Risk of Venous Thromboembolic Events in Patients with Osteonecrosis of the Femoral Head Undergoing Primary Hip Arthroplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source from Taiwan National Health Insurance Research Database (NHIRD)
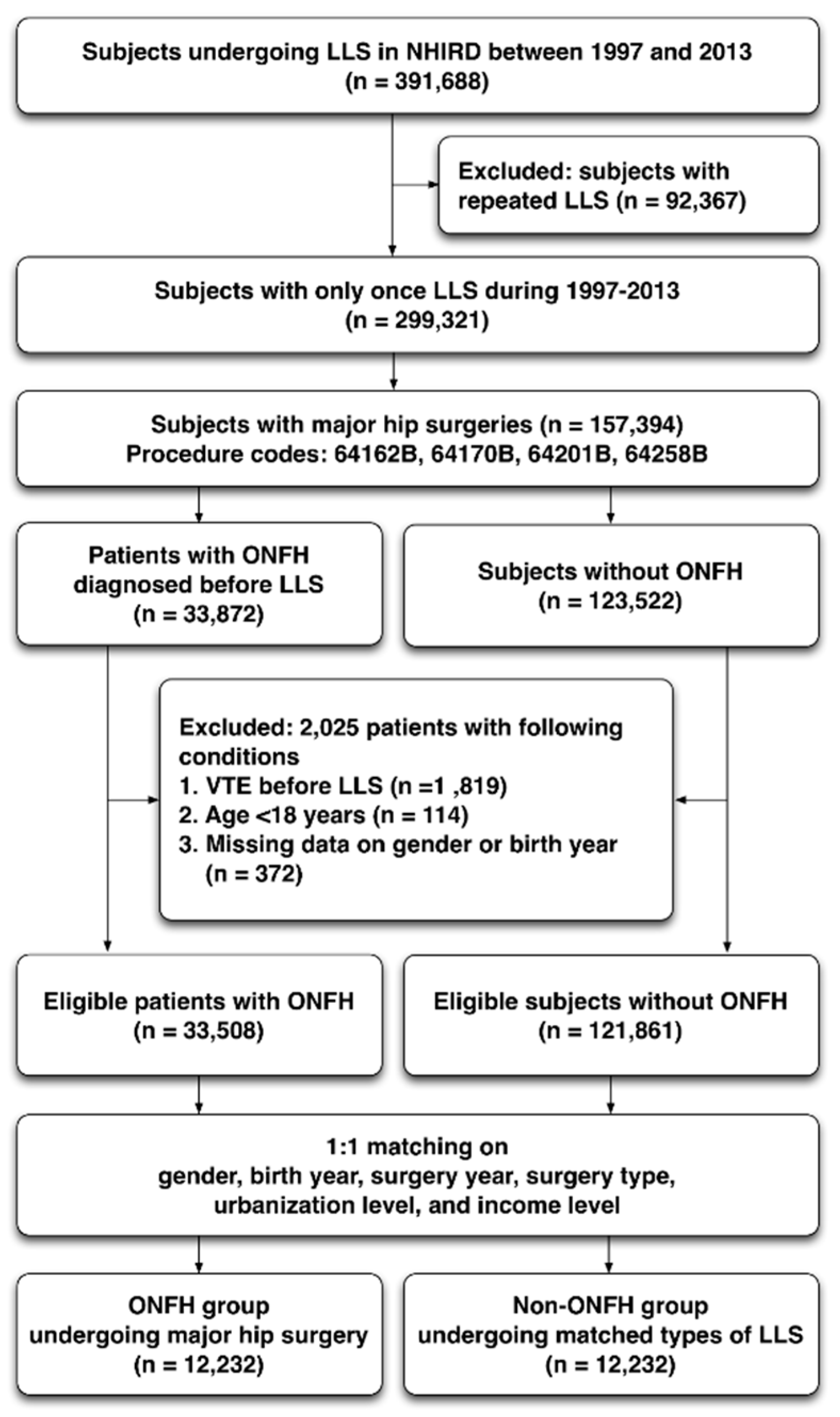
2.2. Study Population
2.3. Diagnosis Confirmation and Acquisition of Medical and Surgical Information
2.4. Comorbidities and Outcomes
2.5. Statistical Analysis
3. Results
3.1. Demographic Data of the Surgical Patients with and without ONFH
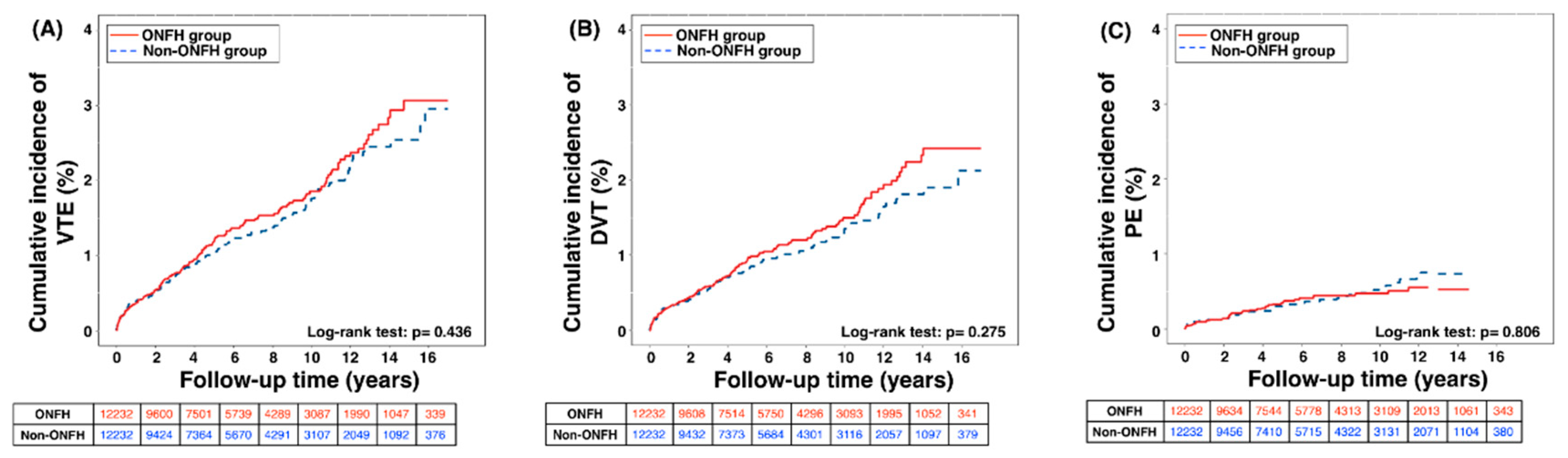
3.2. Outcome Comparison for Incidence Rate and Adjusted Risk of VTE, DVT, and PE
3.3. Multivariate Analysis for Identifying the Risk Factors for Post-Operative VTE, DVT and PE
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ONFH | osteonecrosis of femoral head |
| VTE | venous thromboembolic events |
| LLS | lower limb surgery |
| NHIRD | national health insurance research database |
| PHR | partial hip replacement |
| THR | total hip replacement |
| NSAID | non-steroidal anti-inflammatory drug |
| DVT | deep venous thrombosis |
| PE | pulmonary embolism |
| CI | confidence interval |
| HR | hazard ratio |
| MACCE | major adverse cardiovascular or cerebrovascular events |
References
- Mont, M.A.; Hungerford, D.S. Non-traumatic avascular necrosis of the femoral head. J. Bone Joint Surg. Am. 1995, 77, 459–474. [Google Scholar] [CrossRef] [PubMed]
- Lafforgue, P. Pathophysiology and natural history of avascular necrosis of bone. Joint Bone Spine 2006, 73, 500–507. [Google Scholar] [CrossRef] [PubMed]
- DiGiovanni, C.W.; Patel, A.; Calfee, R.; Nickisch, F. Osteonecrosis in the foot. J. Am. Acad. Orthop. Surg. 2007, 15, 208–217. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lieberman, J.R.; Conduah, A.; Urist, M.R. Treatment of osteonecrosis of the femoral head with core decompression and human bone morphogenetic protein. Clin. Orthop. Relat. Res. 2004, 429, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.G.; Cui, Q.; Kuskowski, M.; Mihalko, W.M.; Saleh, K.J. Outcomes of total and unicompartmental knee arthroplasty for secondary and spontaneous osteonecrosis of the knee. J. Bone Joint Surg. Am. 2006, 88, 76–82. [Google Scholar]
- Woo, S.B.; Hellstein, J.W.; Kalmar, J.R. Narrative [corrected] review: Bisphosphonates and osteonecrosis of the jaws. Ann. Intern. Med. 2006, 144, 753–761. [Google Scholar] [CrossRef]
