NT-ProBNP Predicts Total Mortality, Emergency Department Visits, Hospitalization, Intensive-Care Unit Admission, and Cardiovascular Events in Hemodialysis Patients
Abstract
:1. Introduction
2. Experimental Section
2.1. Ethics
2.2. Patients
2.3. Outcome Events Definition
2.4. Comorbidities of Interest
2.5. Procedures
2.6. Serum Analyses
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
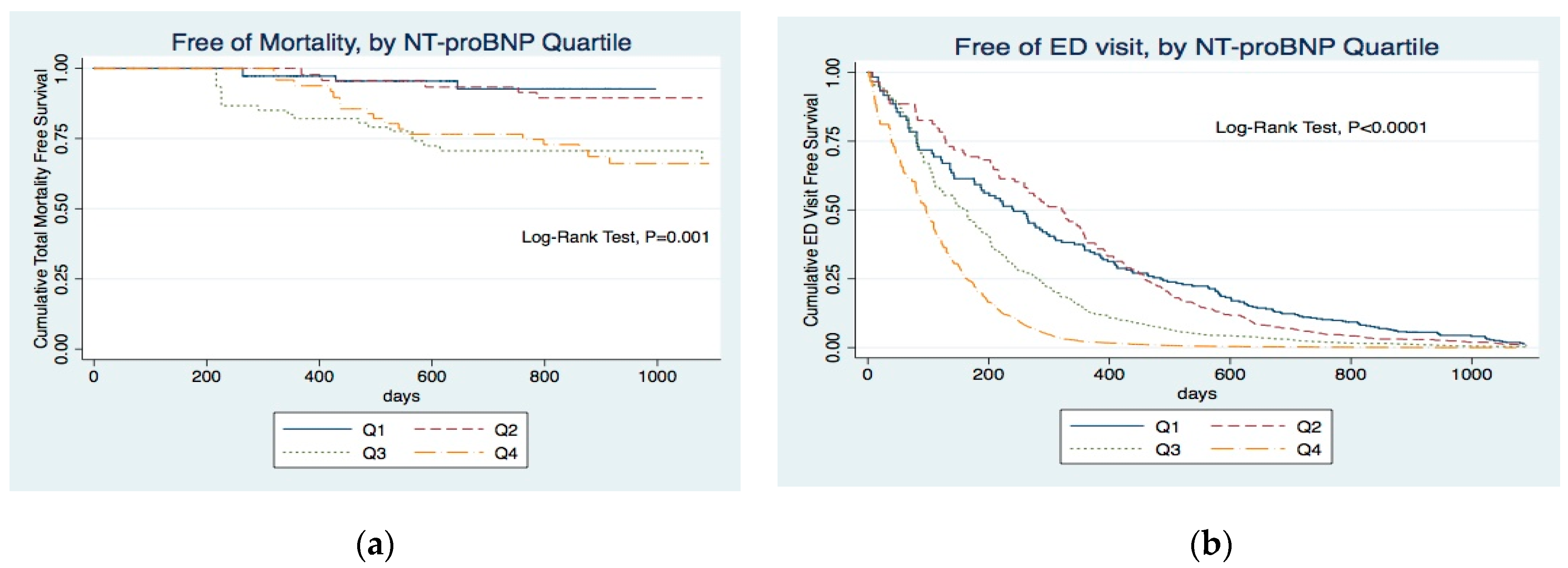
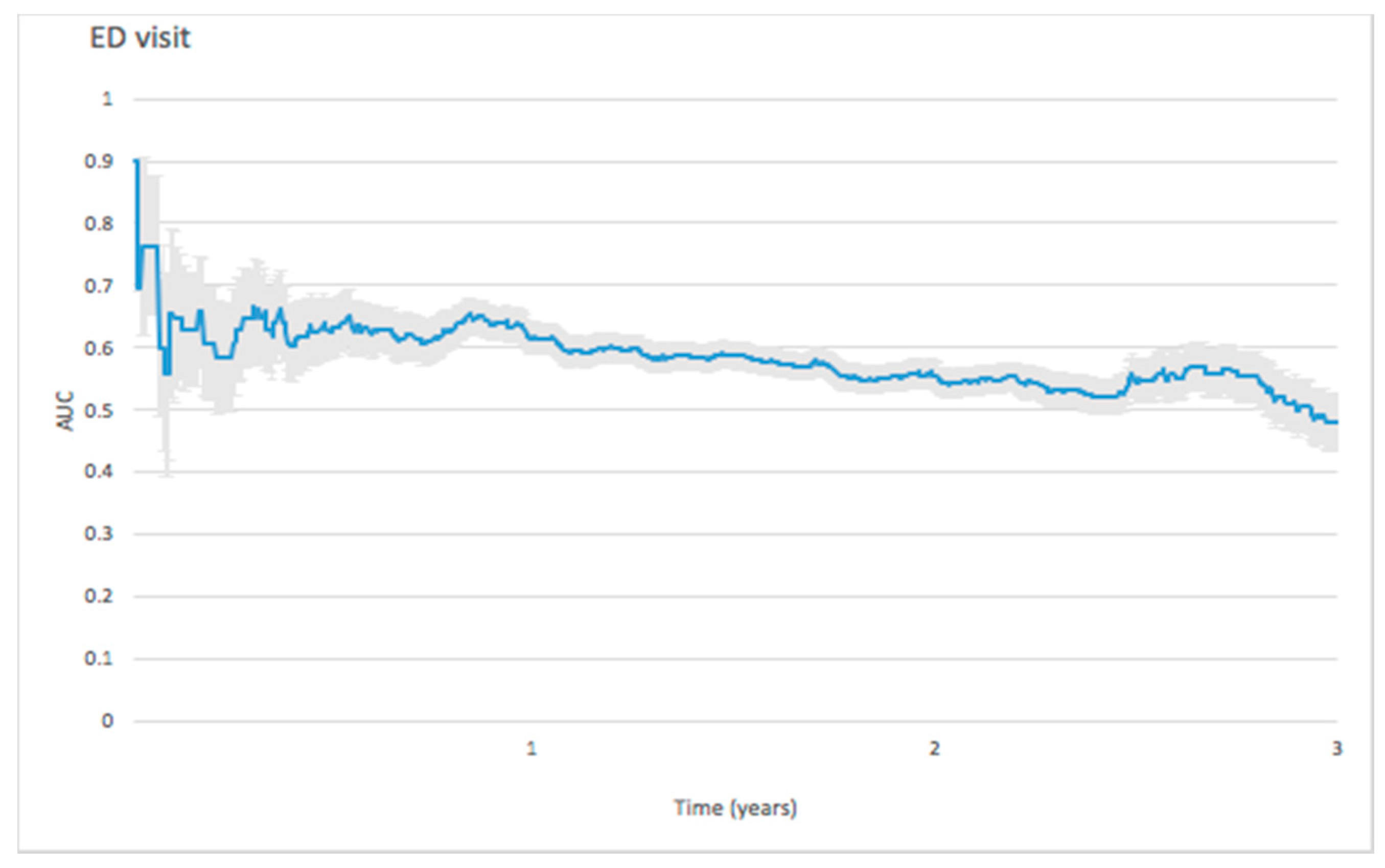
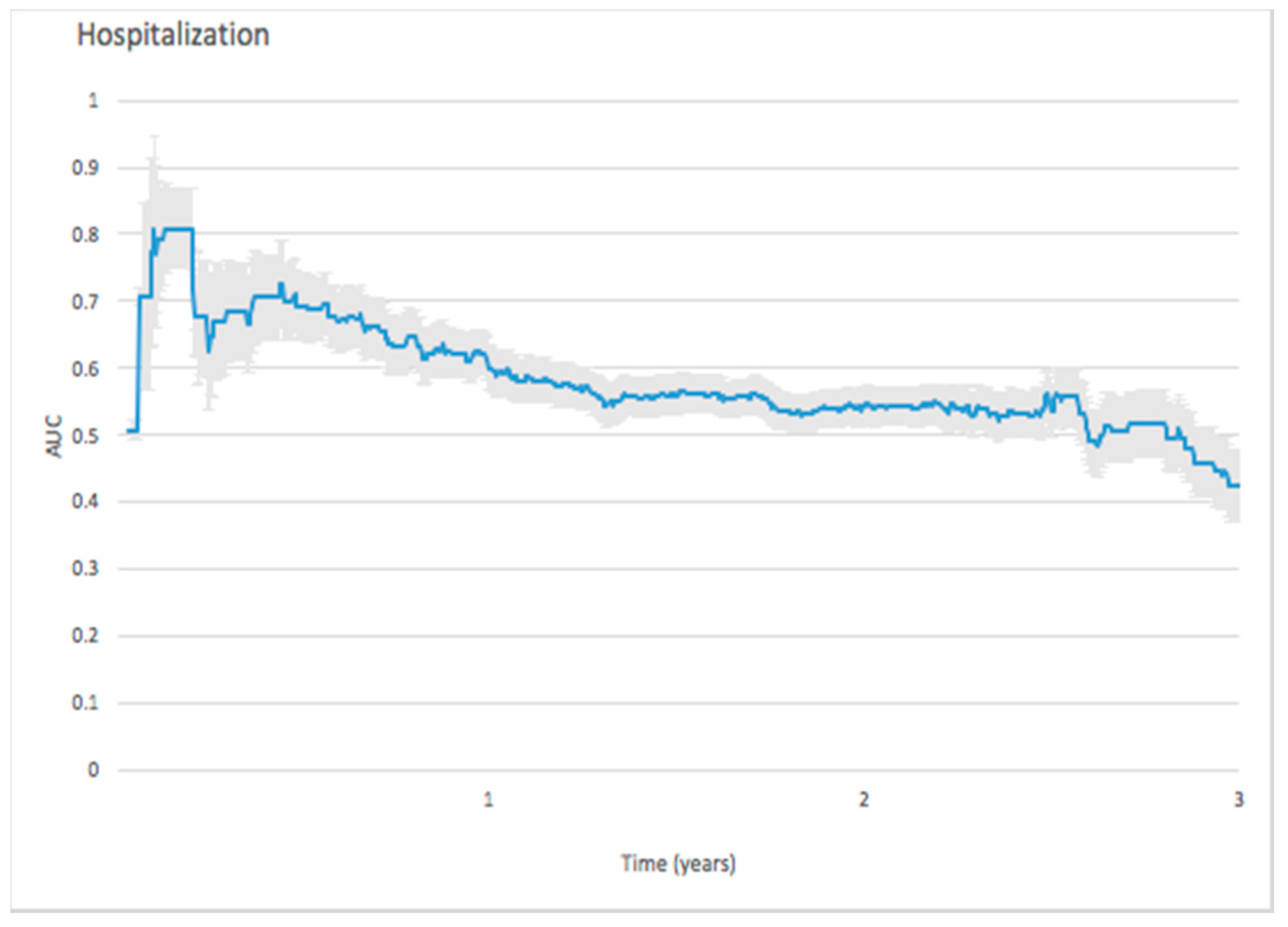
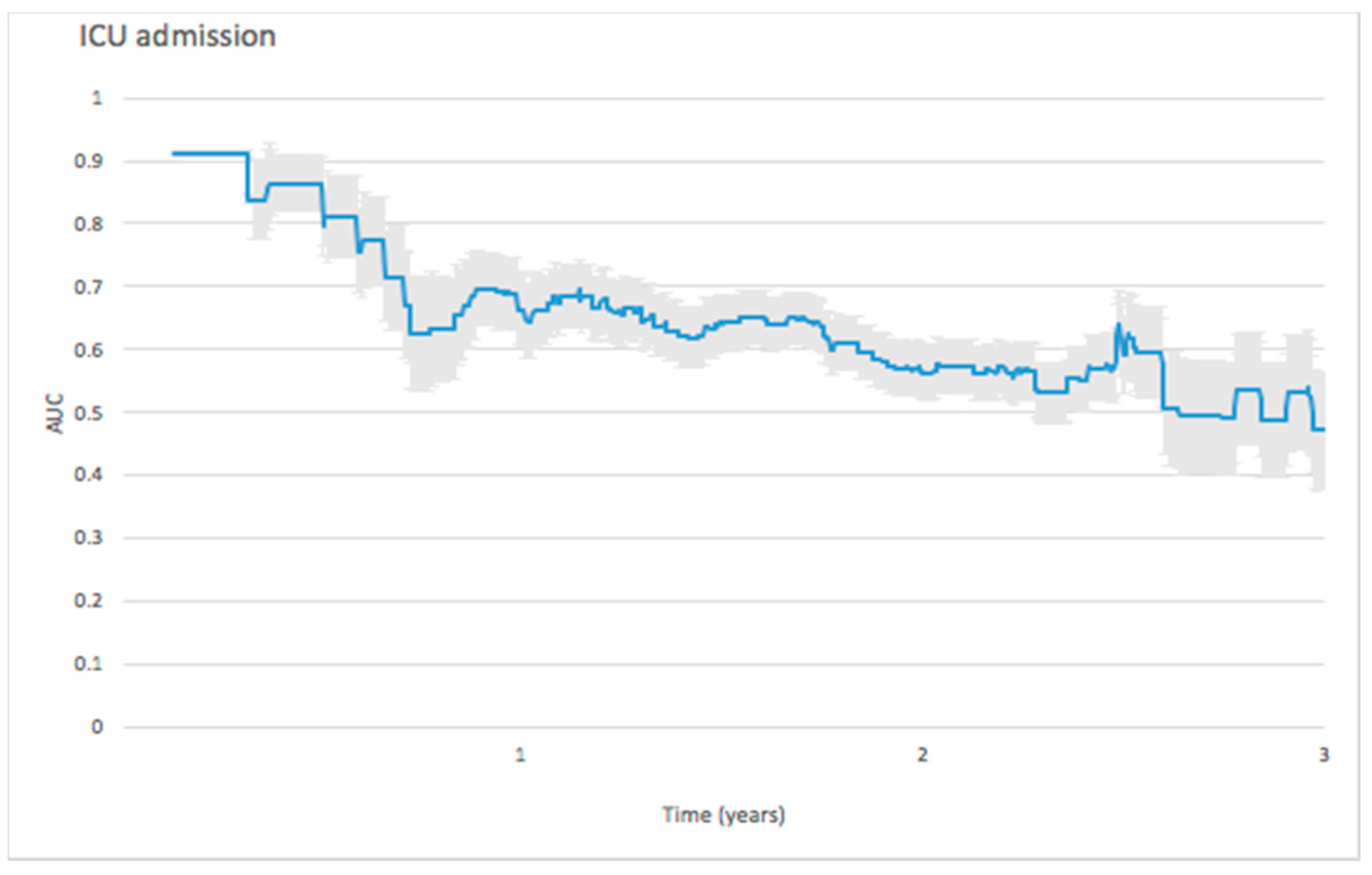
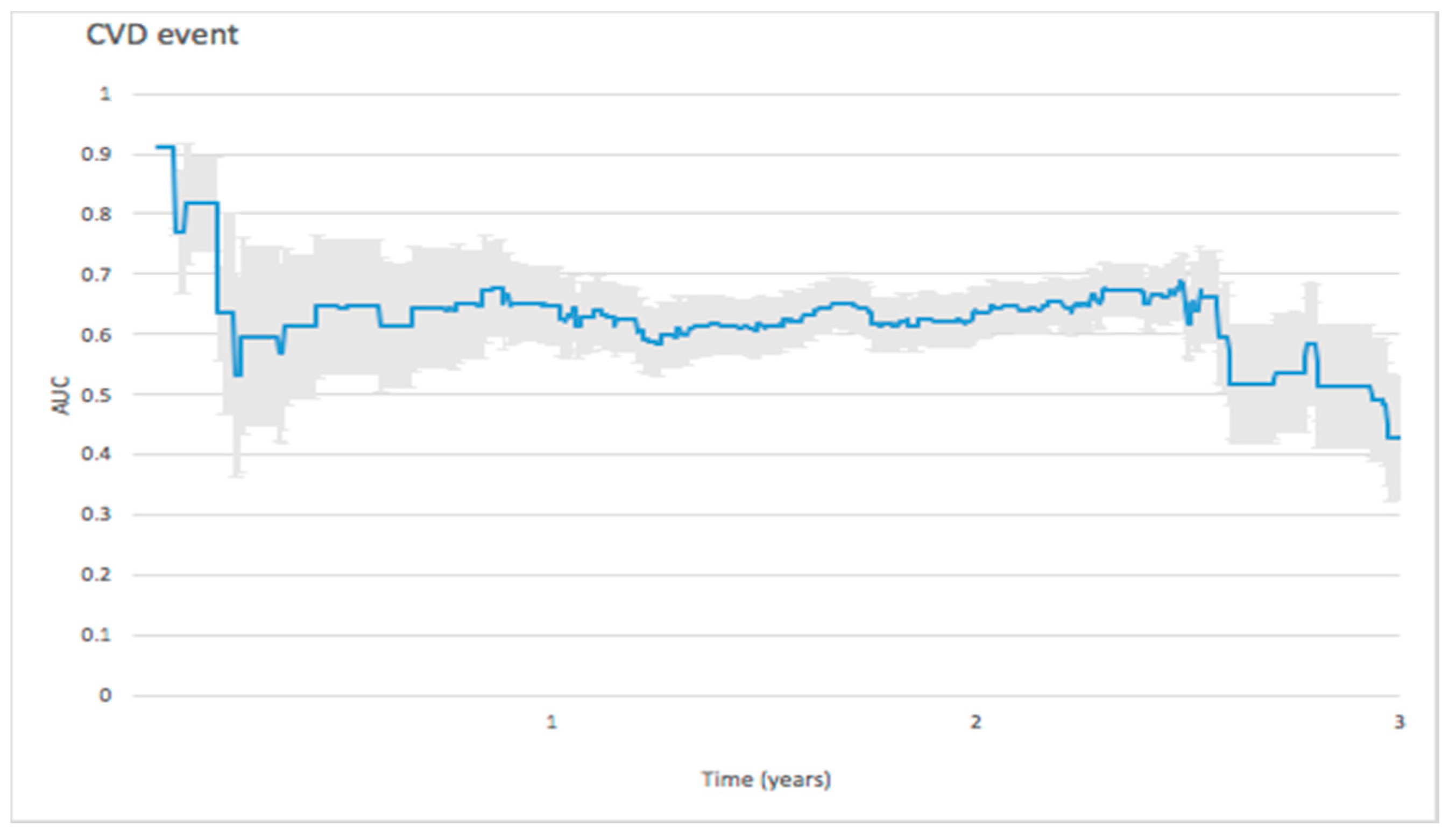
3.2. Predictive Ability of N-Terminal Pro B-Type Natriuretic Peptide (NT-ProBNP) Values for Different Clinical Outcomes at Different Time Points
3.2.1. Mortality
3.2.2. Emergency Department (ED) Visit
3.2.3. Hospitalization
3.2.4. Intensive-Care Unit (ICU) Admission
3.2.5. Cardiovascular Events
4. Discussion
4.1. Hospitalization, ICU Admission, and Cardiovascular Events
4.2. Predictive Ability Over Time
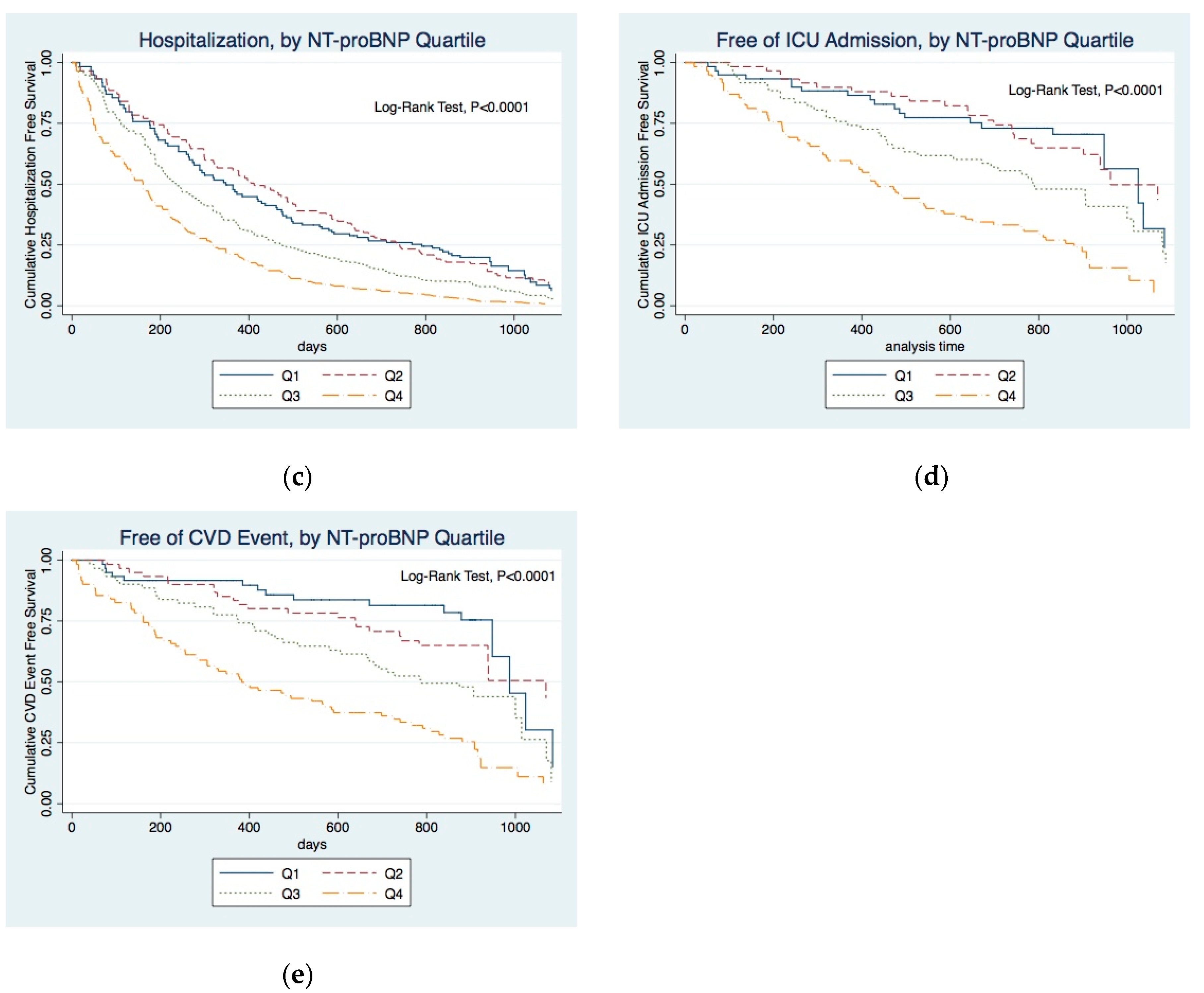
4.2.1. Mortality
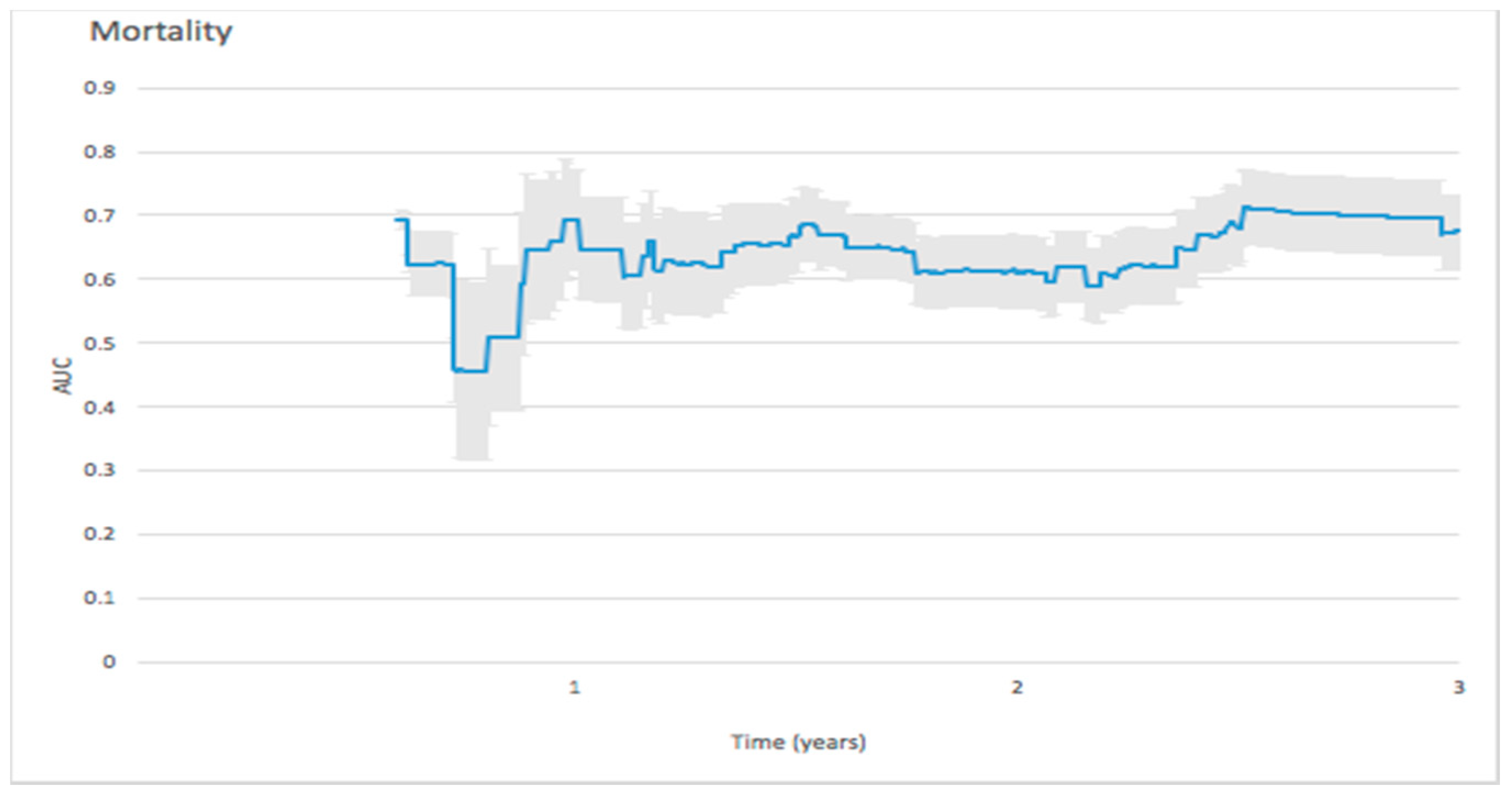
4.2.2. ED Visit
4.2.3. Predicting Hospitalization
4.2.4. Predicting ICU Admission
4.2.5. Cardiovascular Events
4.3. Limitations
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Januzzi, J.L.; van Kimmenade, R.; Lainchbury, J.; Bayes-Genis, A.; Ordonez-Llanos, J.; Santalo-Bel, M.; Pinto, Y.M.; Richards, M. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: An international pooled analysis of 1256 patients: The International Collaborative of NT-proBNP Study. Eur. Heart J. 2005, 27, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-T.; Tseng, Y.-T.; Chu, T.-W.; Chen, J.; Lai, M.-Y.; Tang, W.-R.; Shiao, C.-C. N-terminal pro b-type natriuretic peptide (NT-pro-BNP) -based score can predict in-hospital mortality in patients with heart failure. Sci. Rep. 2016, 6, 29590. [Google Scholar] [CrossRef]
