Women’s Preferences for Maternal Healthcare Services in Bangladesh: Evidence from a Discrete Choice Experiment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Aim and Objectives
2.2. Study Setting
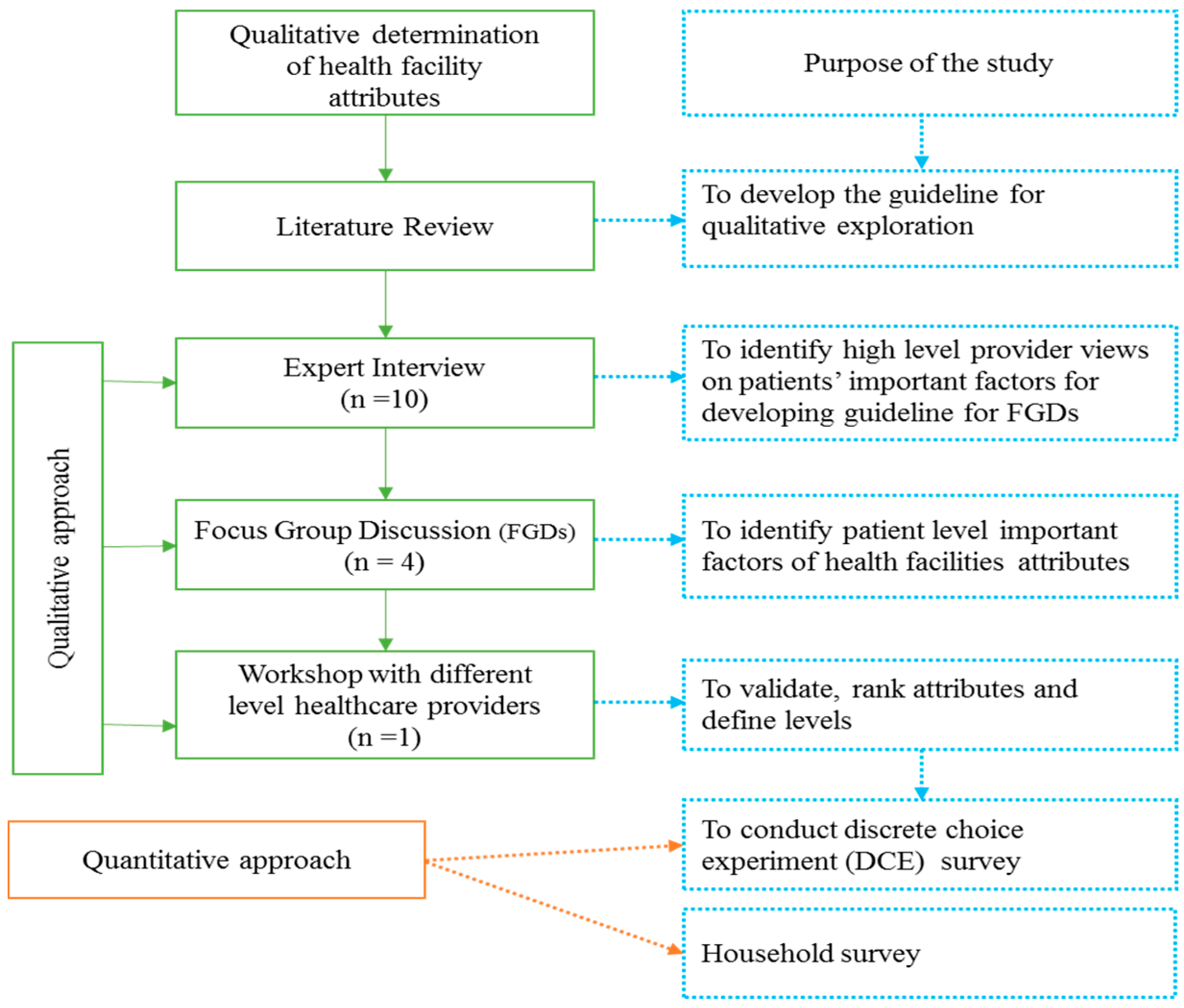
2.3. Research Design
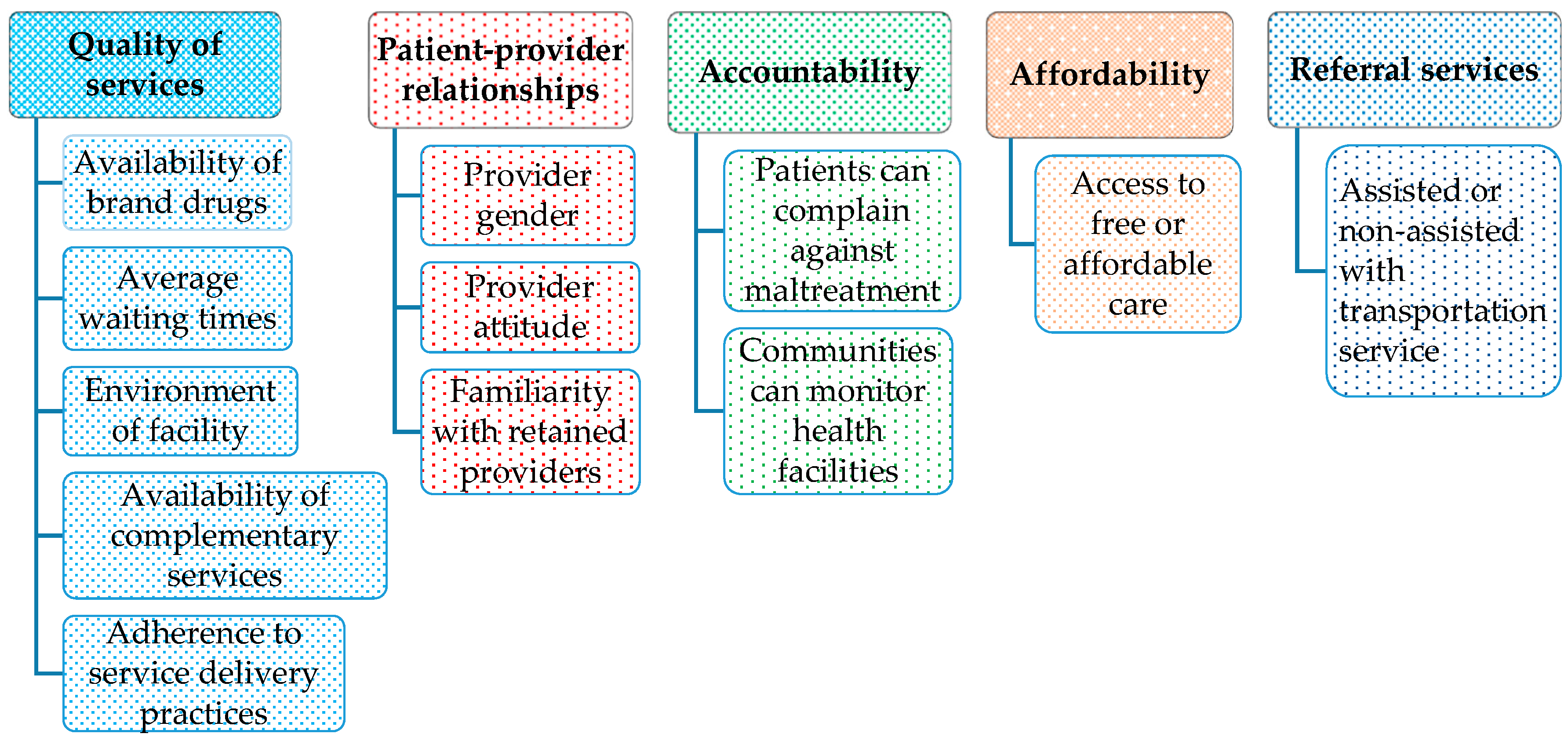
2.4. Qualitative Approach
2.4.1. Literature Review
2.4.2. Expert Interviews
2.4.3. Focus Group Discussions
2.4.4. Final Workshop
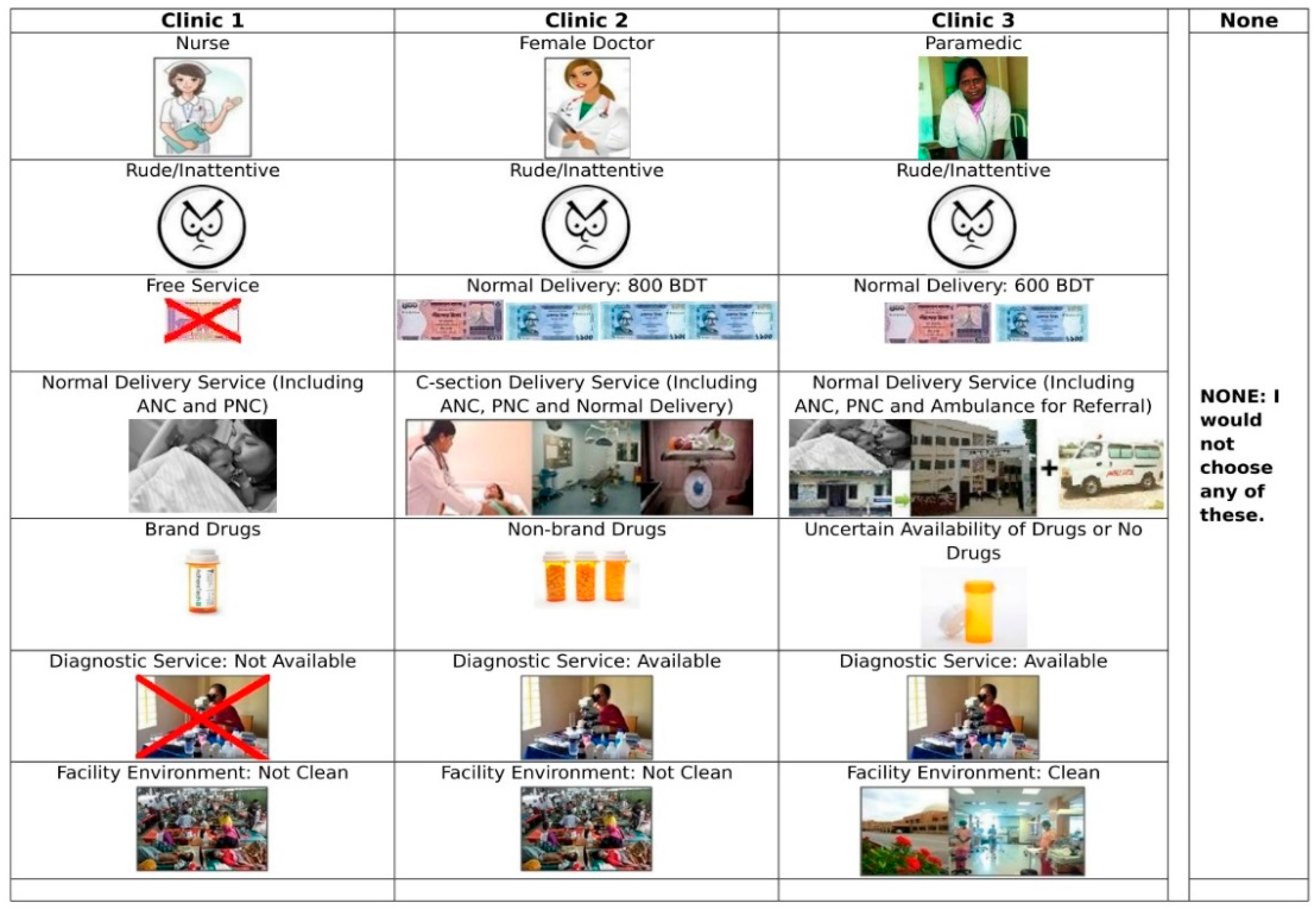
2.5. Quantitative Approach
2.6. Sample Size
2.7. Data Collection Procedure
2.8. Ethical Approval
2.9. Estimation Strategy
2.9.1. Descriptive Analysis
2.9.2. Hierarchical Bayes Analysis
3. Results
3.1. Background Characteristics
3.2. Discrete Choice Experiment Results
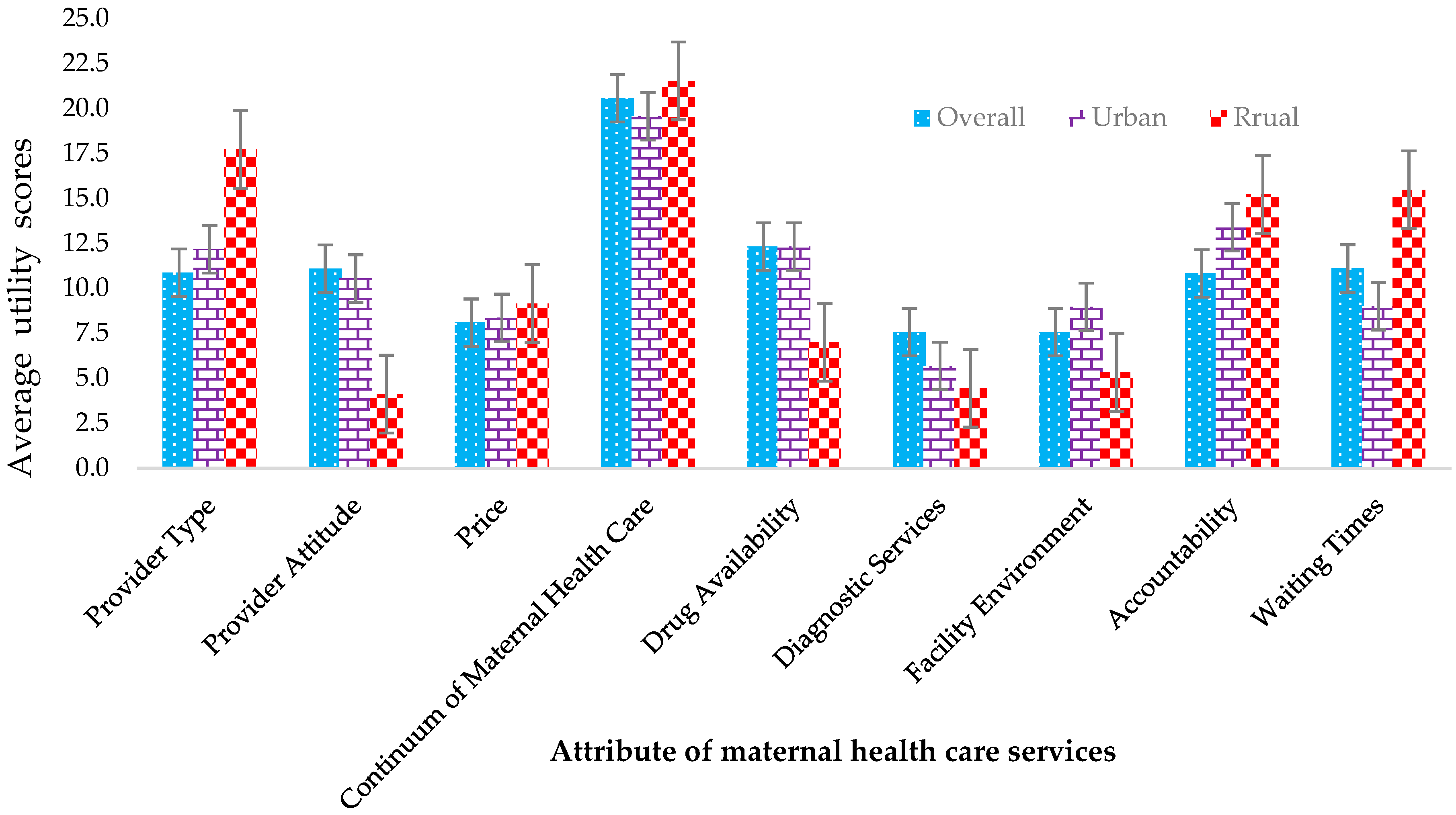
3.2.1. DCE Attribute Rankings by Average Utility
3.2.2. Distribution and Factors Influencing Higher Utility Scores for Maternal Health Services
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A


References
