Long-Term Outcome of Potential Celiac Disease in Genetically at-Risk Children: The Prospective CELIPREV Cohort Study
Abstract
:1. Introduction
2. Methods
2.1. HLA Genotype
2.2. Serologic Assay
2.3. Small-Bowel Biopsies
2.4. Outcome Measures
2.5. Statistical Analyses
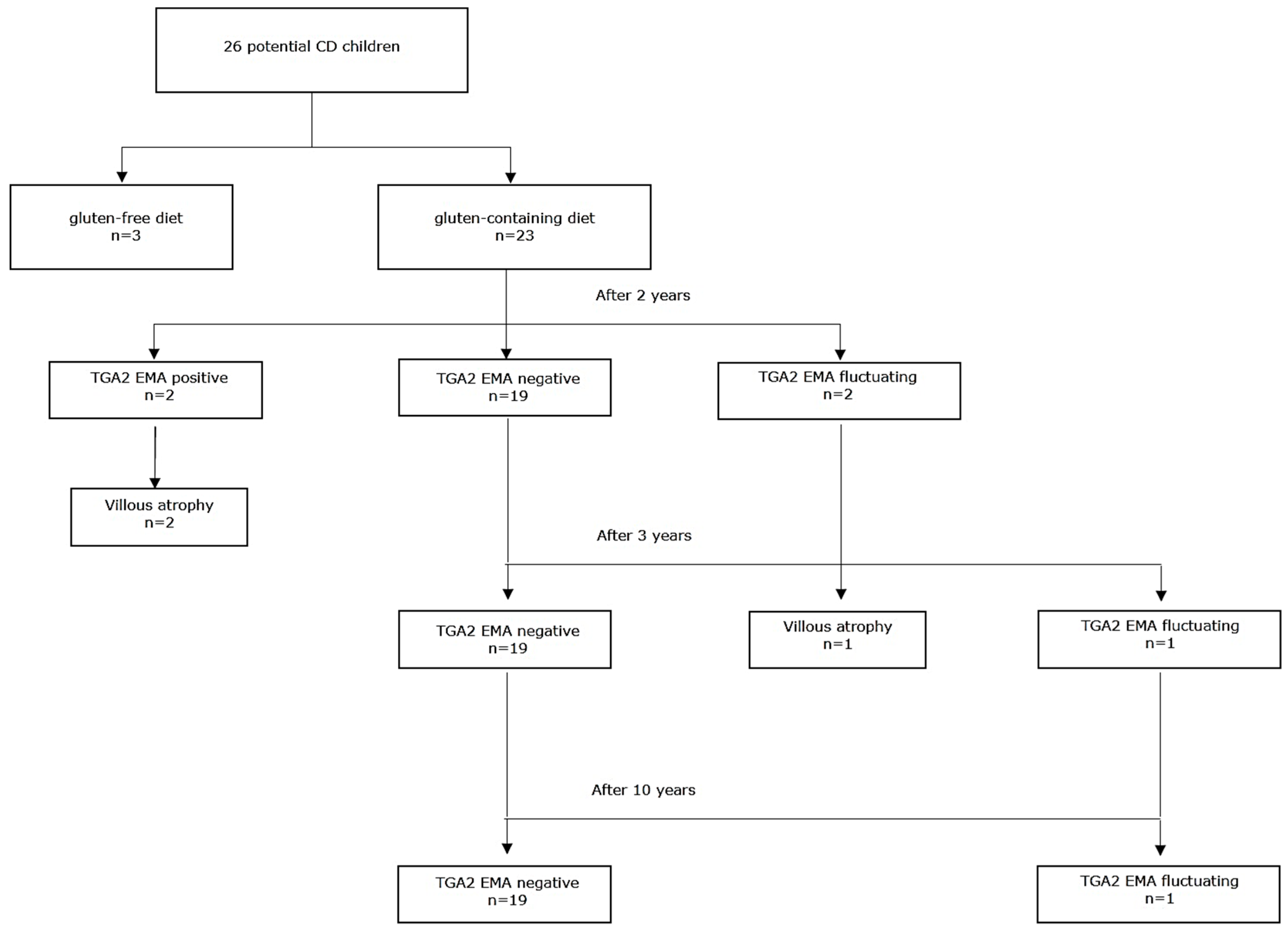
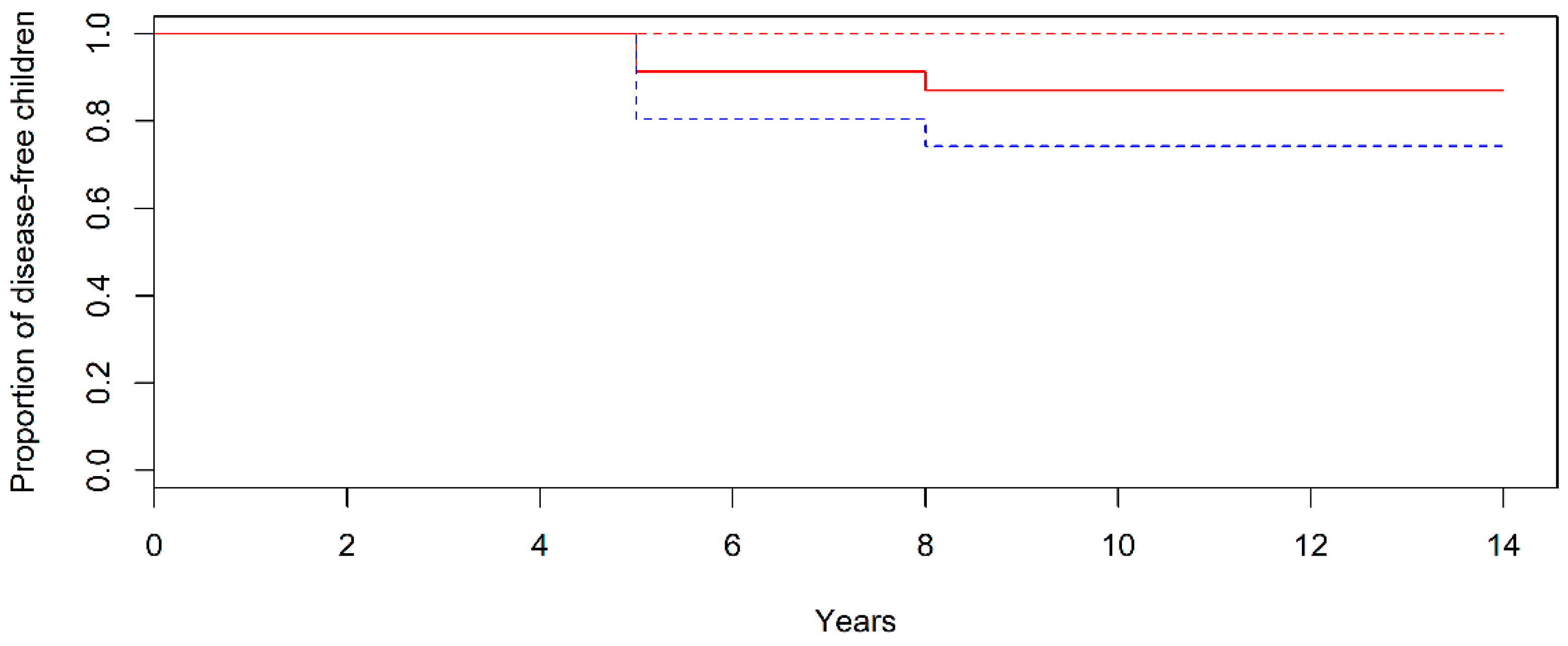
3. Results
3.1. Patients
3.2. Study Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgements
- 1
- Department of Pediatrics, AO-IRCCS Santa Maria Nuova Hospital, Reggio Emilia, Italy
- 2
- Department of Pediatrics, “La Sapienza” University, Roma, Italy
- 3
- Department of Pediatrics, University of Torino, Italy
- 4
- Department of Pediatrics, San Raffaele Hospital, Milano, Italy
- 5
- Department of Pediatrics, Bianchi-Melacrino Morelli Hospital, Reggio Calabria, Italy
- 6
- Paediatric Gastroenterology Unit, G. Gaslini Institute, Genova, Italy
- 7
- Department of Pediatrics, University of Padova, Italy
- 8
- Department of Pediatrics, “Federico II” University of Naples, Napoli, Italy
- 9
- Cystic Fibrosis and Paediatric Gastroenterology Unit, University Hospital ’G. Martino’, Messina, Italy
- 10
- Department of Pediatrics, Rovereto Hospital, Rovereto (TN), Italy
- 11
- Department of Pediatrics, University of Pisa, Italy
- 12
- Department of Pediatrics, Buzzi Children Hospital, Milano, Italy
Conflicts of Interest
References
- Fasano, A.; Catassi, C. Celiac disease. N. Engl. J. Med. 2012, 367, 2419–2426. [Google Scholar] [CrossRef] [PubMed]
- Lionetti, E.; Castellaneta, S.; Francavilla, R.; Pulvirenti, A.; Tonutti, E.; Amarri, S.; Barbato, M.; Barbera, C.; Barera, G.; Bellantoni, A.; et al. Introduction of gluten, HLA status and the risk of celiac disease in children. N. Engl. J. Med. 2014, 371, 1295–1303. [Google Scholar] [CrossRef] [PubMed]
