The Trends in Opioid Use in Castile and Leon, Spain: A Population-Based Registry Analysis of Dispensations in 2015 to 2018
Abstract
1. Introduction
2. Experimental Section
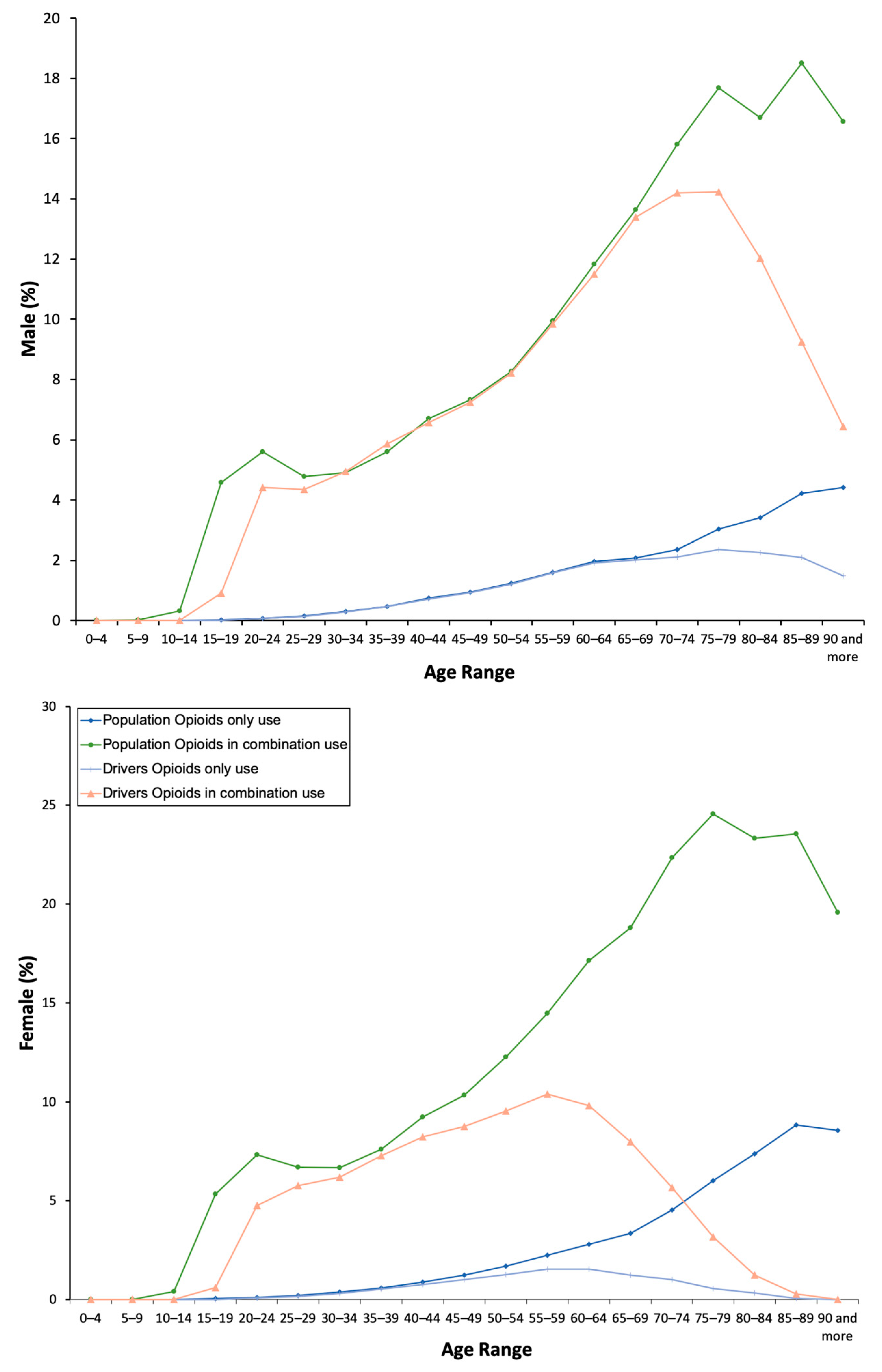
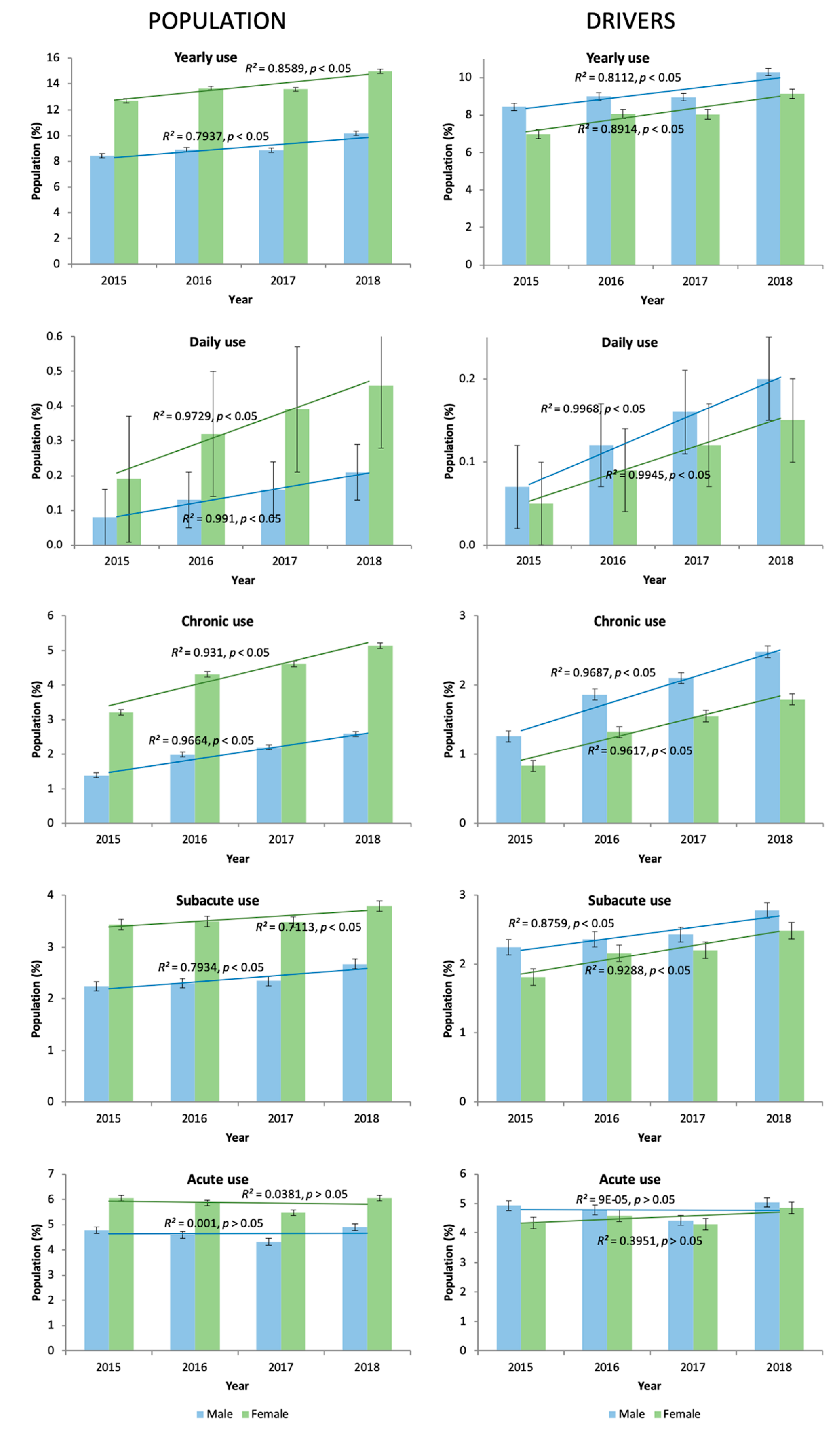
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cicero, T.J.; Ellis, M.S. Understanding the demand side of the prescription opioid epidemic: Does the initial source of opioids matter? Drug. Alcohol. Depend. 2017, 173 (Suppl. 1), S4–S10. [Google Scholar] [CrossRef]
- Rosner, B.; Neicun, J.; Yang, J.C.; Roman-Urrestarazu, A. Opioid prescription patterns in Germany and the global opioid epidemic: Systematic review of available evidence. PLoS ONE 2019, 14, e0221153. [Google Scholar] [CrossRef] [PubMed]
- Van Amsterdam, J.; van den Brink, W. The Misuse of Prescription Opioids: A Threat for Europe? Curr. Drug Abuse Rev. 2015, 8, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Gomes, T.; Tadrous, M.; Mamdani, M.M.; Paterson, J.M.; Juurlink, D.N. The Burden of Opioid-Related Mortality in the United States. JAMA Netw. Open 2018, 1, e180217. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.M.; Wollersheim, D. Who Are Dispensed the Bulk Amount of Prescription Opioids? J. Clin. Med. 2019, 8, 293. [Google Scholar] [CrossRef]
- Compton, W.M.; Jones, C.M. Epidemiology of the U.S. opioid crisis: The importance of the vector. Ann. N. Y. Acad. Sci. 2019, 1451, 130–143. [Google Scholar] [CrossRef]
