Regorafenib CSF Penetration, Efficacy, and MRI Patterns in Recurrent Malignant Glioma Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Follow-Up and Statistical Analysis
2.3. Neuroimaging
2.4. Collection of Serum and Cerebrospinal Fluid Samples of Patients
2.5. Liquid Chromatography/Tandem Mass Spectrometry-Based Quantification of Regorafenib and its Active Metabolites
3. Results
3.1. Patient Characteristics and Treatment
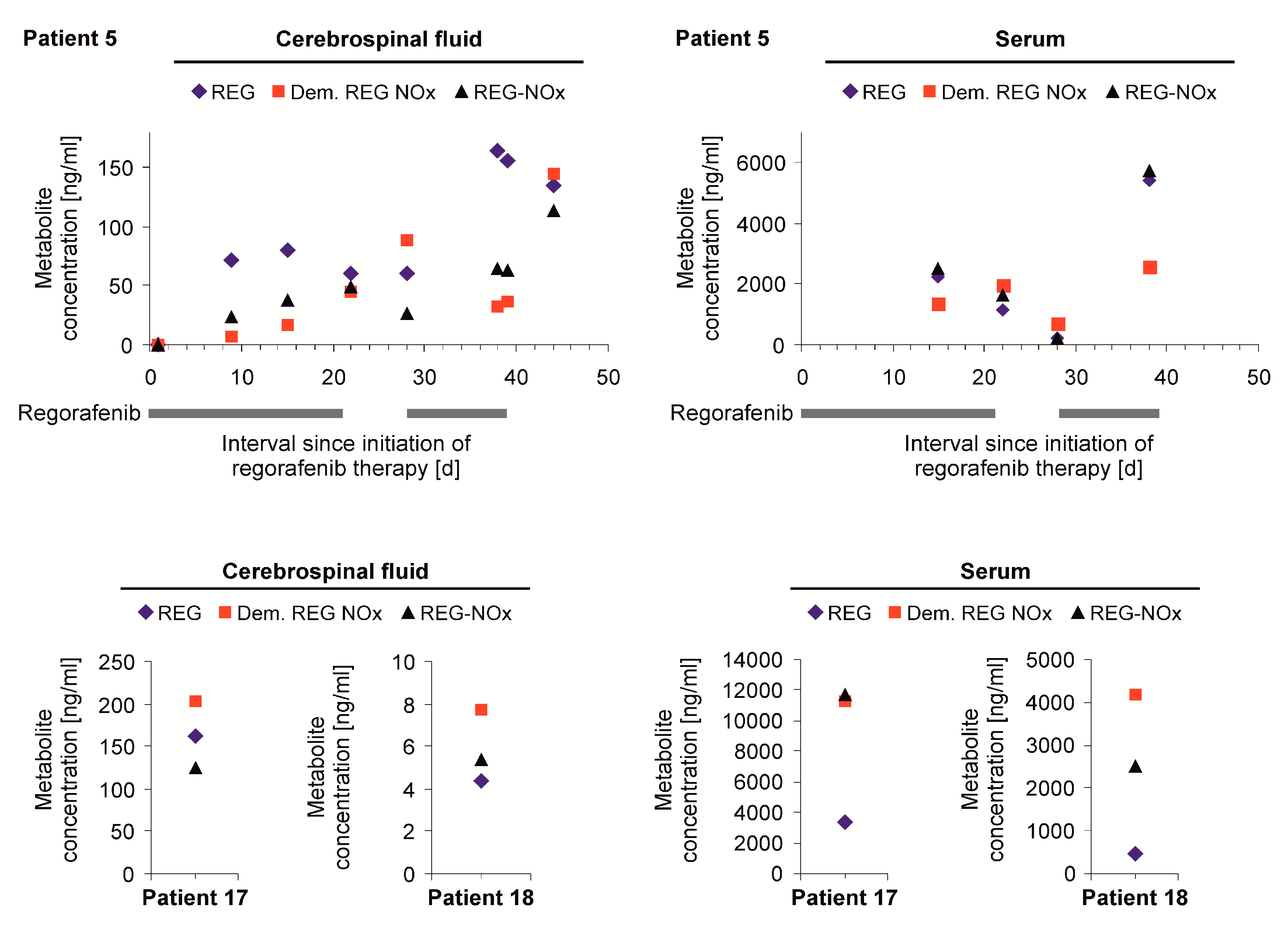
3.2. Detection of Regorafenib and its Metabolites in Cerebrospinal Fluid
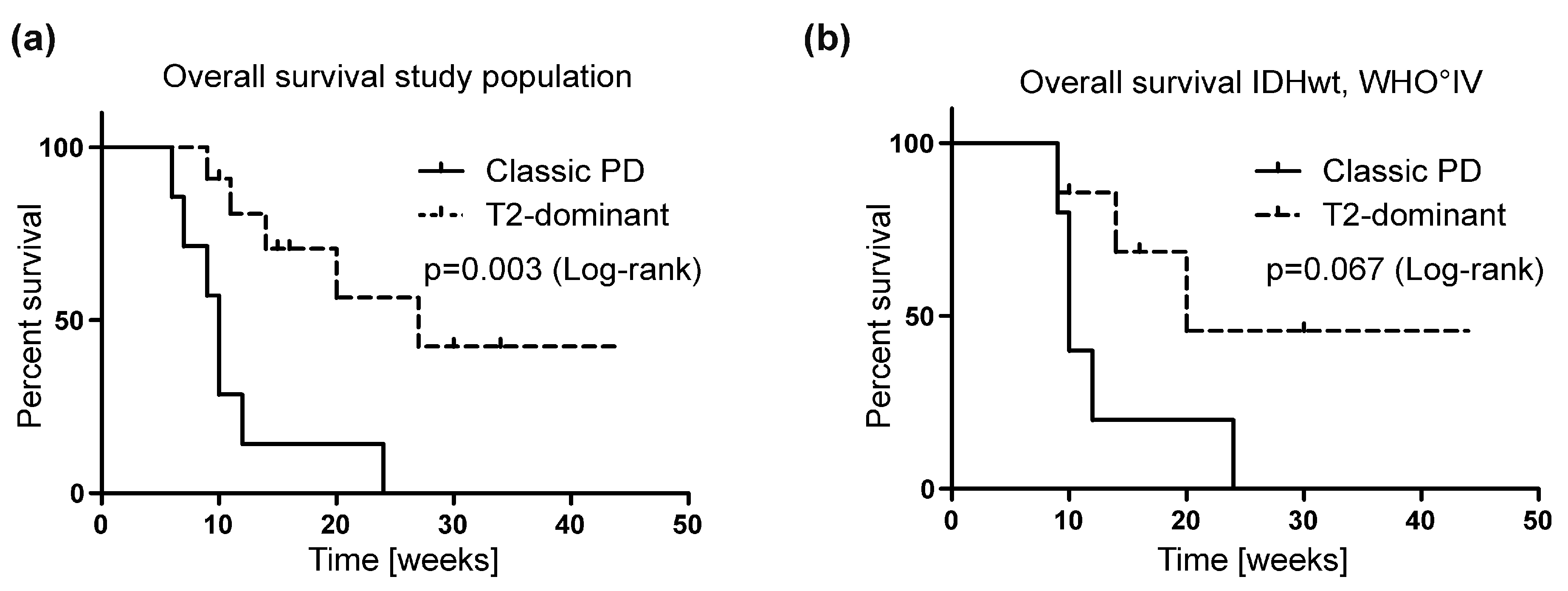
3.3. MRI Growth Patterns under Regorafenib Treatment
3.4. Cerebral Diffusion Weighted Imaging Lesions in Regorafenib-Treated Patients
3.5. Efficacy and Safety Profile of Regorafenib in Recurrent Malignant Glioma Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
Appendix A
LC-MS/MS-Based Quantification of Regorafenib and its Active Metabolites
References
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef]
- Weller, M.; Cloughesy, T.; Perry, J.R.; Wick, W. Standards of care for treatment of recurrent glioblastoma--are we there yet? Neuro-Oncology 2013, 15, 4–27. [Google Scholar] [CrossRef]
- Ronellenfitsch, M.W.; Steinbach, J.P.; Wick, W. Epidermal growth factor receptor and mammalian target of rapamycin as therapeutic targets in malignant glioma: Current clinical status and perspectives. Target. Oncol. 2010, 5, 183–191. [Google Scholar] [CrossRef]
- Chinot, O.L.; Wick, W.; Mason, W.; Henriksson, R.; Saran, F.; Nishikawa, R.; Carpentier, A.F.; Hoang-Xuan, K.; Kavan, P.; Cernea, D.; et al. Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N. Engl. J. Med. 2014, 370, 709–722. [Google Scholar] [CrossRef]
- Batchelor, T.T.; Mulholland, P.; Neyns, B.; Nabors, L.B.; Campone, M.; Wick, A.; Mason, W.; Mikkelsen, T.; Phuphanich, S.; Ashby, L.S.; et al. Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 3212–3218. [Google Scholar] [CrossRef]
- Hutterer, M.; Hattingen, E.; Palm, C.; Proescholdt, M.A.; Hau, P. Current standards and new concepts in MRI and PET response assessment of antiangiogenic therapies in high-grade glioma patients. Neuro-Oncology 2015, 17, 784–800. [Google Scholar] [CrossRef]