- Lionetti, E.; Castellaneta, S.; Pulvirenti, A.; Tonutti, E.; Francavilla, R.; Fasano, A.; Catassi, C.; Italian Working Group of Weaning and Celiac Disease Risk. Prevalence and natural history of potential celiac disease in at family-risk infants prospectively investigated from birth. J. Pediatr. 2012, 161, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Vriezinga, S.L.; Auricchio, R.; Bravi, E.; Castillejo, G.; Chmielewska, A.; Crespo Escobar, P.; Kolaček, S.; Koletzko, S.; Korponay-Szabo, I.R.; Mummert, E.; et al. Randomized feeding intervention in infants at high risk for celiac disease. N. Engl. J. Med. 2014, 371, 1304–1315. [Google Scholar] [CrossRef] [PubMed]
- Simell, S.; Hoppu, S.; Hekkala, A.; Simell, T.; Stahlberg, M.R.; Viander, M.; Yrjänäinen, H.; Grönlund, J.; Markula, P.; Simell, V.; et al. Fate of five celiac disease-associated antibodies during normal diet in genetically at-risk children observed from birth in a natural history study. Am. J. Gastroenterol. 2007, 102, 2026–2035. [Google Scholar] [CrossRef] [PubMed]
- Liu, E.; Bao, F.; Barriga, K.; Miao, D.; Yu, L.; Erlich, H.A.; Haas, J.E.; Eisenbarth, G.S.; Rewers, M.J.; Hoffenberg, E.J. Fluctuating transglutaminase autoantibodies are related to histologic features of celiac disease. Clin. Gastroenterol. Hepatol. 2003, 1, 356–362. [Google Scholar] [CrossRef]
- Husby, S.; Koletzko, S.; Korponay-Szabó, I.R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. European society for pediatric gastroenterology, hepatology and nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [CrossRef]
- Lionetti, E.; Castellaneta, S.; Francavilla, R.; Pulvirenti, A.; Catassi, C.; SIGENP Working Group of Weaning and CD Risk. Mode of Delivery and Risk of Celiac Disease: Risk of Celiac Disease and Age at Gluten Introduction Cohort Study. J. Pediatr. 2017, 184, 81–86. [Google Scholar] [CrossRef]
- Romanos, J.; van Diemen, C.C.; Nolte, I.M.; Trynka, G.; Zhernakova, A.; Fu, J.; Bardella, M.T.; Barisani, D.; McManus, R.; van Heel, D.A.; et al. Analysis of HLA and non-HLA alleles can identify individuals at high risk for celiac disease. Gastroenterology 2009, 137, 834–840. [Google Scholar] [CrossRef]