- Memirie, S.T.; Verguet, S.; Norheim, O.F.; Levin, C.; Johansson, K.A. Inequalities in utilization of maternal and child health services in Ethiopia: The role of primary health care. BMC Health Serv. Res. 2016, 16, 51. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Trends in Maternal Mortality: 1990 to 2015; Tech. Rep.; WHO, UNICEF, UNFPA and The World Bank Estimates: Geneva, Switzerland, 2015; Volume 2012. [Google Scholar]
- Alkema, L.; Chou, D.; Hogan, D.; Zhang, S.; Moller, A.B.; Gemmill, A.; Fat, D.M.; Boerma, T.; Temmerman, M.; Mathers, C.; et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the un maternal mortality estimation Inter-Agency group. Lancet 2016, 387, 462–474. [Google Scholar] [CrossRef]
- The World Health Organization (WHO). Maternal Mortality, Department of Reproductive Health and Research; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Akhter, S. Maternal Health Care Seeking Behaviour of Women from Lower and Upper Socio-Economic Groups of Dhaka, Bangladesh—Fear or Fashion? Ph.D. Thesis, School of the Environment, Flinders University, Adelaide, Australia, 2015. [Google Scholar]
- Chowdhury, S.; Banu, L.; Chowdhury, T.; Rubayet, S.; Khatoon, S. Achieving Millennium Development Goals 4 and 5 in Bangladesh. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 36–46. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population Research and Training (NIPORT); MEASURE Evaluation; ICDDR B. Bangladesh Maternal Mortality and Health Care Survey 2010; National Institute of Population Research and Training (NIPORT); MEASURE Evaluation; ICDDR B: Dhaka, Bangladesh, 2012.
- Shahabuddin, A.S.M.; Delvaux, T.; Abouchadi, S.M.S. Utilization of maternal health services among adolescent women in Bangladesh: A scoping review of the literature. Trop. Med. Int. Health 2015, 20, 822–829. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Success Factors for Women’s and Children’s Health: Bangladesh; WHO Press: Geneva, Switzerland, 2015. [Google Scholar]
- Akhter, S. Use of modern maternal health care by mothers in Bangladesh: A critical analysis. Int. Acad. J. Soc. Sci. 2014, 3, 61–76. [Google Scholar]
- MDG-5. (n.d.). Improve Maternal Health. 2015. Available online: http://www.who.int/topics/millennium_development_goals/maternal_health/en/ (accessed on 25 March 2018).
