Combined Effects of MMP-7, MMP-8 and MMP-26 on the Risk of Ischemic Stroke
Abstract
1. Introduction
2. Research Design and Methods
2.1. Study Population
2.2. Data Collection
2.3. Genomic DNA Isolation and Genotyping of MMP-7, MMP-8 and MMP-26
2.4. Weighted Genetic Risk Score of MMP-7, MMP-8 and MMP-26
2.5. Statistical Analysis
3. Results
3.1. Basic Characteristics of Ischemic Stroke Cases and Controls
3.2. Association Between Selected SNPs and Risk of Ischemic Stroke Risk
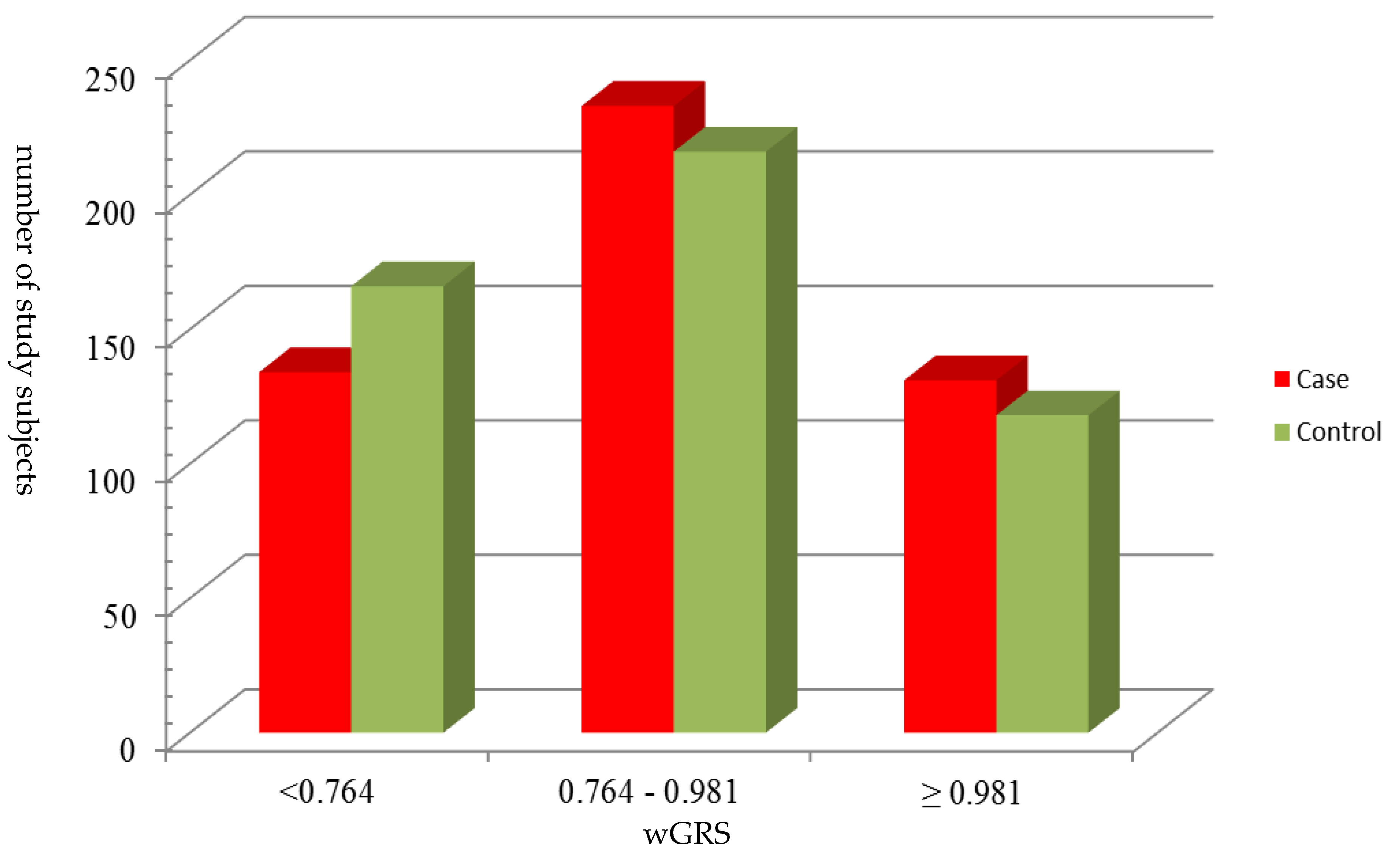
3.3. Association Between wGRS and Risk of Ischemic Stroke Risk
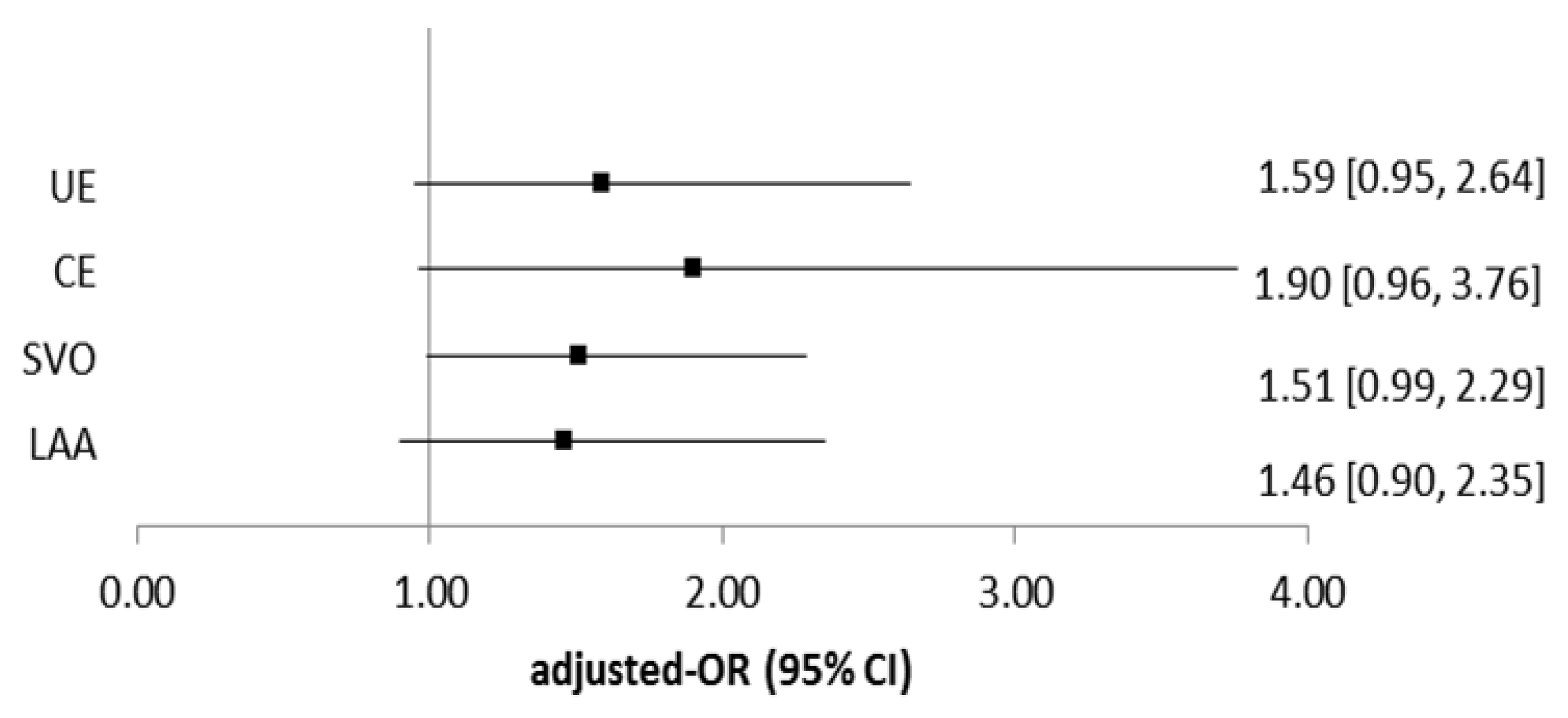
3.4. Association Between wGRS and Risk of Ischemic Stroke Risk in Subgroup Analysis
3.5. Interaction Between High wGRS and Greater Number of Modifiable Cardiovascular Disease Risk Factors on the Risk of Ischemic Stroke
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Genotyping of MMP-7, MMP-8 and MMP-26
| SNP | Primer (5′→3′) a | PCR Condition | RFLP Condition | Product Size (bp) | ||||
|---|---|---|---|---|---|---|---|---|
| Temp (°C) | Time | Cycles | Restriction Enzyme | Temp (°C) | Time | |||
| rs3740938 | F: TGTTTCAGCTATGGGGTTCC R: TCAAGCAACCCTATCCAACC | 95 | 30′ | 35 | BtgI | 37 | 1 h | GG: 388, 88 |
| 57.4 | 30′ | GA: 487, 399, 88 | ||||||
| 72 | 30′ | AA: 487 | ||||||
| rs1940475 | F: TGGAAAGAACCCACGGTATC R: ACAGCAAGACCCCTATGTGC | 95 | 30′ | 35 | BccI | 37 | 4 h | CC: 276, 182 |
| 58.1 | 30′ | CT: 458, 276, 182 | ||||||
| 72 | 30′ | TT: 458 | ||||||
| rs11225395 | F: TTGTATGGGGCCTAGAGCTG R: CTCATTCTCCCTCTCCCTTG | 95 | 30′ | 35 | SfcI | 37 | 4 h | CC: 358, 132, |
| 59.2 | 30′ | CT: 490, 358, 132 | ||||||
| 72 | 30′ | TT: 490 | ||||||
| rs11568818 | F: TGGTACCATAATGTCCTGAATG R: TCGTTATTGGCAGGAAGCACACAATGAATT | 95 | 30′ | 35 | EcoRI-HF | 37 | 1 h | AA: 150 |
| 59.3 | 30′ | AG: 150, 120, 30 | ||||||
| 72 | 30′ | GG: 120, 30 | ||||||
| rs2499966 | F: GATTAGGAATAGACCTTTGCATTTTCGTAC R: GACTTAACCAAAGTTTCATAGC | 95 | 30′ | 35 | Hpy166Ц | 37 | 0.5h | CC: 114, 29 |
| 58 | 30′ | CA: 143, 114, 29 | ||||||
| 72 | 30′ | AA: 143 | ||||||
