Effectiveness of the Botulinum Toxin for Treating Sialorrhea in Patients with Parkinson’s Disease: A Systematic Review
Abstract
1. Introduction
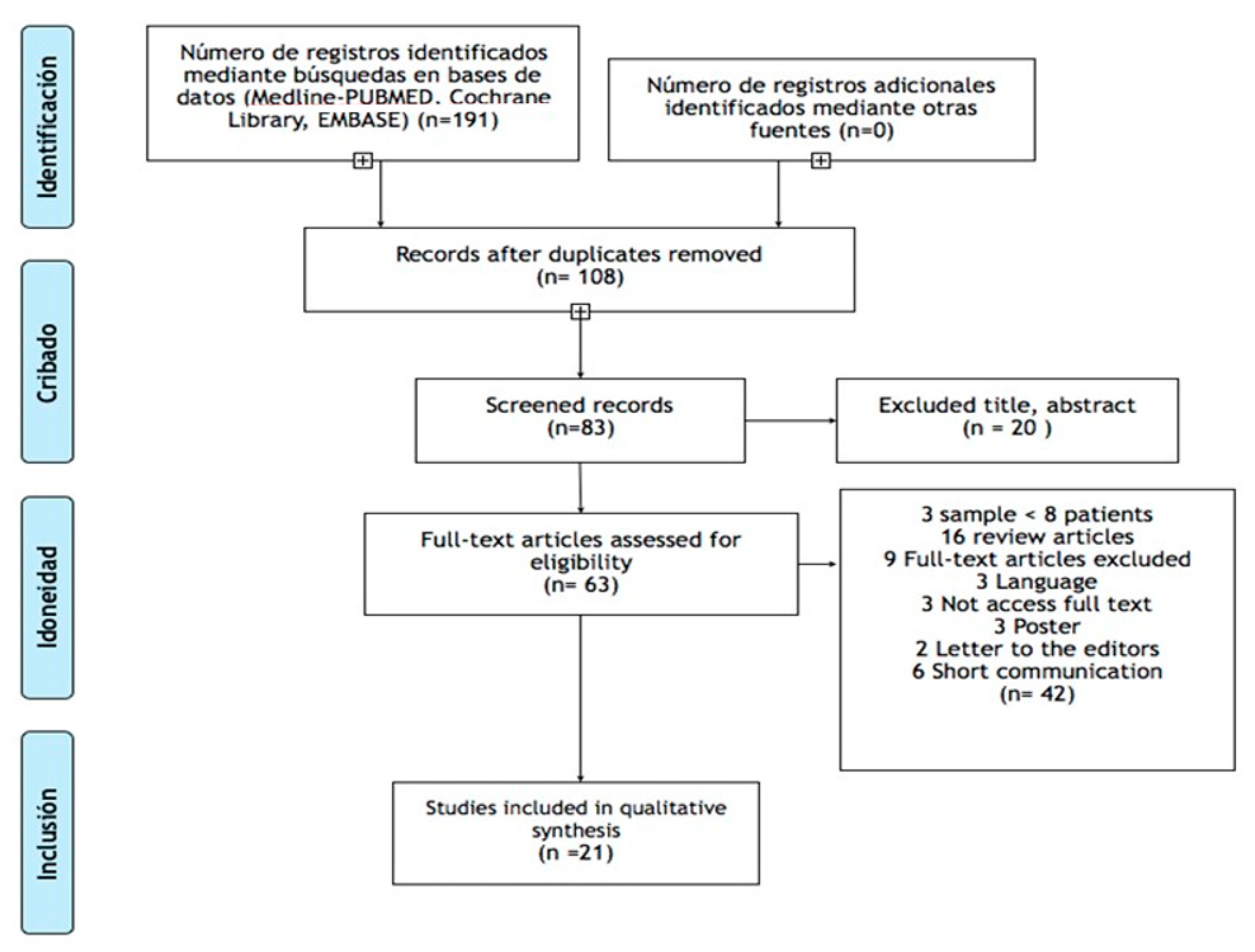
2. Materials and Methods
2.1. Focused Methodology
2.2. Search Strategy
2.3. Selection Criteria
2.4. Outcome Measurement Type
3. Outcomes
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Connolly, B.S.; Lang, A.E. Pharmacological treatment of Parkinson disease: A review. JAMA 2014, 30, 1670–1683. [Google Scholar] [CrossRef] [PubMed]
- Seppi, K.; Ray Chaudhuri, K.; Coelho, M.; Fox, S.H.; Katzenschlager, R.; Perez Lloret, S.; Weintraub, D.; Sampaio, C.; The collaborators of the Parkinson’s Disease Update on Non-Motor Symptoms Study Group on behalf of the Movement Disorders Society Evidence-Based Medicine Committee. Update on treatments for nonmotor symptoms of Parkinson’s disease-an evidence-based medicine review. Mov. Disord. 2019. [Google Scholar] [CrossRef] [PubMed]
- Møller, E.; Karlsborg, M.; Bardow, A.; Lykkeaa, J.; Nissen, F.H.; Bakke, M. Treatment of severe drooling with botulinum toxin in amyotrophic lateral sclerosis and Parkinson’s disease: Efficacy and possible mechanisms. Acta Odontol. Scand. 2011, 69, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Bruno, V.A.; Fox, S.H.; Mancini, D.; Miyasaki, J.M. Botulinum Toxin Use in Refractory Pain and Other Symptoms in Parkinsonism. Can. J. Neurol. Sci. 2016, 43, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F. Botulinum toxin in parkinsonism: The when, how, and which for botulinum toxin injections. Toxicon 2018, 147, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Chinnapongse, R.; Gullo, K.; Nemeth, P.; Zhang, Y.; Griggs, L. Safety and Efficacy of Botulinum Toxin Type B for Treatment of Sialorrhea in Parkinson’s Disease: A Prospective Double-Blind Trial. Mov. Disord. 2012, 27, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Caravaca, M.T.; Cáceres-Redondo, M.T.; Huertas-Fernández, I.; Vargas-González, L.; Carrillo, F.; Carballo, M.; Mir, P. The use of botulinum toxin in the treatment of sialorrhea in parkinsonian disorders. Neurol. Sci. 2015, 36, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Jost, W.H. The option of sonographic guidance in Botulinum toxin injection for drooling in Parkinson’s disease. J. Neural Transm. 2016, 123, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Nicaretta, D.H.; de Rosso, A.L.Z.; Maliska, C.; Costa, M.M. Scintigraphic analysis of the parotid glands in patients with sialorrhea and Parkinson’s disease. Parkinsonism Relat. Disord. 2008, 14, 338–341. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.Q.; Ge, N.N.; Zhu, H.H.; Sha, Z.T.; Jiang, T.; Zhang, Y.D.; Tian, Y.Y. Dihydroergotoxine mesylate for the treatment of sialorrhea in Parkinson’s disease. Parkinsonism Relat. Disord. 2018, 58, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Mazlan, M.; Rajasegaran, S.; Engkasan, J.P.; Nawawi, O.; Goh, J.K.; Freddy, S.J. A Double- Blind Randomized Controlled Trial Investigating the Most Efficacious Dose of Botulinum Toxin-A for Sialorrhea Treatment in Asian Adults with Neurological. Toxins 2015, 7, 3758–3770. [Google Scholar] [CrossRef] [PubMed]
