Effects of Adding Interferential Therapy Electro-Massage to Usual Care after Surgery in Subacromial Pain Syndrome: A Randomized Clinical Trial
Abstract
1. Introduction
2. Methods
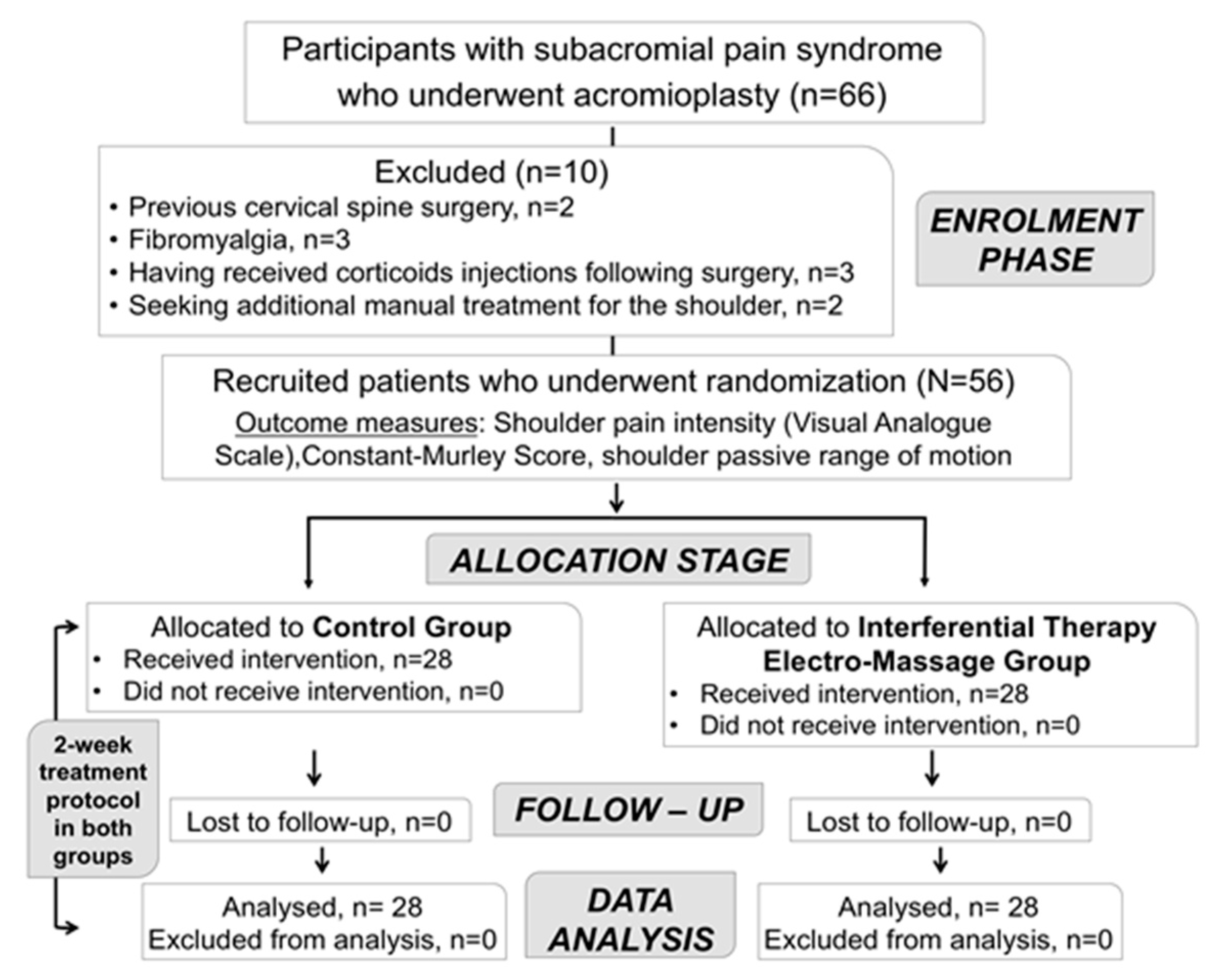
2.1. Study Design
2.2. Participants
2.3. Study Protocol
2.4. Outcome Measures
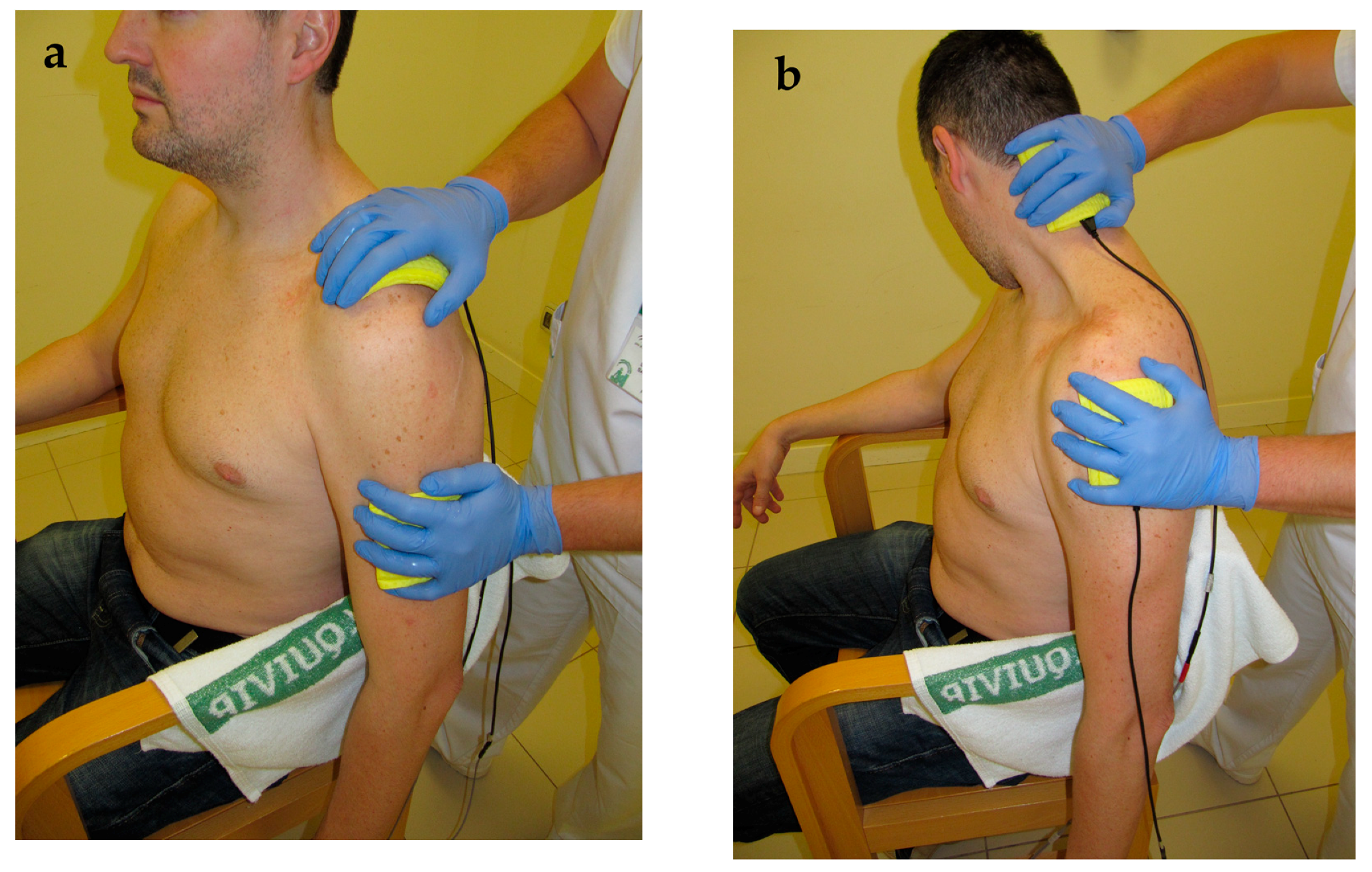
2.5. Interventions
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef]
- Van der Windt, D.A.; Thomas, E.; Pope, D.P.; de Winter, A.F.; Macfarlane, G.J.; Bouter, L.M.; Silman, A.J. Occupational risk factors for shoulder pain: A systematic review. Occup. Environ. Med. 2000, 57, 433–442. [Google Scholar] [CrossRef]
- Calvo Lobo, C.; Romero Morales, C.; Rodríguez Sanz, D.; Sanz Corbalán, I.; Sánchez Romero, E.A.; Fernández Carnero, J.; López López, D. Comparison of hand grip strength and upper limb pressure pain threshold between older adults with or without non-specific shoulder pain. PeerJ 2017, 5, e2995. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, C.; Adebajo, A.; Hay, E.; Carr, A. Shoulder pain: Diagnosis and management in primary care. BMJ 2005, 331, 1124–1128. [Google Scholar] [CrossRef] [PubMed]
- Diercks, R.; Bron, C.; Dorrestijn, O.; Meskers, C.; Naber, R.; de Ruiter, T.; Willems, J.; Winters, J.; van der Woude, H.J.; Association, D.O. Guideline for diagnosis and treatment of subacromial pain syndrome: A multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop. 2014, 85, 314–322. [Google Scholar] [CrossRef]
- Lewis, J.; Sim, J.; Barlas, P. Acupuncture and electro-acupuncture for people diagnosed with subacromial pain syndrome: A multicentre randomized trial. Eur. J. Pain 2017, 21, 1007–1019. [Google Scholar] [CrossRef] [PubMed]
- Tangrood, Z.J.; Gisselman, A.S.; Sole, G.; Ribeiro, D.C. Clinical course of pain and disability in patients with subacromial shoulder pain: A systematic review protocol. BMJ Open 2018, 8, e019393. [Google Scholar] [CrossRef]
- Virta, L.; Joranger, P.; Brox, J.I.; Eriksson, R. Costs of shoulder pain and resource use in primary health care: A cost-of-illness study in Sweden. BMC Musculoskelet. Disord. 2012, 13, 17. [Google Scholar] [CrossRef] [PubMed]
- Desmeules, F.; Braën, C.; Lamontagne, M.; Dionne, C.E.; Roy, J.S. Determinants and predictors of absenteeism and return-to-work in workers with shoulder disorders. Work 2016, 55, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Faber, E.; Kuiper, J.I.; Burdorf, A.; Miedema, H.S.; Verhaar, J.A. Treatment of impingement syndrome: A systematic review of the effects on functional limitations and return to work. J. Occup. Rehabil. 2006, 16, 7–25. [Google Scholar] [CrossRef] [PubMed]