- Bayes-Genis, A.; Lopez, L.; Zapico, E.; Cotes, C.; Santaló, M.; Ordóñez-Llanos, J.; Cinca, J. NT-ProBNP reduction percentage during admission for acutely decompensated heart failure predicts long-term cardiovascular mortality. J. Card. Fail. 2005, 11, S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Bibbins-Domingo, K.; Gupta, R.; Na, B.; Wu, A.H.B.; Schiller, N.B.; Whooley, M.A. N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart disease. JAMA 2007, 297, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Verdiani, V.; Ognibene, A.; Rutili, M.S.; Lombardo, C.; Bacci, F.; Terreni, A.; Nozzoli, C. NT-ProBNP reduction percentage during hospital stay predicts long-term mortality and readmission in heart failure patients. J. Cardiovasc. Med. 2008, 9, 694–699. [Google Scholar] [CrossRef] [PubMed]
- Vázquez, R.; Alcántara, G.; Ventura, M.-D.-J.; Hinojosa-Heredia, H.; Cueto-Manzano, A.; Cisneros, A.; Madonia-Juseino, C.; Belio-Caro, F.; Trinidad-Ramos, P.; Ilabaca, B.; et al. NT-proBNP, fluid volume overload and dialysis modality are independent predictors of mortality in ESRD patients. Nephrol. Dial. Transplant. 2010, 25, 551–557. [Google Scholar] [CrossRef]
- McGill, D.; Talaulikar, G.; Potter, J.M.; Koerbin, G.; Hickman, P.E. Over time, high-sensitivity TnT replaces NT-proBNP as the most powerful predictor of death in patients with dialysis-dependent chronic renal failure. Clin. Chim. Acta 2010, 411, 936–939. [Google Scholar] [CrossRef] [PubMed]
- Madsen, L.H.; Ladefoged, S.; Corell, P.; Schou, M.; Hildebrandt, P.R.; Atar, D. N-terminal pro brain natriuretic peptide predicts mortality in patients with end-stage renal disease in hemodialysis. Kidney Int. 2007, 71, 548–554. [Google Scholar] [CrossRef] [Green Version]
- Svensson, M.; Gorst-Rasmussen, A.; Schmidt, E.B.; Jorgensen, K.A.; Christensen, J.H. NT-pro-BNP is an independent predictor of mortality in patients with end-stage renal disease. Clin. Nephrol. 2009, 71, 380–386. [Google Scholar] [CrossRef]
- Gutiérrez, O.M.; Tamez, H.; Bhan, I.; Zazra, J.; Tonelli, M.; Wolf, M.; Januzzi, J.L.; Chang, Y.; Thadhani, R. N-terminal pro-B-type natriuretic peptide (NT-proBNP) concentrations in hemodialysis patients: Prognostic value of baseline and follow-up measurements. Clin. Chem. 2008, 54, 1339–1348. [Google Scholar] [CrossRef]
- Chambless, L.E.; Diao, G. Estimation of time-dependent area under the ROC curve for long-term risk prediction. Stat. Med. 2006, 25, 3474–3486. [Google Scholar] [CrossRef] [PubMed]
- Heagerty, P.J.; Lumley, T.; Pepe, M.S. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 2000, 56, 337–344. [Google Scholar] [CrossRef]