- Li, G.; Chihuri, S. Prescription opioids, alcohol and fatal motor vehicle crashes: A population-based case-control study. Inj. Epidemiol. 2019, 6, 11. [Google Scholar] [CrossRef]
- Herrera-Gómez, F.; García-Mingo, M.; Colás, M.; González-Luque, J.C.; Álvarez, F.J. Opioids in oral fluid of Spanish drivers. Drug. Alcohol Depend. 2018, 187, 35–39. [Google Scholar] [CrossRef]
- Chihuri, S.; Li, G. Use of prescription opioids and motor vehicle crashes: A meta analysis. Accid. Anal. Prev. 2017, 109, 123–131. [Google Scholar] [CrossRef]
- Cheatle, M.D.; Barker, C. Improving opioid prescription practices and reducing patient risk in the primary care setting. J. Pain. Res. 2014, 7, 301–311. [Google Scholar] [CrossRef]
- Chihuri, S.; Li, G. Use of Prescription Opioids and Initiation of Fatal 2-Vehicle Crashes. JAMA Netw. Open. 2019, 2, e188081. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, M.B.; Jongen, S.; Knoche, A.; Petzke, F.; Vuurman, E.F.; Vollrath, M.; Ramaekers, J.G. Effect of chronic opioid therapy on actual driving performance in non-cancer pain patients. Psychopharmacology 2017, 234, 989–999. [Google Scholar] [CrossRef] [PubMed]
- Fierro, I.; Colás, M.; González-Luque, J.C.; Álvarez, F.J. Roadside opioid testing of drivers using oral fluid: The case of a country with a zero tolerance law, Spain. Subst. Abuse Treat. Prev. Policy 2017, 12, 22. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Abejón, E.; Herrera-Gómez, F.; Criado-Espegel, P.; Alvarez, F.J. Use of driving-impairing medicines by a Spanish population: A population-based registry study. BMJ Open 2017, 7, e017618. [Google Scholar] [CrossRef]