- Steuri, R.; Sattelmayer, M.; Elsig, S.; Kolly, C.; Tal, A.; Taeymans, J.; Hilfiker, R. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: A systematic review and meta-analysis of RCTs. Br. J. Sports Med. 2017, 51, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Lobo, C.; Pacheco-da-Costa, S.; Hita-Herranz, E. Efficacy of deep dry needling on latent myofascial trigger points in older adults with nonspecific shoulder pain: A randomized, controlled clinical trial pilot study. J. Geriatr. Phys. Ther. 2017, 40, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Wu, W.T.; Han, D.S.; Özçakar, L. Static and dynamic shoulder imaging to predict initial effectiveness and recurrence after ultrasound-guided subacromial corticosteroid injections. Arch. Phys. Med. Rehabil. 2017, 98, 1984–1994. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Mezian, K.; Naňka, O.; Wu, W.T.; Lin, C.P.; Özçakar, L. Ultrasound-guided interventions for painful shoulder: From anatomy to evidence. J. Pain Res. 2018, 11, 2311–2322. [Google Scholar] [CrossRef] [PubMed]
- Beard, D.J.; Rees, J.L.; Cook, J.A.; Rombach, I.; Cooper, C.; Merritt, N.; Shirkey, B.A.; Donovan, J.L.; Gwilym, S.; Savulescu, J.; et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): A multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet 2018, 391, 329–338. [Google Scholar] [CrossRef]
- Dong, W.; Goost, H.; Lin, X.B.; Burger, C.; Paul, C.; Wang, Z.L.; Zhang, T.Y.; Jiang, Z.C.; Welle, K.; Kabir, K. Treatments for shoulder impingement syndrome: A PRISMA systematic review and network meta-analysis. Medicine 2015, 94, e510. [Google Scholar] [CrossRef] [PubMed]
- Dorrestijn, O.; Stevens, M.; Winters, J.C.; van der Meer, K.; Diercks, R.L. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. J. Should. Elb. Surg. 2009, 18, 652–660. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.; Cil, A.; Harmsen, W.S.; Schleck, C.; Sperling, J.W.; Cofield, R.H. Arthroscopy and the dramatic increase in frequency of anterior acromioplasty from 1980 to 2005: An epidemiologic study. Arthroscopy 2010, 26, S142–S147. [Google Scholar] [CrossRef]
- Vitale, M.A.; Arons, R.R.; Hurwitz, S.; Ahmad, C.S.; Levine, W.N. The rising incidence of acromioplasty. J. Bone Jt. Surg. Am. 2010, 92, 1842–1850. [Google Scholar] [CrossRef]
- Christiansen, D.H.; Frost, P.; Falla, D.; Haahr, J.P.; Frich, L.H.; Andrea, L.C.; Svendsen, S.W. Effectiveness of standardized physical therapy exercises for patients with difficulty returning to usual activities after decompression surgery for subacromial impingement syndrome: Randomized controlled trial. Phys. Ther. 2016, 96, 787–796. [Google Scholar] [CrossRef]
- Pastora-Bernal, J.M.; Martín-Valero, R.; Barón-López, F.J.; Moyano, N.G.; Estebanez-Pérez, M.J. Telerehabilitation after arthroscopic subacromial decompression is effective and not inferior to standard practice: Preliminary results. J. Telemed. Telecare 2018, 24, 428–433. [Google Scholar] [CrossRef]