- Wen, P.Y.; Macdonald, D.R.; Reardon, D.A.; Cloughesy, T.F.; Sorensen, A.G.; Galanis, E.; Degroot, J.; Wick, W.; Gilbert, M.R.; Lassman, A.B.; et al. Updated response assessment criteria for high-grade gliomas: Response assessment in neuro-oncology working group. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 1963–1972. [Google Scholar] [CrossRef]
- Wilhelm, S.M.; Dumas, J.; Adnane, L.; Lynch, M.; Carter, C.A.; Schutz, G.; Thierauch, K.H.; Zopf, D. Regorafenib (BAY 73-4506): A new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int. J. Cancer 2011, 129, 245–255. [Google Scholar] [CrossRef]
- Grothey, A.; Van Cutsem, E.; Sobrero, A.; Siena, S.; Falcone, A.; Ychou, M.; Humblet, Y.; Bouche, O.; Mineur, L.; Barone, C.; et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): An international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013, 381, 303–312. [Google Scholar] [CrossRef]
- Demetri, G.D.; Reichardt, P.; Kang, Y.K.; Blay, J.Y.; Rutkowski, P.; Gelderblom, H.; Hohenberger, P.; Leahy, M.; von Mehren, M.; Joensuu, H.; et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): An international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013, 381, 295–302. [Google Scholar] [CrossRef]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V.; et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 389, 56–66. [Google Scholar] [CrossRef]
- Hamed, H.A.; Tavallai, S.; Grant, S.; Poklepovic, A.; Dent, P. Sorafenib/regorafenib and lapatinib interact to kill CNS tumor cells. J. Cell Physiol. 2015, 230, 131–139. [Google Scholar] [CrossRef]
- Zhao, P.; Wang, Y.; Kang, X.; Wu, A.; Yin, W.; Tang, Y.; Wang, J.; Zhang, M.; Duan, Y.; Huang, Y. Dual-targeting biomimetic delivery for anti-glioma activity via remodeling the tumor microenvironment and directing macrophage-mediated immunotherapy. Chem. Sci. 2018, 9, 2674–2689. [Google Scholar] [CrossRef]
- Lombardi, G.; De Salvo, G.L.; Brandes, A.A.; Eoli, M.; Ruda, R.; Faedi, M.; Lolli, I.; Pace, A.; Daniele, B.; Pasqualetti, F.; et al. Regorafenib compared with lomustine in patients with relapsed glioblastoma (REGOMA): A multicentre, open-label, randomised, controlled, phase 2 trial. Lancet Oncol. 2019, 20, 110–119. [Google Scholar] [CrossRef]
- Stupp, R. Drug development for glioma: Are we repeating the same mistakes? Lancet Oncol. 2019, 20, 10–12. [Google Scholar] [CrossRef]