- Herrera-Gómez, F.; Gutierrez-Abejón, E.; Criado-Espegel, P.; Álvarez, F.J. The Problem of Benzodiazepine Use and Its Extent in the Driver Population: A Population-Based Registry Study. Front. Pharmacol. 2018, 9, 408. [Google Scholar] [CrossRef]
- Herrera-Gómez, F.; Gutierrez-Abejón, E.; Álvarez, F.J. Antipsychotics in the general population and the driver population: Comparisons from a population-based registry study. Int. Clin. Psychopharmacol. 2019, 34, 184–188. [Google Scholar] [CrossRef]
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M.; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef]
- Brady, K.T.; McCauley, J.L.; Back, S.E. Prescription Opioid Misuse, Abuse, and Treatment in the United States: An Update. Am. J. Psychiatry 2016, 173, 18–26. [Google Scholar] [CrossRef]
- Herrera-Gómez, F.; García-Mingo, M.; Colás, M.; González-Luque, J.C.; Alvarez, F.J. Drivers who tested positive for cannabis in oral fluid: A longitudinal analysis of administrative data for Spain between 2011 and 2016. BMJ Open 2019, 9, e026648. [Google Scholar] [CrossRef]
- Minsterio De Sanidad Servicios Sociales e lgualdad. Utilización de medicamentos opioides en España durante el periodo 2008-2015; Agencia Española de Medicamentos y Productos Sanitarios INFORME DE UTILIZACIÓN DE MEDICAMENTOS U/OPI/V1/13022017: Madrid, Spain, 21 February 2017.