| SNP | Primer (5′→3′) a | PCR Condition | Product Size (bp) | ||
|---|---|---|---|---|---|
| Temp (°C) | Time | Cycles | |||
| rs10502001 | F1: GCCAATCATGATGTCAGCAG R1: CCTATAACTGGAATGTTAAACTCGCA F2: GGCTTCTGCATTATTTCTATGAGGC R2: ACAGGAACCAAAGGCAAGAG | 95 | 30′ | 35 | CC: 537, 236 |
| 64 | 30′ | CT: 537, 345, 236 | |||
| 72 | 30′ | TT: 537, 345 | |||
| rs2499953 | F1: GTACCGTCCTTCTGAGACC R1: GGAGTGGCGACTCCTTGTT F2: TTTCCATCAATTTTTCCTGAGCG R2: GCTGCCAATGAAAGCAGAA | 95 | 30′ | 35 | AA: 434, 149 |
| 53.7 | 30′ | AG: 434, 326, 149 | |||
| 72 | 30′ | GG: 434, 326 | |||
References
- Mathers, C.D.; Boerma, T.; Ma Fat, D. Global and regional causes of death. Br. Med. Bull. 2009, 92, 7–32. [Google Scholar] [CrossRef] [PubMed]
- Thammaroj, J.; Subramaniam, V.; Bhattacharya, J.J. Stroke in Asia. Neuroimaging Clin. N. Am. 2005, 15, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Tonk, M.; Haan, J. A review of genetic causes of ischemic and hemorrhagic stroke. J. Neurol. Sci. 2007, 257, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.Y.; Han, L.Y.; Huang, X.D.; Guan, C.H.; Mao, X.L.; Ye, Z.S. Association of Matrix Metalloproteinase-1 and Matrix Metalloproteinase-3 Gene Variants with Ischemic Stroke and Its Subtype. J. Stroke Cerebrovasc. Dis. 2017, 26, 368–375. [Google Scholar] [CrossRef]
- Pasterkamp, G.; Schoneveld, A.H.; Hijnen, D.J.; de Kleijn, D.P.; Teepen, H.; van der Wal, A.C.; Borst, C. Atherosclerotic arterial remodeling and the localization of macrophages and matrix metalloproteases 1, 2 and 9 in the human coronary artery. Atherosclerosis 2000, 150, 245–253. [Google Scholar] [CrossRef]
- Hu, W.; Wei, R.; Wang, L.; Lu, J.; Liu, H.; Zhang, W. Correlations of MMP-1, MMP-3, and MMP-12 with the degree of atherosclerosis, plaque stability and cardiovascular and cerebrovascular events. Exp. Ther. Med. 2018, 15, 1994–1998. [Google Scholar] [CrossRef]
- Mahdessian, H.; Perisic Matic, L.; Lengquist, M.; Gertow, K.; Sennblad, B.; Baldassarre, D.; Veglia, F.; Humphries, S.E.; Rauramaa, R.; de Faire, U.; et al. Integrative studies implicate matrix metalloproteinase-12 as a culprit gene for large-artery atherosclerotic stroke. J. Intern. Med. 2017, 282, 429–444. [Google Scholar] [CrossRef]