- Beatti, A.; Raynor, A.; Souvlis, T.; Chipchase, L. The analgesic effect of interferential therapy on clinical and experimentally induced pain. Phys. Ther. Rev. 2010, 15, 243–252. [Google Scholar] [CrossRef]
- Lara-Palomo, I.C.; Aguilar-Ferrándiz, M.E.; Matarán-Peñarrocha, G.A.; Saavedra-Hernández, M.; Granero-Molina, J.; Fernández-Sola, C.; Castro-Sánchez, A.M. Short-term effects of interferential current electro-massage in adults with chronic non-specific low back pain: A randomized controlled trial. Clin. Rehabil. 2013, 27, 439–449. [Google Scholar] [CrossRef] [PubMed]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 2006, 15 (Suppl. 2), S192–S300. [Google Scholar] [CrossRef]
- Yu, H.; Côté, P.; Shearer, H.M.; Wong, J.J.; Sutton, D.A.; Randhawa, K.A.; Varatharajan, S.; Southerst, D.; Mior, S.A.; Ameis, A.; et al. Effectiveness of passive physical modalities for shoulder pain: Systematic review by the Ontario protocol for traffic injury management collaboration. Phys. Ther. 2015, 95, 306–318. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Green, S.; Mrocki, M.A.; Surace, S.J.; Deitch, J.; McBain, B.; Lyttle, N.; Buchbinder, R. Electrotherapy modalities for rotator cuff disease. Cochrane Database Syst. Rev. 2016, 6, CD012225. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, J.P.; Armijo Olivo, S.; Magee, D.J.; Gross, D.P. Effectiveness of interferential current therapy in the management of musculoskeletal pain: A systematic review and meta-analysis. Phys. Ther. 2010, 90, 1219–1238. [Google Scholar] [CrossRef]
- Nazligul, T.; Akpinar, P.; Aktas, I.; Unlu Ozkan, F.; Cagliyan Hartevioglu, H. The effect of interferential current therapy on patients with subacromial impingement syndrome: A randomized, double-blind, sham-controlled study. Eur. J. Phys. Rehabil. Med. 2018, 54, 351–357. [Google Scholar] [CrossRef]
- Kelly, S.M.; Wrightson, P.A.; Meads, C.A. Clinical outcomes of exercise in the management of subacromial impingement syndrome: A systematic review. Clin. Rehabil. 2010, 24, 99–109. [Google Scholar] [CrossRef]
- Cadogan, A.; McNair, P.J.; Laslett, M.; Hing, W.A. Diagnostic accuracy of clinical examination and imaging findings for identifying subacromial pain. PLoS ONE 2016, 11, e0167738. [Google Scholar] [CrossRef]
- Van Kampen, D.A.; van den Berg, T.; van der Woude, H.J.; Castelein, R.M.; Scholtes, V.A.; Terwee, C.B.; Willems, W.J. The diagnostic value of the combination of patient characteristics, history, and clinical shoulder tests for the diagnosis of rotator cuff tear. J. Orthop. Surg. Res. 2014, 9, 70. [Google Scholar] [CrossRef] [PubMed]
