Salivary IL-6 mRNA is a Robust Biomarker in Oral Squamous Cell Carcinoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Control Subjects
2.2. Saliva Collection and Processing
2.3. Reverse Transcription and Real-Time Quantitative PCR (qPCR)
2.4. Enzyme-Linked Immune-Sorbent Assay (ELISA)
2.5. Immunohistochemistry (IHC)
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
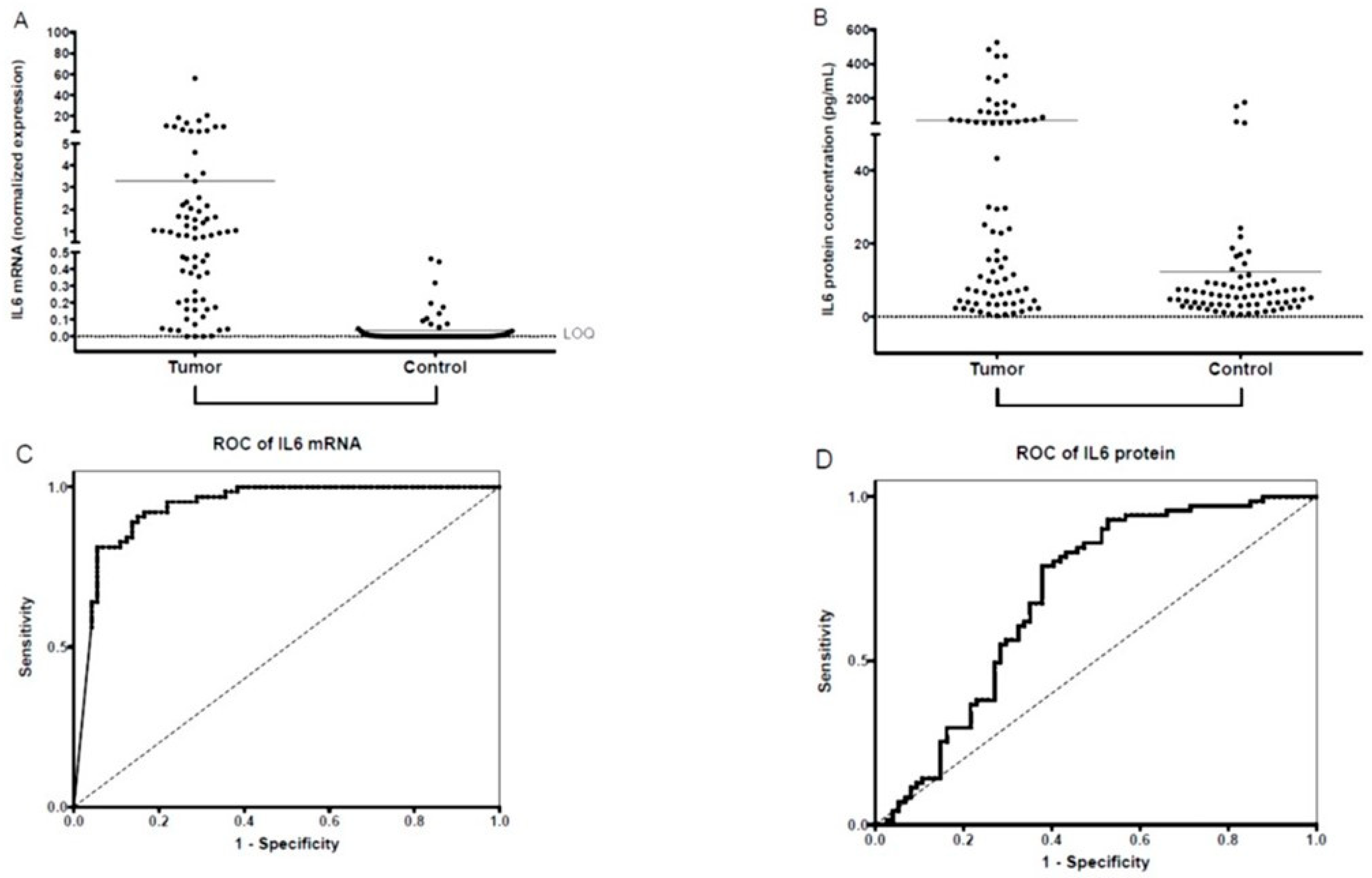
3.2. Salivary IL-6 mRNA and IL-6 Protein Expression
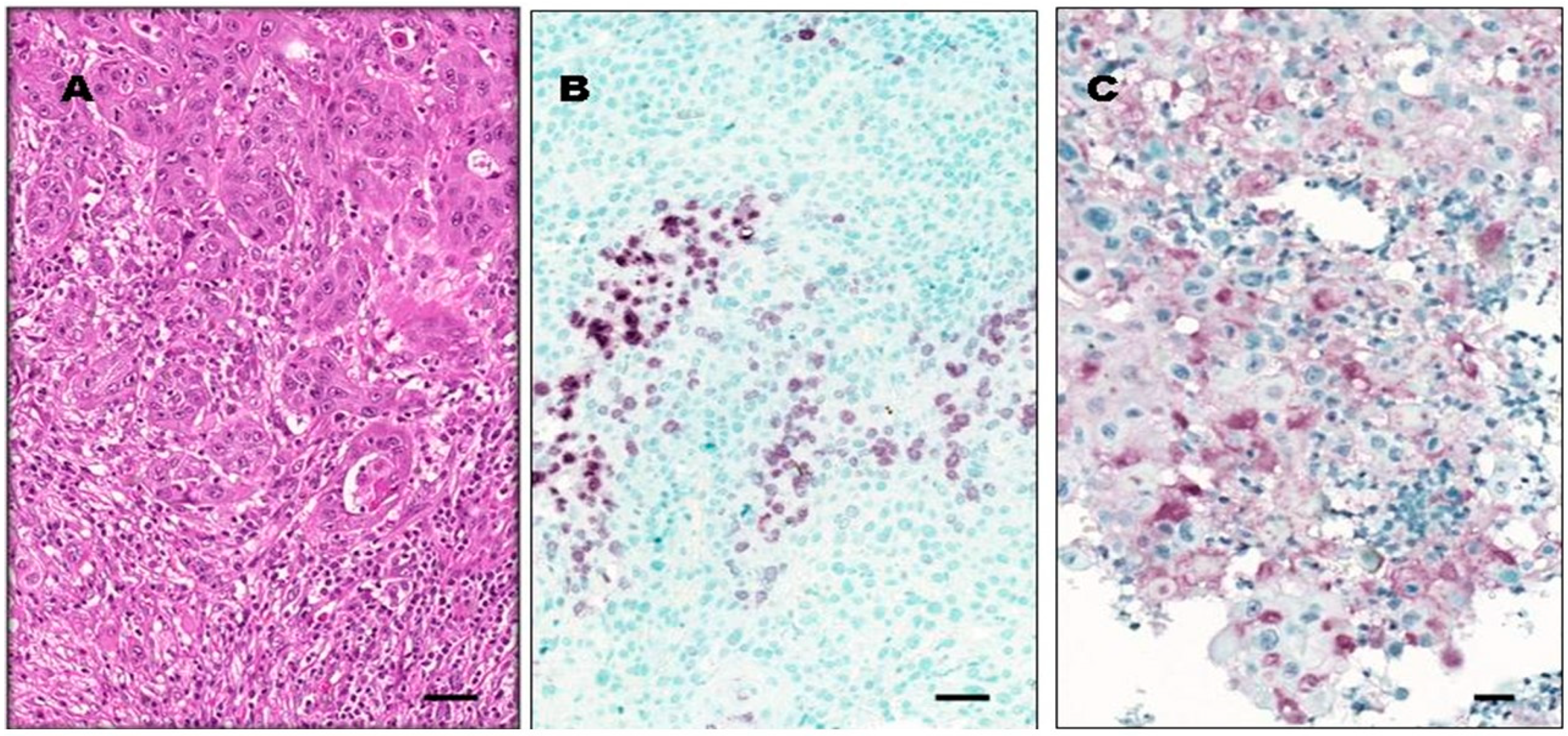
3.3. IL-6 Protein Expression in OSCC Tumor Tissue
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Diz, P.; Meleti, M.; Diniz-Freitas, M.; Vescovi, P.; Warnakulasuriya, S.; Johnson, N.W.; Kerr, A.R. Oral and pharyngeal cancer in Europe: Incidence, mortality and trends as presented to the Global Oral Cancer Forum. Trans. Res. Oral Oncol. 2017, 2, 1–13. [Google Scholar] [CrossRef]
- Zhang, H.; Dziegielewski, P.T.; Biron, V.L.; Szudek, J.; Al-Qahatani, K.H.; O’Connell, D.A. Survival outcomes of patients with advanced oral cavity squamous cell carcinoma treated with multimodal therapy: A multi-institutional analysis. J. Otolaryngol. Head Neck Surg. 2013, 42, 30. [Google Scholar] [CrossRef] [PubMed]
- Carreras-Torras, C.; Gay-Escoda, C. Techniques for early diagnosis of oral squamous cell carcinoma: Systematic review. Med. Oral Patol. Oral Cir. Bucal. 2015, 20, e305–e315. [Google Scholar] [CrossRef] [PubMed]
- SahebJamee, M.; Eslami, M.; AtarbashiMoghadam, F.; Sarafnejad, A. Salivary concentration of TNFalpha, IL1 alpha, IL6, and IL8 in oral squamous cell carcinoma. Med. Oral Patol. Oral Cir. Bucal. 2008, 13, E292–E295. [Google Scholar] [PubMed]
- Wu, J.Y.; Yi, C.; Chung, H.R.; Wang, D.J.; Chang, W.C.; Lee, S.Y.; Lin, C.T.; Yang, Y.C.; Yang, W.C. Potential biomarkers in saliva for oral squamous cell carcinoma. Oral Oncol. 2010, 46, 226–231. [Google Scholar] [CrossRef]
- Panta, P.; Venna, V.R. Salivary RNA signatures in oral cancer detection. Anal. Cell. Pathol. 2014, 2014, 450629. [Google Scholar] [CrossRef]
- Khan, R.S.; Khurshid, Z.; Akhbar, S.; Faraz Moin, S. Advances of Salivary Proteomics in Oral Squamous Cell Carcinoma (OSCC) Detection: An Update. Proteomes 2016, 4, 41. [Google Scholar] [CrossRef]
- Radhika, T.; Jeddy, N.; Nithya, S.; Muthumeenakshi, R.M. Salivary biomarkers in oral squamous cell carcinoma—An insight. J. Oral Biol. Craniofac. Res. 2016, 6, S51–S54. [Google Scholar] [CrossRef]