- Uria, J.A.; Lopez-Otin, C. Matrilysin-2, a new matrix metalloproteinase expressed in human tumors and showing the minimal domain organization required for secretion, latency, and activity. Cancer Res. 2000, 60, 4745–4751. [Google Scholar]
- Halpert, I.; Sires, U.I.; Roby, J.D.; Potter-Perigo, S.; Wight, T.N.; Shapiro, S.D.; Welgus, H.G.; Wickline, S.A.; Parks, W.C. Matrilysin is expressed by lipid-laden macrophages at sites of potential rupture in atherosclerotic lesions and localizes to areas of versican deposition, a proteoglycan substrate for the enzyme. Proc. Natl. Acad. Sci. USA 1996, 93, 9748–9753. [Google Scholar] [CrossRef]
- Abbas, A.; Aukrust, P.; Russell, D.; Krohg-Sorensen, K.; Almas, T.; Bundgaard, D.; Bjerkeli, V.; Sagen, E.L.; Michelsen, A.E.; Dahl, T.B.; et al. Matrix metalloproteinase 7 is associated with symptomatic lesions and adverse events in patients with carotid atherosclerosis. PLoS ONE 2014, 9, e84935. [Google Scholar] [CrossRef]
- Herman, M.P.; Sukhova, G.K.; Libby, P.; Gerdes, N.; Tang, N.; Horton, D.B.; Kilbride, M.; Breitbart, R.E.; Chun, M.; Schonbeck, U. Expression of neutrophil collagenase (matrix metalloproteinase-8) in human atheroma: A novel collagenolytic pathway suggested by transcriptional profiling. Circulation 2001, 104, 1899–1904. [Google Scholar] [CrossRef] [PubMed]
- Rekhter, M.D.; Zhang, K.; Narayanan, A.S.; Phan, S.; Schork, M.A.; Gordon, D. Type I collagen gene expression in human atherosclerosis. Localization to specific plaque regions. Am. J. Pathol. 1993, 143, 1634–1648. [Google Scholar] [PubMed]
- Dozier, S.; Escobar, G.P.; Lindsey, M.L. Matrix metalloproteinase (MMP)-7 activates MMP-8 but not MMP-13. Med. Chem. 2006, 2, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Tuomainen, A.M.; Kormi, I.; Havulinna, A.S.; Tervahartiala, T.; Salomaa, V.; Sorsa, T.; Pussinen, P.J. Serum tissue-degrading proteinases and incident cardiovascular disease events. Eur. J. Prev. Cardiol. 2014, 21, 806–812. [Google Scholar] [CrossRef] [PubMed]