- Lama, S.; Aki, K. Barriers in Utilization of maternal health care services: Perceptions of rural women in Eastern Nepal. Kathmandu Univ. Med. J. 2014, 12, 253–258. [Google Scholar] [CrossRef]
- Hurst, T.E.; Semrau, K.; Patna, M.; Gawande, A.; Hirschhorn, L.R. Demand-side interventions for maternal care: Evidence of more use, not better outcomes. BMC Pregnancy Childbirth 2015, 15, 297. [Google Scholar] [CrossRef]
- Dosari, A.A.F. Causes of adverse pregnancy outcomes and the role of maternal periodontal status—A review of the literature. Open Dent. J. 2012, 6, 79–84. [Google Scholar]
- Jacobs, B.; Ir, P.; Bigdeli, M.; Annear, P.L.; Damme, W.V. Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012, 27, 288–300. [Google Scholar] [CrossRef]
- Ensor, T.; Cooper, S. Overcoming barriers to health service access: Influencing the demand side. Health Policy Plan. 2004, 19, 69–79. [Google Scholar] [CrossRef]
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Rahman, M.H. Poverty and access to health care in developing countries. Ann. N. Y. Acad. Sci. 2008, 1136, 161–171. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, T.S.; Bedford, K.J.; Thiede, M.; McIntyre, D. Synthesizing qualitative and quantitative evidence on non-financial access barriers: Implications for assessment at the district level. Int. J. Equity Health 2015, 14, 54. [Google Scholar] [CrossRef] [PubMed]
- United Nations (UN). Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations General Assembly: New York, NY, USA, 2015. [Google Scholar]
- Louviere, J.; Hensher, D.; Swait, J. Stated Choice Methods: Analysis and Applications; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Bridges, J.F.P.; Hauber, A.B.; Marshall, D.; Lloyd, A.; Prosser, L.A.; Regier, D.A.; Johnson, F.R.; Mauskopf, J. Conjoint analysis applications in health—A checklist: A report of the ISPOR good research practices for conjoint analysis task force. Value Health 2011, 14, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Viney, R.; Lancsar, E.; Louviere, J. Discrete choice experiments to measure consumer preferences for health and healthcare. Expert Rev. Pharmacoecon. Outcomes Res. 2002, 2, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Ryan, M.; Gerard, K. Using discrete choice experiments to value health care programmes: Current practice and future research reflections. Appl. Health Econ. Health Policy 2003, 2, 55–64. [Google Scholar] [PubMed]
- Marshall, D.A.; McGregor, E.; Currie, G. Measuring preferences for colorectal cancer (CRC) screening—What are the implications for moving forward? Patient 2010, 3, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Bridges, J.; Kinter, E.; Kidane, L.; Heinzen, R.R.; McCormick, C. Things are looking up since we started listening to patients: Recent trends in the application of conjoint analysis in health 1970–2007. Patient 2008, 1, 273–282. [Google Scholar] [CrossRef]
- Green, P.E.; Srinivasan, V. Conjoint analysis in consumer research: Issues and outlook. J. Consum. Res. 1978, 5, 103–123. [Google Scholar] [CrossRef]
- Lancsar, E.; Louviere, J. Conducting discrete choice experiments to inform healthcare decision making: A user’s guide. Pharmacoeconomics 2008, 26, 661–677. [Google Scholar] [CrossRef]
- Weston, A.; Fitzgerald, P. Discrete choice experiment to derive willingness to pay for methyl aminolevulinate photodynamic therapy versus simple excision surgery in basal cell carcinoma. Pharmacoeconomics 2004, 22, 1195–1208. [Google Scholar] [CrossRef]
- Kruk, M.E.; Paczkowski, M.M.; Tegegn, A.; Tessema, F.; Hadley, C.; Asefa, M.; Galea, S. Women’s preferences for obstetric care in rural Ethiopia: A population-based discrete choice experiment in a region with low rates of facility delivery. J. Epidemiol. Community Health 2010, 64, 984–988. [Google Scholar] [CrossRef] [PubMed]
- Hollowell, J.; Li, Y.; Malouf, R.; Buchanan, J. Women’s birth place preferences in the United Kingdom: A systematic review and narrative synthesis of the quantitative literature. BMC Pregnancy Childbirth 2016, 16, 213. [Google Scholar] [CrossRef] [PubMed]
- Kruk, M.E.; Paczkowski, M.; Mbaruku, G.; de Pinho, H.; Galea, S. Women’s preferences for place of delivery in rural Tanzania: A population-based discrete choice experiment. Am. J. Public Health 2009, 99, 1666–1672. [Google Scholar] [CrossRef] [PubMed]
- Mühlbacher, A.C.; Lincke, H.-J.; Nübling, M. Evaluating patients’ preferences for multiple myeloma therapy, a discrete-choice experiment. Psychosoc. Med. 2008, 5. [Google Scholar]
- Wittink, M.N.; Cary, M.; TenHave, T.; Baron, J.; Gallo, J.J. Towards patient-centered care for depression: Conjoint methods to tailor treatment based on preferences. Patient 2010, 3, 145–157. [Google Scholar] [CrossRef] [PubMed]
- King, M.T.; Hall, J.; Lancsar, E.; Fiebig, D.; Hossain, I.; Louviere, J.; Reddel, H.K.; Jenkins, C.R. Patient preferences for managing asthma: Results from a discrete choice experiment. Health Econ. 2006, 16, 703–717. [Google Scholar] [CrossRef]
- Roux, L.; Ubach, C.; Donaldson, C.; Ryan, M. Valuing the benefits of weight loss programs: An application of the discrete choice experiment. Obes. Res. 2004, 12, 1342–1351. [Google Scholar] [CrossRef]
- Hauber, A.B.; Johnson, F.R.; Sauriol, L.; Lescrauwaet, B. Risking health to avoid injections: Preferences of Canadians with type 2 diabetes. Diabetes Care 2005, 28, 2243–2245. [Google Scholar] [CrossRef]
- Johnson, F.R.; Manjunath, R.; Mansfield, C.A.; Clayton, L.J.; Hoerger, T.J.; Zhang, P. High-risk individuals’ willingness to pay for diabetes risk-reduction programs. Diabetes Care 2006, 29, 1351–1356. [Google Scholar] [CrossRef]
- Rose, J.M.; Bliemer, M.C.J. Sample size requirements for stated choice experiments. Transportation 2013, 40, 1021–1041. [Google Scholar] [CrossRef]
- Chromy, J.R. Probability proportional to size (PPS) sampling. In Encyclopedia of Survey Research Methods; Lavrakas, P.J., Ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2011. [Google Scholar]
- Sawtooth’s Choice-Based Conjoint with Hierarchical Bayes [Computer Program]. Version 4.4.6.; Sawtooth Software Inc.: Sequim, WA, USA, 2007.