- Jacob, L.; Kostev, K. Prevalence of pain medication prescriptions in France, Germany, and the UK—A cross-sectional study including 4,270,142 patients. Postgrad. Med. 2018, 130, 32–36. [Google Scholar] [CrossRef]
- Schubert, I.; Ihle, P.; Sabatowski, R. Increase in Opiate Prescription in Germany between 2000 and 2010. Dtsch. Ärztebl. Int. 2013, 110, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Werber, A.; Marschall, U.; L’hoest, H.; Hauser, W.; Moradi, B.; Schiltenwolf, M. Opioid therapy in the treatment of chronic pain conditions in Germany. Pain. Physician 2015, 18, E323–E331. [Google Scholar] [PubMed]
- Cragg, A.; Hau, J.P.; Woo, S.A.; Kitchen, S.A.; Liu, C.; Doyle-Waters, M.M.; Hohl, C.M. Risk Factors for Misuse of Prescribed Opioids: A Systematic Review and Meta-Analysis. Ann. Emerg. Med. 2019, 74, 634–646. [Google Scholar] [CrossRef] [PubMed]
- Sherman, R.E.; Anderson, S.A.; dal Pan, G.J.; Gray, G.W.; Gross, T.; Hunter, N.L.; LaVange, L.; Marinac-Dabic, D.; Marks, P.W.; Robb, M.A.; et al. Real-World Evidence—What Is It and What Can It Tell Us? N. Engl. J. Med. 2016, 375, 2293–2297. [Google Scholar] [CrossRef]

| Population Using Opioids % (95 CI) | Drivers Using Opioids % (95 CI) | |||||
|---|---|---|---|---|---|---|
| Total | Opioids only | Opioids in Association | Total | Opioids only | Opioids in Association | |
| Total | 11.44 (11.32–11.56) | 1.78 (1.66–1.91) | 10.29 (10.17–10.41) | 8.72 (8.57–8.88) | 1.04 (0.88–1.2) | 8.3 (8.14–8.45) |
| Male | 9.07 (8.9–9.24) | 1.19 (1.01–1.37) | 8.27 (8.1–8.45) | 9.17 (8.97–9.37) | 1.17 (0.96–1.38) | 8.59 (8.39–8.8) |
| Female | 13.73 (13.56–13.89) | 2.35 (2.18–2.53) | 12.24 (12.07–12.41) | 8.06 (7.81–8.3) | 0.84 (0.59–1.1) | 7.85 (7.6–8.1) |
| χ2, p | 3144.861, p = 0.001 | 1570.787, p = 0.001 | 2003.986, p = 0.001 | 16,871.0, p = 0.001 | 1979.537, p = 0.001 | 15,501.654, p = 0.001 |
| Type of use | ||||||
| Chronic | ||||||
| Total | 3.2 (3.13–3.26) | 1.03 (0.93–1.12) | 2.69 (2.62–2.75) | 1.7 (1.63–1.77) | 0.51 (0.4–0.63) | 2.15 (2.07–2.23) |
| Male | 2.04 (1.95–2.12) | 0.63 (0.5–0.76) | 2.14 (2.05–2.23) | 1.92 (1.83–2.02) | 0.6 (0.45–0.74) | 2.03 (1.93–2.14) |
| Female | 4.32 (4.22–4.42) | 1.41 (1.27–1.55) | 3.21 (3.12–3.3) | 1.37 (1.27–1.48) | 0.39 (0.22–0.56) | 2.07 (1.94–2.2) |