- Lakraj, A.A.; Moghimi, N.; Jabbari, B. Sialorrhea, anatomy, pathophysiology and treatment with emphasis on the role of botulinum toxins. Toxins 2013, 5, 1010–1031. [Google Scholar] [CrossRef] [PubMed]
- Evangelos, A.; Michael, R.; Theodoros, A.; Vasiliki, Z.; Thomas, Z.; Ioannis, E. Volume matters, the influence of different botulinum toxin-A dilutions for sialorrhea in amyotrophic lateral sclerosis. Muscle Nerve 2013, 47, 276–278. [Google Scholar] [CrossRef] [PubMed]
- Guidubaldi, A.; Fasano, A.; Ialongo, T.; Piano, C.; Pompili, M.; Masciana, R.; Siciliani, L.; Sabatelli, M.; Bentivoglio, A.R. Botulinum Toxin A Versus B in Sialorrhea, A Prospective, Randomized, Double-Blind, Crossover Pilot Study in Patients with Amyotrophic Lateral Sclerosis or Parkinson’s Disease. Mov. Disord. 2011, 26, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Møller, E.; Daugaard, D.; Holm, O.; Winge, K.; Bardow, A.; Lykkeaa, J.; Belhage, B.; Bakke, M. Repeated treatments of drooling with botulinum toxin B in neurology. Acta Neurol. Scan. 2015, 131, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Şen, A.; Arpaci, B. Effects of repeated botulinum toxin treatment for sialorrhea in patients with Parkinson’s Disease. Noro-Psikyatri. Arsivi. 2015, 52, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Breheret, R.; Bizon, A.; Jeufroy, C.; Laccourreye, L. Ultrasound-guided botulinum toxin injections for treatment of drooling. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2011, 128, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Narayanaswami, P.; Geisbush, T.; Tarulli, A.; Raynor, E.; Gautam, S.; Tarsy, D.; Gronseth, G. Drooling in Parkinson’s disease: A randomized controlled trial of incobotulinum toxin A and meta-analysis of Botulinum toxins. Parkinsonism Relat. Disord. 2016, 30, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Petracca, M.; Guidubaldi, A.; Ricciardi, L.; Ialongo, T.; Del Grande, A.; Mulas, D.; Di Stasio, E.; Bentivoglio, A.R. Botulinum Toxin A and B in sialorrhea: Long-term data and literature overview. Toxicon 2015, 107, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Lagalla, G.; Millevolte, M.; Capecci, M.; Provinciali, L.; Ceravolo, M.G. Long-lasting benefits of botulinum toxin type B in Parkinson’s disease-related drooling. J. Neurol. 2009, 256, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Tiigimäe-Saar, J.; Taba, P.; Tamme, T. Does Botulinum neurotoxin type A treatment for sialorrhea change oral health? Clin. Oral Investig. 2017, 21, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Svetel, M.; Vasić, M.; Dragasević, N.; Pekmezović, T.; Petrović, I.; Kostić, V. Botulinum toxin in the treatment of sialorrhea. Vojnosanit. Pregl. 2009, 66, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Lagalla, G.; Millevolte, M.; Capecci, M.; Provinciali, L.; Ceravolo, M.G. Botulinum toxin type A for drooling in Parkinson’s disease: A double-blind, randomized, placebo-controlled study. Mov. Disord. 2006, 21, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Nóbrega, A.C.; Rodrigues, B.; Torres, A.C.; Enzo, A.; Melo, A. Does botulinum toxin decrease frequency and severity of sialorrhea in Parkinson’s disease? J. Neurol. Sci. 2007, 253, 85–87. [Google Scholar] [CrossRef] [PubMed]