- Chao, Y.C.; Wang, S.J.; Chu, H.C.; Chang, W.K.; Hsieh, T.Y. Investigation of alcohol metabolizing enzyme genes in Chinese alcoholics with avascular necrosis of hip joint, pancreatitis and cirrhosis of the liver. Alcohol. Alcohol. 2003, 38, 431–436. [Google Scholar] [CrossRef]
- Juery, P. Avascular necrosis after a steroid injection. CMAJ 2007, 176, 814. [Google Scholar] [CrossRef][Green Version]
- Urbaniak, J.R.; Harvey, E.J. Revascularization of the femoral head in osteonecrosis. J. Am. Acad. Orthop. Surg. 1998, 6, 44–54. [Google Scholar] [CrossRef]
- Mankin, H.J. Nontraumatic necrosis of bone (osteonecrosis). N. Engl. J. Med. 1992, 326, 1473–1479. [Google Scholar]
- Chang, C.C.; Greenspan, A.; Gershwin, M.E. Osteonecrosis: Current perspectives on pathogenesis and treatment. Semin. Arthritis Rheum. 1993, 23, 47–69. [Google Scholar] [CrossRef]
- Chim, S.M.; Tickner, J.; Chow, S.T.; Kuek, V.; Guo, B.; Zhang, G.; Rosen, V.; Erber, W.; Xu, J. Angiogenic factors in bone local environment. Cytokine Growth Factor Rev. 2013, 24, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Kerachian, M.A.; Harvey, E.J.; Cournoyer, D.; Chow, T.Y.; Seguin, C. Avascular necrosis of the femoral head: Vascular hypotheses. Endothelium 2006, 13, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Sung, P.H.; Yang, Y.H.; Chiang, H.J.; Chiang, J.Y.; Chen, C.J.; Yip, H.K.; Lee, M.S. Cardiovascular and Cerebrovascular Events Are Associated With Nontraumatic Osteonecrosis of the Femoral Head. Clin. Orthop. Relat. Res. 2018, 476, 865–874. [Google Scholar] [CrossRef]
- Seguin, C.; Kassis, J.; Busque, L.; Bestawros, A.; Theodoropoulos, J.; Alonso, M.L.; Harvey, E.J. Non-traumatic necrosis of bone (osteonecrosis) is associated with endothelial cell activation but not thrombophilia. Rheumatology 2008, 47, 1151–1155. [Google Scholar] [CrossRef]
- Tabrizchi, R. Corticosteroids and endothelial dysfunction. Vasc. Health Risk Manag. 2005, 1, 261–262. [Google Scholar] [CrossRef]
- Wolberg, A.S.; Rosendaal, F.R.; Weitz, J.I.; Jaffer, I.H.; Agnelli, G.; Baglin, T.; Mackman, N. Venous thrombosis. Nat. Rev. Dis. Primers 2015, 1, 15006. [Google Scholar] [CrossRef]
- Niikura, T.; Sakai, Y.; Lee, S.Y.; Iwakura, T.; Kuroda, R.; Kurosaka, M. Rate of venous thromboembolism after complex lower-limb fracture surgery without pharmacological prophylaxis. J. Orthop. Surg. 2015, 23, 37–40. [Google Scholar] [CrossRef]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef]