- Lohavanichbutr, P.; Zhang, Y.; Wang, P.; Gu, H.; Nagana Gowda, G.A.; Djukovic, D.; Buas, M.F.; Raftery, D.; Chen, C. Salivary metabolite profiling distinguishes patients with oral cavity squamous cell carcinoma from normal controls. PLoS ONE 2018, 13, e0204249. [Google Scholar] [CrossRef]
- Zhao, S.Y.; Wang, J.; Ouyang, S.B.; Huang, Z.K.; Liao, L. Salivary Circular RNAs Hsa_Circ_0001874 and Hsa_Circ_0001971 as Novel Biomarkers for the Diagnosis of Oral Squamous Cell Carcinoma. Cell. Physiol. Biochem. 2018, 47, 2511–2521. [Google Scholar] [CrossRef]
- Sahibzada, H.A.; Khurshid, Z.; Khan, R.S.; Naseem, M.; Siddique, K.M.; Mali, M.; Zafar, M.S. Salivary IL-8, IL-6 and TNF-α as potential diagnostic biomarkers for oral cancer. Diagnostics 2017, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Horváth, J.; Szabó, A.; Tar, I.; Dezső, B.; Kiss, C.; Márton, I.; Scholtz, B. Oral health may affect the performance of mRNA-based saliva biomarkers for oral squamous cell cancer. Pathol. Oncol. Res. 2018, 24, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Csősz, É.; Lábiscsák, P.; Kalló, G.; Márkus, B.; Emri, M.; Szabó, A.; Tar, I.; Tőzsér, J.; Kiss, C.; Márton, I. Proteomics investigation of OSCC-specific salivary biomarkers in a Hungarian population highlights the importance of identification of population-tailored biomarkers. PLoS ONE 2017, 12, e0177282. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Oral Health Surveys: Basic Methods, 4th ed.; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Lang, N.P.; Corbet, E.F. Periodontal diagnosis in daily practice. Int. Dent. J. 1995, 45, 3–15. [Google Scholar] [PubMed]
- Pindborg, J.J.; Reichart, P.A.; Smith, C.J.; Van der Waal, I. Histological Typing of Cancer and Precancer of the Oral Mucosa. WHO International Histological Classification of Tumours, 2nd ed.; Springer: Berlin, Germany, 1997. [Google Scholar]
- Sobin, L.H.; Gospodarowitz, M.K.; Wittekind, C. Head and Neck Tumours: Lip and oral cavity. In TNM Classification of Malignant Tumours, 7th ed.; Wiley-Blackwell: Chichester, UK, 2010; pp. 25–29. [Google Scholar]