- Ondo, W.G.; Hunter, C.; Moore, W. A double-blind placebo-controlled trial of botulinum toxin B for sialorrhea in Parkinson’s disease. Neurology 2004, 62, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Mancini, F.; Zangaglia, R.; Cristina, S.; Sommaruga, M.G.; Martignoni, E.; Nappi, G.; Pacchetti, C. Double-blind, placebo-controlled study to evaluate the efficacy and safety of botulinum toxin type A in the treatment of drooling in parkinsonism. Mov. Disord. 2003, 18, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Friedman, A.; Potulska, A. Quantitative assessment of parkinsonian sialorrhea and results of treatment with botulinum toxin. Parkinsonism Relat. Disord. 2001, 7, 329–332. [Google Scholar] [CrossRef]
- Pal, P.K.; Calne, D.B.; Calne, S.; Tsui, J.K. Botulinum toxin A as treatment for drooling saliva in PD. Neurology 2000, 54, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Santamato, A. Botulinum toxin type A in the treatment of sialorrhea in Parkinson’s disease. J. Am. Geriatr. Soc. 2008, 56, 765–767. [Google Scholar] [CrossRef] [PubMed]
- Rosales, R.L.; Bigalke, H.; Dressler, D. Pharmacology of botulinum toxin: Differences between type A preparations. Eur. J. Neurol. 2006, 13 (Suppl. S1), 2–10. [Google Scholar] [PubMed]
- Chauhuri, K.R.; Martínez-Marín, P.; Brown, R.G.; Schapira, A.H.; Strocchi, F.; Sethi, K.; Odin, P.; Brown, R.G.; Koller, W.; Barone, P.; et al. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: The NM-SQuest study. Mov. Disord. 2006, 21, 916–923. [Google Scholar] [CrossRef] [PubMed]
- Chauhuri, K.R.; Martínez-Marín, P.; Brown, R.G.; Sethi, K.; Strocchi, F.; Odin, P. The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: Results from an international pilot study. Mov. Disord. 2007, 22, 1901–1911. [Google Scholar] [CrossRef] [PubMed]
- Kalf, J.G.; Borm, G.F.; de Swart, B.J.; Bloem, B.R.; Zwarts, M.J.; Munneke, M. Reproducibility and validity of patient-rated assessment of speech, swallowing, and saliva control in Parkinson’s disease. Arch. Phys. Med. Rehabil. 2011, 92, 1152–1158. [Google Scholar] [CrossRef] [PubMed]
- Marks, L.; Turner, K.; O’Sullivan, J.; Deighton, B.; Lees, A. Drooling in Parkinson’s disease: A novel speech and language therapy intervention. Int. J. Lang. Commun. Disord. 2001, 36, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Visser, M.; Marinus, J.; Stiggellbout, A.M.; van Hilten, J.J. Assessment of autonomic dysfunction in Parkinson’s disease: The SCOPA-AUT. Mov. Disord. 2004, 19, 1306–1312. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Lloret, S.; Pirán Arce, G.; Rossi, M.; Caivano Nemet, M.L.; Salsamendi, P.; Merello, M. Validation of a new scale for the evaluation of sialorrhea in patients with Parkinson’s disease. Mov. Disord. 2007, 22, 107–111. [Google Scholar]
- Thomas-Stonell, N.; Grrenberg, J. Three treatment approaches and clinical factors in the reduction of drooling. Dysphagia 1988, 3, 73–78. [Google Scholar] [CrossRef] [PubMed]
| Focused Question | Is the Botulinum Toxin Therapy Effective for Treating Sialorrhea in Patients with Parkinson’s Disease? |
|---|---|
| Population | Patients with Parkinson’s disease and sialorrhea |
| Exposure | Patient under treatment with botulinum toxin |
| Outcomes | Administered doses, treatment outcomes, side effects, efficacy of treatment over time |