- Howell, J. Sawtooth Software-Research Paper Series: CBC/HB for Beginners; Sawtooth Software Inc.: Sequim, WA, USA, 2009. [Google Scholar]
- Sarker, B.K.; Rahman, M.; Rahman, T.; Hossain, J.; Reichenbach, L.; Mitra, D.K. Reasons for preference of home delivery with traditional birth attendants (TBAs) in Rural Bangladesh: A qualitative exploration. PLoS ONE 2016, 11, e0146161. [Google Scholar] [CrossRef] [PubMed]
- Some, T.D.; Sombie, I.; Meda, N. Women’s perceptions of homebirths in two rural medical districts in Burkina Faso: A qualitative study. Reprod. Health 2011, 8, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Titaley, C.R.; Hunter, C.L.; Dibley, M.J.; Heywood, P. Why do some women still prefer traditional birth attendants and home delivery? A qualitative study on delivery care services in West Java Province, Indonesia. BMC Pregnancy Childbirth 2010, 10, 43. [Google Scholar] [CrossRef] [PubMed]
- Sychareun, V.; Hansana, V.; Somphet, V.; Xayavong, S.; Phengsavanh, A.; Popenoe, R. Reasons rural laotians choose home deliveries over delivery at health facilities: A qualitative study. BMC Pregnancy Childbirth. 2012, 12, 86. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Regional Office for the Western Pacific. Bangladesh Health System Review; WHO Regional Office for the Western Pacific: Manila, Philippines, 2015; Available online: http://www.who.int/iris/handle/10665/208214 (accessed on 20 October 2018).
- Aktar, S. Health care seeking behavior for safe motherhood: Findings from rural Bangladesh. Bangladesh E-J. Sociol. 2012, 9, 57–70. [Google Scholar]
- Islam, M.S.; Ullah, M.W. People’s Participation in Health Services: A study of Bangladesh ’s Rural Health Complex; No. BDRWPS 7; Bangladesh Development Research Center (BDRC): Falls Church, VA, USA, 2009; Volume 7. [Google Scholar]
- Okonofua, F.; Ogu, R.; Agholor, K.; Okike, O.; Abdus-salam, R.; Gana, M.; Randawa, A.; Abe, E.; Durodola, A.; Galadanci, H. Qualitative assessment of women’s satisfaction with maternal health care in referral hospitals in Nigeria. Reprod. Health 2017, 14, 44. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Shengelia, L. Analysis on maternal healthcare situation Bangladesh: A review. Divers. Equal. Health Care 2016, 13, 360–364. [Google Scholar] [CrossRef]
- The World Health Organization (WHO). Sexual and Reproductive Health: Prevention and Elimination of Disrespect and Abuse During Childbirth. Available online: http://www.who.int/reproductivehealth/topics/maternal_perinatal/statement-childbirth-programs/en/ (accessed on 15 January 2019).
- Alam, N.; Chowdhury, M.E.; Kouanda, S.; Seppey, M.; Alam, A.; Savadogo, J.R.; Fournier, P. The role of transportation to access maternal care services for women in rural Bangladesh and Burkina Faso: A mixed methods study. Int. J. Gynaecol. Obstet. 2016, 135, S45–S50. [Google Scholar] [CrossRef] [PubMed]