- Tsakiris, I.; Torocsik, D.; Gyongyosi, A.; Dozsa, A.; Szatmari, I.; Szanto, A.; Soos, G.; Nemes, Z.; Igali, L.; Marton, I.; et al. Carboxypeptidase-M is regulated by lipids and CSFs in macrophages and dendritic cells and expressed selectively in tissue granulomas and foam cells. Lab. Investig. 2012, 92, 345–361. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Szabó, K.; Papp, G.; Dezso, B.; Zeher, M. The histopathology of labial salivary glands in primary Sjögren’ syndrome: Focusing on follicular helper T cells in the inflammatory infiltrates. Mediators Inflamm. 2014, 2014, 631787. [Google Scholar] [CrossRef]
- Nemes, J.A.; Redl, P.; Boda, R.; Kiss, C.; Márton, I.J. Oral cancer report from Northeastern Hungary. Pathol. Oncol. Res. 2008, 14, 85–92. [Google Scholar] [CrossRef]
- Németh, Z.; Turi, K.; Léhner, G.; Veres, D.S.; Csurgay, K. The prognostic role of age in oral cancer. A clinical study. Magy. Onkol. 2013, 57, 166–172. (In Hungarian) [Google Scholar]
- St John, M.A.; Li, Y.; Zhou, X.; Denny, P.; Ho, C.M.; Montemagno, C.; Shi, W.; Qi, F.; Wu, B.; Sinha, U.; et al. Interleukin 6 and interleukin 8 as potential biomarkers for oral cavity and oropharyngeal squamous cell carcinoma. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 929–935. [Google Scholar] [CrossRef]
- Brinkmann, O.; Kastratovic, D.A.; Dimitrijevic, M.V.; Konstantinovic, V.S.; Jelovac, D.B.; Antic, J.; Nesic, V.S.; Markovic, S.Z.; Martinovic, Z.R.; Akin, D.; et al. Oral squamous cell carcinoma detection by salivary biomarkers in Serbian population. Oral Oncol. 2011, 47, 51–55. [Google Scholar] [CrossRef]
- Gai, C.; Camussi, F.; Broccoletti, R.; Gambino, A.; Cabras, M.; Molinaro, L.; Carossa, S.; Camussi, G.; Arduino, P.G. Salivary extracellular vesicle-associated miRNAs as potential biomarkers in oral squamous cell carcinoma. BMC Cancer 2018, 18, 439. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Li, Q.; Chen, J.; Yi, P.; Xu, X.; Fan, Y.; Cui, B.; Yu, Y.; Li, X.; Du, Y.; et al. Salivary protease spectrum biomarkers of oral cancer. Int. J. Oral Sci. 2019, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Rhodus, N.L.; Ho, V.; Miller, C.S.; Myers, S.; Ondrey, F. NF-kappaB dependent cytokine levels in saliva of patients with oral paraneoplastic lesions and oral squamous cell carcinoma. Cancer Detect. Prev. 2005, 29, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Duffy, S.A.; Taylor, J.M.; Terrell, J.E.; Islam, M.; Li, Y.; Wolf, G.T.; Teknos, T.N. Interleukin-6 predicts recurrence and survival among head and neck cancer patients. Cancer 2008, 113, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Katakura, A.; Kamiyama, I.; Takano, N.; Shibahara, T.; Muramatsu, T.; Ishihara, K.; Takagi, R.; Shouno, T. Comparison of salivary cytokine levels in oral cancer patients and healthy subjects. Bull. Tokyo Dent. Coll. 2007, 48, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Sato, J.; Goto, J.; Murata, T.; Kitamori, S.; Yamazaki, Y.; Satoh, A.; Kitagawa, Y. Changes in saliva interleukin-6 levels in patients with oral squamous cell carcinoma. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, 330–336. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Korostoff, A.; Reder, L.; Masood, R.; Sinha, U.K. The role of salivary cytokine biomarkers in tongue cancer invasion and mortality. Oral Oncol. 2011, 47, 282–287. [Google Scholar] [CrossRef]
- Brailo, V.; Vucicevic-Boras, V.; Lukac, J.; Biocina-Lukenda, D.; Zilic-Alajbeg, I.; Milenovic, A.; Balija, M. Salivary and serum interleukin 1 beta, interleukin 6 and tumor necrosis factor alpha in patients with leukoplakia and oral cancer. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e10–e15. [Google Scholar] [CrossRef]
- Lisa Cheng, Y.S.; Jordan, L.; Gorugantula, L.M.; Schneiderman, E.; Chen, H.S.; Rees, T. Salivary interleukin-6 and -8 in patients with oral cancer and patients with chronic oral inflammatory diseases. J. Periodontol. 2014, 85, 956–965. [Google Scholar] [CrossRef]
- Arduino, P.G.; Menegatti, E.; Cappello, N.; Martina, E.; Gardino, N.; Tanteri, C.; Cavallo, F.; Scully, C.; Broccoletti, R. Possible role for interleukins as biomarkers for mortality and recurrence in oral cancer. Int. J. Biol. Markers 2015, 30, e262–e266. [Google Scholar] [CrossRef]
- Panneer Selvam, N.; Sadaksharam, J. Salivary interleukin-6 in the detection of oral cancer and precancer. Asia. Pac. J. Clin. Oncol. 2015, 11, 236–241. [Google Scholar] [CrossRef]
- Rao, M.; Ramesh, A.; Adapa, S.; Thomas, B.; Shetty, J. Correlation of salivary levels of interleukin-6 and albumin with oral squamous cell carcinoma. J. Health Res. Rev. 2016, 3, 11–14. [Google Scholar] [CrossRef]
- Juretic, M.; Cerovic, R.; Belusic-Gobic, M.; Brekalo Prso, I.; Kqiku, L.; Spalj, S.; Pezelj-Ribaric, S. Salivary levels of TNF-α and IL-6 in patients with oral premalignant and malignant lesions. Folia Biol. 2013, 59, 99–102. [Google Scholar]
