Less Is More: Ulnar Lengthening Alone without Radial Corrective Osteotomy in Forearm Deformity Secondary to Hereditary Multiple Exostoses
Abstract
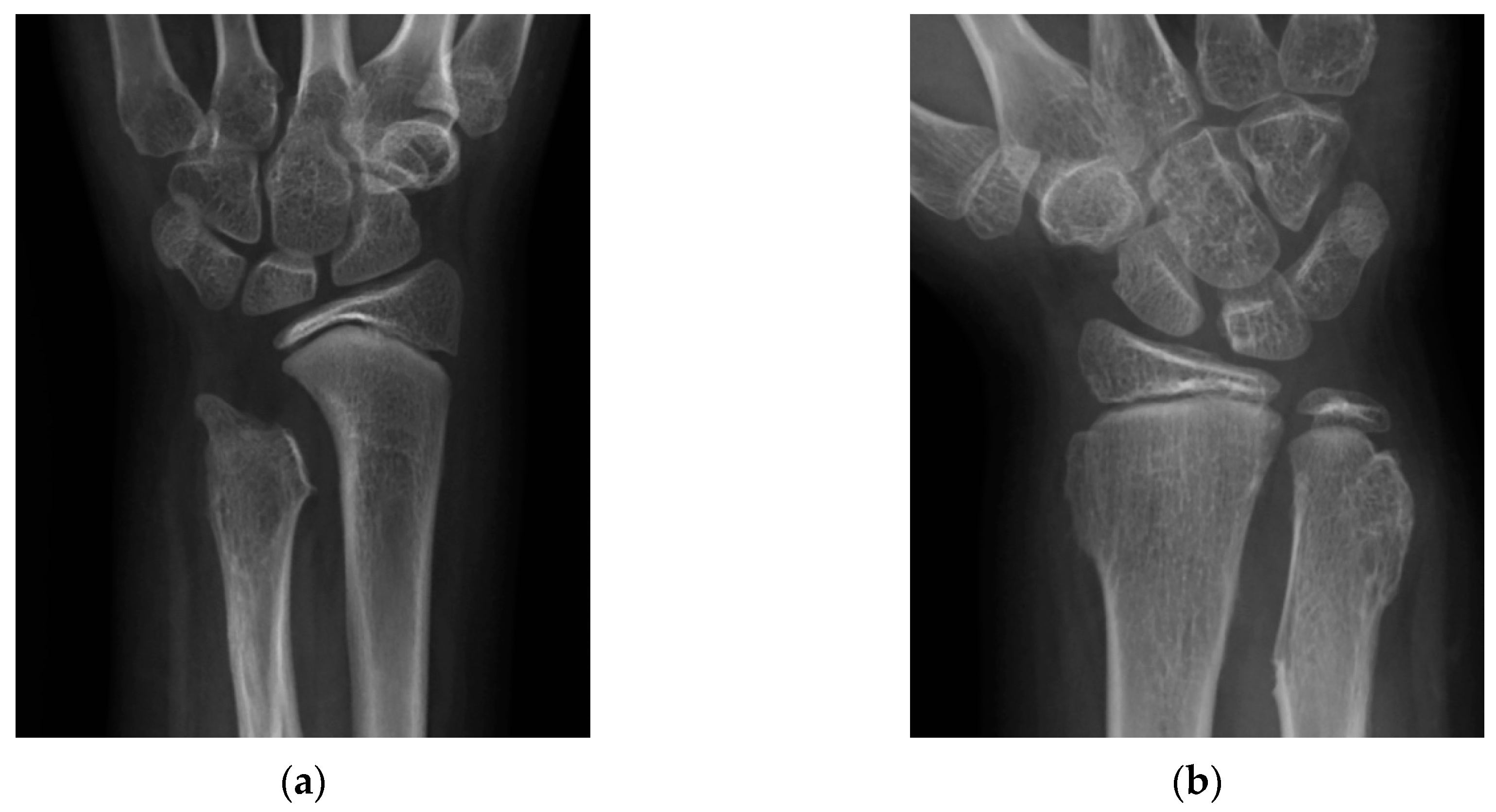
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Sandell, L.J. Multiple hereditary exostosis, EXT genes, and skeletal development. J. Bone Jt. Surg. Am. 2009, 91, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Chhina, H.; Davis, J.C.; Alvarez, C.M. Health-related quality of life in people with hereditary multiple exostoses. J. Pediatr. Orthop. 2012, 32, 210–214. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosi, R.; Ragone, V.; Caldarini, C.; Serra, N.; Usuelli, F.G.; Facchini, R.M. The impact of hereditary multiple exostoses on quality of life, satisfaction, global health status, and pain. Arch. Orthop. Trauma Surg. 2017, 137, 209–215. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosi, R.; Caldarini, C.; Ragone, V.; Facchini, R.M. Effect of multiple hereditary exostoses on sports activity in children. J. Orthop. 2018, 15, 927–930. [Google Scholar] [CrossRef]
- Schmale, G.A.; Conrad, E.U., 3rd; Raskind, W.H. The natural history of hereditary multiple exostoses. J. Bone Jt. Surg. Am. 1994, 76, 986–992. [Google Scholar] [CrossRef]
- Solomon, L. Bone growth in diaphysial aclasis. J. Bone Jt. Surg. Br. 1961, 43-B, 700–716. [Google Scholar] [CrossRef]
- Shin, E.K.; Jones, N.F.; Lawrence, J.F. Treatment of multiple hereditary osteochondromas of the forearm in children: A study of surgical procedures. J. Bone Jt. Surg. Br. 2006, 88, 255–260. [Google Scholar] [CrossRef]
- Rodgers, W.B.; Hall, J.E. One-bone forearm as a salvage procedure for recalcitrant forearm deformity in hereditary multiple exostoses. J. Pediatr. Orthop. 1993, 13, 587–591. [Google Scholar] [CrossRef]