- Kebir, S.; Rauschenbach, L.; Radbruch, A.; Lazaridis, L.; Schmidt, T.; Stoppek, A.K.; Pierscianek, D.; Stuschke, M.; Forsting, M.; Sure, U.; et al. Regorafenib in patients with recurrent high-grade astrocytoma. J. Cancer Res. Clin. Oncol. 2019, 145, 1037–1042. [Google Scholar] [CrossRef]
- Tzaridis, T.; Gepfner-Tuma, I.; Hirsch, S.; Skardelly, M.; Bender, B.; Paulsen, F.; Schaub, C.; Weller, J.; Schäfer, N.; Herrlinger, U.; et al. Regorafenib in advanced high-grade glioma: A retrospective bicentric analysis. Neuro-Oncology 2019. [Google Scholar] [CrossRef]
- Capper, D.; Jones, D.T.W.; Sill, M.; Hovestadt, V.; Schrimpf, D.; Sturm, D.; Koelsche, C.; Sahm, F.; Chavez, L.; Reuss, D.E.; et al. DNA methylation-based classification of central nervous system tumours. Nature 2018, 555, 469–474. [Google Scholar] [CrossRef]
- Ellingson, B.M.; Bendszus, M.; Boxerman, J.; Barboriak, D.; Erickson, B.J.; Smits, M.; Nelson, S.J.; Gerstner, E.; Alexander, B.; Goldmacher, G.; et al. Consensus recommendations for a standardized Brain Tumor Imaging Protocol in clinical trials. Neuro-Oncology 2015, 17, 1188–1198. [Google Scholar]
- Radbruch, A.; Lutz, K.; Wiestler, B.; Baumer, P.; Heiland, S.; Wick, W.; Bendszus, M. Relevance of T2 signal changes in the assessment of progression of glioblastoma according to the Response Assessment in Neurooncology criteria. Neuro-Oncology 2012, 14, 222–229. [Google Scholar] [CrossRef]
- Rieger, J.; Bahr, O.; Muller, K.; Franz, K.; Steinbach, J.; Hattingen, E. Bevacizumab-induced diffusion-restricted lesions in malignant glioma patients. J. Neuro-Oncol. 2010, 99, 49–56. [Google Scholar] [CrossRef]
- Server, A.; Kulle, B.; Maehlen, J.; Josefsen, R.; Schellhorn, T.; Kumar, T.; Langberg, C.W.; Nakstad, P.H. Quantitative apparent diffusion coefficients in the characterization of brain tumors and associated peritumoral edema. Acta Radiol 2009, 50, 682–689. [Google Scholar] [CrossRef]
- Patel, P.; Baradaran, H.; Delgado, D.; Askin, G.; Christos, P.; John Tsiouris, A.; Gupta, A. MR perfusion-weighted imaging in the evaluation of high-grade gliomas after treatment: A systematic review and meta-analysis. Neuro-Oncology 2017, 19, 118–127. [Google Scholar] [CrossRef]