- Oberhuber, G.; Granditsch, G.; Vogelsang, H. The histopathology of coeliac disease: Time for a standardized report scheme for pathologists. Eur. J. Gastroenterol. Hepatol. 1999, 11, 1185–1194. [Google Scholar] [CrossRef]
- Auricchio, R.; Tosco, A.; Piccolo, E.; Galatola, M.; Izzo, V.; Maglio, M.; Paparo, F.; Troncone, R.; Greco, L. Potential celiac children: 9-year follow-up on a gluten-containing diet. Am. J. Gastroenterol. 2014, 109, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Kurppa, K.; Ashorn, M.; Iltanen, S.; Koskinen, L.L.; Saavalainen, P.; Koskinen, O.; Mäki, M.; Kaukinen, K. Celiac disease without villous atrophy in children: A prospective study. J. Pediatr. 2010, 157, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Mandile, R.; Discepolo, V.; Scapaticci, S.; Del Vecchio, M.R.; Maglio, M.A.; Greco, L.; Troncone, R.; Auricchio, R. The Effect of Gluten-free Diet on Clinical Symptoms and the Intestinal Mucosa of Patients With Potential Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 654–656. [Google Scholar] [CrossRef] [PubMed]
- Biagi, F.; Trotta, L.; Alfano, C.; Balduzzi, D.; Staffieri, V.; Bianchi, P.I.; Marchese, A.; Vattiato, C.; Zilli, A.; Luinetti, O.; et al. Prevalence and natural history of potential celiac disease in adult patients. Scand. J. Gastroenterol. 2013, 48, 537–542. [Google Scholar] [CrossRef]
- Volta, U.; Caio, G.; Giancola, F.; Rhoden, K.J.; Ruggeri, E.; Boschetti, E.; Stanghellini, V.; De Giorgio, R. Features and Progression of Potential Celiac Disease in Adults. Clin. Gastroenterol. Hepatol. 2016, 14, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Simell, S.; Hoppu, S.; Simell, T.; Ståhlberg, M.R.; Viander, M.; Routi, T.; Simell, V.; Veijola, R.; Ilonen, J.; Hyöty, H. Age at development of type 1 diabetes- and celiac diseaseassociated antibodies and clinical disease in genetically susceptible children observed from birth. Diabetes Care. 2010, 33, 774–779. [Google Scholar] [CrossRef] [PubMed]
