A Longitudinal, Population-Level, Big-Data Study of Helicobacter pylori-Related Disease across Western Australia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Data
2.3. Methods
2.4. Data Availability
3. Results
3.1. Overview
3.2. Sex and UBT
3.3. Efficacy of Treatment and Gender Bias in Resistance
3.4. H. Pylori Related Disease in Aboriginal Australians
3.5. H. Pylori Related Disease in Non-Aboriginal Australians and People Born Overseas
3.6. Socio-Economic Indicators and H. pylori-Related Disease
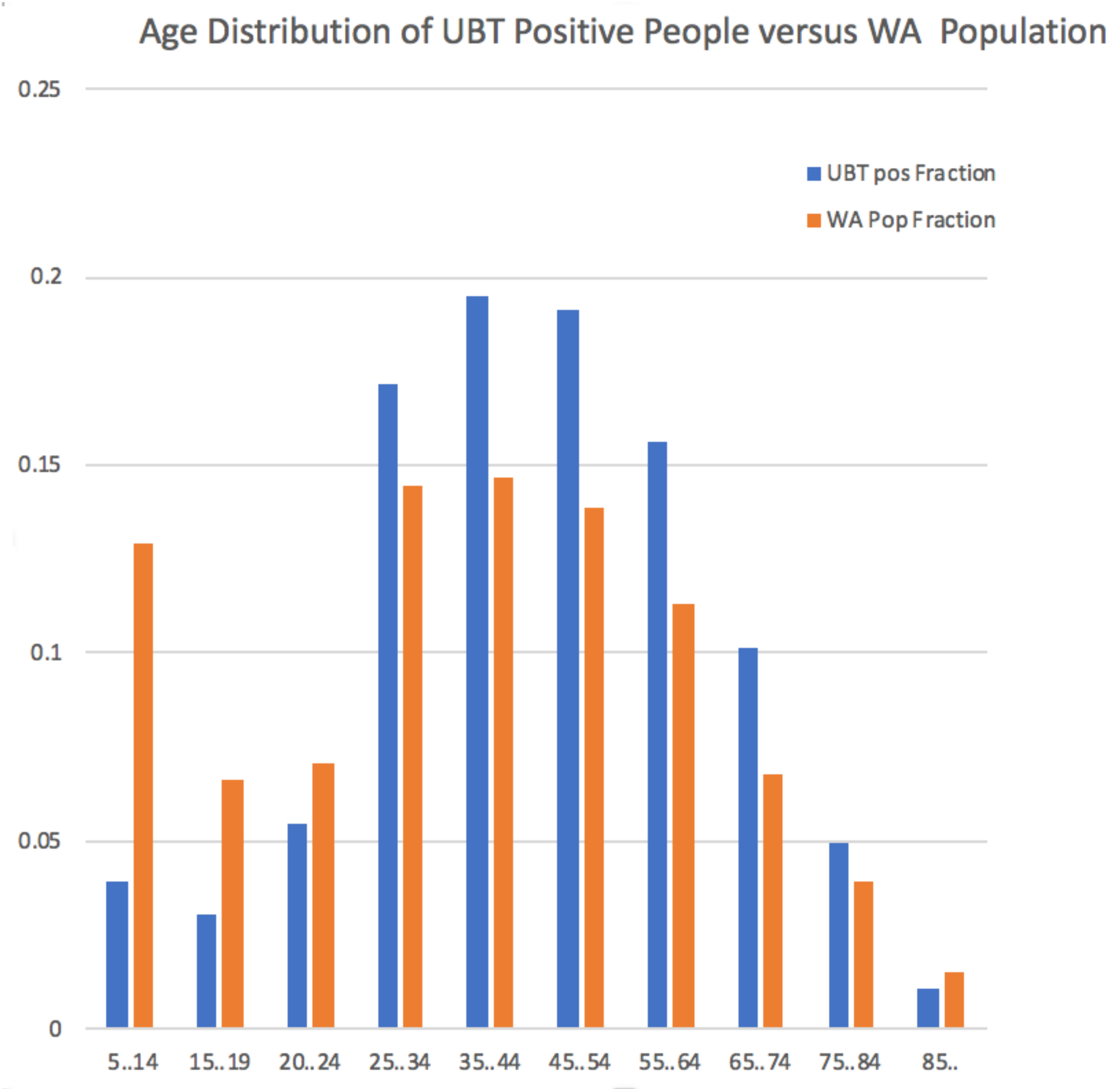
3.7. Age and UBT
4. Discussion
4.1. Limitations
4.2. Prevalence and Demographic Results
4.3. Sex Bias in H. pylori Disease
4.4. Efficacy of H. pylori Treatment and Bias in Treatment Failure
5. Conclusions
- H. pylori infection is largely seen as a solved problem. However, we were able to find groups within the community who are disproportionately affected by H. pylori-related disease, notably Aboriginal Australians and migrants to Australia. There are also some individuals in whom the infection is particularly refractory.