- Sorsa, T.; Tervahartiala, T.; Leppilahti, J.; Hernandez, M.; Gamonal, J.; Tuomainen, A.M.; Lauhio, A.; Pussinen, P.J.; Mantyla, P. Collagenase-2 (MMP-8) as a point-of-care biomarker in periodontitis and cardiovascular diseases. Therapeutic response to non-antimicrobial properties of tetracyclines. Pharmacol. Res. 2011, 63, 108–113. [Google Scholar] [PubMed]
- Esenwa, C.C.; Elkind, M.S. Inflammatory risk factors, biomarkers and associated therapy in ischaemic stroke. Nat. Rev. Neurol. 2016, 12, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Khamis, Z.I.; Zorio, D.A.; Chung, L.W.; Sang, Q.X. The Anti-inflammatory Role of Endometase/Matrilysin-2 in Human Prostate Cancer Cells. J. Cancer 2013, 4, 296–303. [Google Scholar] [CrossRef]
- Hsieh, Y.C.; Jeng, J.S.; Lin, H.J.; Hu, C.J.; Yu, C.C.; Lien, L.M.; Peng, G.S.; Chen, C.I.; Tang, S.C.; Chi, N.F.; et al. Epistasis analysis for estrogen metabolic and signaling pathway genes on young ischemic stroke patients. PLoS ONE 2012, 7, e47773. [Google Scholar] [CrossRef]
- Adams, H.P., Jr.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E., 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar] [CrossRef]
- Graziewicz, M.A.; Day, B.J.; Copeland, W.C. The mitochondrial DNA polymerase as a target of oxidative damage. Nucleic Acids Res. 2002, 30, 2817–2824. [Google Scholar] [CrossRef]
- Lee, P.H.; Shatkay, H. F-SNP: Computationally predicted functional SNPs for disease association studies. Nucleic Acids Res. 2008, 36, D820–D824. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Taylor, J.A. SNPinfo: Integrating GWAS and candidate gene information into functional SNP selection for genetic association studies. Nucleic Acids Res. 2009, 37, W600–W605. [Google Scholar] [CrossRef] [PubMed]
- McLaren, W.; Gil, L.; Hunt, S.E.; Riat, H.S.; Ritchie, G.R.; Thormann, A.; Flicek, P.; Cunningham, F. The Ensembl Variant Effect Predictor. Genome Biol. 2016, 17, 122. [Google Scholar] [CrossRef] [PubMed]