- Hegedus, E.J.; Goode, A.P.; Cook, C.E.; Michener, L.; Myer, C.A.; Myer, D.M.; Wright, A.A. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br. J. Sports Med. 2012, 46, 964–978. [Google Scholar] [CrossRef] [PubMed]
- Michener, L.A.; Walsworth, M.K.; Doukas, W.C.; Murphy, K.P. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch. Phys. Med. Rehabil. 2009, 90, 1898–1903. [Google Scholar] [CrossRef] [PubMed]
- Kvalvaag, E.; Røe, C.; Engebretsen, K.B.; Soberg, H.L.; Juel, N.G.; Bautz-Holter, E.; Sandvik, L.; Brox, J.I. One year results of a randomized controlled trial on radial extracorporeal shock wave treatment, with predictors of pain, disability and return to work in patients with subacromial pain syndrome. Eur. J. Phys. Rehabil. Med. 2018, 54, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Paavola, M.; Malmivaara, A.; Taimela, S.; Kanto, K.; Järvinen, T.L.; Investigators, F. Finnish Subacromial Impingement Arthroscopy Controlled Trial (FIMPACT): A protocol for a randomised trial comparing arthroscopic subacromial decompression and diagnostic arthroscopy (placebo control), with an exercise therapy control, in the treatment of shoulder impingement syndrome. BMJ Open 2017, 7, e014087. [Google Scholar] [CrossRef] [PubMed]
- Albornoz-Cabello, M.; Maya-Martín, J.; Domínguez-Maldonado, G.; Espejo-Antúnez, L.; Heredia-Rizo, A.M. Effect of interferential current therapy on pain perception and disability level in subjects with chronic low back pain: A randomized controlled trial. Clin. Rehabil. 2017, 31, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Albornoz-Cabello, M.; Rebollo, J.; García, R. Personal Psychological Apprehension Scale (EAPP) in physical therapy. Rev. Iberoam. Fisioter. Kinesiol. 2005, 8, 77–87. [Google Scholar] [CrossRef]
- Houghton, P.E.; Nussbaum, E.L.; Hoens, A.M. Electrophysical agents—Contraindications and precautions: An evidence-based approach to clinical decision making in physical therapy. Physiother. Can. 2010, 62, 1–80. [Google Scholar] [CrossRef]
- Albornoz-Cabello, M.; Maya-Martin, J.; Toledo-Marhuenda, J.V. Electroterapia practica. Avances en Investigación Clínica; Elsevier: Barcelona, Spain, 2016. [Google Scholar]
- Holmgren, T.; Oberg, B.; Sjöberg, I.; Johansson, K. Supervised strengthening exercises versus home-based movement exercises after arthroscopic acromioplasty: A randomized clinical trial. J. Rehabil. Med. 2012, 44, 12–18. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63 (Suppl. 11), S240–S252. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Wyrwich, K.W.; Beaton, D.; Cleeland, C.S.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Kerns, R.D.; Ader, D.N.; et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J. Pain 2008, 9, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Tashjian, R.Z.; Deloach, J.; Porucznik, C.A.; Powell, A.P. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J. Should. Elb. Surg. 2009, 18, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Romeo, A.A.; Mazzocca, A.; Hang, D.W.; Shott, S.; Bach, B.R. Shoulder scoring scales for the evaluation of rotator cuff repair. Clin. Orthop. Relat. Res. 2004, 427, 107–114. [Google Scholar] [CrossRef]