- Bjorck, S.; Brundin, C.; Lorinc, E.; Lynch, K.F.; Agardh, D. Screening detects a high proportion of celiac disease in young HLA-genotyped children. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Waisbourd-Zinman, O.; Hojsak, I.; Rosenbach, Y.; Mozer-Glassberg, Y.; Shalitin, S.; Phillip, M.; Shamir, R. Spontaneous normalization of anti-tissue transglutaminase antibody levels is common in children with type 1 diabetes mellitus. Dig. Dis. Sci. 2012, 57, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- Castellaneta, S.; Piccinno, E.; Oliva, M.; Cristofori, F.; Vendemiale, M.; Ortolani, F.; Papadia, F.; Catassi, C.; Cavallo, L.; Francavilla, R. High rate of spontaneous normalization of celiac serology in a cohort of 446 children with type 1 diabetes: A prospective study. Diabetes Care. 2015, 38, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Liu, E.; Dong, F.; Barón, A.E.; Taki, I.; Norris, J.M.; Frohnert, B.I.; Hoffenberg, E.J.; Rewers, M. High Incidence of Celiac Disease in a Long-term Study of Adolescents With Susceptibility Genotypes. Gastroenterology 2017, 152, 1329–1336. [Google Scholar] [CrossRef]
- Troncone, R.; Jabri, B. Coeliac disease and gluten sensitivity. J. Intern. Med. 2011, 269, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Lundin, K.E. Commentary: Transient coeliac disease back on stage again? Scand. J. Gastroenterol. 2005, 40, 1137–1139. [Google Scholar] [CrossRef] [PubMed]
| Not-Developing Overt CD (n = 20) | Developing Overt CD (n = 3) | |
|---|---|---|
| Median age at diagnosis, mo | 24 | 36 |
| Female sex, no. (%) | 10 (50) | 2 (66.7) |
| First-degree relative with CD, no. (%) | ||
| Type of relative | ||
| Father | 1 (5) | 2 (66.7) |
| Mother | 9 (45) | 0 |
| Brother | 2 (10) | 0 |
| Sister | 8 (40) | 1 (33.3) |
| Breastfed, no. (%) | 16 (80) | 1 (33.3) |
| Duration of breastfeeding, mo | 6.3 ± 5.8 | 9 ± 15.6 |
| Introduction of gluten, no. (%) | ||
| At 6 mo, Group A | 13 (65) | 1 (33.3) |