- Laxton, R.C.; Hu, Y.; Duchene, J.; Zhang, F.; Zhang, Z.; Leung, K.Y.; Xiao, Q.; Scotland, R.S.; Hodgkinson, C.P.; Smith, K.; et al. A role of matrix metalloproteinase-8 in atherosclerosis. Circ. Res. 2009, 105, 921–929. [Google Scholar] [CrossRef]
- Pradhan-Palikhe, P.; Pussinen, P.J.; Vikatmaa, P.; Palikhe, A.; Kivimäki, A.S.; Lepäntalo, M.; Salo, T.; Sorsa, T. Single nucleotide polymorphism –799C/T in matrix metalloproteinase-8 promoter region in arterial disease. Innate Immun. 2012, 18, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.Z.; Du, X.M.; Jing, Q.M.; Li, X.X.; Gu, R.X.; Wang, J.; Han, Y.L. Impact of matrix metalloproteinase-8 gene variations on the risk of thoracic aortic dissection in a Chinese Han population. Mol. Biol. Rep. 2013, 40, 5953–5958. [Google Scholar] [CrossRef]
- Cauchi, S.; Meyre, D.; Durand, E.; Proenca, C.; Marre, M.; Hadjadj, S.; Choquet, H.; De Graeve, F.; Gaget, S.; Allegaert, F.; et al. Post genome-wide association studies of novel genes associated with type 2 diabetes show gene-gene interaction and high predictive value. PLoS ONE 2008, 3, e2031. [Google Scholar] [CrossRef]
- Panayiotou, A.G.; Griffin, M.B.; Tyllis, T.; Georgiou, N.; Bond, D.; Humphries, S.E.; Nicolaides, A.N. Association of genotypes at the matrix metalloproteinase (MMP) loci with carotid IMT and presence of carotid and femoral atherosclerotic plaques. Vasc. Med. 2013, 18, 298–306. [Google Scholar] [CrossRef]
- Andersson, T.; Alfredsson, L.; Kallberg, H.; Zdravkovic, S.; Ahlbom, A. Calculating measures of biological interaction. Eur. J. Epidemiol. 2005, 20, 575–579. [Google Scholar] [CrossRef]
- Peeters, W.; Moll, F.L.; Vink, A.; van der Spek, P.J.; de Kleijn, D.P.; de Vries, J.P.; Verheijen, J.H.; Newby, A.C.; Pasterkamp, G. Collagenase matrix metalloproteinase-8 expressed in atherosclerotic carotid plaques is associated with systemic cardiovascular outcome. Eur. Heart J. 2011, 32, 2314–2325. [Google Scholar] [CrossRef]