- Kamarudin, A.N.; Cox, T.; Kolamunnage-Dona, R. Time-dependent ROC curve analysis in medical research: Current methods and applications. BMC Med. Res. Methodol. 2017, 17, 53. [Google Scholar] [CrossRef] [PubMed]
- Alexander, R.T.; Hemmelgarn, B.R.; Wiebe, N.; Bello, A.; Samuel, S.; Klarenbach, S.W.; Curhan, G.C.; Tonelli, M.; Network, F.T.A.K.D. Kidney stones and cardiovascular events: A cohort study. Clin. J. Am. Soc. Nephrol. 2014, 9, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.A.; Mann, A.; Cannon, G.W.; Mikuls, T.R.; Reimold, A.M.; Caplan, L. Validation of Diagnostic and Procedural Codes for Identification of Acute Cardiovascular Events in US Veterans with Rheumatoid Arthritis. EGEMS 2013, 1, 1023. [Google Scholar] [CrossRef] [PubMed]
- Ku, E.; Gassman, J.; Appel, L.J.; Smogorzewski, M.; Sarnak, M.J.; Glidden, D.V.; Bakris, G.; Gutiérrez, O.M.; Hebert, L.A.; Ix, J.H.; et al. BP Control and Long-Term Risk of ESRD and Mortality. J. Am. Soc. Nephrol. 2017, 28, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Ehteshami, P.; Sarnak, M.J.; Tighiouart, H.; Jun, M.; Ninomiya, T.; Foote, C.; Rodgers, A.; Zhang, H.; Wang, H.; et al. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: A systematic review and meta-analysis. CMAJ Can. Med. Assoc. J. 2013, 185, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, A.; Earley, A.; Haynes, S.M.; Uhlig, K. Systematic review: Blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann. Intern. Med. 2011, 154, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Miranda, C.H.; Borges, M.D.C.; Matsuno, A.K.; Vilar, F.C.; Gali, L.G.; Volpe, G.J.; Schmidt, A.; Pazin-Filho, A.; da Silva, F.M.F.; de Castro-Jorge, L.A.; et al. Evaluation of cardiac involvement during dengue viral infection. Clin. Infect. Dis. 2013, 57, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Mindikoglu, A.L.; Dowling, T.C.; Weir, M.R.; Seliger, S.L.; Christenson, R.H.; Magder, L.S. Performance of chronic kidney disease epidemiology collaboration creatinine-cystatin C equation for estimating kidney function in cirrhosis. Hepatology 2014, 59, 1532–1542. [Google Scholar] [CrossRef]