| Author | Number of Patients | Study Design | Outcome Measurement | Findings | Method to Locate Glands | Side Effects |
|---|---|---|---|---|---|---|
| Lagalla et al. [20] | 36 | A double-blind, randomised, placebo-controlled study | Drooling Severity and Frequency Scale, DSFS, visuo-analogic ratings of familial distress, VAS-FD, and social distress, VAS-SD) and (saliva production by weighing dental rolls. The Global Impression Score (GIS) | BTXB represents a safe and efficacious tool for the management of PD related drooling, ensuring a long-lasting waning of this disabling symptom. | External anatomical landmarks | x |
| Tiigimäe-Saa et al. [21] | 20 | open clinical trial | Drooling was evaluated using subjective scales and objective assessment of salivary flow rate and oral health. | BNT-A injections according to the current protocol can effectively manage sialorrhea while maintaining oral health. | Ultrasound guidance | x |
| Svetelet al. [22]. | 13 | open clinical trial | Activities of Daily Living of the Unified Parkinson’s Disease Rating Scale (UPDRS). | Botulinum toxin-A injections to easily accessible parotid glands, without necessity for ultrasound guidance. | Ultrasound guidance and External anatomical landmarks | x |
| Lagalla et al. [23] | 32 | double-blind, randomized placebo-controlled study | Subjective measures included a visual analogue rating of drooling frequency (VAS-D), as well as assessment of patient embarrassment within the familial (VAS-FD) and social (VAS-SD) context. | Subjects treated with BoNTX experienced a reduction in both drooling frequency and familial and social disability (Time × Group effect: p < 0.01), as well as in saliva production (Time × Group effect: p < 0.0001). | External anatomical landmarks | x |
| Nóbrega et al. [24] | 21 | open clinical trial | Drooling severity and frequency | The severity of drooling decreased in 18 (86%) patients, while frequency was reduced in 8 (38%). In 11 (52%) patients, the frequency of drooling remained constant. | Ultrasound | bilateral local oedema |
| Ondo, W.G. [25] | 16 | A double-blind placebo/treatment | The Unified Parkinson’s Disease Rating Scale (UPDRS), questionnaires regarding drooling, Visual Analogue Scale, global impressions, salivary gland imaging, and a dysphagia questionnaire. | Injections of botulinum toxin B into the parotid and submandibular glands appear to effectively improve sialorrhea without compromising dysphagia in patients with PD. | Anatomic landmarks | x |
| Mancini, F. [26] | 20 | Double-blind, placebo-controlled study | Drooling Severity and Drooling Frequency scales | BTX injection into parotids and submandibular glands, is an effective and safe treatment for drooling. | Ultrasound | x |
| Friedman et al. [27] | 11 | Cases/control | The Unified Parkinson’s Disease Rating Scale (UPDRS), saliva production by weighing dental rolls. | Botulinum toxin may be an effective and safe treatment of parkinsonian sialorrhea. | Anatomic landmarks | No |
| Pal et al. [28] | 9 | open clinical trial | Rating scales for severity and frequency of drooling and saliva production by weighing dental rolls. | Intraparotid BTX-A can be a useful, safe, and simple treatment for reducing the accumulation of saliva in neurologically impaired patients. | Anatomic landmarks | No |