- Sung, P.H.; Chiang, H.J.; Yang, Y.H.; Chiang, J.Y.; Chen, C.J.; Yip, H.K.; Lee, M.S. Nationwide study on the risk of unprovoked venous thromboembolism in non-traumatic osteonecrosis of femoral head. Int. Orthop. 2018, 42, 1469–1478. [Google Scholar] [CrossRef]
- Cheng, T.-M. Taiwan’s National Health Insurance system: High value for the dollar. In Six Countries, Six Reform Models: The Health Reform Experience of Israel, The Netherlands, New Zealand, Singapore, Switzerland and Taiwan; Okma, K.G.H., Crivelli, L., Eds.; World Scientific Publishing Company: Singapore, 2009; pp. 71–204. [Google Scholar]
- Wilbur, J.; Shian, B. Deep Venous Thrombosis and Pulmonary Embolism: Current Therapy. Am. Fam. Phys. 2017, 95, 295–302. [Google Scholar]
- Lowe, G.D. Virchow’s triad revisited: Abnormal flow. Pathophysiol. Haemost. Thromb. 2003, 33, 455–457. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Khavanin, N.; Rambachan, A.; McCarthy, R.J.; Mlodinow, A.S.; De Oliveria, G.S., Jr.; Stock, M.C.; Gust, M.J.; Mahvi, D.M. Surgical duration and risk of venous thromboembolism. JAMA Surg. 2015, 150, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, K.; Kawasaki, T.; Nakamura, N.; Yoshikawa, H.; Sugano, N. Natural course of asymptomatic deep venous thrombosis in hip surgery without pharmacologic thromboprophylaxis in an Asian population. Clin. Orthop. Relat. Res. 2010, 468, 2430–2436. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, H.; Yokoyama, Y.; Iida, Y.; Terashima, F.; Hasegawa, K.; Saito, T.; Suguro, T.; Wada, A. Incidence of venous thromboembolism after spine surgery. J. Orthop. Sci. 2012, 17, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.A.; Lucas, R.; Vojnovic, I.; Hasan, K.; Pepper, J.R.; Warner, T.D. Stronger inhibition by nonsteroid anti-inflammatory drugs of cyclooxygenase-1 in endothelial cells than platelets offers an explanation for increased risk of thrombotic events. FASEB J. 2006, 20, 2468–2475. [Google Scholar] [CrossRef]
- Fosslien, E. Cardiovascular complications of non-steroidal anti-inflammatory drugs. Ann. Clin. Lab. Sci. 2005, 35, 347–385. [Google Scholar]
- Walker, C.; Biasucci, L.M. Cardiovascular safety of non-steroidal anti-inflammatory drugs revisited. Postgrad. Med. 2018, 130, 55–71. [Google Scholar] [CrossRef]