- Boxerman, J.L.; Schmainda, K.M.; Weisskoff, R.M. Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am. J. Neuroradiol. 2006, 27, 859–867. [Google Scholar]
- Zopf, D.; Heinig, R.; Thierauch, K.-H.; Hirth-Dietrich, C.; Hafner, F.-T.; Christensen, O.; Lin, T.; Wilhelm, S.; Radtke, M. Abstract 1666: Regorafenib (BAY 73-4506): Preclinical pharmacology and clinical identification and quantification of its major metabolites. Cancer Res. 2010, 70 (Suppl. 8), 1666. [Google Scholar] [CrossRef]
- Zopf, D.; Fichtner, I.; Bhargava, A.; Steinke, W.; Thierauch, K.H.; Diefenbach, K.; Wilhelm, S.; Hafner, F.T.; Gerisch, M. Pharmacologic activity and pharmacokinetics of metabolites of regorafenib in preclinical models. Cancer Med. 2016, 5, 3176–3185. [Google Scholar] [CrossRef]
- Rieger, J.; Bahr, O.; Ronellenfitsch, M.W.; Steinbach, J.; Hattingen, E. Bevacizumab-induced diffusion restriction in patients with glioma: Tumor progression or surrogate marker of hypoxia? J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, e477. [Google Scholar] [CrossRef]
- Gerisch, M.; Hafner, F.T.; Lang, D.; Radtke, M.; Diefenbach, K.; Cleton, A.; Lettieri, J. Mass balance, metabolic disposition, and pharmacokinetics of a single oral dose of regorafenib in healthy human subjects. Cancer Chemother. Pharm. 2018, 81, 195–206. [Google Scholar] [CrossRef]
- Collins, J.M.; Dedrick, R.L. Distributed model for drug delivery to CSF and brain tissue. Am. J. Physiol. 1983, 245, R303–R310. [Google Scholar] [CrossRef]
- De Lange, E.C.; Danhof, M. Considerations in the use of cerebrospinal fluid pharmacokinetics to predict brain target concentrations in the clinical setting: Implications of the barriers between blood and brain. Clin. Pharmacokinet. 2002, 41, 691–703. [Google Scholar] [CrossRef]
- Pope, W.B.; Xia, Q.; Paton, V.E.; Das, A.; Hambleton, J.; Kim, H.J.; Huo, J.; Brown, M.S.; Goldin, J.; Cloughesy, T. Patterns of progression in patients with recurrent glioblastoma treated with bevacizumab. Neurology 2011, 76, 432–437. [Google Scholar] [CrossRef]
- Nowosielski, M.; Ellingson, B.M.; Chinot, O.L.; Garcia, J.; Revil, C.; Radbruch, A.; Nishikawa, R.; Mason, W.P.; Henriksson, R.; Saran, F.; et al. Radiologic progression of glioblastoma under therapy-an exploratory analysis of AVAglio. Neuro-Oncology 2018, 20, 557–566. [Google Scholar] [CrossRef]