- Dikova, V.R.; Principe, S.; Bagan, J.V. Salivary inflammatory proteins in patients with oral potentially malignant disorders. J. Clin. Exp. Dent. 2019, 11, e659–e664. [Google Scholar] [CrossRef] [PubMed]
- Jinno, T.; Kawano, S.; Maruse, Y.; Matsubara, R.; Goto, Y.; Sakamoto, T.; Hashiguchi, Y.; Kaneko, N.; Tanaka, H.; Kitamura, R. Increased expression of interleukin-6 predicts poor response to chemoradiotherapy and unfavorable prognosis in oral squamous cell carcinoma. Oncol. Rep. 2015, 33, 2161–2168. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Kimura, T.; Ueta, E.; Tatemoto, Y.; Osaki, T. Characteristic cytokine generation patterns in cancer cells and infiltrating lymphocytes in oral squamous cell carcinomas and the influence of chemoradiation combined with immunotherapy on these patterns. Oncology 2003, 64, 407–415. [Google Scholar] [CrossRef]
- Petruzzi, M.N.; Cherubini, K.; Salum, F.G.; de Figueiredo, M.A. Role of tumour-associated macrophages in oral squamous cells carcinoma progression: An update on current knowledge. Diagn. Pathol. 2017, 12, 32. [Google Scholar] [CrossRef]
- Rossi, J.F.; Lu, Z.Y.; Jourdan, M.; Klein, B. Interleukin-6 as a therapeutic target. Clin. Cancer Res. 2015, 21, 1248–1257. [Google Scholar] [CrossRef]
| - | Patients (N = 95) | Controls (N = 80) | P | |
|---|---|---|---|---|
| Sex | Male | 60 (63%) | 30 (37%) | 0.004 * |
| Female | 35 (37%) | 50 (63%) | ||
| Age | (years; mean ± SD) | 61.7 ± 9.8 | 61.7 ± 9.2 | 0.982 ** |
| OSCC stage | ||||
| N = 70 | St I | 14 (20%) | – | na *** |
| St II | 22 (31%) | – | na *** | |
| St III | 13 (19%) | – | na*** | |
| St IV | 21 (30%) | – | na *** | |
| Histological grade | ||||
| N = 70 | G1 | 17 (24%) | – | na *** |
| G2 | 42 (60%) | – | na *** | |
| G3 | 11 (16%) | – | na *** | |
| DMFT | (N; mean ± SD) | 64; 27.6 ± 6.4 | 47; 24.8 ± 6.9 | 0.011 ** |
| GI | (N; mean ± SD) | 36; 0.53 ± 0.49 | 41; 0.42 ± 0.34 | 0.79 ** |
| Ethanol consumption | at least once a week | 46 (48%) | 14 (30%) | 0.035 * |
| less than once a week | 49 (52%) | 33 (70%) | ||
| Smoking | regular smoking | 62 (65%) | 8 (17%) | <0.001 * |
| non-smoker or occasional smoker | 33 (35%) | 40 (83%) |
| IL-6 mRNA Normalized Values | IL-6 Protein [pg/mL] | |||||||
|---|---|---|---|---|---|---|---|---|
| Sample | N | mean | SE | p * | N | mean | SE | p * |
| OSCC | ||||||||
| St I-II | 31 | 1.634 | 0.400 | <0.001 | 30 | 59.72 | 18.09 | <0.001 |
