura Crítica y la síntesis de la evidencia científica. Madrid: Plan Nacional para el SNS del MSC. Servicio de Evaluación de Tecnologías Sanitarias del País Vasco (Osteba); 2006. Inform. Available online: http://www.lecturacritica.com/es/acerca.php (accessed on 9 April 2017).
- Nakatani, K.; Yukioka, H.; Fujimori, M.; Maeda, C.; Noguchi, H.; Ishihara, S.; Yamanaka, I.; Tase, C. Utility of colorimetric end-tidal carbon dioxide detector for monitoring during prehospital cardiopulmonary resuscitation. Am. J. Emerg. Med. 1999, 17, 203–206. [Google Scholar] [CrossRef]
- Pahuja, A.; Hunt, K.; Murthy, V.; Bhat, P.; Bhat, R.; Milner, A.D.; Greenough, A. Relationship of resuscitation, respiratory function monitoring data and outcomes in preterm infants. Eur. J. Pediatr. 2018, 177, 1617–1624. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, G.A.; Finn, D.; Kenosi, M.; Livingstone, V.; O’Toole, J.M.; Boylan, G.B.; O’Halloran, K.D.; Ryan, A.C.; Dempsey, E.M. A Randomized Controlled Trial of End-Tidal Carbon Dioxide Detection of Preterm Infants in the Delivery Room. J. Pediatr. 2017, 182, 74–78. [Google Scholar] [CrossRef]
- Hawkes, G.A.; Kenosi, M.; Finn, D.; O’Toole, J.M.; O’Halloran, K.D.; Boylan, G.B.; Ryan, A.C.; Dempsey, E.M. Delivery room end tidal CO2 monitoring in preterm infants <32 weeks. Arch. Dis. Child. Fetal Neonatal Ed. 2016, 101, F62–F65. [Google Scholar]
- Ngan, A.Y.; Cheung, P.-Y.; Hudson-Mason, A.; O’Reilly, M.; van Os, S.; Kumar, M.; Aziz, K.; Schmolzer, G.M. Using exhaled CO2 to guide initial respiratory support at birth: A randomised controlled trial. Arch. Dis. Child. 2017, 102, F525–F531. [Google Scholar] [CrossRef]
- Thallinger, M.; Ersdal, H.L.; Francis, F.; Yeconia, A.; Mduma, E.; Kidanto, H.; Linde, J.E.; Eilevstjønn, J.; Gunnes, N.; Størdal, K. Born not breathing: A randomised trial comparing two self-inflating bag-masks during newborn resuscitation in Tanzania. Resuscitation 2017, 116, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Murthy, V.; D’Costa, W.; Shah, R.; Fox, G.F.; Campbell, M.E.; Milner, A.D.; Greenough, A. Prematurely born infants’ response to resuscitation via an endotracheal tube or a face mask. Early Hum. Dev. 2015, 91, 235–238. [Google Scholar] [CrossRef]
- Mizumoto, H.; Iki, Y.; Yamashita, S.; Hata, D. Expiratory CO2 as the first sign of successful ventilation during neonatal resuscitation. Pediatr. Int. 2015, 57, 186–188. [Google Scholar] [CrossRef]
- Blank, D.; Rich, W.; Leone, T.; Garey, D.; Finer, N. Pedi-cap color change precedes a significant increase in heart rate during neonatal resuscitation. Resuscitation 2014, 85, 1568–1572. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.Y.; Rich, W.; Finer, N.N.; Leone, T.A. Quantitative end-tidal carbon dioxide monitoring in the delivery room: A randomized controlled trial. J. Pediatr. 2013, 163, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Hooper, S.B.; Fouras, A.; Siew, M.L.; Wallace, M.J.; Kitchen, M.J.; Pas, A.B. t.; Klingenberg, C.; Lewis, R.A.; Davis, P.G.; Morley, C.J.; et al. Expired CO2 Levels Indicate Degree of Lung Aeration at Birth. PLoS ONE 2013, 8, e70895. [Google Scholar] [CrossRef]
- Murthy, V.; O’Rourke-Potocki, A.; Dattani, N.; Fox, G.F.; Campbell, M.E.; Milner, A.D.; Greenough, A. End tidal carbon dioxide levels during the resuscitation of prematurely born infants. Early Hum. Dev. 2012, 88, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Finer, N.N.; Rich, W.; Wang, C.; Leone, T. Airway Obstruction During Mask Ventilation of Very Low Birth Weight Infants During Neonatal Resuscitation. Pediatrics 2009, 123, 865–869. [Google Scholar] [CrossRef] [PubMed]
- Palme-Kilander, C.; Tunell, R. Pulmonary gas exchange during facemask ventilation immediately after birth. Arch. Dis. Child. 1993, 68, 11–16. [Google Scholar] [CrossRef]
- Leturiondo, M.; Ruiz de Gauna, S.; Ruiz, J.M.; Julio Gutiérrez, J.; Leturiondo, L.A.; González-Otero, D.M.; Russell, J.K.; Zive, D.; Daya, M. Influence of chest compression artefact on capnogram-based ventilation detection during out-of-hospital cardiopulmonary resuscitation. Resuscitation 2018, 124, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Davis, D.P.; Sell, R.E.; Wilkes, N.; Sarno, R.; Husa, R.D.; Castillo, E.M.; Lawrence, B.; Fisher, R.; Brainard, C.; Dunford, J.V. Electrical and mechanical recovery of cardiac function following out-of-hospital cardiac arrest. Resuscitation 2013, 84, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Hess, D.; Eitel, D. Monitoring during resuscitation. Respir. Care 1992, 37, 739–768. [Google Scholar] [PubMed]
| Author/year | Study Design | Total N/BVM Ventilated N | Location/Cause of Cardiac Arrest | Professional Assisting | Type of Capnography | Outcome | Time of End-tidal CO2 Measurement | Evidence Level USPSTF |
|---|---|---|---|---|---|---|---|---|
