Prevalence, Risk Factors and Course of Osteoporosis in Patients with Crohn’s Disease at a Tertiary Referral Center
Abstract
1. Introduction
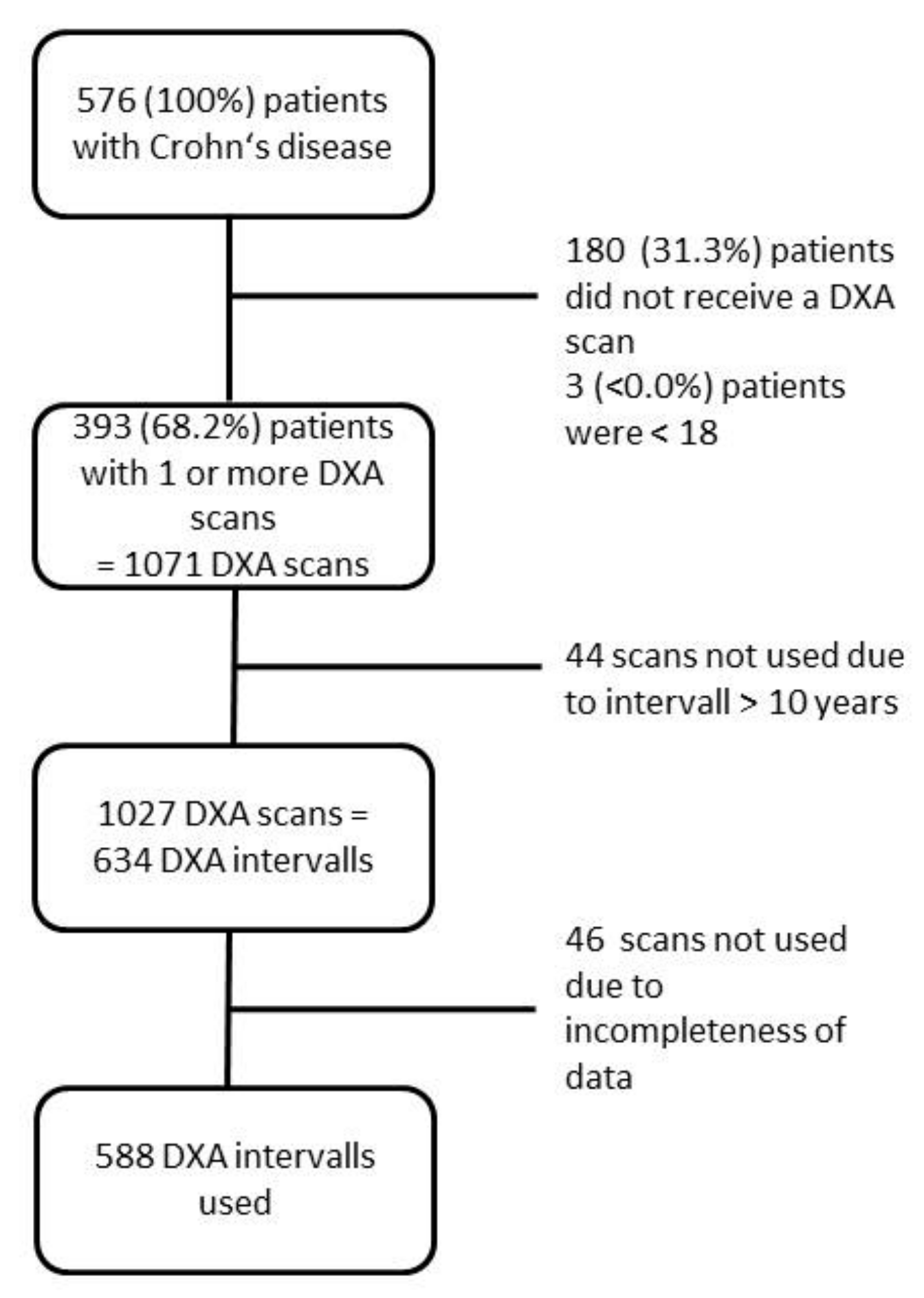
2. Materials and Methods
2.1. Study Design and Data Extraction
2.2. Definitions
2.3. Definitions of Variables
2.4. Dual X-Ray Energy Absorptiometry (DXA)
2.5. Study Endpoints
2.6. Statistical Analyses
3. Results
3.1. Patient Characteristics at First BMD Measurement
3.2. Prevalence of Osteopenia and Osteoporosis at First DXA Scan
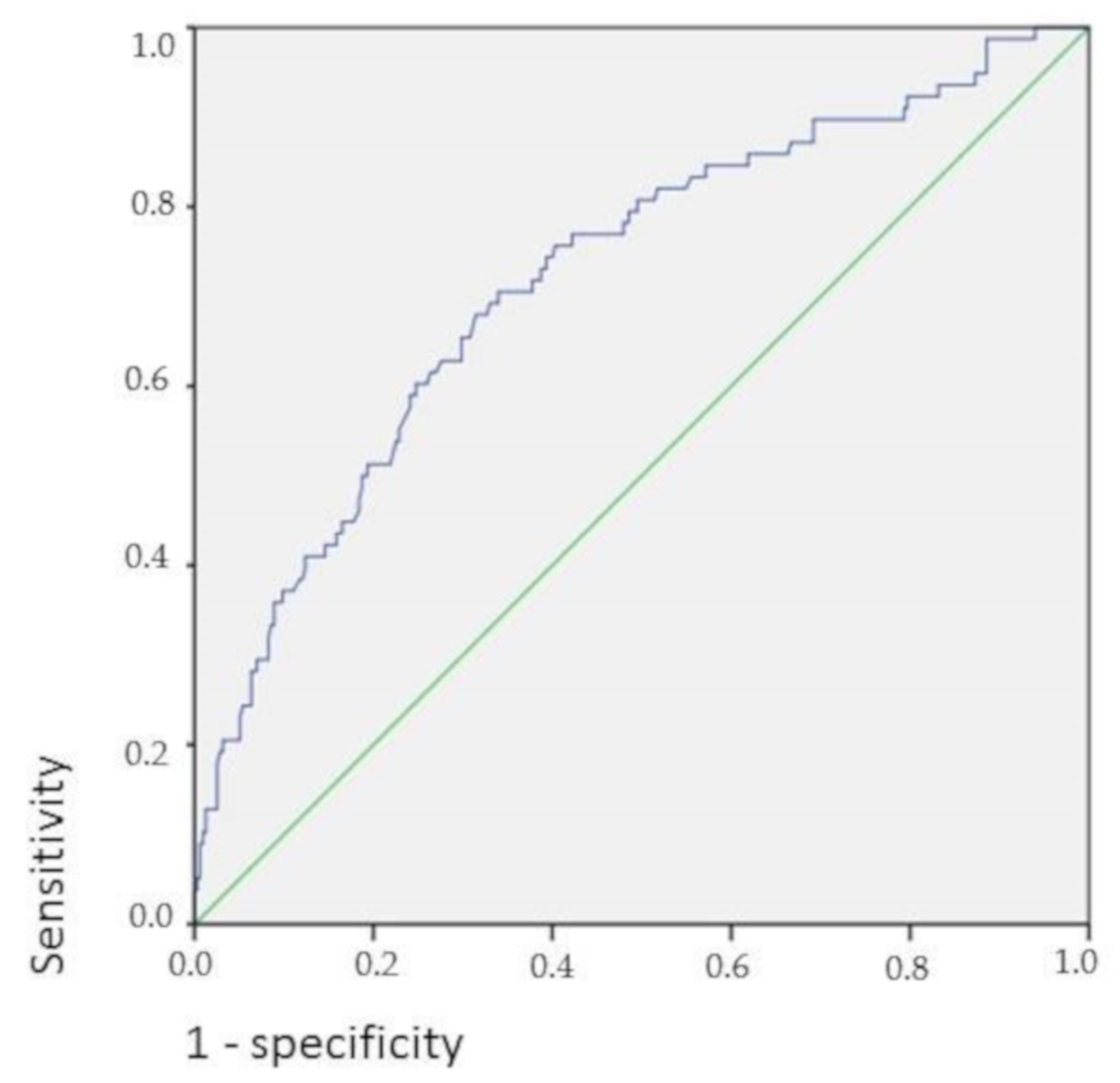
3.3. Evaluation of Risk Factors for Osteoporosis
3.4. Course of BMD over Time and Relation to CD Therapy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Larsen, S.; Bendtzen, K.; Nielsen, O.H. Extraintestinal manifestations of inflammatory bowel disease: Epidemiology, diagnosis, and management. Ann. Med. 2010, 42, 97–114. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.S.; Burakoff, R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol. Hepatol. 2011, 7, 235–241. [Google Scholar]
- Szafors, P.; Che, H.; Barnetche, T.; Morel, J.; Gaujoux-Viala, C.; Combe, B.; Lukas, C. Risk of fracture and low bone mineral density in adults with inflammatory bowel diseases. A systematic literature review with meta-analysis. Osteoporos. Int. 2018, 11, 2389–2397. [Google Scholar] [CrossRef] [PubMed]
- Compston, J.E.; Judd, D.; Crawley, E.O.; Evans, W.D.; Evans, C.; Church, H.A.; Reid, E.M.; Rhodes, J. Osteoporosis in patients with inflammatory bowel disease. Gut 1987, 28, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Pigot, F.; Roux, C.; Chaussade, S.; Hardelin, D.; Pelleter, O.; Montbrun, T.D.P.; Listrat, V.; Dougados, M.; Couturier, D.; Amor, B. Low bone mineral density in patients with inflammatory bowel disease. Dig. Dis. Sci. 1992, 37, 1396–1403. [Google Scholar] [CrossRef]
- Ali, T.; Lam, D.; Bronze, M.S.; Humphrey, M.B. Osteoporosis in inflammatory bowel disease. Am. J. Med. 2009, 122, 599–606. [Google Scholar] [CrossRef]
- Siffledeen, J.S.; Siminoski, K.; Jen, H.; Fedorak, R.N. Vertebral fractures and role of low bone mineral density in crohn’s disease. Clin. Gastroenterol. Hepatol. 2007, 5, 721–727. [Google Scholar] [CrossRef]