- Pussinen, P.J.; Sarna, S.; Puolakkainen, M.; Ohlin, H.; Sorsa, T.; Pesonen, E. The balance of serum matrix metalloproteinase-8 and its tissue inhibitor in acute coronary syndrome and its recurrence. Int. J. Cardiol. 2013, 167, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Lind, L.; Siegbahn, A.; Lindahl, B.; Stenemo, M.; Sundstrom, J.; Arnlov, J. Discovery of New Risk Markers for Ischemic Stroke Using a Novel Targeted Proteomics Chip. Stroke 2015, 46, 3340–3347. [Google Scholar] [CrossRef] [PubMed]
- Kormi, I.; Nieminen, M.T.; Havulinna, A.S.; Zeller, T.; Blankenberg, S.; Tervahartiala, T.; Sorsa, T.; Salomaa, V.; Pussinen, P.J. Matrix metalloproteinase-8 and tissue inhibitor of matrix metalloproteinase-1 predict incident cardiovascular disease events and all-cause mortality in a population-based cohort. Eur. J. Prev. Cardiol. 2017, 24, 1136–1144. [Google Scholar] [CrossRef] [PubMed]
- Molloy, K.J.; Thompson, M.M.; Jones, J.L.; Schwalbe, E.C.; Bell, P.R.; Naylor, A.R.; Loftus, I.M. Unstable carotid plaques exhibit raised matrix metalloproteinase-8 activity. Circulation 2004, 110, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.G.; Xiao, A.Z.; Ni, J.; Man, Y.G.; Sang, Q.X. Expression of matrix metalloproteinase-26 in multiple human cancer tissues and smooth muscle cells. Ai Zheng = Aizheng = Chin. J. Cancer 2009, 28, 1168–1175. [Google Scholar] [CrossRef]
- Decock, J.; Long, J.R.; Laxton, R.C.; Shu, X.O.; Hodgkinson, C.; Hendrickx, W.; Pearce, E.G.; Gao, Y.T.; Pereira, A.C.; Paridaens, R.; et al. Association of matrix metalloproteinase-8 gene variation with breast cancer prognosis. Cancer Res. 2007, 67, 10214–10221. [Google Scholar] [CrossRef]
- Du, J.; Jin, T.; Cao, Y.; Chen, J.; Guo, Y.; Sun, M.; Li, J.; Zhang, X.; Wang, G.; Wang, J. Association between genetic polymorphisms of MMP8 and the risk of steroid-induced osteonecrosis of the femoral head in the population of northern China. Medicine 2016, 95, e4794. [Google Scholar] [CrossRef]
| Variables a | Cases N = 500 | Controls N = 500 | p Value b |
|---|---|---|---|
| Age | 61.33 ± 11.07 | 61.17 ± 10.99 | 0.8085 |
| Males | 333 (66.60) | 333 (66.60) | 1.0000 |
| Smoking | 241 (48.59) | 154 (30.86) | <0.0001 |