- Gunter, B.R.; Butler, K.A.; Wallace, R.L.; Smith, S.M.; Harirforoosh, S. Non-steroidal anti-inflammatory drug-induced cardiovascular adverse events: A meta-analysis. J. Clin. Pharm. Ther. 2017, 42, 27–38. [Google Scholar] [CrossRef]
- Lee, L.H.; Gallus, A.; Jindal, R.; Wang, C.; Wu, C.C. Incidence of Venous Thromboembolism in Asian Populations: A Systematic Review. Thromb. Haemost. 2017, 117, 2243–2260. [Google Scholar] [CrossRef]
| ONFH Group (n = 12232) | Non-ONFH * Group (n = 12232) | ||||
|---|---|---|---|---|---|
| Variables | No. | % | No. | % | p-Value |
| Gender | 1.000 | ||||
| Female | 5654 | 46.2 | 5654 | 46.2 | |
| Male | 6578 | 53.8 | 6578 | 53.8 | |
| Age (years) | 1.000 | ||||
| 18–65 | 6533 | 53.4 | 6533 | 53.4 | |
| >65 | 5699 | 46.6 | 5699 | 46.6 | |
| Median age (IQR) | 61.9 (53–72) | 61.9 (53–72) | |||
| Urbanization level | 1.000 | ||||
| 1 (rural) | 1212 | 9.9 | 1212 | 9.9 | |
| 2 | 2441 | 20.0 | 2441 | 20.0 | |
| 3 | 5990 | 49.0 | 5990 | 49.0 | |
| 4 (urban) | 2589 | 21.2 | 2589 | 21.2 | |
| Income level | 1.000 | ||||
| 1 (lowest) | 3319 | 27.1 | 3319 | 27.1 | |
| 2 | 2075 | 17.0 | 2075 | 17.0 | |
| 3 | 4896 | 40.0 | 4896 | 40.0 | |
| 4 (highest) | 1942 | 15.9 | 1942 | 15.9 | |
| Surgical procedure | 1.000 | ||||
| THR | 8516 | 69.6 | 8516 | 69.6 | |
| PHR | 3596 | 29.4 | 3596 | 29.4 | |
| Revision of hip replacement | 120 | 1.0 | 120 | 1.0 | |
| Comorbidities | |||||
| Hypertension | 7694 | 62.9 | 7836 | 64.1 | 0.059 |
| Diabetes mellitus | 3592 | 29.4 | 3902 | 31.9 | <0.001 |
| Dyslipidemia | 4597 | 37.6 | 4350 | 35.6 | 0.001 |
| Gout | 3138 | 25.7 | 2658 | 21.7 | <0.001 |
| Systemic lupus erythematosus | 214 | 1.7 | 61 | 0.5 | <0.001 |
| Atrial fibrillation | 649 | 5.3 | 622 | 5.1 | 0.437 |
| Coronary heart disease | 3836 | 31.4 | 3734 | 30.5 | 0.158 |
| Peripheral vascular disease | 1010 | 8.3 | 1048 | 8.6 | 0.381 |
| Chronic kidney disease | 1217 | 9.9 | 1248 | 10.2 | 0.510 |
| Obesity | 116 | 0.9 | 156 | 1.3 | 0.015 |
| Drug exposure (>1 month) | |||||
| NSAID | 10,242 | 83.7 | 9623 | 78.7 | <0.001 |
| Steroid | 4099 | 32.8 | 3255 | 26.6 | <0.001 |
| Outcomes | |||||
| VTE | 167 | 1.4 | 152 | 1.2 | 0.398 |
| DVT | 133 | 1.1 | 115 | 0.9 | 0.251 |
| PE | 44 | 0.4 | 46 | 0.4 | 0.833 |