- Komaki, Y.; Komaki, F.; Micic, D.; Ido, A.; Sakuraba, A. Risk of Fractures in Inflammatory Bowel Diseases: A Systematic Review and Meta-Analysis. J. Clin. Gastroenterol. 2019, 53, 441–448. [Google Scholar] [CrossRef]
- Bjarnason, I.; Macpherson, A.; Mackintosh, C.; Buxton-Thomas, M.; Forgacs, I.; Moniz, C. Reduced bone density in patients with inflammatory bowel disease. Gut 1997, 40, 228–233. [Google Scholar] [CrossRef]
- Dear, K.L.; Compston, J.E.; Hunter, J.O. Treatment for Crohn’s disease that minimise steroid doses are associated with a reduced risk of osteoporosis. Clin. Nutr. 2001, 20, 541–546. [Google Scholar] [CrossRef]
- Silvennoinen, J.A.; Lehtola, J.K.; Niemela, S.E. Smoking is a risk factor for osteoporosis in women with inflammatory bowel disease. Scand. J. Gastroenterol. 1996, 31, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Dar, R.E.; Mazor, Y.; Karban, A.; Ish-Shalom, S.; Segal, E. Risk Factors for Low Bone Density in Inflammatory Bowel Disease: Use of Glucocorticoids, Low Body Mass Index, and Smoking. Dig. Dis. 2019, 37, 284–290. [Google Scholar]
- Schulte, C.; Goebell, H.; Roher, H.D.; Schulte, K.M. Genetic determinants of IL-6 expression levels do not influence bone loss in inflammatory bowel disease. Dig. Dis. Sci. 2001, 46, 2521–2528. [Google Scholar] [CrossRef] [PubMed]
- Kaneshiro, S.; Ebina, K.; Shi, K.; Higuchi, C.; Hirao, M.; Okamoto, M.; Koizumi, K.; Morimoto, T.; Yoshikawa, H.; Hashimoto, J. IL-6 negatively regulates osteoblast differentiation through the SHP2/MEK2 and SHP2/Akt2 pathways in vitro. J. Bone Miner. Metab. 2014, 32, 378–392. [Google Scholar] [CrossRef]
- Kim, H.J. New understanding of glucocorticoid action in bone cells. BMB Rep. 2010, 43, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Gowen, S.; Hannan, W.J.; Ferguson, A. Low bone mineral density in crohn’s disease, but not in ulcerative colitis at diagnosis. Gastroenterology 1994, 107, 1031–1039. [Google Scholar] [CrossRef]