| Alcohol drinking | 105 (21.13) | 67 (13.40 ) | 0.0012 |
| Hypertension | 374 (74.80) | 263 (52.60) | <0.0001 |
| Diabetes | 227 (45.40) | 83 (16.60) | <0.0001 |
| Hyperlipidemia | 414 (82.97) | 405 (81.00) | 0.4189 |
| Obesity | 143 (29.61) | 99 (20.00) | 0.0005 |
| Gene | rs Number a | Region | Risk Allele | Risk Allele Frequency | Other Allele | Additive Model | Dominant Model | Recessive Model |
|---|---|---|---|---|---|---|---|---|
| aOR (95%CI) b | aOR (95%CI) b | aOR (95%CI) b | ||||||
| MMP-7 | rs10502001 | 11q22.2 | C | 0.72 | T | 1.06 (0.83–1.35) | 1.79 (1.01–3.16) c | 0.93 (0.68–1.26) |
| MMP-7 | rs11568818 | 11q22.2 | G | 0.08 | A | 0.98 (0.65–1.46) | 1.00 (0.65–1.55) | 0.58 (0.09–3.56) |
| MMP-8 | rs3740938 | 11q22.2 | A | 0.25 | G | 1.02 (0.80–1.30) | 0.87 (0.64–1.18) | 1.92 (1.03–3.58) c |
| MMP-8 | rs1940475 | 11q22.2 | C | 0.60 | T | 1.11 (0.89–1.39) | 1.06 (0.69–1.62) | 1.20 (0.87–1.66) e |
| MMP-8 | rs11225395 | 11q22.2 | T | 0.39 | C | 1.02 (0.81–1.28) | 0.94 (0.68–1.29) | 1.24 (0.79–1.93) e |
| MMP-26 | rs2499953 | 11p15.4 | G | 0.30 | A | 1.00 (0.78–1.26) | 0.99 (0.73–1.35) | 1.00 (0.58–1.72) |
| MMP-26 | rs2499966 | 11p15.4 | C | 0.75 | A | 1.27 (0.98–1.63) d | 0.82 (0.43–1.56) | 1.49 (1.10–2.04) c |
| Variables | Adjusted-OR a (95% CI) |
|---|---|
| Smoking | |
| No | 1.00 (ref.) |
| Yes | 2.54 (1.81–3.56) c |
| Alcohol drinking | |
| No | 1.00 (ref.) |
| Yes | 1.40 (0.95–2.07) |
| Obesity | |
| No | 1.00 (ref.) |
| Yes | 1.31 (0.94–1.81) |
| Hypertension | |
| No | 1.00 (ref.) |
| Yes | 2.38 (1.75–3.24) c |
| Diabetes | |
| No | 1.00 (ref.) |
| Yes | 3.63 (2.66–4.95) c |
| wGRS b | |
| <0.764 | 1.00 (ref.) |
| 0.764–0.981 | 1.50 (1.08–2.08) c |
| ≥ 0.981 | 1.59 (1.09–2.32) c |
| Variables | Ca/Co | Adjusted OR (95% CI) a | ||
|---|---|---|---|---|
| wGRS <0.764 | wGRS ≥0.764 | |||
| Age | ≦55 | 149/151 | 1.00 (ref) | 1.38 (0.75–2.53) |
| >55 | 329/343 | 1.00 (ref) | 1.62 (1.13–2.33) b | |
| sex | Female | 158/164 | 1.00 (ref) | 1.44 (0.83–2.50) |
| Male | 320/330 | 1.00 (ref) | 1.60 (1.10–2.33) b | |
| Smoking | No | 244/343 | 1.00 (ref) | 1.57 (1.04–2.36) b |