| ONFH (n = 12232) | Non-ONFH (n = 12232) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Event | PY | Rate * | Event | PY | Rate | IRR | 95% CI | p-Value |
| VTE | 167 | 78,820.55 | 21.19 | 152 | 78,224.69 | 19.43 | 1.09 | 0.88–1.36 | 0.440 |
| DVT | 133 | 78,940.20 | 16.85 | 115 | 78,356.04 | 14.68 | 1.15 | 0.89–1.47 | 0.279 |
| PE | 44 | 79,253.03 | 5.55 | 46 | 78,669.39 | 5.85 | 0.95 | 0.63–1.44 | 0.806 |
| Gender | |||||||||
| Female | 101 | 34,524.82 | 29.25 | 62 | 34,457.93 | 17.99 | 1.63 | 1.19–2.23 | 0.003 |
| Male | 66 | 44,295.73 | 14.90 | 90 | 43,766.76 | 20.56 | 0.72 | 0.53–1.00 | 0.047 |
| Age | |||||||||
| 18–65 years | 58 | 42,933.20 | 13.51 | 64 | 42,372.27 | 15.10 | 0.89 | 0.63–1.28 | 0.538 |
| >65 years | 109 | 35,887.35 | 30.37 | 88 | 35,852.42 | 24.55 | 1.24 | 0.93–1.64 | 0.137 |
| Hypertension | |||||||||
| No | 43 | 28,179.04 | 15.26 | 48 | 27,305.24 | 17.58 | 0.87 | 0.58–1.31 | 0.500 |
| Yes | 124 | 50,641.50 | 24.49 | 104 | 50,919.45 | 20.42 | 1.20 | 0.92–1.56 | 0.173 |
| Diabetes mellitus | |||||||||
| No | 105 | 54,228.76 | 19.36 | 104 | 51,999.40 | 20.00 | 0.97 | 0.74–1.27 | 0.815 |
| Yes | 62 | 24,591.79 | 25.21 | 48 | 26,225.29 | 18.30 | 1.38 | 0.95–2.01 | 0.096 |
| Dyslipidemia | |||||||||
| No | 93 | 49,459.34 | 18.80 | 103 | 51,513.41 | 19.99 | 0.94 | 0.71–1.24 | 0.668 |
| Yes | 74 | 29,361.21 | 25.20 | 49 | 26,711.28 | 18.34 | 1.37 | 0.96–1.97 | 0.085 |
| Gout | |||||||||
| No | 118 | 57,675.98 | 20.46 | 115 | 60,791.02 | 18.92 | 1.08 | 0.84–1.40 | 0.550 |
| Yes | 49 | 21,144.57 | 23.17 | 37 | 17,433.67 | 21.22 | 1.09 | 0.71–1.67 | 0.686 |
| Systemic lupus erythematosus | |||||||||
| No | 163 | 77,577.48 | 21.01 | 150 | 77,867.36 | 19.26 | 1.09 | 0.87–1.36 | 0.443 |
| Yes | 4 | 1243.06 | 32.18 | 2 | 357.33 | 55.97 | 0.57 | 0.11–3.14 | 0.523 |
| Atrial fibrillation | |||||||||
| No | 154 | 74,240.54 | 20.74 | 139 | 73,796.08 | 18.84 | 1.10 | 0.88–1.39 | 0.410 |
| Yes | 13 | 4580.01 | 28.38 | 13 | 4428.61 | 29.35 | 0.97 | 0.45–2.09 | 0.932 |
| Chronic ischemic heart disease | |||||||||
| No | 85 | 52,647.86 | 16.15 | 96 | 53,130.35 | 18.07 | 0.89 | 0.67–1.20 | 0.450 |
| Yes | 82 | 26,172.68 | 31.33 | 56 | 25,094.34 | 22.32 | 1.40 | 1.00–1.97 | 0.050 |
| Peripheral vascular disease | |||||||||
| No | 140 | 71,858.15 | 19.48 | 132 | 71,302.58 | 18.51 | 1.05 | 0.83–1.33 | 0.674 |
| Yes | 27 | 6962.40 | 38.78 | 20 | 6922.11 | 28.89 | 1.34 | 0.75–2.39 | 0.319 |