- Leslie, W.D.; Miller, N.; Rogala, L.; Bernstein, C.N. Vitamin D status and bone density in recently diagnosed inflammatory bowel disease: The Manitoba IBD Cohort Study. Am. J. Gastroenterol. 2008, 103, 1451–1459. [Google Scholar] [CrossRef]
- Abraham, B.P.; Prasad, P.; Malaty, H.M. Vitamin D deficiency and corticosteroid use are risk factors for low bone mineral density in inflammatory bowel disease patients. Dig. Dis. Sci. 2014, 59, 1878–1884. [Google Scholar] [CrossRef]
- Krajcovicova, A.; Hlavaty, T.; Killinger, Z.; Miznerova, E.; Toth, J.; Letkovsky, J.; Nevidanska, M.; Cierny, D.; Koller, T.; Zelinkova, Z.; et al. Combination therapy with an immunomodulator and anti-TNFα agent improves bone mineral density in IBD patients. J. Crohns. Colitis. 2014, 8, 1693–1701. [Google Scholar] [CrossRef]
- Marshall, D.; Johnell, O.; Wedel, H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 1996, 312, 1254–1259. [Google Scholar] [CrossRef]
- Cummings, S.R.; Browner, W.; Black, D.M.; Nevitt, M.C.; Genant, H.K.; Cauley, J.; Ensrud, K.; Palermo, L.; Scott, J.; Vogt, T.M. Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet 1993, 341, 72–75. [Google Scholar] [CrossRef]
- Melek, J.; Sakuraba, A. Efficacy and safety of medical therapy for low bone mineral density in patients with inflammatory bowel disease: A metaanalysis and systematic review. Clin. Gastroenterol. Hepatol. 2014, 12, 32–44. [Google Scholar] [CrossRef] [PubMed]
- Cosman, F.; de Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R. Clinician’s guide to prevention, treatment of osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381. [Google Scholar] [CrossRef] [PubMed]
- Cranney, A.; Wells, G.; Willan, A.; Griffith, L.; Zytaruk, N.; Robinson, V.; Black, D.; Adachi, J.; Shea, B.; Tugwell, P.; et al. Meta-analyses of therapies for postmenopausal osteoporosis. II. Meta-analysis of alendronate for the treatment of postmenopausal women. Endocr. Rev. 2002, 23, 508–516. [Google Scholar] [CrossRef]
- Gomollón, F.; Dignass, A.; Annese, V.; Tilg, H.; Van Assche, G.; Lindsay, J.O.; Peyrin-Biroulet, L.; Cullen, G.J.; Daperno, M.; Kucharzik, T.; et al. ECCO guideline/consensus paper 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 1: Diagnosis and Medical Management. J. Crohn’s Colitis. 2017, 11, 3–25. [Google Scholar] [CrossRef]