- Henseler, J.F.; Kolk, A.; van der Zwaal, P.; Nagels, J.; Vliet Vlieland, T.P.; Nelissen, R.G. The minimal detectable change of the Constant score in impingement, full-thickness tears, and massive rotator cuff tears. J. Should. Elb. Surg. 2015, 24, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Werner, B.C.; Holzgrefe, R.E.; Griffin, J.W.; Lyons, M.L.; Cosgrove, C.T.; Hart, J.M.; Brockmeier, S.F. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J. Should. Elb. Surg. 2014, 23, e275–e282. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Vargas, A.I.; Roldán-Jiménez, C. Validity and reliability of arm abduction angle measured on smartphone: A cross-sectional study. BMC Musculoskelet. Disord. 2016, 17, 93. [Google Scholar] [CrossRef]
- Mejia-Hernandez, K.; Chang, A.; Eardley-Harris, N.; Jaarsma, R.; Gill, T.K.; McLean, J.M. Smartphone applications for the evaluation of pathologic shoulder range of motion and shoulder scores-a comparative study. JSES Open Access 2018, 2, 109–114. [Google Scholar] [CrossRef]
- Jones, A.; Sealey, R.; Crowe, M.; Gordon, S. Concurrent validity and reliability of the Simple Goniometer iPhone app compared with the Universal Goniometer. Physiother. Theory Pract. 2014, 30, 512–516. [Google Scholar] [CrossRef]
- Koh, P.S.; Seo, B.K.; Cho, N.S.; Park, H.S.; Park, D.S.; Baek, Y.H. Clinical effectiveness of bee venom acupuncture and physiotherapy in the treatment of adhesive capsulitis: A randomized controlled trial. J. Should. Elb. Surg. 2013, 22, 1053–1062. [Google Scholar] [CrossRef]
- Kuhn, J.E. Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol. J. Should. Elb. Surg. 2009, 18, 138–160. [Google Scholar] [CrossRef]
- Karel, Y.H.J.M.; Scholten-Peeters, G.G.M.; Thoomes-de Graaf, M.; Duijn, E.; van Broekhoven, J.B.; Koes, B.W.; Verhagen, A.P. Physiotherapy for patients with shoulder pain in primary care: A descriptive study of diagnostic- and therapeutic management. Physiotherapy 2017, 103, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Van Der Heijden, G.J.; Leffers, P.; Wolters, P.J.; Verheijden, J.J.; van Mameren, H.; Houben, J.P.; Bouter, L.M.; Knipschild, P.G. No effect of bipolar interferential electrotherapy and pulsed ultrasound for soft tissue shoulder disorders: A randomised controlled trial. Ann. Rheum. Dis. 1999, 58, 530–540. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.A.F.P.; Dibai-Filho, A.V.; Moreira, W.A.; Rivas, S.Q.; Silva, E.D.S.; Garrido, A.C.B. Effect of adding interferential current in an exercise and manual therapy program for patients with unilateral shoulder impingement syndrome: A randomized clinical trial. J. Manip. Physiol. Ther. 2018, 41, 218–226. [Google Scholar] [CrossRef]