| χ2, p | 1985.911, p = 0.001 | 1170.328, p = 0.001 | 1085.825, p = 0.001 | 4601.091, p = 0.001 | 1108.628, p = 0.001 | 3676.290, p = 0.001 |
| Subacute | ||||||
| Total | 2.98 (2.91–3.04) | 0.58 (0.5–0.65) | 2.31 (2.25–2.37) | 2.34 (2.26–2.42) | 0.4 (0.3–0.5) | 1.33 (1.27–1.4) |
| Male | 2.39 (2.3–2.48) | 0.43 (0.32–0.54) | 1.48 (1.41–1.56) | 2.46 (2.35–2.56) | 0.44 (0.31–0.57) | 1.17 (1.09–1.24) |
| Female | 3.55 (3.46–3.63) | 0.72 (0.62–0.82) | 3.11 (3.02–3.2) | 2.16 (2.03–2.29) | 0.34 (0.18–0.5) | 1.22 (1.12–1.32) |
| χ2, p | 328.39, p = 0.001 | 293.255, p = 0.001 | 239.633, p = 0.001 | 4662.045, p = 0.001 | 614.929, p = 0.001 | 4406.436, p = 0.001 |
| Acute | ||||||
| Total | 5.26 (5.18–5.35) | 0.18 (0.14–0.22) | 5.3 (5.21–5.38) | 4.68 (4.57–4.8) | 0.13 (0.07–0.19) | 4.67 (4.55–4.79) |
| Male | 4.65 (4.52–4.77) | 0.13 (0.07–0.19) | 4.65 (4.52–4.78) | 4.79 (4.65–4.94) | 0.14 (0.07–0.21) | 4.62 (4.47–4.77) |
| Female | 5.86 (5.75–5.98) | 0.22 (0.17–0.28) | 5.92 (5.8–6.04) | 4.52 (4.33–4.71) | 0.12 (0.02–0.21) | 4.61 (4.41–4.8) |
| χ2, p | 214.78. p = 0.001 | 76.966. p = 0.001 | 239.790. p = 0.001 | 7414.013. p = 0.001 | 258.198. p = 0.001 | 7365.078. p = 0.001 |
| Daily use | ||||||
| Total | 0.24 (0.12–0.37) | 0.13 (0.01–0.27) | 0.11 (0.01–0.21) | 0.13 (0.04–0.25) | 0.07 (0.02–0.13) | 0.08 (0.01–0.13) |
| Male | 0.14 (0.01–0.30) | 0.08 (0.01–0.17) | 0.07 (0.01–0.13) | 0.14 (0.07–0.28) | 0.08 (0.03–0.14) | 0.07 (0.01–0.15) |
| Female | 0.34 (0.16–0.52) | 0.18 (0.01–0.36) | 0.16 (0.06–0.26) | 0.1 (0.05–0.19) | 0.05 (0.01–0.11) | 0.05 (0.01–0.09) |
| χ2, p | 317.198, p = 0.001 | 255.709, p = 0.001 | 266.803, p = 0.001 | 357.012, p = 0.001 | 160.226, p = 0.001 | 506.183, p = 0.00 |
| Average of driving-impairing medicines; population opioid use | ||||||
| Total | 2.54 (2.53–2.54) | 3.16 (3.14–3.18) | 2.49 (2.49–2.50) | 2.34 (2.33–2.36) | 3.04 (3.01–3.07) | 2.31 (2.30–2.33) |
| Male | 2.28 (2.26–2.29) | 2.87 (2.83–2.9) | 2.24 (2.23–2.26) | 2.26 (2.24–2.27) | 2.86 (2.82–2.9) | 2.22 (2.20–2.23) |
| Female | 2.66 (2.65–2.67) | 3.29 (3.27–3.32) | 2.63 (2.61–2.64) | 2.49 (2.47–2.51) | 3.36 (3.3–3.42) | 2.45 (2.43–2.47) |
| t, p | −30.520, p = 0.001 | −19.564, p = 0.001 | −41.237, p = 0.001 | −14.153, p = 0.001 | −14.425, p = 0.001 | −16.290, p = 0.001 |