- Stasangi, J.; Siverberg, M.S.; Vermeire, S.; Colombel, J.F. The Montreal classification of inflammatory bowel disease: Controversies, consensus, and implications. Gut 2006, 55, 749–753. [Google Scholar] [CrossRef]
- Kanis, J.A. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: Synopsis of a WHO report. Osteoporos. Int. 1994, 4, 368–381. [Google Scholar] [CrossRef]
- Krela-Kaźmierczak, I.; Michalak, M.; Szymczak-Tomczak, A.; Łykowska-Szuber, L.; Stawczyk-Eder, K.; Waszak, K.; Kucharski, M.A.; Dobrowolska, A.; Eder, P. Prevalence of osteoporosis and osteopenia in a population of patients with inflammatory bowel diseases from the Wielkopolska Region. Pol. Arch. Intern. Med. 2018, 128, 447–454. [Google Scholar] [CrossRef]
- Zali, M.; Bahari, A.; Firouzi, F.; Daryani, N.E.; Aghazadeh, R.; Emam, M.M.; Rezaie, A.; Shalmani, H.M.; Naderi, N.; Maleki, B.; et al. Bone mineral density in Iranian patients with inflammatory bowel disease. Int. J. Colorectal. Dis. 2006, 21, 758–766. [Google Scholar] [CrossRef]
- Wade, S.W.; Strader, C.; Fitzpatrick, L.A.; Anthony, M.S.; O’Malley, C.D. Estimating prevalence of osteoporosis: Examples from industrialized countries. Arch. Osteoporos. 2014, 9, 182. [Google Scholar] [CrossRef]
- Strozyk, D.; Gress, T.M.; Breitling, L.P. Smoking and bone mineral density: Comprehensive analyses of the third National Health and Nutrition Examination Survey (NHANES III). Arch. Osteoporos. 2018, 13, 16. [Google Scholar] [CrossRef] [PubMed]
- Van Staa, T.P.; Leufkens, H.G.; Cooper, C. The epidemiology of corticosteroid-induced osteoporosis: A meta-analysis. Osteoporos. Int. 2002, 10, 777–787. [Google Scholar] [CrossRef] [PubMed]
- Miranda-Bautista, J.; Verdejo, C.; Díaz-Redondo, A.; Bretón, I.; Bellón, J.M.; Pérez-Valderas, M.D.; Caballero-Marcos, A.; de Dios-Lascuevas, M.; González-Río, E.; García-Sánchez, C.; et al. Metabolic bone disease in patients diagnosed with inflammatory bowel disease from Spain. Therap. Adv. Gastroenterol. 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Burt, L.A.; Billington, E.O.; Rose, M.S.; Raymond, D.A.; Hanley, D.A.; Boyd, S.K. Effect of High-Dose Vitamin D Supplementation on Volumetric Bone Density and Bone Strength: A Randomized Clinical Trial. JAMA. 2019, 322, 736–745. [Google Scholar] [CrossRef]