- Cheing, G.L.; So, E.M.; Chao, C.Y. Effectiveness of electroacupuncture and interferential eloctrotherapy in the management of frozen shoulder. J. Rehabil. Med. 2008, 40, 166–170. [Google Scholar] [CrossRef]
- Alptekin, H.K.; Aydın, T.; İflazoğlu, E.S.; Alkan, M. Evaluatıng the effectiveness of frozen shoulder treatment on the right and left sides. J. Phys. Ther. Sci. 2016, 28, 207–212. [Google Scholar] [CrossRef]
- Suriya-amarit, D.; Gaogasigam, C.; Siriphorn, A.; Boonyong, S. Effect of interferential current stimulation in management of hemiplegic shoulder pain. Arch. Phys. Med. Rehabil. 2014, 95, 1441–1446. [Google Scholar] [CrossRef]
- Gunay Ucurum, S.; Kaya, D.O.; Kayali, Y.; Askin, A.; Tekindal, M.A. Comparison of different electrotherapy methods and exercise therapy in shoulder impingement syndrome: A prospective randomized controlled trial. Acta Orthop. Traumatol. Turc. 2018, 52, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Resende, L.; Merriwether, E.; Rampazo, É.; Dailey, D.; Embree, J.; Deberg, J.; Liebano, R.E.; Sluka, K.A. Meta-analysis of transcutaneous electrical nerve stimulation for relief of spinal pain. Eur. J. Pain 2018, 22, 663–678. [Google Scholar] [CrossRef] [PubMed]
- Venancio, R.C.; Pelegrini, S.; Gomes, D.Q.; Nakano, E.Y.; Liebano, R.E. Effects of carrier frequency of interferential current on pressure pain threshold and sensory comfort in humans. Arch. Phys. Med. Rehabil. 2013, 94, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Oosterhof, J.; Wilder-Smith, O.H.; de Boo, T.; Oostendorp, R.A.; Crul, B.J. The long-term outcome of transcutaneous electrical nerve stimulation in the treatment for patients with chronic pain: A randomized, placebo-controlled trial. Pain Pract. 2012, 12, 513–522. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, J.; Armijo-Olivo, S.; Funabashi, M.; Miciak, M.; Dick, B.; Warren, S.; Rashiq, S.; Magee, D.J.; Gross, D.P. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: An experimental controlled study. Phys. Ther. 2014, 94, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Fuentes-Contreras, J.; Armijo-Olivo, S.; Magee, D.J.; Gross, D.P. A preliminary investigation into the effects of active interferential current therapy and placebo on pressure pain sensitivity: A random crossover placebo controlled study. Physiotherapy 2011, 97, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Jarit, G.J.; Mohr, K.J.; Waller, R.; Glousman, R.E. The effects of home interferential therapy on post-operative pain, edema, and range of motion of the knee. Clin. J. Sport Med. 2003, 13, 16–20. [Google Scholar] [CrossRef] [PubMed]