| Average of driving-impairing medicines; population daily opioid use | ||||||
| Total | 3.52 (3.46–3.58) | 3.77 (3.7–3.83) | 3.23 (3.17–3.29) | 3.67 (3.55–3.79) | 3.93 (3.8–4.06) | 3.31 (3.21–3.42) |
| Male | 3.29 (3.16–3.41) | 3.57 (3.44–3.69) | 2.91 (2.8–3.02) | 3.40 (3.25–3.54) | 3.7 (3.55–3.85) | 2.99 (2.87–3.12) |
| Female | 3.60 (3.53–3.67) | 3.86 (3.78–3.94) | 3.35 (3.29–3.42) | 4.18 (3.96–4.2) | 4.41 (4.17–4.65) | 3.82 (3.63–4.01) |
| t, p | −3.561, p = 0.012 | −3.657, p = 0.001 | −6.321, p = 0.001 | −5.580, p = 0.001 | −4.769, p = 0.001 | −7.094, p = 0.001 |
| Population Using Opioids % (95 CI) | Drivers Using Opioids % (95 CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2015 | 2016 | 2017 | 2018 | |
| Total | 10.59 (10.47–10.71) | 11.31 (11.19–11.43) | 11.25 (11.13–11.37) | 12.6 (12.48–12.72) | 7.86 (7.71–8.02) | 8.63 (8.47–8.78) | 8.59 (8.43–8.74) | 9.82 (9.67–9.97) |
| Male | 8.41 (8.23–8.58) | 8.87 (8.7–9.05) | 8.84 (8.67–9.02) | 10.16 (9.99–10.33) | 8.44 (8.24–8.64) | 9 (8.8–9.2) | 8.95 (8.75–9.15) | 10.29 (10.09–10.49) |
| Female | 12.7 (12.54–12.87) | 13.66 (13.49–13.83) | 13.57 (13.4–13.74) | 14.97 (14.8–15.13) | 6.99 (6.74–7.23) | 8.07 (7.83–8.32) | 8.04 (7.79–8.28) | 9.13 (8.88–9.37) |
| χ2, p | 3022.886, p = 0.001 | 2623.495, p = 0.001 | 2850.157, p = 0.001 | 3144.861, p = 0.001 | 15,215.257, p = 0.001 | 15,624.29, p = 0.001 | 15,862.716, p = 0.001 | 16,871, p = 0.001 |
| Type of use | ||||||||
| Chronic | ||||||||
| Total | 2.32 (2.26–2.38) | 3.16 (3.1–3.23) | 3.42 (3.35–3.49) | 3.88 (3.81–3.96) | 1.09 (1.03–1.15) | 1.64 (1.57–1.71) | 1.87 (1.8–1.95) | 2.2 (2.12–2.27) |
| Male | 1.39 (1.32–1.46) | 1.98 (1.89–2.06) | 2.19 (2.1–2.28) | 2.59 (2.5–2.69) | 1.26 (1.18–1.34) | 1.86 (1.76–1.95) | 2.1 (2–2.2) | 2.48 (2.37–2.58) |
| Female | 3.21 (3.13–3.3) | 4.31 (4.21–4.41) | 4.61 (4.51–4.71) | 5.13 (5.03–5.24) | 0.83 (0.75–0.92) | 1.32 (1.22–1.43) | 1.55 (1.44–1.66) | 1.79 (1.68–1.9) |
| χ2, p | 1558.149, p = 0.001 | 1617.673, p = 0.001 | 1907.393, p = 0.001 | 1985.911, p = 0.001 | 2548.811, p = 0.001 | 3635.145, p = 0.001 | 3924.455, p = 0.001 | 4601.091, p = 0.001 |
| Subacute | ||||||||
| Total | 2.84 (2.78––2.91) | 2.91 (2.84–2.97) | 2.92 (2.86–2.98) | 3.24 (3.17–3.31) | 2.07 (1.99–2.16) | 2.28 (2.2––2.36) | 2.34 (2.25–2.42) | 2.66 (2.58–2.74) |