| Variable | n = 393 |
|---|---|
| Male, n (%) | 175 (44.5) |
| Age at diagnosis of IBD (years), median (range) | 23 (8–68) |
| Age at first DXA scan (years), median (range) | 36 (18–77) |
| Montreal classification of CD: | |
| Age, n (A1:A2:A3), n = 391 | 45:302:44 |
| Location, n (L1:L2:L3:L4), n = 392 | 116:57:219:38 |
| Behavior, n (B1:B2:B3), n = 392 | 132:91:168 |
| Disease duration at first DXA scan (years), median (range) | 8 (0–61) |
| Presence of at least one extraintestinal manifestation, n (%) | 211 (53.7) |
| Active cigarette smoking at first DXA scan, n = 224 (%) | 146 (37.2) |
| BMI (kg/m²), mean ± SD (range) | 24.2 ± 5.1 (14.6–45.7) |
| History of anti-TNFα treatment, n (%) | 91 (23.2) |
| History of anti-integrin treatment, n (%) | 3 (0.8) |
| History of anti-interleukin treatment, n (%) | 0 (0) |
| History of immunomodulator treatment, n (%) | 143 (36.4) |
| History of bowel resection(s), n (%) | 268 (68.2) |
| Short bowel syndrome, n (%) | 7 (1.8) |
| Ostomy, n (%) | 26 (6.6) |
| BMD, mean ± SD (range) | 0.919 ± 0.136 (0.478–1.362) |
| BMD lumbar spine, mean ± SD (range) | 0.963 ± 0.146 (0.524–1.453) |
| BMD femur, mean ± SD (range) | 0.874 ± 0.153 (0.432–1.430) |
| BMD according to T-score of WHO | |
| Normal BMD:osteopenia:osteoporosis (n:n:n) | 157:158:78 |
| Number of DXA scans per patient | |
| 1, n (%) | 160 (40.7) |
| 2, n (%) | 73 (18.6) |
| 3, n (%) | 54 (13.7) |
| 4, n (%) | 39 (9.9) |
| 5, n (%) | 27 (6.9) |
| 6, n (%) | 11 (2.8) |
| 7, n (%) | 8 (2.0) |
| 8, n (%) | 9 (2.3) |
| 9, n (%) | 6 (1.5) |
| 10, n (%) | 2 (0.5) |
| 11, n (%) | 3 (0.8) |
| 12, n (%) | 1 (0.3) |
| Osteoporosis | No Osteoporosis | p-Value | |
|---|---|---|---|
| Variable | n = 78 | n = 315 | |
| Male, n (%) | 43 (55.1) | 132 (41.9) | 0.035 1 |
| Age at diagnosis of CD (years), median (range) | 23 (8–66) | 23 (9–68) | 0.413 2 |