- Kelly, J.P.; James, M.A. Radiographic Outcomes of Hemiepiphyseal Stapling for Distal Radius Deformity Due to Multiple Hereditary Exostoses. J. Pediatr. Orthop. 2016, 36, 42–47. [Google Scholar] [CrossRef]
- El-Sobky, T.A.; Samir, S.; Atiyya, A.N.; Mahmoud, S.; Aly, A.S.; Soliman, R. Current paediatric orthopaedic practice in hereditary multiple osteochondromas of the forearm: A systematic review. SICOT J. 2018, 4, 10. [Google Scholar] [CrossRef]
- Masada, K.; Tsuyuguchi, Y.; Kawai, H.; Kawabata, H.; Noguchi, K.; Ono, K. Operations for forearm deformity caused by multiple osteochondromas. J. Bone Jt. Surg. Br. 1989, 71, 24–29. [Google Scholar] [CrossRef]
- Nimityongskul, P.; Anderson, L.D.; Sri, P. Plastic deformation of the forearm: A review and case reports. J. Trauma 1991, 31, 1678–1685. [Google Scholar] [CrossRef] [PubMed]
- Tarmuzi, N.A.; Abdullah, S.; Osman, Z.; Das, S. Paediatric forearm fractures: Functional outcome of conservative treatment. Bratisl. Lek. Listy 2009, 110, 563–568. [Google Scholar] [PubMed]
- Fogel, G.R.; McElfresh, E.C.; Peterson, H.A.; Wicklund, P.T. Management of deformities of the forearm in multiple hereditary osteochondromas. J. Bone Jt. Surg. Am. 1984, 66, 670–680. [Google Scholar] [CrossRef]
- Tang, Z.W.; Cao, Y.L.; Liu, T.; Chen, T.; Zhang, X.S. Management of forearm deformities with ulnar shortening more than 15 mm caused by hereditary multiple osteochondromas. Eur. J. Orthop. Surg. Traumatol. 2013, 23, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Vogt, B.; Tretow, H.L.; Daniilidis, K.; Wacker, S.; Buller, T.C.; Henrichs, M.P.; Roedl, R.W.; Schiedel, F. Reconstruction of forearm deformity by distraction osteogenesis in children with relative shortening of the ulna due to multiple cartilaginous exostosis. J. Pediatr. Orthop. 