| Male | 2.24 (2.15–2.33) | 2.3 (2.21–2.4) | 2.34 (2.25–2.43) | 2.67 (2.58–2.77) | 2.25 (2.14–2.35) | 2.36 (2.26–2.47) | 2.43 (2.32–2.54) | 2.78 (2.67–2.89) |
| Female | 3.43 (3.33–3.52) | 3.49 (3.4–3.58) | 3.48 (3.39–3.57) | 3.79 (3.69–3.88) | 1.81 (1.68–1.94) | 2.16 (2.03–2.29) | 2.2 (2.07–2.33) | 2.49 (2.35–2.62) |
| χ2, p | 434.257, p = 0.001 | 220.048, p = 0.001 | 254.568, p = 0.001 | 328.39, p = 0.001 | 4265.404, p = 0.001 | 4359.183, p = 0.001 | 4528.862, p = 0.001 | 4662.045, p = 0.001 |
| Acute | ||||||||
| Total | 5.43 (5.34–5.52) | 5.24 (5.15–5.32) | 4.91 (4.83–4.99) | 5.48 (5.39–5.57) | 4.7 (4.57–4.82) | 4.7 (4.59–4.82) | 4.37 (4.26–4.49) | 4.96 (4.85–5.07) |
| Male | 4.78 (4.65–4.91) | 4.59 (4.47–4.72) | 4.32 (4.19–4.44) | 4.89 (4.76–5.02) | 4.93 (4.77–5.08) | 4.78 (4.63–4.93) | 4.43 (4.28–4.57) | 5.04 (4.89–5.18) |
| Female | 6.06 (5.95–6.18) | 5.86 (5.74–5.97) | 5.48 (5.37–5.59) | 6.05 (5.93–6.16) | 4.34 (4.14–4.54) | 4.59 (4.4–4.78) | 4.3 (4.11–4.48) | 4.85 (4.67–5.03) |
| χ2, p | 313.76, p = 0.001 | 196.406, p = 0.001 | 208.622, p = 0.001 | 214.78, p = 0.001 | 8349.901, p = 0.001 | 7441.297, p = 0.001 | 7286.667, p = 0.001 | 7414.013, p = 0.001 |
| Daily use | ||||||||
| Total | 0.13 (0.01–0.26) | 0.22 (0.1–0.35) | 0.28 (0.15–0.41) | 0.34 (0.21–0.46) | 0.06 (0–0.11) | 0.11 (0.01–0.21) | 0.15 (0.05–0.25) | 0.18 (0.02–0.34) |
| Male | 0.08 (0–0.16) | 0.13 (0.04–0.25) | 0.16 (0.06–0.26) | 0.21 (0.02–0.39) | 0.07 (0.02–0.13) | 0.12 (0.02–0.23) | 0.16 (0.06–0.26) | 0.2 (0.1–0.35) |
| Female | 0.19 (0.01–0.36) | 0.32 (0.14–0.49) | 0.39 (0.21–0.57) | 0.46 (0.28–0.64) | 0.05 (0–0.1) | 0.09 (0.04–0.16) | 0.12 (0.02–0.23) | 0.15 (0.05–0.25) |
| χ2, p | 196.231, p = 0.001 | 256.032, p = 0.001 | 265.263, p = 0.001 | 317.198, p = 0.001 | 132.567, p = 0.001 | 214.021, p = 0.001 | 307.247, p = 0.001 | 357.012, p = 0.001 |
| Average of driving-impairing medicines; population opioid use | ||||||||
| Total | 2.51 (2.50–2.52) | 2.55 (2.55–2.56) | 2.53 (2.52–2.53) | 2.55 (2.54–2.56) | 2.30 (2.29–2.32) | 2.35 (2.34–2.37) | 2.36 (2.34–2.37) | 2.38 (2.37–2.40) |
| Male | 2.22 (2.21–2.24) | 2.30 (2.28–2.31) | 2.28 (2.26––2.29) | 2.33 (2.32–2.34) | 2.21 (2.10–2.22) | 2.27 (2.25–2.28) | 2.27 (2.25–2.28) | 2.30 (2.29–2.32) |