| Chronic kidney disease | |||||||||
| No | 146 | 70,479.76 | 20.72 | 133 | 70,274.14 | 18.93 | 1.09 | 0.87–1.38 | 0.451 |
| Yes | 21 | 8340.79 | 25.18 | 19 | 7950.55 | 23.90 | 1.05 | 0.57–1.96 | 0.869 |
| Obesity | |||||||||
| No | 166 | 78,215.13 | 21.22 | 150 | 77,406.90 | 19.38 | 1.10 | 0.88–1.37 | 0.419 |
| Yes | 1 | 605.42 | 16.52 | 2 | 817.79 | 24.46 | 0.68 | 0.06–7.45 | 0.749 |
| Exposure to NSAID | |||||||||
| <1 month | 30 | 6941.74 | 43.22 | 39 | 10,403.76 | 37.49 | 1.15 | 0.72–1.86 | 0.558 |
| 1–6 months | 47 | 24,723.47 | 19.01 | 50 | 25,783.44 | 19.39 | 0.98 | 0.66–1.46 | 0.922 |
| >6 months | 90 | 47,155.33 | 19.09 | 63 | 42,037.49 | 14.99 | 1.27 | 0.92–1.76 | 0.141 |
| Exposure to steroid | |||||||||
| <1 month | 99 | 46,136.23 | 21.46 | 105 | 51,630.36 | 20.34 | 1.06 | 0.80–1.39 | 0.702 |
| 1–6 months | 45 | 21,297.60 | 21.13 | 32 | 18,851.76 | 16.97 | 1.24 | 0.79–1.96 | 0.344 |
| >6 months | 23 | 11,386.72 | 20.20 | 15 | 7742.57 | 19.37 | 1.04 | 0.54–2.00 | 0.900 |
| Follow-up period after surgery | |||||||||
| <30 days | 9 | 999.91 | 90.01 | 12 | 1000.38 | 119.95 | 0.75 | 0.32–1.78 | 0.515 |
| 31–365 days | 34 | 10,464.17 | 32.49 | 34 | 10,380.73 | 32.75 | 0.99 | 0.62–1.60 | 0.974 |
| 1–3 years | 38 | 19,209.97 | 19.78 | 31 | 18,864.33 | 16.43 | 1.20 | 0.75–1.93 | 0.444 |
| 3–5 years | 32 | 15,023.24 | 21.30 | 22 | 14,751.51 | 14.91 | 1.43 | 0.83–2.46 | 0.198 |
| >5 years | 54 | 33,123.25 | 16.30 | 53 | 33,227.75 | 15.95 | 1.02 | 0.70–1.49 | 0.910 |
| VTE | DVT | PE | |||||||
|---|---|---|---|---|---|---|---|---|---|
| aHR | 95% CI | p-Value | aHR | 95% CI | p-Value | aHR | 95% CI | p-Value | |
| ONFH | 1.14 | 0.91–1.42 | 0.262 | 1.22 | 0.94–1.56 | 0.130 | 0.95 | 0.62–1.44 | 0.802 |
| Gender (ref.: female) | |||||||||
| Male | 0.84 | 0.66–1.07 | 0.152 | 0.92 | 0.69–1.21 | 0.530 | 0.68 | 0.43–1.09 | 0.106 |
| Age (ref.: 18–65 years) | |||||||||
| >65 years | 1.62 | 1.24–2.11 | <0.001 | 1.55 | 1.15–2.10 | 0.004 | 1.72 | 1.04–2.84 | 0.035 |
| Comorbidities | |||||||||
| Hypertension | 1.09 | 0.82–1.45 | 0.540 | 1.11 | 0.81–1.53 | 0.507 | 1.01 | 0.59–1.73 | 0.978 |
| Diabetes mellitus | 0.97 | 0.76–1.24 | 0.796 | 1.06 | 0.80–1.41 | 0.678 | 0.73 | 0.45–1.17 | 0.185 |
| Dyslipidemia | 1.05 | 0.81–1.35 | 0.732 | 0.94 | 0.70–1.25 | 0.649 | 1.58 | 0.99–2.51 | 0.053 |
| Gout | 1.23 | 0.94–1.60 | 0.133 | 1.26 | 0.93–1.70 | 0.130 | 1.05 | 0.63–1.75 | 0.861 |