| At 12 mo, Group B | 7 (35) | 2 (66.7) |
| TGA2 level at diagnosis, xUNL | 5.0 ± 4.6 | 4.7 ± 4.3 |
| Caesarean delivery, no. (%) | 7 (35) | 2 (66.7) |
| HLA genotype, no. (%) | ||
| Standard risk | 14 (70) | 1 (33.3) |
| High risk | 6 (30) | 2 (66.7) |
| Marsh score at first biopsy, no. (%) | ||
| Marsh 0 | 13 (65) | 1 (33.3) |
| Marsh 1 | 7 (35) | 2 (66.7) |
| Serology outcome (TGA2 and EMA), no. (%) | ||
| Persistent positivity * | 0 | 2 (66.7) |
| Fluctuation | 1 (5%) | 1 (33.3) |
| Spontaneous remission * | 19 (95%) | 0 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lionetti, E.; Castellaneta, S.; Francavilla, R.; Pulvirenti, A.; Naspi Catassi, G.; Catassi, C.; The SIGENP Working Group of Weaning and CD Risk. Long-Term Outcome of Potential Celiac Disease in Genetically at-Risk Children: The Prospective CELIPREV Cohort Study. J. Clin. Med. 2019, 8, 186. https://doi.org/10.3390/jcm8020186
Lionetti E, Castellaneta S, Francavilla R, Pulvirenti A, Naspi Catassi G, Catassi C, The SIGENP Working Group of Weaning and CD Risk. Long-Term Outcome of Potential Celiac Disease in Genetically at-Risk Children: The Prospective CELIPREV Cohort Study. Journal of Clinical Medicine. 2019; 8(2):186. https://doi.org/10.3390/jcm8020186
Chicago/Turabian StyleLionetti, Elena, Stefania Castellaneta, Ruggiero Francavilla, Alfredo Pulvirenti, Giulia Naspi Catassi, Carlo Catassi, and The SIGENP Working Group of Weaning and CD Risk. 2019. "Long-Term Outcome of Potential Celiac Disease in Genetically at-Risk Children: The Prospective CELIPREV Cohort Study" Journal of Clinical Medicine 8, no. 2: 186. https://doi.org/10.3390/jcm8020186
APA StyleLionetti, E., Castellaneta, S., Francavilla, R., Pulvirenti, A., Naspi Catassi, G., Catassi, C., & The SIGENP Working Group of Weaning and CD Risk. (2019). Long-Term Outcome of Potential Celiac Disease in Genetically at-Risk Children: The Prospective CELIPREV Cohort Study. Journal of Clinical Medicine, 8(2), 186. https://doi.org/10.3390/jcm8020186