| St III-IV | 23 | 23.694 | 19.850 | <0.001 | 28 | 102.44 | 28.22 | <0.001 |
| G1 | 9 | 1.440 | 0.501 | <0.001 | 16 | 39.08 | 10.92 | 0.005 |
| G2 | 34 | 16.327 | 13.550 | <0.001 | 35 | 102.56 | 26.24 | <0.001 |
| G3 | 11 | 2.505 | 1.540 | <0.001 | 7 | 63.58 | 22.45 | 0.010 |
| Total | 74 | 3.301 | 0.885 | <0.001 | 74 | 70.98 | 14.06 | <0.001 |
| Control | 64 | 0.037 | 0.012 | 71 | 12.45 | 3.29 | ||
| In Transformed IL-6 mRNA | In Transformed IL-6 Protein | ||||
|---|---|---|---|---|---|
| Adjusted linear regression coefficient | p-value | Adjusted linear regression coefficient | p-value | ||
| Sex | female/male | −0.181 | 0.1 | −0.159 | 0.11 |
| Age | Year | 0.234 | 0.037 | 0.174 | 0.094 |
| DMFT | 0.234 | 0.037 | 0.174 | 0.094 | |
| Gingival index | 0.094 | 0.488 | 0.201 | 0.1 | |
| Alcohol consumption | |||||
| at least once a | |||||
| week/less than | 0.561 | 0.07 | −0.1 | 0.375 | |
| once a week | |||||
| Smoking | |||||
| regular smoking | |||||
| non-smoker or | −0.134 | 0.232 | 0.005 | 0.959 | |
| Occasional | |||||
| smoker | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Márton, I.J.; Horváth, J.; Lábiscsák, P.; Márkus, B.; Dezső, B.; Szabó, A.; Tar, I.; Piffkó, J.; Jakus, P.; Barabás, J.; et al. Salivary IL-6 mRNA is a Robust Biomarker in Oral Squamous Cell Carcinoma. J. Clin. Med. 2019, 8, 1958. https://doi.org/10.3390/jcm8111958
Márton IJ, Horváth J, Lábiscsák P, Márkus B, Dezső B, Szabó A, Tar I, Piffkó J, Jakus P, Barabás J, et al. Salivary IL-6 mRNA is a Robust Biomarker in Oral Squamous Cell Carcinoma. Journal of Clinical Medicine. 2019; 8(11):1958. https://doi.org/10.3390/jcm8111958
Chicago/Turabian StyleMárton, Ildikó Judit, József Horváth, Péter Lábiscsák, Bernadett Márkus, Balázs Dezső, Adrienn Szabó, Ildikó Tar, József Piffkó, Petra Jakus, József Barabás, and et al. 2019. "Salivary IL-6 mRNA is a Robust Biomarker in Oral Squamous Cell Carcinoma" Journal of Clinical Medicine 8, no. 11: 1958. https://doi.org/10.3390/jcm8111958
APA StyleMárton, I. J., Horváth, J., Lábiscsák, P., Márkus, B., Dezső, B., Szabó, A., Tar, I., Piffkó, J., Jakus, P., Barabás, J., Barabás, P., Olasz, L., Kövér, Z., Tőzsér, J., Sándor, J., Csősz, É., Scholtz, B., & Kiss, C. (2019). Salivary IL-6 mRNA is a Robust Biomarker in Oral Squamous Cell Carcinoma. Journal of Clinical Medicine, 8(11), 1958. https://doi.org/10.3390/jcm8111958