| Santamato et al. [29] | 18 | open clinical trial | Questionnaire-Based Scoring System for Drool—the dose of Botox used per parotid glanding Severity and Frequency. | The severity and the frequency of drooling decreased in all patients after BTX-A after a 30-day follow-up. | Ultrasound | adverse effects could be dysphagia and chewing difficulties |
| Breheret et al. [17] | 14 | Retrospective review between May 2002 and February 2008 | Quality of life questionnaire from 6–8 weeks after the injections. (0 = no efficacy, 1 = partial efficacy, 2 = good efficacy but of brief duration (<1 month), 3 = very effective: resolution of drooling, 4 = patient died or lost to follow-up). | Beneficial effect in 66% of cases. The most effective protocol was injection of 20 U of toxin into each submandibular (submaxillary) gland and 30 U into each parotid gland. | Ultrasound | No major complications were observed (haematoma of the floor of the mouth or paralysis). |
| Bruno et al. [4] | 160 | Retrospective review of patients who received treatment with injections between 1995 and 2014 | Response to treatment was assessed by using a subjective Clinical Global Impression (CGI) consisting of five points (3 = very much improved, 2 = much improved, 1 = minimally improved, 0 = no change, and −1 = worse). The CGI assessment was performed after the first set of injections and in the last recorded visit. | Improvement in pain in 81% of cases, which was maintained in the last recorded visit, without significant differences with the result after the first injection. BTX treatment could play a safe and useful role in the treatment of pain in this population. | Electromyography | x |
| Chinnapongse et al. [6] | 54 | Prospective, multicentre, randomised, double-blind design | Follow-up of subjects for four weeks and up to 20 weeks. Primary measure: safety/tolerability as assessed by adverse events. Secondary measure: Efficacy, assessed by means of the Drooling Frequency and Severity Scale and unstimulated salivary flow rate. | Gastrointestinal adverse events in 31% of the active group compared to 7% in the placebo group, with dry mouth being the most common. No serious adverse events or treatment discontinuations due to adverse events. Significant improvement in DFSS at 4 weeks postinjection and decreased unstimulated salivary flow rate. | External anatomical landmarks | x |
| Gómez-Caravaca et al. [7] | 53 | Retrospective study with a long-term follow-up, between 2007 and 2013. | Variables: previous treatment, number of visits, average dose administered, duration of treatment effect and latency, assessment of response to treatment (less drooling), increased doses, mean years of follow-up and adverse events. The response to treatment was evaluated on a scale of 1 (minimal response) to 10 (maximum response), and patients were considered as responders if they scored greater than zero in this scale. | There was an improvement after treatment in 65.22% of patients with an average score of 6.85 ± 1.58 points on a scale from 0 to 10. The duration of the effect of treatment was 4.38 ± 2.11 months, with a latency period of 10.06 ± 9.63 days. | External anatomical landmarks | Mild and infrequent: skin reaction and weakness in the muscles of mastication and one case of previous dysphagia was slightly exacerbated. |