- While the number of people with borderline test results is small, the majority of people with an initial borderline test result did not have a follow-up UBT. As some of these are likely to have been positive, there is cause for concern.
- In both personal and health-economic terms [36], it is better to test and treat the infection, and thereby eliminate the disease [22]. This remains the case even for early stage gastric cancer [37]. The approach we have taken highlighted infection hotspots (seen in Supplementary Table S4). Similar analyses could help planners target education about test-and-treat to physicians and their patients.
- The open questions thrown up by this study are: Why is it that the first-line treatment fails significantly more often for H. pylori infection in women than in men, but why are men presenting with symptoms significantly earlier than women; are their symptoms worse?
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Blecker, U.; Lanciers, S.; Keppens, E.; Vandenplas, Y. Evolution of Helicobacter pylori Positivity in Infants Born from Positive Mothers. J. Pediatr. Gastr. Nutr. 1994, 19, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Rothenbacher, D.; Inceoglu, J.; Bode, G.; Brenner, H. Acquisition of Helicobacter pylori infection in a high-risk population occurs within the first 2 years of life. J. Pediatr. 2000, 136, 744–748. [Google Scholar] [CrossRef]
- Malaty, H.M.; El-Kasabany, A.; Graham, D.Y.; Miller, C.C.; Reddy, S.G.; Srinivasan, S.R.; Yamaoka, Y.; Berenson, G.S. Age at acquisition of Helicobacter pylori infection: A follow-up study from infancy to adulthood. Lancet 2002, 359, 931–935. [Google Scholar] [CrossRef]
- Rowland, M.; Daly, L.; Vaughan, M.; Higgins, A.; Bourke, B.; Drumm, B. Age-specific incidence of Helicobacter pylori. Gastroenterology 2006, 130, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.R. Unidentified Curved Bacilli on Gastric Epithelium in Active Chronic Gastritis. Lancet 1983, 321, 1273. [Google Scholar]
- Kusters, J.G.; van Vliet, A.H.; Kuipers, E.J. Pathogenesis of Helicobacter pylori infection. Clin. Microbiol. Rev. 2006, 19, 449–490. [Google Scholar] [CrossRef]
- Goh, K.L.; Chan, W.K.; Shiota, S.; Yamaoka, Y. Epidemiology of Helicobacter pylori infection and public health implications. Helicobacter 2011, 16, 1–9. [Google Scholar] [CrossRef]
- Eusebi, L.H.; Zagari, R.M.; Bazzoli, F. Epidemiology of Helicobacter pylori infection. Helicobacter 2014, 19, 1–5. [Google Scholar] [CrossRef]
- Peach, H.G.; Pearce, D.C.; Farish, S.J. Helicobacter pylori infection in an Australian regional city: Prevalence and risk factors. Med. J. Aust. 1997, 167, 310–313. [Google Scholar] [CrossRef]
- Moujaber, T.; MacIntyre, C.; Backhouse, J.; Gidding, H.; Quinn, H.; Gilbert, G. The seroepidemiology of Helicobacter pylori infection in Australia. Int. J. Infect. Dis. 2008, 12, 500–504. [Google Scholar] [CrossRef]