- Larson, E.; Vail, D.; Mbaruku, G.M.; Kimweri, A.; Freedman, L.P.; Kruk, M.E. Moving toward patient-centered care in Africa: A discrete choice experiment of preferences for delivery care among 3003 Tanzanian women. PLoS ONE 2015, 10, e0135621. [Google Scholar] [CrossRef]
- Shayo, E.H.; Senkoro, K.P.; Momburi, R.; Olsen, O.E.; Byskov, J.; Makundi, E.A.; Mboera, L.E.G. Access and utilisation of healthcare services in rural Tanzania: A comparison of public and non-public facilities using quality, equity, and trust dimensions. Glob. Public Health 2016, 11, 407–422. [Google Scholar] [CrossRef] [PubMed]
- Ryan, M.; Farrar, S. Using conjoint analysis to elicit preferences for health care. BMJ 2000, 320, 1530–1533. [Google Scholar] [CrossRef] [PubMed]
- Sarker, A.R.; Sheikh, N.; Mahumud, R.A.; Sultana, M. Determinants of adolescent maternal healthcare utilization in Bangladesh. Public Health 2018, 157, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Sultana, M.; Mahumud, R.A.; Ali, N.; Ahmed, S.; Islam, Z.; Khan, J.A.M.; Sarker, A.R. Cost of introducing group prenatal care (GPC) in Bangladesh: A supply-side perspective. Saf. Health 2017, 3, 8. [Google Scholar] [CrossRef]
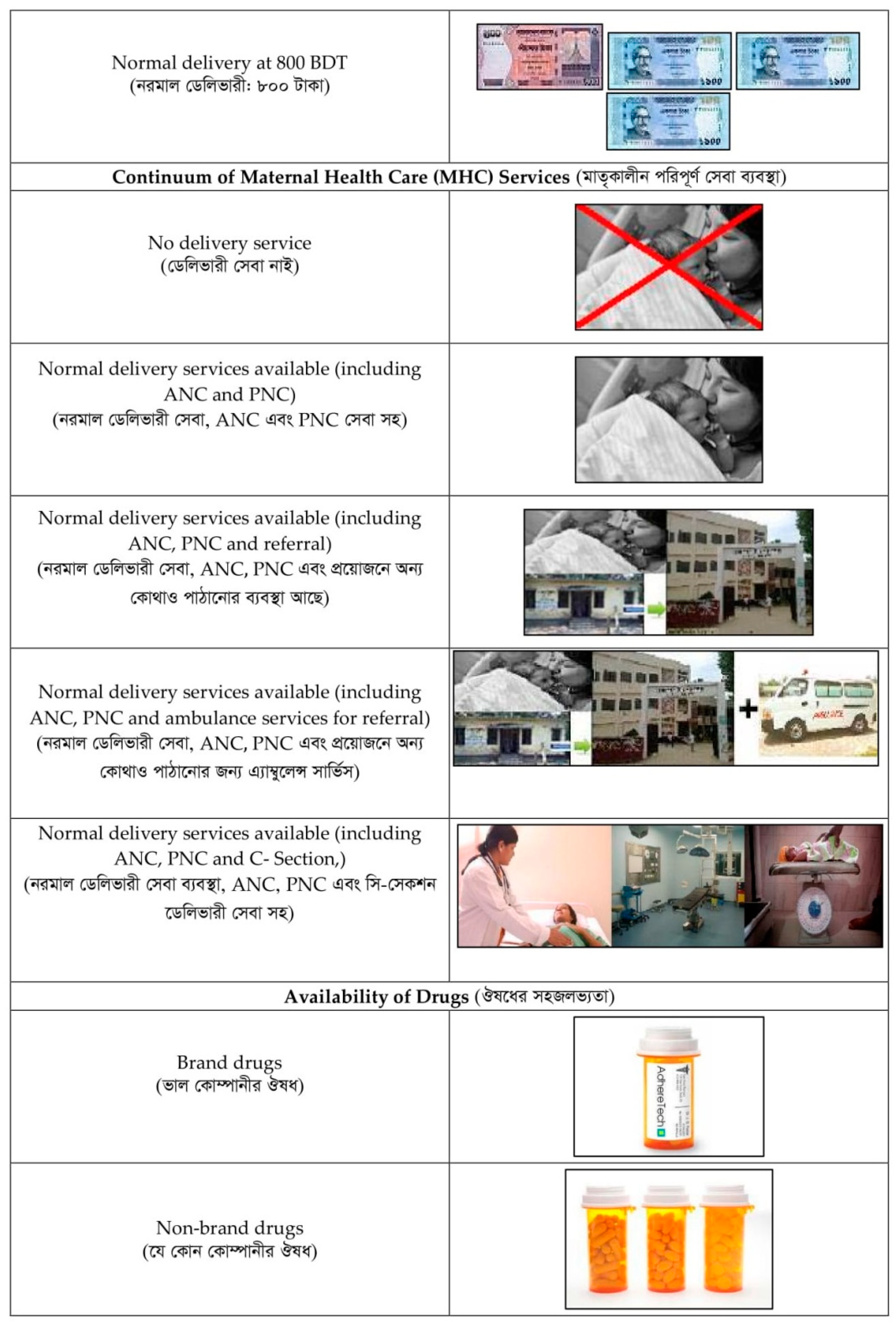
| Attributes | Attribute Levels |
|---|---|
| Availability of Provider | 1 = Paramedic |
| 2 = Nurse | |
| 3 = Female Doctor | |
| 4 = Male Doctor | |
| Provider Attitude | 1 = Polite |
| 2 = Rude | |
| Price | 1 = No fee |
| 2 = Normal delivery (≤600 BDT) | |
| 3 = Normal delivery (≤800 BDT) | |
| Continuum of Maternal Healthcare (MHC) Services | 1 = No delivery service |
| 2 = Normal delivery + (ANC and PNC) | |
| 3 = Normal delivery + (ANC, PNC and Referral) | |
| 4 = Normal delivery + (ANC, PNC and Ambulance services for referral) | |
| 5 = Normal delivery + (C-section, ANC, and PNC) | |
| Availability of Drug | 1 = Brand drugs |
| 2 = Non-brand drugs | |
| 3 = Uncertain or no drugs | |
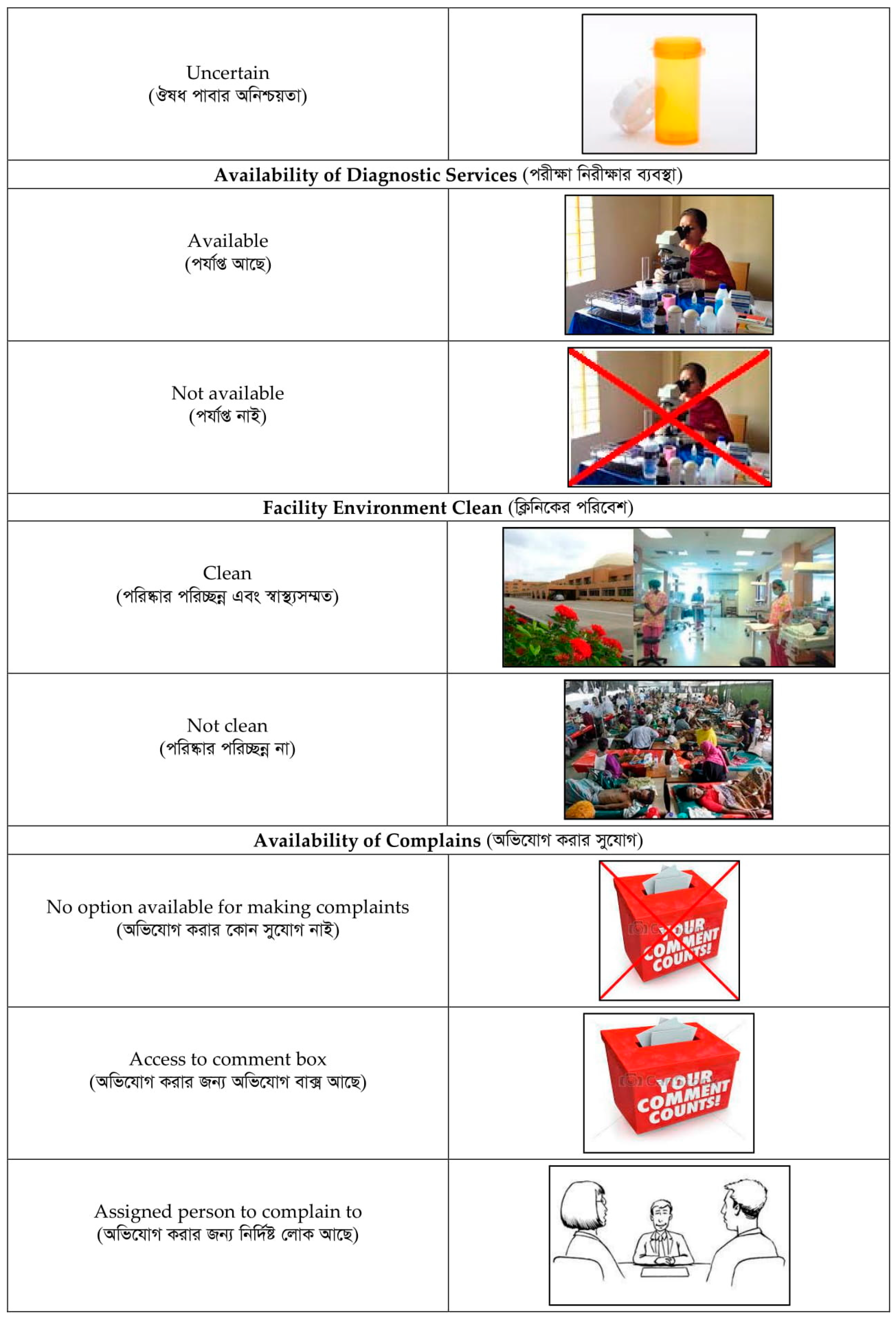
| Availability of Diagnostic Services | 1 = Yes |
| 2 = No | |
| Facility Environment Clean | 1 = Yes |
| 2 = No | |
| Availability for Complains | 1 = No option |
| 2 = Comment box | |
| 3 = Assigned person | |
| 4 = Phone line | |
| Waiting Times (in minutes) | 1 = <60 |
| 2 = 60–120 | |
| 3 = >1204 = None |
| Variables | Mean (SD)/n (%) |
|---|---|
| Average Age, Mean (SD) | 35.782 (10.969) |
| Age group in years | |
| 19–24 | 25 (4.160) |
| 25–35 | 369 (61.400) |
| 36–45 | 122 (20.300) |
| 46–64 | 65 (10.820) |
| ≥65 | 20 (3.330) |
| Education Background, n (%) | |
| No education | 143 (23.794) |
| Primary | 160 (26.622) |
| Secondary | 269 (44.759) |
| Higher secondary | 21 (3.494) |
| Tertiary | 8 (1.331) |
| Household Size, n (%) | |
| <4 | 184 (30.616) |
| 4–5 | 298 (49.584) |
| ≥6 | 119 (19.800) |
| Household Main Occupation, n (%) | |
| Farmer | 22 (3.661) |
| Day Laborer | 36 (5.990) |
| Service Holder | 162 (26.955) |
| Business Owner | 138 (22.962) |