| Mazlan et al. [11] | 30 | Prospective, double-blind randomised controlled trial between September 2010 and February 2014 | The primary outcome was the amount of saliva reduction, measured by the differential weight (wet versus dry) of intraoral dental gauze at baseline and at 2, 6, 12 and 24 weeks after injection. The secondary outcome was the subjective report of drooling by using the Drooling Frequency and Severity Scale (DFSS). | Saliva reduction in response to all doses of botulinum toxin A. No significant differences between doses. Greater mean reduction in those groups receiving the highest doses. The group that received 200 U of Dysport ® showed the greatest saliva reduction until 24 weeks and reported the most significant improvement in the DFSS score. | Ultrasound | Viscous saliva |
| Guidubaldi et al. [14] | 14 | Prospective, randomised, double-blind, crossover pilot study | Objective evaluations (cotton roll weight) and subjective evaluations (ad hoc clinical scales) were performed at baseline, after one and four weeks, and every four weeks until drooling returned to baseline. | Subjective and objective improvements in all patients. Latency was shorter upon use of botulinum toxin B (three days) compared to botulinum toxin A (six days). The mean duration of benefits was similar for bot. toxin A (75 days) and B (90 days). Either 250 U Dysport or 2500 U Neurobloc have similar effectiveness and safety in controlling sialorrhoea. | Ultrasound | Change to saliva thickness |
| Møller et al. [3] | 12 | Open, prospective study | Patients were followed up for two months with evaluations every second week by means of self-assessed rating scales for drooling intensity, discomfort and treatment effect, and determination of unstimulated whole saliva flow rate. | Drooling and saliva flow were reduced (p < 0.05) two weeks after treatment, without side effects. The maximal reductions during the observation period were 40% for drooling and 30% for saliva flow. There was a variation in flow. Amylase activity and total protein concentration generally increased with decreasing flow (p ≤ 0.03). | Ultrasound | Seven patients dropped out shortly after the first treatment due to marked worsening of their disease-related condition. |
| Møller et al. [15] | 17 | Discomfort caused by drooling was rated on a VAS (0–100), and on a scale describing frequency and severity of drooling (0 = no drooling/dry to 7 = constant drooling). Measures were obtained after 6, 12 and 18 weeks. Perception of treatment effectiveness was also measured. Saliva flow was measured with cotton rolls in 2-min collection periods. The composition of saliva was also analysed. | Number of treatment series in each patient was 1–7. Saliva flow rate and drooling were reduced 30%–70% six weeks after treatment in the first series, while sodium, chloride, and total protein increased 20–80% (t-tests; p < 0.05). After 12 weeks, drooling was still significantly reduced (20%), saliva flow tended to be, and saliva composition was back to baseline. | Ultrasound | Viscous saliva and dry mouth | |