- Windsor, H.M.; Morrow, S.D.; Marshall, B.J.; Abioye-Kuteyi, E.A.; Leber, J.M.; Bulsara, M.K. Prevalence of Helicobacter pylori in Indigenous Western Australians: Comparison between urban and remote rural populations. Med. J. Aust. 2005, 182, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Hardikar, W.; Grimwood, K. Prevalence of Helicobacter pylori infection in asymptomatic children. J. Paediatr. Child Health 1995, 31, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Cherian, S.; Forbes, D.; Sanfilippo, F.; Cook, A.; Burgner, D. The epidemiology of Helicobacter pylori infection in African refugee children resettled in Australia. Med. J. Aust. 2008, 189, 438–441. [Google Scholar] [CrossRef] [PubMed]
- Ricci, C.; Holton, J.; Vaira, D. Diagnosis of Helicobacter pylori: Invasive and non-invasive tests. Best Pract. Res. Clin. Gastroenterol. 2007, 21, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.K.; Kuo, F.C.; Liu, C.J.; Wu, M.C.; Shih, H.Y.; Wang, S.S.; Wu, J.Y.; Kuo, C.H.; Huang, Y.K.; Wu, D.C. Diagnosis of Helicobacter pylori infection: Current options and developments. World J. Gastroenterol. 2015, 21, 11221. [Google Scholar] [CrossRef] [PubMed]
- Marshall, B.J.; Surveyor, I. Carbon-14 Urea Breath Test for the Diagnosis of Campylobacter Pylori Associated Gastritis. J. Nucl. Med. 1988, 29, 11–16. [Google Scholar] [PubMed]
- Ferwana, M.; Abdulmajeed, I.; Alhajiahmed, A.; Madani, W.; Firwana, B.; Hasan, R.; Altayar, O.; Limburg, P.J.; Murad, M.H.; Knawy, B. Accuracy of urea breath test in Helicobacter pylori infection: Meta-analysis. World J. Gastroenterol. 2015, 21, 1305. [Google Scholar] [CrossRef]
- Leide-Svegborn, S.; Stenström, K.; Olofsson, M.; Mattsson, S.; Nilsson, L.E.; Nosslin, B.; Pau, K.; Johansson, L.; Erlandsson, B.; Hellborg, R.; et al. Biokinetics and radiation doses for carbon-14 urea in adults and children undergoing the Helicobacter pylori breath test. Eur. J. Nucl. Med. 1999, 26, 573–580. [Google Scholar] [CrossRef]
- Bentur, Y.; Matsui, D.; Koren, G. Safety of 14C-UBT for diagnosis of Helicobacter pylori infection in pregnancy. Can. Fam. Phys. 2009, 55, 479–480. [Google Scholar]
- Graham, D.Y.; Klein, P.D.; Doyle, J.; Evans, J.; Evans, D.G.; Alpert, L.C.; Opekun, A.R.; Boutton, T.W. Campylobacter pylori Detected Noninvasively by the 13C-Urea Breath Test. Lancet 1987, 329, 1174–1177. [Google Scholar]
- Australian Bureau of Statistics. Data Packs for the 2011 Australian Census. 2011. Available online: http://www.abs.gov.au/websitedbs/censushome.nsf/home/datapacks?opendocument&navpos=250 (accessed on 14 February 2017).
- Malfertheiner, P.; Megraud, F.; O’Morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori Infection—The Maastricht V/Florence Consensus Report. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef] [PubMed]
- The pandas project. Python Data Analysis Library. 2019. Available online: https://pandas.pydata.org/ (accessed on 7 October 2019).
- Scipy.org. Scientific Computing Tools for Python (statistics functions). 2019. Available online: https://docs.scipy.org/doc/scipy/reference/stats.html (accessed on 7 October 2019).
- Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS). 2018. Available online: https://www.abs.gov.au/websitedbs/D3310114.nsf/home/Australian+Statistical+Geography+Standard+(ASGS) (accessed on 9 October 2018).