| Rickshaw/Van/Boatman | 51 (8.486) |
| Woodworker/ Foreman | 48 (7.987) |
| Bus/Scooter Driver/Helper | 59 (9.817) |
| Small/Micro Business Owner | 50 (8.319) |
| Unemployed | 5 (0.832) |
| Others | 30 (4.992) |
| Community, n (%) | |
| Urban | 453 (75.374) |
| Rural | 148 (24.626) |
| Socio-Economic Status, n (%) | |
| Non-poor | 116 (19.301) |
| Poor | 341 (56.739) |
| Poorest | 144 (23.960) |
| Attributes | All Participants | Community | ||||
|---|---|---|---|---|---|---|
| Urban | Rural | |||||
| Mean ± SD | Coefficient (SE) | Mean ± SD | Coefficient (SE) | Mean ± SD | Coefficient (SE) | |
| Availability of Provider | ||||||
| Paramedic | −6.693 ± 38.127 | −0.067 (0.051) | −21.600 ± 35.867 | −0.155 (0.06) | 41.492 ± 48.796 | 0.277 (0.092) |
| Nurse | −22.370 ± 33.837 | −0.149 (0.051) | −29.111 ± 41.732 | −0.239 (0.059) | −26.407 ± 66.176 | −0.195 (0.097) |
| Female doctor | 29.639 ± 38.445 | 0.223 (0.048) | 29.601 ± 36.527 | 0.252 (0.055) | −0.643 ± 64.586 | −0.018 (0.096) |
| Male doctor | −0.576 ± 37.875 | −0.007 (0.049) | 21.112 ± 37.293 | 0.145 (0.056) | −14.441 ± 50.231 | −0.064 (0.088) |
| Provider Attitude | ||||||
| Polite | 47.702 ± 32.891 | 0.335 (0.027) | 45.267 ± 32.003 | 0.328 (0.031) | −2.042 ± 24.112 | −0.004 (0.051) |
| Rude | −47.702 ± 32.891 | −0.335 (0.027) | −45.267 ± 32.003 | −0.328 (0.031) | 2.042 ± 24.112 | 0.004 (0.051) |
| Price | ||||||
| Free service | −2.073 ± 36.813 | −0.055 (0.037) | −10.862 ± 32.133 | −0.061 (0.043) | 13.249 ± 33.301 | 0.081 (0.068) |
| Normal delivery (≤600 BDT) | 1.259 ± 31.256 | 0.036 (0.036) | −9.932 ± 33.033 | −0.06 (0.043) | −34.528 ± 28.508 | −0.147 (0.069) |
| Normal delivery (≤800 BDT) | 0.814 ± 37.527 | 0.018 (0.036) | 20.794 ± 33.334 | 0.122 (0.041) | 21.279 ± 29.856 | 0.066 (0.069) |
| Availability of Continuum of MHC Services | ||||||
| No delivery service | −92.464 ± 65.582 | −0.711 (0.065) | −85.145 ± 68.01 | −0.734 (0.075) | 30.196 ± 57.435 | 0.194 (0.105) |
| Normal delivery + (ANC and PNC) | −10.641 ± 42.318 | −0.059 (0.055) | −0.263 ± 42.37 | 0.006 (0.063) | −15.542 ± 48.11 | −0.087 (0.103) |
| Normal delivery + (ANC, PNC and Referral) | 17.748 ± 41.368 | 0.052 (0.054) | 27.069 ± 37.565 | 0.154 (0.063) | −17.832 ± 62.514 | −0.276 (0.108) |
| Normal delivery + (ANC, PNC and Ambulance) | 30.836 ± 33.955 | 0.268 (0.053) | 21.336 ± 40.964 | 0.234 (0.061) | −19.643 ± 67.414 | −0.064 (0.104) |
| Normal delivery + (C-section, ANC, PNC) | 54.521 ± 39.482 | 0.449 (0.060) | 37.004 ± 47.748 | 0.341 (0.068) | 22.819 ± 98.579 | 0.234 (0.114) |
| Availability of Drug | ||||||
| Brand drugs | 55.076 ± 39.352 | 0.461 (0.036) | 58.682 ± 35.787 | 0.512 (0.042) | 20.177 ± 28.421 | 0.164 (0.071) |
| Non-brand drugs | −33.784 ± 30.481 | −0.283 (0.038) | −33.142 ± 29.862 | −0.316 (0.044) | −6.821 ± 24.371 | 0.006 (0.072) |
| Uncertain | −21.292 ± 32.847 | −0.178 (0.037) | −25.539 ± 27.174 | −0.196 (0.043) | −13.377 ± 27.001 | −0.169 (0.074) |