| Female | 2.65 (2.64–2.66) | 2.68 (2.67–2.69) | 2.65 (2.64–2.66) | 2.67 (2.66–2.68) | 2.47 (2.44–2.49) | 2.49 (2.47–2.51) | 2.50 (2.47–2.52) | 2.51 (2.49–2.53) |
| t, p | −45.757, p = 0.001 | −41.513, p = 0.001 | −40.116, p = 0.001 | −38.597, p = 0.001 | −16.855, p = 0.001 | −15.636, p = 0.001 | −16.042, p = 0.001 | −15.142, p = 0.001 |
| Average of driving-impairing medicines; population daily opiois use | ||||||||
| Total | 3.65 (3.57–3.73) | 3.55 (3.49–3.61) | 3.44 (3.39–3.50) | 3.44 (3.34–3.49) | 3.80 (3.63–3.87) | 3.75 (3.63–3.87) | 3.54 (3.43–3.65) | 3.57 (3.47–3.67) |
| Male | 3.42 (3.26–3.58) | 3.42 (3.29–3.54) | 3.15 (3.05––3.25) | 3.17 (3.07–3.27) | 3.53 (3.33–3.72) | 3.51 (3.36–3.65) | 3.27 (3.15–3.40) | 3.27 (3.16–3.39) |
| Female | 3.73 (3.64–3.83) | 3.60 (3.53–3.67) | 3.55 (3.49–3.62) | 3.55 (3.48–3.61) | 4.39 (4.05–4.73) | 4.22 (4–4.24) | 4.01 (3.81–4.21) | 4.11 (3.92–4.29) |
| t, p | −3.263, p = 0.001 | −2.553, p = 0.011 | −6.410, p = 0.001 | −6.443, p = 0.001 | −4.579, p = 0.001 | −5.230, p = 0.001 | −6.110, p = 0.001 | −7.451, p = 0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera-Gómez, F.; Gutierrez-Abejón, E.; Ayestarán, I.; Criado-Espegel, P.; Álvarez, F.J. The Trends in Opioid Use in Castile and Leon, Spain: A Population-Based Registry Analysis of Dispensations in 2015 to 2018. J. Clin. Med. 2019, 8, 2148. https://doi.org/10.3390/jcm8122148
Herrera-Gómez F, Gutierrez-Abejón E, Ayestarán I, Criado-Espegel P, Álvarez FJ. The Trends in Opioid Use in Castile and Leon, Spain: A Population-Based Registry Analysis of Dispensations in 2015 to 2018. Journal of Clinical Medicine. 2019; 8(12):2148. https://doi.org/10.3390/jcm8122148
Chicago/Turabian StyleHerrera-Gómez, Francisco, Eduardo Gutierrez-Abejón, Ignacio Ayestarán, Paloma Criado-Espegel, and F. Javier Álvarez. 2019. "The Trends in Opioid Use in Castile and Leon, Spain: A Population-Based Registry Analysis of Dispensations in 2015 to 2018" Journal of Clinical Medicine 8, no. 12: 2148. https://doi.org/10.3390/jcm8122148
APA StyleHerrera-Gómez, F., Gutierrez-Abejón, E., Ayestarán, I., Criado-Espegel, P., & Álvarez, F. J. (2019). The Trends in Opioid Use in Castile and Leon, Spain: A Population-Based Registry Analysis of Dispensations in 2015 to 2018. Journal of Clinical Medicine, 8(12), 2148. https://doi.org/10.3390/jcm8122148