| Yes | 234/151 | 1.00 (ref) | 1.46 (0.91–2.35) | |
| Alcohol drinking | No | 376/427 | 1.00 (ref) | 1.57 (1.11–2.20) b |
| Yes | 102/67 | 1.00 (ref) | 1.41 (0.68–2.93) | |
| Hypertension | No | 117/234 | 1.00 (ref) | 1.15 (0.64–2.06) |
| Yes | 361/260 | 1.00 (ref) | 1.68 (1.17–2.42) b | |
| Diabetes | No | 261/411 | 1.00 (ref) | 1.45 (1.00–2.09) b |
| Yes | 217/83 | 1.00 (ref) | 1.77 (1.01–3.10) b | |
| Obesity | No | 335/395 | 1.00 (ref) | 1.53 (1.07–2.21) b |
| Yes | 143/99 | 1.00 (ref) | 1.39 (0.78–2.48) |
| Subgroup | Ca/Co | Adjusted-OR (95% CI) c | S (95% CI) | RERI (95% CI) | AP (95% CI) |
|---|---|---|---|---|---|
| Low genetic risk (wGRS<0.764) | |||||
| Low modifiable CVD risk a | 32/85 | 1.00 (ref) | |||
| High modifiable CVD risk b | 96/78 | 3.59 (2.15–6.00) | 1.65(0.99–2.73) | 1.87(0.16–3.57) d | 0.33(0.07–0.58) d |
| High genetic risk (wGRS≧0.764) | |||||
| Low modifiable CVD risk a | 95/201 | 1.29 (0.80–2.08) | |||
| High modifiable CVD risk b | 255/130 | 5.75 (3.60–9.19) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, F.-I.; Chiou, H.-Y.; Hu, C.-J.; Jeng, J.-S.; Lin, H.-J.; Lee, J.-T.; Lien, L.-M. Combined Effects of MMP-7, MMP-8 and MMP-26 on the Risk of Ischemic Stroke. J. Clin. Med. 2019, 8, 2011. https://doi.org/10.3390/jcm8112011
Hsieh F-I, Chiou H-Y, Hu C-J, Jeng J-S, Lin H-J, Lee J-T, Lien L-M. Combined Effects of MMP-7, MMP-8 and MMP-26 on the Risk of Ischemic Stroke. Journal of Clinical Medicine. 2019; 8(11):2011. https://doi.org/10.3390/jcm8112011
Chicago/Turabian StyleHsieh, Fang-I, Hung-Yi Chiou, Chaur-Jong Hu, Jiann-Shing Jeng, Huey-Juan Lin, Jiunn-Tay Lee, and Li-Ming Lien. 2019. "Combined Effects of MMP-7, MMP-8 and MMP-26 on the Risk of Ischemic Stroke" Journal of Clinical Medicine 8, no. 11: 2011. https://doi.org/10.3390/jcm8112011
APA StyleHsieh, F.-I., Chiou, H.-Y., Hu, C.-J., Jeng, J.-S., Lin, H.-J., Lee, J.-T., & Lien, L.-M. (2019). Combined Effects of MMP-7, MMP-8 and MMP-26 on the Risk of Ischemic Stroke. Journal of Clinical Medicine, 8(11), 2011. https://doi.org/10.3390/jcm8112011