- Peña, E.A.; Strawderman, R.L.; Hollander, M. Nonparametric Estimation With Recurrent Event Data. J. Am. Stat. Assoc. 2001, 96, 1299–1315. [Google Scholar] [CrossRef] [Green Version]
- Andersen, P.K.; Gill, R.D. Cox’s Regression Model for Counting Processes: A Large Sample Study; Mathematisch Centrum: Amsterdam, The Netherlands, 1981; 38p. [Google Scholar]
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S; Chambers, S.J., Eddy, W., Hardle, W., Sheater, S., Tierney, L., Eds.; Springer: New York, NY, USA, 2002. [Google Scholar]
- Heagerty, P.J.; Zheng, Y. Survival model predictive accuracy and ROC curves. Biometrics 2005, 61, 92–105. [Google Scholar] [CrossRef] [PubMed]
- Mark, P.B.; Stewart, G.A.; Gansevoort, R.T.; Petrie, C.J.; McDonagh, T.A.; Dargie, H.J.; Rodger, R.S.C.; Jardine, A.G. Diagnostic potential of circulating natriuretic peptides in chronic kidney disease. Nephrol. Dial. Transplant. 2006, 21, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Racek, J.; Králová, H.; Trefil, L.; Rajdl, D.; Eiselt, J. Brain natriuretic peptide and N-terminal proBNP in chronic haemodialysis patients. Nephron. Clin. Pract. 2006, 103, c162–c172. [Google Scholar] [CrossRef] [PubMed]
- Sheen, V.; Bhalla, V.; Tulua-Tata, A.; Bhalla, M.A.; Weiss, D.; Chiu, A.; Abdeen, O.; Mullaney, S.; Maisel, A. The use of B-type natriuretic peptide to assess volume status in patients with end-stage renal disease. Am. Heart J. 2007, 153, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Keyzer, J.M.; Hoffmann, J.J.; Ringoir, L.; Nabbe, K.C.; Widdershoven, J.W.; Pop, V.J. Age- and gender-specific brain natriuretic peptide (BNP) reference ranges in primary care. Clin. Chem. Lab. Med. 2014, 52, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L., Jr.; Camargo, C.A.; Anwaruddin, S.; Baggish, A.L.; Chen, A.A.; Krauser, D.G.; Tung, R.; Cameron, R.; Nagurney, J.T.; Chae, C.U.; et al. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am. J. Cardiol. 2005, 95, 948–954. [Google Scholar] [CrossRef]
- Bayés-Genís, A.; Santaló-Bel, M.; Zapico-Muñiz, E.; López, L.; Cotes, C.; Bellido, J.; Leta, R.; Casan, P.; Ordóñez-Llanos, J. N-terminal probrain natriuretic peptide (NT-proBNP) in the emergency diagnosis and in-hospital monitoring of patients with dyspnoea and ventricular dysfunction. Eur. J. Heart Fail. 2004, 6, 301–308. [Google Scholar] [CrossRef] [Green Version]