| Contraindications |
|---|
| • Acute inflammation |
| • Pregnancy |
| • Use of electronic devices, including cardiac pacemakers |
| • Active deep vein thrombosis or thrombophlebitis |
| • Tumoral diseases |
| • Use of metal implants when the subject refers unpleasant sensations |
| • Untreated hemorrhagic conditions or active bleeding tissues |
| • Recently radiated tissues |
| • Active tuberculosis, infected tissues, or wounds with underlying osteomyelitis • To the neck or head in individuals with previous seizures • To anterior neck, carotid sinus, over the eyes, or reproductive organs |
| Variable | Intereferential Therapy Electro-Massage Group (n = 28) | Control Group (n = 28) | p Value |
|---|---|---|---|
| Mean age (years) | 47.2 ± 11.6 | 51.9 ± 13.1 | 0.159 |
| Sex (female) % (n) | 42.9% (12) | 64.3% (18) | 0.111 |
| Height (cm) | 170.18 ± 9.21 | 164.64 ± 9.27 | 0.029 |
| Weight (kg) | 80.53 ± 12.72 | 75.71 ± 15.44 | 0.208 |
| Body mass index (kg/m2) | 27.76 ± 3.37 | 27.93 ± 5.08 | 0.884 |
| Arthroscopy surgery % (n) | 85.7% (24) | 89.3% (25) | 0.689 |
| Days after surgery * | 42 (21–58) | 51 (18–62) | 0.221 |
| Affected shoulder; right % (n) | 50% (14) | 57.1% (16) | 0.595 |
| PPAS | 34.21 ± 4.74 | 33.54 ± 9.78 | 0.743 |
| Visual analogue scale (mm) | 69.82 ± 16.74 | 65.71 ± 20.75 | 0.419 |
| Constant-Murley score (0–100) | 29.68 ± 10.4 | 29.71 ± 12.24 | 0.991 |
| Shoulder flexion (°) | 103.61 ± 30.89 | 107.07 ± 32.53 | 0.684 |
| Shoulder extension (°) | 40 ± 10.79 | 40.18 ± 13.3 | 0.956 |
| Shoulder abduction (°) | 84.43 ± 27.5 | 84.25 ± 29.56 | 0.981 |
| Shoulder abduction (°) | 34.5 ± 12.08 | 30.86 ± 9.78 | 0.221 |
| Shoulder internal rotation (°) | 29.32 ± 14.75 | 32.21 ± 8.86 | 0.440 |
| Shoulder external rotation (°) | 59 ± 17.22 | 62.96 ± 20.74 | 0.378 |
| Baseline | After the Two-Week Intervention | Within-Group Changes after Intervention | Between-Group Mean Changes | |
|---|---|---|---|---|
| Visual Analogue Scale (mm) | ||||
| IFT Electro-Massage Group | 69.82 ± 16.74 | 32.68 ± 13.64 | –37.14 ± 13.22 (–42.27 to –32.01) * | –18.92 ± 3.46 (–25.8 to –11.97) † |
| Control Group | 65.71 ± 20.75 | 47.5 ± 22.95 | –18.21 ± 12.71 (–23.14 to –13.28) * | |
| Constant-Murley Score (0–100) | ||||
| IFT Electro-Massage Group | 29.68 ± 10.41 | 56.07 ± 10.96 | 26.39 ± 5.9 (24.1 to 28.68) * | 10.71 ± 1.97 (6.74 to 14.68) † |
| Control Group | 29.71 ± 12.24 | 45.39 ± 13.82 | 15.67 ± 8.61 (12.33 to 19.01) * | |
| Shoulder Flexion (°) | ||||
| IFT Electro-Massage Group | 103.61 ± 30.89 | 146.86 ± 22.1 | 43.25 ± 16.75 (36.75 to 49.74) * | 19.32 ± 4.16 (10.96 to 27.67) † |