| Leturiondo et al. 2017 | Observational retrospective | 232/7 | Out-of-hospital cardiac arrest | Paramedics | Microstream | Distortion of capnogram by chest compression | 20 min | III |
| Pearce et al. 2015 | Observational retrospective | 50/NK | Intra-hospital cardiac arrest by PEA/asystole | A multidisciplinary intra-hospital cardiac arrest team | Mainstream | ROSC and survival at discharge from hospital | Continuous during the first 10 min of cardiac arrest | Not classifiable * |
| Davis et al. 2013 | Observational prospective | 145/NK | Out-of-hospital cardiac arrest | Paramedics | Did not specify | ROSC and correlation with heart rate values | Before, during, and after pauses to check pulse: every 2 min | Not classifiable * |
| Nakatani et al. 1999 | Observational prospective multicentric | 121/48 | Non-traumatic out-of-hospital cardiac arrest | Emergency technicians | Colorimetric | ROSC, survival at admission | 7 to 15 min | II-3 |
| Author/year | Study Design | Total N/Mask Ventilated | Gestational Age | Professional Assisting | Type of Capnography | Outcome | Time of End-tidal CO2 Measurement | Evidence Level USPSTF |
|---|---|---|---|---|---|---|---|---|
| Pahuja et al. 2018 | Observational retrospective | 70 | Preterm | Clinicians | Mainstream | Incidence of intraventricular hemorrhage and bronchopulmonary dysplasia | Continuous during resuscitation | III |
| Hawkes et al. 2017 | Observational prospective | 59 | Preterm | Physicians | Colorimetric and Microstream | Normocarbia within the first hour of life. | Continuous during delivery room ventilation | I |
| Ngan et al. 2017 | Randomized Clinical Trial | 162 | Preterm | Multidisciplinary delivery team | Mainstream | During sustained inflation or positive pressure ventilation | Continuous, during first 60 s | I |
| Thallinger et al. 2017 | Randomized Clinical Trial | 328 | Term | Midwives and nurse anesthetists | Microstream | Tidal volumes and mask leak. Airway pressures and tidal volume comparing 2 devices | 10 min | I |
| Hawkeset al. 2016 | Observational prospective | 35/29 | Preterm | Unspecified | Microstream | Feasibility of EtCO2 monitoring, normocapnia on admission neonatal intensive care unit | Continuous, during first 10 min | III |
| Murthy et al. 2015 | Observational prospective | 35/15 | Preterm | Unspecified | Mainstream | Effectiveness active inflation, tidal volume and pressures. | During 5 first inflations | III |
| Mizumoto et al. 2015 | Observational prospective | 15/7 | Preterm | Pediatricians and nurses | Mainstream | Increase of heart rate and quality of ventilation | Up to 3 min from delivery. | III |
| Blank et al. 2014 | Observational retrospective | 41 | 78% preterm | Multidisciplinary delivery team | Colorimetric | Increase of heart rate | When detector turns to yellow (EtCO2 > 15 mmHg) | III |
| Kong et al. 2013 | Randomized Clinical Trial | 48 | Preterm | Multidisciplinary delivery team | Mainstream and colorimetric | Correlation PCO2 levels in blood gas | Average from last 5 ventilations | I |
| Hooperet al. 2013 | Observational prospective | 10 | Preterm | Multidisciplinary delivery team | Mainstream | Increase of heart rate and quality of ventilation, relationship with tidal volume | Continuous, not specified duration | III |
| Murthy et al. 2012 | Observational prospective | 40 | Preterm | Unspecified | Mainstream | First respiratory effort and tidal volume | Since first inspiratory effort | III |
| Fineret al. 2009 | Observational retrospective | 24 | Preterm | Multidisciplinary delivery team | Colorimetric | Determining if airway was patent | Continuous, not specified duration | III |
| Palme-Kilander and Turner. 1993 | Observational prospective | 30/28 | Term | Unspecified | Beckman Liston Becker II (volumetric) | Increase of heart rate and quality of ventilation | Every 15 s. Up to 5 min | III |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cereceda-Sánchez, F.J.; Molina-Mula, J. Systematic Review of Capnography with Mask Ventilation during Cardiopulmonary Resuscitation Maneuvers. J. Clin. Med. 2019, 8, 358. https://doi.org/10.3390/jcm8030358
Cereceda-Sánchez FJ, Molina-Mula J. Systematic Review of Capnography with Mask Ventilation during Cardiopulmonary Resuscitation Maneuvers. Journal of Clinical Medicine. 2019; 8(3):358. https://doi.org/10.3390/jcm8030358
Chicago/Turabian StyleCereceda-Sánchez, Francisco José, and Jesús Molina-Mula. 2019. "Systematic Review of Capnography with Mask Ventilation during Cardiopulmonary Resuscitation Maneuvers" Journal of Clinical Medicine 8, no. 3: 358. https://doi.org/10.3390/jcm8030358
APA StyleCereceda-Sánchez, F. J., & Molina-Mula, J. (2019). Systematic Review of Capnography with Mask Ventilation during Cardiopulmonary Resuscitation Maneuvers. Journal of Clinical Medicine, 8(3), 358. https://doi.org/10.3390/jcm8030358