- Ganau, M.; Paris, M.; Syrmos, N.; Ganau, L.; Ligarotti, G.K.I.; Moghaddamjou, A.; Prisco, L.; Ambu, R.; Chibbaro, S. How Nanotechnology and Biomedical Engineering Are Supporting the Identification of Predictive Biomarkers in Neuro-Oncology. Medicines (Basel) 2018, 5. [Google Scholar] [CrossRef]
- Ganau, L.; Prisco, L.; Ligarotti, G.K.I.; Ambu, R.; Ganau, M. Understanding the Pathological Basis of Neurological Diseases Through Diagnostic Platforms Based on Innovations in Biomedical Engineering: New Concepts and Theranostics Perspectives. Medicines (Basel) 2018, 5. [Google Scholar] [CrossRef]
- Jost, G.; Pietsch, H.; Grenacher, L. Dynamic contrast-enhanced computed tomography to assess antitumor treatment effects: Comparison of two contrast agents with different pharmacokinetics. Invest Radiol. 2013, 48, 715–721. [Google Scholar] [CrossRef]
- Mong, S.; Ellingson, B.M.; Nghiemphu, P.L.; Kim, H.J.; Mirsadraei, L.; Lai, A.; Yong, W.; Zaw, T.M.; Cloughesy, T.F.; Pope, W.B. Persistent diffusion-restricted lesions in bevacizumab-treated malignant gliomas are associated with improved survival compared with matched controls. AJNR Am. J. Neuroradiol. 2012, 33, 1763–1770. [Google Scholar] [CrossRef]
- Cachia, D.; Elshafeey, N.A.; Kamiya-Matsuoka, C.; Hatami, M.; Alfaro-Munoz, K.D.; Mandel, J.J.; Colen, R.; DeGroot, J.F. Radiographic patterns of progression with associated outcomes after bevacizumab therapy in glioblastoma patients. J. Neuro-Oncol. 2017, 135, 75–81. [Google Scholar] [CrossRef]
- Gupta, A.; Young, R.J.; Karimi, S.; Sood, S.; Zhang, Z.; Mo, Q.; Gutin, P.H.; Holodny, A.I.; Lassman, A.B. Isolated diffusion restriction precedes the development of enhancing tumor in a subset of patients with glioblastoma. AJNR Am. J. Neuroradiol. 2011, 32, 1301–1306. [Google Scholar] [CrossRef]
- Bahr, O.; Harter, P.N.; Weise, L.M.; You, S.J.; Mittelbronn, M.; Ronellenfitsch, M.W.; Rieger, J.; Steinbach, J.P.; Hattingen, E. Sustained focal antitumor activity of bevacizumab in recurrent glioblastoma. Neurology 2014, 83, 227–234. [Google Scholar] [CrossRef]
- Ellingson, B.M.; Cloughesy, T.F.; Lai, A.; Nghiemphu, P.L.; Lalezari, S.; Zaw, T.; Motevalibashinaeini, K.; Mischel, P.S.; Pope, W.B. Quantification of edema reduction using differential quantitative T2 (DQT2) relaxometry mapping in recurrent glioblastoma treated with bevacizumab. J. Neuro-Oncol. 2012, 106, 111–119. [Google Scholar] [CrossRef]