- O’Brien, R.J.; Squire, I.B.; Demme, B.; Davies, J.E.; Ng, L.L. Pre-discharge, but not admission, levels of NT-proBNP predict adverse prognosis following acute LVF. Eur. J. Heart Fail. 2003, 5, 499–506. [Google Scholar] [CrossRef]
- Stolz, D.; Breidthardt, T.; Christ-Crain, M.; Bingisser, R.; Miedinger, D.; Leuppi, J.; Beat, M.; Michael, T.; Christian, M. Use of B-type natriuretic peptide in the risk stratification of acute exacerbations of COPD. Chest 2008, 133, 1088–1094. [Google Scholar] [CrossRef]
- Tsuchida, K.; Tanabe, K. Plasma brain natriuretic peptide concentrations and the risk of cardiovascular events and death in general practice. J. Cardiol. 2008, 52, 212–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masson, S.; Latini, R.; Anand, I.S.; Vago, T.; Angelici, L.; Barlera, S.; Missov, E.D.; Clerico, A.; Tognoni, G.; Cohn, J.N. Direct comparison of B-type natriuretic peptide (BNP) and amino-terminal proBNP in a large population of patients with chronic and symptomatic heart failure: The Valsartan Heart Failure (Val-HeFT) Data. Clin. Chem. 2006, 52, 1528–1538. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; Sakhuja, R.; O’Donoghue, M.; Baggish, A.L.; Anwaruddin, S.; Chae, C.U.; Cameron, R.; Krauser, D.G.; Tung, R.; Camargo, C.A., Jr.; et al. Utility of amino-terminal pro–brain natriuretic peptide testing for prediction of 1-year mortality in patients with dyspnea treated in the emergency department. Arch. Intern. Med. 2006, 166, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.P.; Borque, L.; Rus, A.; Vicente, B.; Ramirez, Y.; Lasa, L. Comparison of BNP and NT-proBNP assays in the approach to the emergency diagnosis of acute dyspnea. J. Clin. 2006, 20, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Nakata, K.; Komukai, K.; Yoshii, Y.; Miyanaga, S.; Kubota, T.; Kosuga, T.; Suzuki, K.; Yamada, T.; Yoshida, J.; Kimura, H.; et al. The Optimal Cut-off Value of Plasma BNP to Differentiate Heart Failure in the Emergency Department in Japanese Patients with Dyspnea. Intern. Med. 2015, 54, 2975–2980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noveanu, M.; Breidthardt, T.; Potocki, M.; Reichlin, T.; Twerenbold, R.; Uthoff, H.; Socrates, T.; Arenja, N.; Reiter, M.; Meissner, J.; et