| Narayanaswami et al. [18] | 10 | Randomised, double blind, placebo-controlled crossover trial. | 1. Subjects returned monthly for three evaluations after each injection. Outcome measures were saliva weight and Drooling Frequency and Severity Scale. 2. Systematic review of literature, followed by inverse variance meta-analyses using random effects models. | 1. There was no significant change in the primary outcome of saliva weight one month after injection in the treatment period compared to placebo period. 2. Secondary outcomes did not change either. Meta-analysis of six studies demonstrated significant benefit of Botulinum toxin on functional outcomes. This study did not demonstrate efficacy of incobotulinum toxin A for drooling in PD, but lacked precision to exclude moderate benefit. Studies evaluating higher doses of incobotulinum toxin A into the parotid glands may be useful. | Unspecified | Difficulty during mastication and in the motor control of tongue. Viscous saliva. |
| Petracca et al. [19] | 65 | Retrospective trial | Drooling Frequency and Severity Scale four weeks after intervention | 250 U of botulinum toxin A and 2500 U of botulinum toxin B are safe and effective in the treatment of sialorrhoea, even in long-term follow-up. The older the age, the longer the benefit duration. Patients with PD showed a more favourable safety-efficacy ratio than patients with ALS did. | Ultrasound | Change of saliva thickness |
| Sen et al. [16] | 16 | Retrospective analysis between February 2009 and September 2013 | Severity of sialorrhoea prior to treatment was measured in accordance with Drooling Frequency and Severity Scale (DFSS). Efficacy was assessed 4 weeks after injections of BoNT-A by using DFSS and according to the subjective evaluation of patients and/or carers (caregivers). | Efficacy was 100% and mean improvement in sialorrhoea was 71.78 ± 12.95%. There was a significant difference between the first and last application regarding the mean duration of efficacy (17.28 ± 9.21 weeks and 18.03 ± 9.02 weeks, respectively, p = 0.001). Repeated BoNT-A injections are safe and effective in the treatment of sialorrhoea in patients with PD. | External anatomical landmarks | Not seen |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Roca, J.A.; Pons-Fuster, E.; Lopez-Jornet, P. Effectiveness of the Botulinum Toxin for Treating Sialorrhea in Patients with Parkinson’s Disease: A Systematic Review. J. Clin. Med. 2019, 8, 317. https://doi.org/10.3390/jcm8030317
Ruiz-Roca JA, Pons-Fuster E, Lopez-Jornet P. Effectiveness of the Botulinum Toxin for Treating Sialorrhea in Patients with Parkinson’s Disease: A Systematic Review. Journal of Clinical Medicine. 2019; 8(3):317. https://doi.org/10.3390/jcm8030317
Chicago/Turabian StyleRuiz-Roca, Juan Antonio, Eduardo Pons-Fuster, and Pia Lopez-Jornet. 2019. "Effectiveness of the Botulinum Toxin for Treating Sialorrhea in Patients with Parkinson’s Disease: A Systematic Review" Journal of Clinical Medicine 8, no. 3: 317. https://doi.org/10.3390/jcm8030317
APA StyleRuiz-Roca, J. A., Pons-Fuster, E., & Lopez-Jornet, P. (2019). Effectiveness of the Botulinum Toxin for Treating Sialorrhea in Patients with Parkinson’s Disease: A Systematic Review. Journal of Clinical Medicine, 8(3), 317. https://doi.org/10.3390/jcm8030317