| Age at first DXA scan (years), median (range) | 44 (18–77) | 34 (18–75) | 0.009 2 |
| Montreal classification of CD: | |||
| Age | 0.028 1 | ||
| A1 | 10 (13.0) | 35 (11.1) | |
| A2 | 52 (67.5) | 250 (79.6) | |
| A3 | 15 (19.5) | 29 (9.2) | |
| Location | 0.462 1 | ||
| L1 | 24 (31.2) | 92 (29.2) | |
| L2 | 7 (9.1) | 50 (15.9) | |
| L3 | 46 (59.7) | 172 (54.6) | |
| L4 | 5 (6.5) | 33 (10.5) | 0.290 1 |
| Behavior | 0.816 1 | ||
| B1 | 25 (32.1) | 107 (43.2) | |
| B2 | 17 (21.8) | 74 (23.6) | |
| B3 | 36 (46.2) | 132 (42.2) | |
| Disease duration at first DXA scan (years), median (range) | 10.5 (0–61) | 8 (0–40) | 0.028 2 |
| Presence of at least one extraintestinal manifestation, n (%) | 42 (53.8) | 169 (53.7) | 0.975 1 |
| Active cigarette smoking at first DXA scan, n (%) | 28 (36.8) | 118 (38.9) | 0.736 1 |
| BMI (kg/m²), mean ± SD (range) | 21.3 ± 4.2 (14.6–33.3) | 24.9 ± 5.0 (15.2–45.7) | <0.001 2 |
| History of anti-TNFα treatment, n (%) | 15 (19.2) | 76 (24.1) | 0.359 1 |
| History of anti-integrin treatment, n (%) | 2 (2.6) | 1 (0.3) | 0.042 1 |
| History of immunomodulator treatment, n (%) | 28 (35.9) | 115 (36.5) | 0.920 1 |
| History of bowel resection(s), n (%) | 66 (84.6) | 202 (64.1) | 0.001 1 |
| Short bowel syndrome, n (%) | 5 (6.4) | 2 (0.6) | 0.001 1 |
| Ostomy, n (%) | 8 (10.3) | 18 (5.7) | 0.148 1 |
| Parameter | Odds Ratio (OR) | 95% CI | p-Value |
|---|---|---|---|
| Male sex | 2.511 | (1.377; 4.576) | 0.003 |
| Age at first DXA scan (years) | 1.053 | (1.026; 1.081) | <0.001 |
| Disease duration at first DXA scan (years) | 0.985 | (0.953; 1.018) | 0.372 |
| BMI (in kg/m²) | 0.761 | (0.697; 0.831) | <0.001 |
| History of anti-integrin treatment | 2.800 | (0.164; 47.729) | 0.477 |
| History of bowel resection(s) | 3.253 | (1.514; 6.989) | 0.003 |
| Short bowel syndrome | 2.783 | (0.371; 20.887) | 0.320 |
| Variable | Estimate | 95% CI | p-Value |
|---|---|---|---|
| Male sex | 0.025 | (0.014; 0.036) | <0.001 |
| Age at diagnose of CD (in years) | −0.003 | (−0.005; −0.001) | 0.001 |
| Age at DXA scan (in years) | 0.002 | (<0.001; 0.004) | 0.023 |