al. Direct comparison of serial B-type natriuretic peptide and NT-proBNP levels for prediction of short- and long-term outcome in acute decompensated heart failure. Crit. Care 2011, 15, R1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bettencourt, P.; Ferreira, S.; Azevedo, A.; Ferreira, A. Preliminary data on the potential usefulness of B-type natriuretic peptide levels in predicting outcome after hospital discharge in patients with heart failure. Am. J. Med. 2002, 113, 215–219. [Google Scholar] [CrossRef]
- Cheng, V.; Kazanagra, R.; Garcia, A.; Lenert, L.; Krishnaswamy, P.; Gardetto, N.; Clopton, P.; Maisel, A. A rapid bedside test for B-type peptide predicts treatment outcomes in patients admitted for decompensated heart failure: A pilot study. J. Am. Coll. Cardiol. 2001, 37, 386–391. [Google Scholar] [CrossRef]
- Logeart, D.; Thabut, G.; Jourdain, P.; Chavelas, C.; Beyne, P.; Beauvais, F.; Bouvier, E.; Solal, A.C. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J. Am. Coll. Cardiol. 2004, 43, 635–641. [Google Scholar] [CrossRef] [Green Version]
- Krzych, Ł.J.; Szurlej, D.; Kołodziej, T.; Machej, L.; Węglarzy, A.; Błach, A.; Wilczyński, M.; Woś, S.; Bochenek, A. Diagnostic accuracy of pre-operative NT-proBNP level in predicting short-term outcomes in coronary surgery: A pilot study. Kardiol. Pol. 2011, 69, 1121–1127. [Google Scholar]
- Wolsk, E.; Claggett, B.; Pfeffer, M.A.; Diaz, R.; Dickstein, K.; Gerstein, H.C.; Lawson, F.C.; Lewis, E.F.; Maggioni, A.P.; McMurray, J.J.V.; et al. Role of B-Type Natriuretic Peptide and N-Terminal Prohormone BNP as Predictors of Cardiovascular Morbidity and Mortality in Patients With a Recent Coronary Event and Type 2 Diabetes Mellitus. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Ishibashi, Y.; Tanaka, F.; Omama, S.; Onoda, T.; Takahashi, T.; Tanno, K.; Ohsawa, M.; Sakata, K.; Koshiyama, M.; et al. Ability of B-Type Natriuretic Peptide Testing to Predict Cardioembolic Stroke in the General Population- Comparisons With C-Reactive Protein and Urinary Albumin. Circ. J. 2018, 82, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
| NT-ProBNP Quartile | ||||||
|---|---|---|---|---|---|---|