| Characteristics | All Patients (n = 21) | Classic (n = 7, 33%) | T2-Dominant (n = 11, 52%) |
|---|---|---|---|
| General | |||
| Age, y, median (range) | 49 (37–80) | 40 (37–80) | 53 (38–72) |
| Female, % (n) | 38 (8) | 29 (2) | 45 (5) |
| Karnofsky performance status scale, %, median (range) | 70 (50–100) | 80 (50–90) | 70 (50–100) |
| Histology, % (n) | |||
| Isocitrate dehydrogenase (IDH)-wildtype | 71 (15) | 71 (5) | 73 (8) |
| IDH-mutant | 19 (4) | 29 (2) | 18 (2) |
| IDH unknown | 10 (2) | 0 (0) | 9 (1) |
| 1p/19q co-deletion | 5 (1) | 0 (0) | 9 (1) |
| WHO IV | 81 (17) | 86 (6) | 73 (8) |
| WHO III | 19 (4) | 14 (1) | 24 (3) |
| O6-methylguanin-DNA methyltransferase (MGMT) status, % (n) | |||
| Unmethylated | 33 (7) | 43 (3) | 27 (3) |
| Methylated | 38 (8) | 29 (2) | 55 (6) |
| Inconclusive | 19 (4) | 14 (1) | 9 (1) |
| Surgery | |||
| No. of resections, median (range) | 1 (0–3) | 1 (1–2) | 1 (0–2) |
| Patients with 1 resection, % (n) | 62 (13) | 86 (6) | 55 (6) |
| Patients with biopsy only, % (n) | 5 (1) | 0 (0) | 9 (1) |
| Previous Radiotherapy | |||
| No. of radiotherapies, median (range) | 2 (1–3) | 2 (1–2) | 1 (1–2) |
| Patients without radiotherapy, % (n) | 0 (0) | 0 (0) | 0 (0) |
| Previous chemotherapy | |||
| No. of chemotherapies, median (range) | 2 (1–5) | 2 (1–3) | 2 (1–5) |
| Previous NovoTTF-100A, % (n) | 24 (5) | 14 (1) | 27 (3) |
| Recurrences | |||
| No. of recurrences, median (range) | 2 (1–7) | 2 (1–4) | 2 (1–6) |
| Patients with 1 recurrence, % (n) | 19 (4) | 14 (1) | 27 (3) |
| Time from diagnosis to REG, days, median (range) | 553 (217–4525) | 561 (269–4515) | 508 (217–4384) |
| Concomitant therapy, % (n) | |||
| Regorafenib (REG) monotherapy | 90 (19) | 86 (6) | 91 (10) |
| REG + radiotherapy | 5 (1) | 0 (0) | 9 (1) |
| REG + temozolomide | 5 (1) | 14 (1) | 0 (0) |
| Time to first MRI after initiation of REG, days, median (range) | 49 (12–77) | 44 (20–56) | 49 (12–77) |
| Characteristics | All Patients (n = 21) | Classic (n = 7, 33%) | T2-Dominant (n = 11, 52%) |
|---|---|---|---|
| Treatment, days, median (range) | 45 (19–139) | 37 (19–55) | 56 (28–139) |