| Montreal classification of CD: | |||
| L1 | 0 | ||
| L2 | 0.006 | (−0.012; 0.024) | 0.529 |
| L3 | −0.001 | (−0.013; 0.011) | 0.833 |
| B1 | 0 | ||
| B2 | −0.012 | (−0.027; 0.004) | 0.132 |
| B3 | −0.011 | (−0.027; 0.003) | 0.122 |
| Disease duration to first DXA scan | −0.003 | (−0.005; −0.001) | 0.018 |
| First bone density | −0.180 | (−0.119; −0.232) | <0.001 |
| Presence of at least one extraintestinal manifestation | 0.013 | (0.002; 0.024) | 0.002 |
| BMI | 0.002 | (<0.001; 0.003) | 0.011 |
| History of anti-TNFα treatment | −0.012 | (−0.026; 0.003) | 0.118 |
| History of immunomodulator treatment | −0.016 | (−0.028; −0.003) | 0.012 |
| History of bowel resections | 0.013 | (0.000; 0.028) | 0.050 |
| Steroid treatment during interval | −0.011 | (−0.021; −0.001) | 0.028 |
| Smoking during interval | −0.007 | (−0.021; 0.006) | 0.244 |
| Calcium during interval | 0.006 | (−0.008; 0.019) | 0.401 |
| Vitamin D during interval | −0.009 | (−0.023; 0.005) | 0.219 |
| Bisphosphonates during interval | −0.011 | (−0.026; 0.002) | 0.094 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoffmann, P.; Krisam, J.; Kasperk, C.; Gauss, A. Prevalence, Risk Factors and Course of Osteoporosis in Patients with Crohn’s Disease at a Tertiary Referral Center. J. Clin. Med. 2019, 8, 2178. https://doi.org/10.3390/jcm8122178
Hoffmann P, Krisam J, Kasperk C, Gauss A. Prevalence, Risk Factors and Course of Osteoporosis in Patients with Crohn’s Disease at a Tertiary Referral Center. Journal of Clinical Medicine. 2019; 8(12):2178. https://doi.org/10.3390/jcm8122178
Chicago/Turabian StyleHoffmann, Peter, Johannes Krisam, Christian Kasperk, and Annika Gauss. 2019. "Prevalence, Risk Factors and Course of Osteoporosis in Patients with Crohn’s Disease at a Tertiary Referral Center" Journal of Clinical Medicine 8, no. 12: 2178. https://doi.org/10.3390/jcm8122178
APA StyleHoffmann, P., Krisam, J., Kasperk, C., & Gauss, A. (2019). Prevalence, Risk Factors and Course of Osteoporosis in Patients with Crohn’s Disease at a Tertiary Referral Center. Journal of Clinical Medicine, 8(12), 2178. https://doi.org/10.3390/jcm8122178