| Parameter | Q1 (<2296, n = 58) | Q2 (2296–4568, n = 58) | Q3 (4568–13,360, n = 58) | Q4 (>13,360, n = 58) | p | P-trend |
| Age, mean (SD), years | 63.1 (13.0) | 63.9 (12.7) | 66.6 (12.6) | 66.1 (12.6) | 0.375 | 0.115 |
| Gender, male (%) | 40 (69) | 29 (50) | 29 (50) | 27 (46.6) | 0.064 | 0.022 |
| SBP, mean (SD) | 142.03 (19.945) | 154.69 (49.49) | 151.64 (28.01) | 144.86 (24.65) | 0.134 | 0.355 |
| DBP, mean (SD) | 76.1 (12.78) | 75.74 (14.82) | 77.97 (14.45) | 76.88 (14.99) | 0.843 | 0.588 |
| BMI, mean (SD) | 24.54 (3.19) | 24.21 (4.068) | 24.53 (3.60) | 23.19 (2.98) | 0.125 | 0.070 |
| ALT, median (IQR) | 15 (12–21.25) | 13.5 (10–20.5) | 16.5 (11–21.25) | 14.5 (11–22.5) | 0.679 | 0.924 |
| BUN, mean (SD) | 84.98 (22.62) | 81.74 (20.15) | 81.17 (20.96) | 80.81 (20.59) | 0.700 | 0.292 |
| UA, median (IQR) | 8.25 (7.175–9.025) | 7.85 (6.8–8.475) | 7.65 (6.7–8.5) | 7.7 (6.3–8.7) | 0.238 | 0.053 |
| Na, median (IQR) | 135 (132–137) | 134 (132–136) | 135 (133–137) | 134.5 (132–136.2) | 0.491 | 0.961 |
| K, median (IQR) | 4.7 (4.175–5) | 4.9 (4.375–5.225) | 4.8 (4.375–5.4) | 5 (4.25–5.425) | 0.246 | 0.128 |
| Ca, median (IQR) | 8.7 (8.28–9.29) | 8.68 (8.12–9.24) | 8.42 (8.16–9.16) | 8.72 (8.04–9.29) | 0.855 | 0.543 |
| P, median (IQR) | 5.1 (4.375–5.8) | 5.05 (4.1–5.9) | 5.2 (4.5–6.525) | 5.2 (4.175–6.5) | 0.627 | 0.441 |
| Hb, median (IQR) | 10.6 (9.475–11.15) | 9.9 (9.475–10.625) | 10.2 (9.6–10.825) | 10.3 (8.8–11.125) | 0.427 | 0.537 |
| PTH, median (IQR) | 215.3 (74.3–422.1) | 207.1 (73.2–355.2) | 179.4 (86.4–275.2) | 206.9 (69.5–455.6) | 0.427 | 0.986 |
| Ferritin, median (IQR) | 346.9 (164–478.8) | 378.3 (217–536.2) | 299.4 (189.6–498.2) | 505.3 (221.9–631.8) | 0.072 | 0.055 |
| HTN, n (%) | 50 (86.2) | 53 (91.4) | 54 (93.1) | 56 (96.6) | 0.271 | 0.048 |
| CAD, n (%) | 30 (51.7) | 21 (36.2) | 40 (69) † | 39 (67.2) † | 0.005 | 0.007 |
| DM, n (%) | 41 (70.7) | 32 (55.2) | 37 (63.8) | 40 (69) | 0.399 | 0.934 |
| Hyperlipidemia, n (%) | 12 (20.7) | 7 (12.1) | 9 (15.5) | 8 (13.8) | 0.573 | 0.412 |
| ALB, median (IQR) | 4 (3.8–4.2) | 4 (3.7–4.2) | 3.9 (3.6–4.1) | 4 (3.575–4.2) | 0.385 | 0.22 |
| CRP, median (IQR) | 0.28 (0.12–0.69) | 0.25 (0.11–0.99) | 0.32 (0.13–0.93) | 0.36 (0.13–0.94) | 0.873 | 0.492 |