- Peura, D.A.; Pambianco, D.J.; Dye, K.R.; Lind, C.; Frierson, H.F.; Hoffman, S.R.; Combs, M.J.; Guilfoyle, E.; Marshall, B.J. Microdose 14C-Urea Breath Test offers Diagnosis of Helicobacter pylori in 10 Minutes. Am. J. Gastroenterol. 1996, 91, 233–238. [Google Scholar] [PubMed]
- Hooi, J.K.; Lai, W.Y.; Ng, W.K.; Suen, M.M.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.; Wu, J.C.; et al. Global prevalence of Helicobacter pylori infection: Systematic review and meta-analysis. Gastroenterology 2017, 153, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Tindberg, Y.; Bengtsson, C.; Granath, F.; Blennow, M.; Nyrén, O.; Granström, M. Helicobacter pylori Infection in Swedish School Children: Lack of Evidence of Child-to-Child Transmission Outside the Family. Gastroenterology 2001, 121, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.K.; Lambert, J.R.; Nicholson, L.; Lukito, W.; Wahlqvist, M. Prevalence of Helicobacter pylori in a Representative Anglo-Celtic Population of Urban Melbourne. J. Gastroen Hepatol. 1998, 13, 505–510. [Google Scholar] [CrossRef] [PubMed]
- EUROGAST Study Group. Epidemiology of, and Risk Factors for, Helicobacter pylori Infection among 3194 Asymptomatic Subjects in 17 Populations. Gut 1993, 34, 1672–1676. [Google Scholar] [CrossRef] [PubMed]
- Naja, F.; Kreiger, N.; Sullivan, T. Helicobacter Pylori Infection in Ontario: Prevalence and Risk Factors. Can. J. Gastroenterol. 2007, 21, 501–506. [Google Scholar] [CrossRef]
- Yu, X.; Yang, X.; Yang, T.; Dong, Q.; Wang, L.; Feng, L. Decreasing Prevalence of Helicobacter pylori According to Birth Cohorts in Urban China. Turk. J. Gastroenterol. 2017, 28, 94–97. [Google Scholar] [CrossRef]
- Chen, Z.; Thompson, S.K.; Jamieson, G.G.; Devitt, P.G.; Watson, D.I. Effect of Sex on Symptoms Associated with Gastroesophageal Reflux. Arch. Surg. 2011, 146, 1164–1169. [Google Scholar] [CrossRef]
- Mitchell, H.; Katelaris, P. Epidemiology, clinical impacts and current clinical management of Helicobacter pylori infection. Med. J. Aust. 2016, 204, 376–380. [Google Scholar] [CrossRef]
- Moayyedi, P.; Feltbower, R.; Crocombe, W.; Mason, S.; Atha, P.; Brown, J.; Dowell, A.; Richards, I.; Axon, A. The effectiveness of omeprazole, clarithromycin and tinidazole in eradicating Helicobacter pylori in a community screen and treat programme. Aliment Pharm. Ther. 2000, 14, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, F.Y.; Tsai, Y.W.; Wen, Y.W.; Kuo, K.N.; Tsai, C.R.; Huang, W.F. Effect of Helicobacter pylori Eradication Therapy on Risk of Hospitalization for a Major Ulcer Event. Pharmacotherapy 2011, 31, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.J.; Kook, M.C.; Kim, Y.I.; Cho, S.J.; Lee, J.Y.; Kim, C.G.; Park, B.; Nam, B.H. Helicobacter pylori Therapy for the Prevention of Metachronous Gastric Cancer. N. Engl. J. Med. 2018, 378, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wise, M.J.; Lamichhane, B.; Webberley, K.M. A Longitudinal, Population-Level, Big-Data Study of Helicobacter pylori-Related Disease across Western Australia. J. Clin. Med. 2019, 8, 1821. https://doi.org/10.3390/jcm8111821
Wise MJ, Lamichhane B, Webberley KM. A Longitudinal, Population-Level, Big-Data Study of Helicobacter pylori-Related Disease across Western Australia. Journal of Clinical Medicine. 2019; 8(11):1821. https://doi.org/10.3390/jcm8111821
Chicago/Turabian StyleWise, Michael J., Binit Lamichhane, and K. Mary Webberley. 2019. "A Longitudinal, Population-Level, Big-Data Study of Helicobacter pylori-Related Disease across Western Australia" Journal of Clinical Medicine 8, no. 11: 1821. https://doi.org/10.3390/jcm8111821
APA StyleWise, M. J., Lamichhane, B., & Webberley, K. M. (2019). A Longitudinal, Population-Level, Big-Data Study of Helicobacter pylori-Related Disease across Western Australia. Journal of Clinical Medicine, 8(11), 1821. https://doi.org/10.3390/jcm8111821