| Regorafenib dose reduction, % (n) | 19 (4) | 0 (0) | 18 (2) |
| Adverse Events, % (n) | |||
| Skin reaction | 33 (7) | 29 (2) | 27 (3) |
| Elevated transaminases | 29 (6) | 29 (2) | 36 (4) |
| Fatigue | 19 (4) | 14 (1) | 18 (2) |
| Infection | 19 (4) | 14 (1) | 9 (1) |
| Myelosuppression | 19 (4) | 29 (2) | 9 (1) |
| Lung-artery embolization | 10 (2) | 0 (0) | 9 (1) |
| Characteristics | All Patients (n = 21) | Classic (n = 7, 33%) | T2-Dominant (n = 11, 52%) |
|---|---|---|---|
| Steroid reduction, % (n) | 10 (2) | 0 (0) | 18 (2) |
| Overall survival, weeks, median (range) | |||
| Total cohort | 14 (4–44) | 10 (6–24) | 27 (9–44) |
| Censored patients, % (n of X) | 33 (7 of 21) | 0 (0 of 7) | 55 (6 of 11) |
| IDH-wildtype WHO IV patients | 10 (9–24) | 20 (9–44) | |
| Censored patients, % (n of X) | 0 (0 of 5) | 57 (4 of 7) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeiner, P.S.; Kinzig, M.; Divé, I.; Maurer, G.D.; Filipski, K.; Harter, P.N.; Senft, C.; Bähr, O.; Hattingen, E.; Steinbach, J.P.; et al. Regorafenib CSF Penetration, Efficacy, and MRI Patterns in Recurrent Malignant Glioma Patients. J. Clin. Med. 2019, 8, 2031. https://doi.org/10.3390/jcm8122031
Zeiner PS, Kinzig M, Divé I, Maurer GD, Filipski K, Harter PN, Senft C, Bähr O, Hattingen E, Steinbach JP, et al. Regorafenib CSF Penetration, Efficacy, and MRI Patterns in Recurrent Malignant Glioma Patients. Journal of Clinical Medicine. 2019; 8(12):2031. https://doi.org/10.3390/jcm8122031
Chicago/Turabian StyleZeiner, Pia S., Martina Kinzig, Iris Divé, Gabriele D. Maurer, Katharina Filipski, Patrick N. Harter, Christian Senft, Oliver Bähr, Elke Hattingen, Joachim P. Steinbach, and et al. 2019. "Regorafenib CSF Penetration, Efficacy, and MRI Patterns in Recurrent Malignant Glioma Patients" Journal of Clinical Medicine 8, no. 12: 2031. https://doi.org/10.3390/jcm8122031
APA StyleZeiner, P. S., Kinzig, M., Divé, I., Maurer, G. D., Filipski, K., Harter, P. N., Senft, C., Bähr, O., Hattingen, E., Steinbach, J. P., Sörgel, F., Voss, M., Steidl, E., & Ronellenfitsch, M. W. (2019). Regorafenib CSF Penetration, Efficacy, and MRI Patterns in Recurrent Malignant Glioma Patients. Journal of Clinical Medicine, 8(12), 2031. https://doi.org/10.3390/jcm8122031