| Control Group | 107.07 ± 32.53 | 131 ± 25.93 | 23.92 ± 14.32 (18.37 to 29.4) * | |
| Shoulder Extension (°) | ||||
| IFT Electro-Massage Group | 40 ± 10.79 | 52 ± 9.86 | 12 ± 7.21 (9.2 to 14.79) * | 1.21 ± 0.92 (–2.64 to 5.07) |
| Control Group | 40.18 ± 13.3 | 50.96 ± 10.38 | 10.78 ± 7.21 (7.99 to 13.57) * | |
| Shoulder Abduction (°) | ||||
| IFT Electro-Massage Group | 84.43 ± 27.5 | 112.18 ± 29.1 | 37.75 ± 15.86 (31.6 to 43.9) * | 12.25 ± 4.39 (3.43 to 21.06) † |
| Control Group | 84.25 ± 29.56 | 109.75 ± 30.1 | 25.5 ± 17.01 (18.9 to 32.09) * | |
| Shoulder Adduction (°) | ||||
| IFT Electro-Massage Group | 34.5 ± 12.08 | 45.54 ± 10.87 | 11.03 ± 7.27 (8.21 to 13.85) * | –2.25 ± 2.33 (–6.93 to 2.43) |
| Control Group | 30.86 ± 9.78 | 44.14 ± 12.94 | 13.28 ± 10 (9.4 to 17.16) * | |
| Shoulder Internal Rotation (°) | ||||
| IFT Electro-Massage Group | 29.32 ± 14.75 | 50.61 ± 13.31 | 21.28 ± 7.71 (18.29 to 24.27) * | 10.5 ± 1.85 (6.77 to 14.22) † |
| Control Group | 32.21 ± 8.86 | 43 ± 11.2 | 10.78 ± 6.09 (8.42 to 13.14) * | |
| Shoulder External Rotation (°) | ||||
| IFT Electro-Massage Group | 59 ± 17.22 | 82.5 ± 10.94 | 23.5 ± 13.82 (18.14 to 28.86) * | 9.46 ± 3.2 (2.86 to 16.06) † |
| Control Group | 62.96 ± 20.74 | 77 ± 16.63 | 14.03 ± 10.61 (9.92 to 18.15) * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albornoz-Cabello, M.; Sanchez-Santos, J.A.; Melero-Suarez, R.; Heredia-Rizo, A.M.; Espejo-Antunez, L. Effects of Adding Interferential Therapy Electro-Massage to Usual Care after Surgery in Subacromial Pain Syndrome: A Randomized Clinical Trial. J. Clin. Med. 2019, 8, 175. https://doi.org/10.3390/jcm8020175
Albornoz-Cabello M, Sanchez-Santos JA, Melero-Suarez R, Heredia-Rizo AM, Espejo-Antunez L. Effects of Adding Interferential Therapy Electro-Massage to Usual Care after Surgery in Subacromial Pain Syndrome: A Randomized Clinical Trial. Journal of Clinical Medicine. 2019; 8(2):175. https://doi.org/10.3390/jcm8020175
Chicago/Turabian StyleAlbornoz-Cabello, Manuel, Jose Antonio Sanchez-Santos, Rocio Melero-Suarez, Alberto Marcos Heredia-Rizo, and Luis Espejo-Antunez. 2019. "Effects of Adding Interferential Therapy Electro-Massage to Usual Care after Surgery in Subacromial Pain Syndrome: A Randomized Clinical Trial" Journal of Clinical Medicine 8, no. 2: 175. https://doi.org/10.3390/jcm8020175
APA StyleAlbornoz-Cabello, M., Sanchez-Santos, J. A., Melero-Suarez, R., Heredia-Rizo, A. M., & Espejo-Antunez, L. (2019). Effects of Adding Interferential Therapy Electro-Massage to Usual Care after Surgery in Subacromial Pain Syndrome: A Randomized Clinical Trial. Journal of Clinical Medicine, 8(2), 175. https://doi.org/10.3390/jcm8020175