| NYHA class III or IV, n (%) | 7 (15.2%) | 6 (10.3%) | 12 (20.7%) | 21 (36.2%) *† | 0.002 | 0.001 |
| Dialysis vintage years, median (IQR) | 1.30 (0.31–3.35) | 1.29 (0.33–4.12) | 1.59 (0.25–4.31) | 1.58 (0.33–3.16) | 0.952 | 0.749 |
| NT-proBNP Quartile | ||||
|---|---|---|---|---|
| Events Observed | Q1 (<2296) | Q2 (2296–4568) | Q3 (4568–13,360) | Q4 (>13,360) |
| Mortality | 3 | 7 | 14 | 22 |
| ED visit | 157 | 222 | 303 | 400 |
| Hospitalization, n (%) | 39 (67) | 42 (72) | 46 (79) | 50 (86) |
| ICU admission | 23 | 33 | 45 | 65 |
| CVD event | 18 | 30 | 39 | 67 |
| Outcome | Unadjusted Model | Adjusted Model | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Total mortality | 1.94 (1.39, 2.71) | <0.0001 | 1.54 (1.08, 2.19) | 0.0158 |
| ED visit | 1.44 (1.23, 1.68) | <0.0001 | 1.36 (1.24, 1.50) | <0.0001 |
| Hospitalization | 1.42 (1.21, 1.65) | <0.0001 | 1.35 (1.19, 1.52) | <0.0001 |
| ICU admission | 1.65 (1.30, 2.11) | <0.0001 | 1.49 (1.20, 1.85) | 0.0003 |
| CVD | 1.71 (1.33, 2.17) | <0.0001 | 1.67 (1.33, 2.10) | <0.0001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-H.; Fu, Y.-C.; Wu, M.-J. NT-ProBNP Predicts Total Mortality, Emergency Department Visits, Hospitalization, Intensive-Care Unit Admission, and Cardiovascular Events in Hemodialysis Patients. J. Clin. Med. 2019, 8, 238. https://doi.org/10.3390/jcm8020238
Chen Y-H, Fu Y-C, Wu M-J. NT-ProBNP Predicts Total Mortality, Emergency Department Visits, Hospitalization, Intensive-Care Unit Admission, and Cardiovascular Events in Hemodialysis Patients. Journal of Clinical Medicine. 2019; 8(2):238. https://doi.org/10.3390/jcm8020238
Chicago/Turabian StyleChen, Yi-Hsin, Yun-Ching Fu, and Ming-Ju Wu. 2019. "NT-ProBNP Predicts Total Mortality, Emergency Department Visits, Hospitalization, Intensive-Care Unit Admission, and Cardiovascular Events in Hemodialysis Patients" Journal of Clinical Medicine 8, no. 2: 238. https://doi.org/10.3390/jcm8020238
APA StyleChen, Y.-H., Fu, Y.-C., & Wu, M.-J. (2019). NT-ProBNP Predicts Total Mortality, Emergency Department Visits, Hospitalization, Intensive-Care Unit Admission, and Cardiovascular Events in Hemodialysis Patients. Journal of Clinical Medicine, 8(2), 238. https://doi.org/10.3390/jcm8020238