| Systemic lupus erythematosus | 2.00 | 0.87–4.58 | 0.104 | 1.83 | 0.67–5.05 | 0.242 | 1.99 | 0.47–8.48 | 0.354 |
| Atrial fibrillation | 1.12 | 0.74–1.70 | 0.580 | 1.08 | 0.67–1.75 | 0.748 | 1.34 | 0.66-2.73 | 0.419 |
| Chronic ischemic heart disease | 1.36 | 1.05–1.74 | 0.018 | 1.23 | 0.92–1.65 | 0.155 | 1.71 | 1.07–2.73 | 0.025 |
| Peripheral vascular disease | 1.57 | 1.14–2.17 | 0.006 | 1.96 | 1.39–2.78 | <.001 | 0.90 | 0.44–1.82 | 0.763 |
| Chronic kidney disease | 0.96 | 0.68–1.35 | 0.810 | 1.04 | 0.71–1.52 | 0.859 | 0.65 | 0.31–1.37 | 0.254 |
| Obesity | 1.06 | 0.34–3.32 | 0.924 | 0.46 | 0.06–3.29 | 0.439 | 2.36 | 0.57–9.76 | 0.236 |
| Drug exposure | |||||||||
| NSAID (ref.: <1 month) | |||||||||
| 1–6 months | 0.48 | 0.35–0.66 | <0.001 | 0.50 | 0.35–0.71 | <0.001 | 0.51 | 0.28–0.92 | 0.027 |
| >6 months | 0.37 | 0.27–0.51 | <0.001 | 0.37 | 0.26–0.53 | <0.001 | 0.34 | 0.18–0.63 | 0.001 |
| Steroid (ref.: <1 month) | |||||||||
| 1–6 months | 1.05 | 0.80–1.39 | 0.719 | 0.97 | 0.70–1.34 | 0.859 | 1.38 | 0.82–2.32 | 0.231 |
| >6 months | 1.03 | 0.71–1.49 | 0.886 | 0.86 | 0.56–1.35 | 0.520 | 1.83 | 0.97–3.43 | 0.062 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sung, P.-H.; Yang, Y.-H.; Chiang, H.-J.; Chiang, J.Y.; Yip, H.-K.; Lee, M.S. Risk of Venous Thromboembolic Events in Patients with Osteonecrosis of the Femoral Head Undergoing Primary Hip Arthroplasty. J. Clin. Med. 2019, 8, 2158. https://doi.org/10.3390/jcm8122158
Sung P-H, Yang Y-H, Chiang H-J, Chiang JY, Yip H-K, Lee MS. Risk of Venous Thromboembolic Events in Patients with Osteonecrosis of the Femoral Head Undergoing Primary Hip Arthroplasty. Journal of Clinical Medicine. 2019; 8(12):2158. https://doi.org/10.3390/jcm8122158
Chicago/Turabian StyleSung, Pei-Hsun, Yao-Hsu Yang, Hsin-Ju Chiang, John Y. Chiang, Hon-Kan Yip, and Mel S. Lee. 2019. "Risk of Venous Thromboembolic Events in Patients with Osteonecrosis of the Femoral Head Undergoing Primary Hip Arthroplasty" Journal of Clinical Medicine 8, no. 12: 2158. https://doi.org/10.3390/jcm8122158
APA StyleSung, P.-H., Yang, Y.-H., Chiang, H.-J., Chiang, J. Y., Yip, H.-K., & Lee, M. S. (2019). Risk of Venous Thromboembolic Events in Patients with Osteonecrosis of the Femoral Head Undergoing Primary Hip Arthroplasty. Journal of Clinical Medicine, 8(12), 2158. https://doi.org/10.3390/jcm8122158