| Availability of Diagnostic Services | ||||||
| Yes | 29.219 ± 24.754 | 0.253 (0.026) | 19.513 ± 22.648 | 0.196 (0.03) | −5.357 ± 23.929 | −0.005 (0.049) |
| No | −29.219 ± 24.754 | −0.253 (0.026) | −19.513 ± 22.648 | −0.196 (0.03) | 5.357 ± 23.929 | 0.005 (0.049) |
| Facility Environment Clean | ||||||
| Yes | 25.772 ± 30.966 | 0.281 (0.046) | 34.2 ± 33.837 | 0.288 (0.054) | −18.524 ± 23.582 | −0.064 (0.083) |
| No | −25.772 ± 30.966 | −0.281 (0.046) | −34.2 ± 33.837 | −0.288 (0.054) | 18.524 ± 23.582 | 0.064 (0.083) |
| Availability for Complains | ||||||
| No option | −18.755 ± 41.247 | −0.169 (0.081) | −31.904 ± 39.918 | −0.337 (0.096) | 28.528 ± 39.394 | 0.298 (0.157) |
| Comment box | 7.086 ± 38.808 | 0.039 (0.083) | 7.266 ± 53.211 | 0.023 (0.094) | 11.681 ± 64.888 | 0.283 (0.162) |
| Assigned person | 1.370 ± 34.466 | 0.008 (0.079) | 21.396 ± 54.669 | 0.251 (0.088) | −23.651 ± 45.518 | −0.413 (0.179) |
| Phone line | 10.299 ± 40.617 | 0.121 (0.078) | 3.243 ± 34.202 | 0.064 (0.091) | −16.558 ± 55.902 | −0.168 (0.155) |
| Waiting Times (in Minutes) | ||||||
| <60 | 5.185 ± 49.355 | 0.085 (0.063) | 12.719 ± 40.61 | 0.184 (0.072) | −51.183 ± 45.092 | −0.093 (0.116) |
| 60–120 | −6.805 ± 41.814 | −0.071 (0.064) | 3.064 ± 27.444 | −0.036 (0.075) | −5.798 ± 41.189 | −0.146 (0.115) |
| >120 | 1.620 ± 52.383 | −0.015 (0.064) | −15.782 ± 40.773 | −0.148 (0.075) | 56.981 ± 55.803 | 0.239 (0.114) |
| None | 8.898 ± 87.603 | −0.321 (0.055) | 5.264 ± 81.022 | −0.368 (0.065) | −9.787 ± 62.002 | −0.882 (0.129) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahumud, R.A.; Alamgir, N.I.; Hossain, M.T.; Baruwa, E.; Sultana, M.; Gow, J.; Alam, K.; Ahmed, S.M.; Khan, J.A.M. Women’s Preferences for Maternal Healthcare Services in Bangladesh: Evidence from a Discrete Choice Experiment. J. Clin. Med. 2019, 8, 132. https://doi.org/10.3390/jcm8020132
Mahumud RA, Alamgir NI, Hossain MT, Baruwa E, Sultana M, Gow J, Alam K, Ahmed SM, Khan JAM. Women’s Preferences for Maternal Healthcare Services in Bangladesh: Evidence from a Discrete Choice Experiment. Journal of Clinical Medicine. 2019; 8(2):132. https://doi.org/10.3390/jcm8020132
Chicago/Turabian StyleMahumud, Rashidul Alam, Nadia Ishrat Alamgir, Md. Tarek Hossain, Elaine Baruwa, Marufa Sultana, Jeff Gow, Khorshed Alam, Syed Masud Ahmed, and Jahangir A.M. Khan. 2019. "Women’s Preferences for Maternal Healthcare Services in Bangladesh: Evidence from a Discrete Choice Experiment" Journal of Clinical Medicine 8, no. 2: 132. https://doi.org/10.3390/jcm8020132
APA StyleMahumud, R. A., Alamgir, N. I., Hossain, M. T., Baruwa, E., Sultana, M., Gow, J., Alam, K., Ahmed, S. M., & Khan, J. A. M. (2019). Women’s Preferences for Maternal Healthcare Services in Bangladesh: Evidence from a Discrete Choice Experiment. Journal of Clinical Medicine, 8(2), 132. https://doi.org/10.3390/jcm8020132