2011, 31, 393–401. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosi, R.; Barbato, A.; Caldarini, C.; Biancardi, E.; Facchini, R.M. Gradual ulnar lengthening in children with multiple exostoses and radial head dislocation: Results at skeletal maturity. J. Child. Orthop. 2016, 10, 127–133. [Google Scholar] [CrossRef]
- Abe, M.; Shirai, H.; Okamoto, M.; Onomura, T. Lengthening of the forearm by callus distraction. J. Hand Surg. Br. 1996, 21, 151–163. [Google Scholar] [CrossRef]
- Ham, J.; Flipsen, M.; Koolen, M.; van der Zwan, A.; Mader, K. Multiple osteochondromas (MO) in the forearm: A 12-year single-centre experience. Strateg. Trauma Limb Reconstr. 2016, 11, 169–175. [Google Scholar] [CrossRef]
- Pritchett, J.W. Lengthening the ulna in patients with hereditary multiple exostoses. J. Bone Jt. Surg. Br. 1986, 68, 561–565. [Google Scholar] [CrossRef]
- Jo, A.R.; Jung, S.T.; Kim, M.S.; Oh, C.S.; Min, B.J. An Evaluation of Forearm Deformities in Hereditary Multiple Exostoses: Factors Associated with Radial Head Dislocation and Comprehensive Classification. J. Hand Surg. Am. 2017, 42, 292.e1–292.e8. [Google Scholar] [CrossRef] [PubMed]
- Stanton, R.P.; Hansen, M.O. Function of the upper extremities in hereditary multiple exostoses. J. Bone Jt. Surg. Am. 1996, 78, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Refsland, S.; Kozin, S.H.; Zlotolow, D.A. Ulnar Distraction Osteogenesis in the Treatment of Forearm Deformities in Children with Multiple Hereditary Exostoses. J. Hand Surg. Am. 2016, 41, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, H.; Tsuchiya, H.; Sakurakichi, K.; Yamashiro, T.; Watanabe, K.; Tomita, K. Correction and lengthening for deformities of the forearm in multiple cartilaginous exostoses. J. Orthop. Sci. 2006, 11, 459–466. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cho, Y.J.; Jung, S.T. Gradual lengthening of the ulna in patients with multiple hereditary exostoses with a dislocated radial head. Yonsei Med. J. 2014, 55, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Morrey, B.F.; Askew, L.J.; Chao, E.Y. A biomechanical study of normal functional elbow motion. J. Bone Jt. Surg. Am. 1981, 63, 872–877. [Google Scholar] [CrossRef]
- Demir, B.; Gursu, S.; Ozturk, K.; Yildirim, T.; Konya, M.N.; Er, T. Single-stage treatment of complete dislocation of radial head and forearm deformity using distraction osteogenesis in paediatric patients having multiple cartilaginous exostosis. Arch. Orthop. Trauma Surg. 2011, 131, 1195–1201. [Google Scholar] [CrossRef]
- Tonogai, I.; Takahashi, M.; Tsutsui, T.; Goto, T.; Hamada, D.; Suzue, N.; Matsuura, T.; Yasui, N.; Sairyo, K. Forearm lengthening by distraction osteogenesis: A report on 5 limbs in 3 cases. J. Med. Investig. 2015, 62, 219–222. [Google Scholar] [CrossRef][Green Version]
| The Senior Group (n = 6) with Radial Correction | The Junior Group (n = 8) without Radial Correction | p Value | |
|---|---|---|---|
| Age (year) | 16.7 ± 4.4 | 8.1 ± 2.5 | <0.01 |
| Gender (Female/Male) | 1/5 | 4/4 | 0.30 |
| Side (Right/Left) | 5/1 | 5/3 | 0.58 |
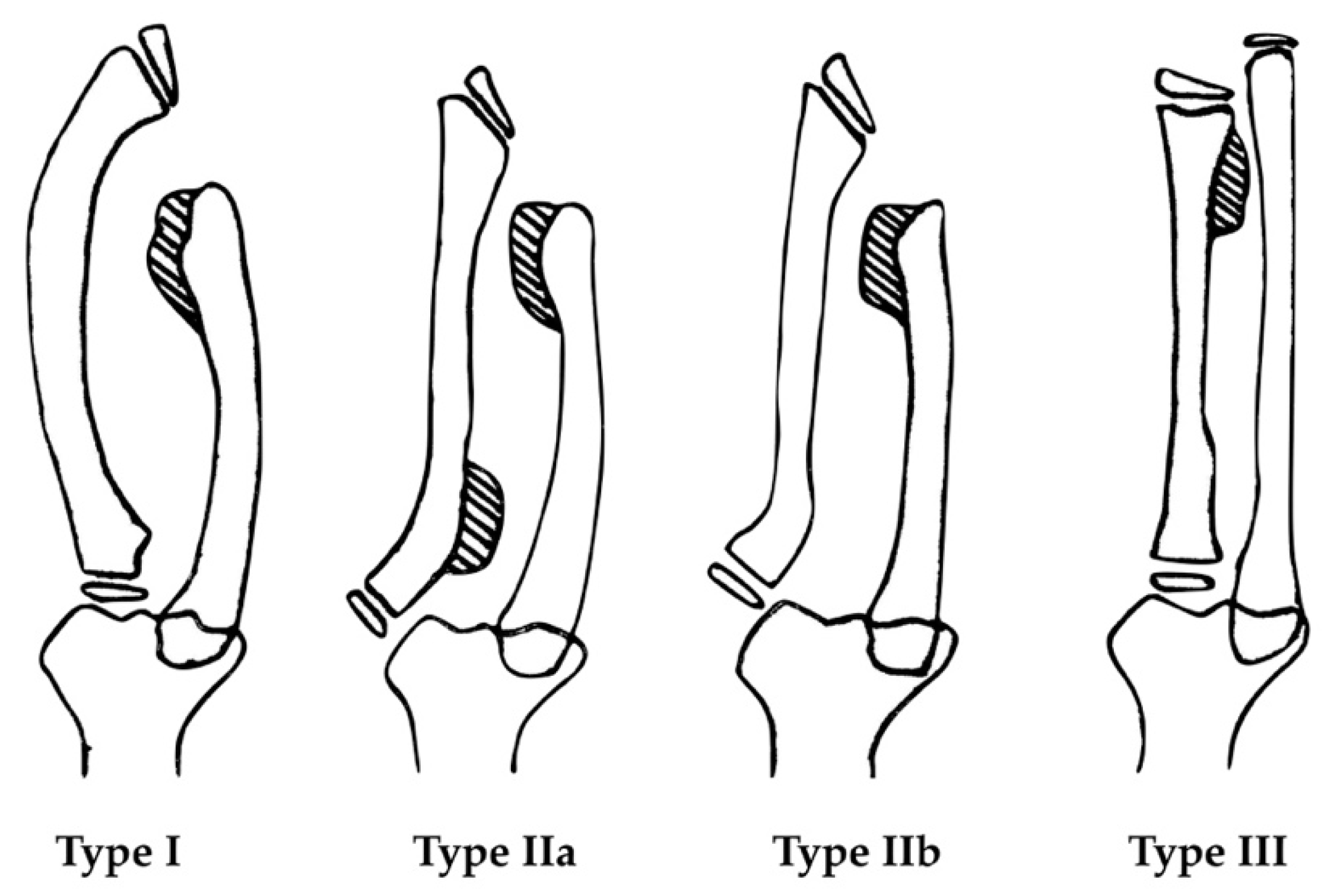
| Masada Classification | |||
| Type I | 4 | 7 | |
| Type IIa | 1 | 0 | |
| Type IIb | 1 | 1 | |
| Elongated length (mm) | 21.3 ± 5.8 | 22.5 ± 2.4 | 0.43 |
| EFT (day) | 204.3 ± 63.7 | 159.0 ± 38.8 | 0.14 |
| EFI (day/cm) | 104.9 ± 53.6 | 72.0 ± 20.0 | 0.20 |
| Follow-up (month) | 38.7 ± 22 | 51.4 ± 18.6 | 0.12 |
| The Senior Group (n = 6) | The Junior Group (n = 8) | p Value | |
|---|---|---|---|
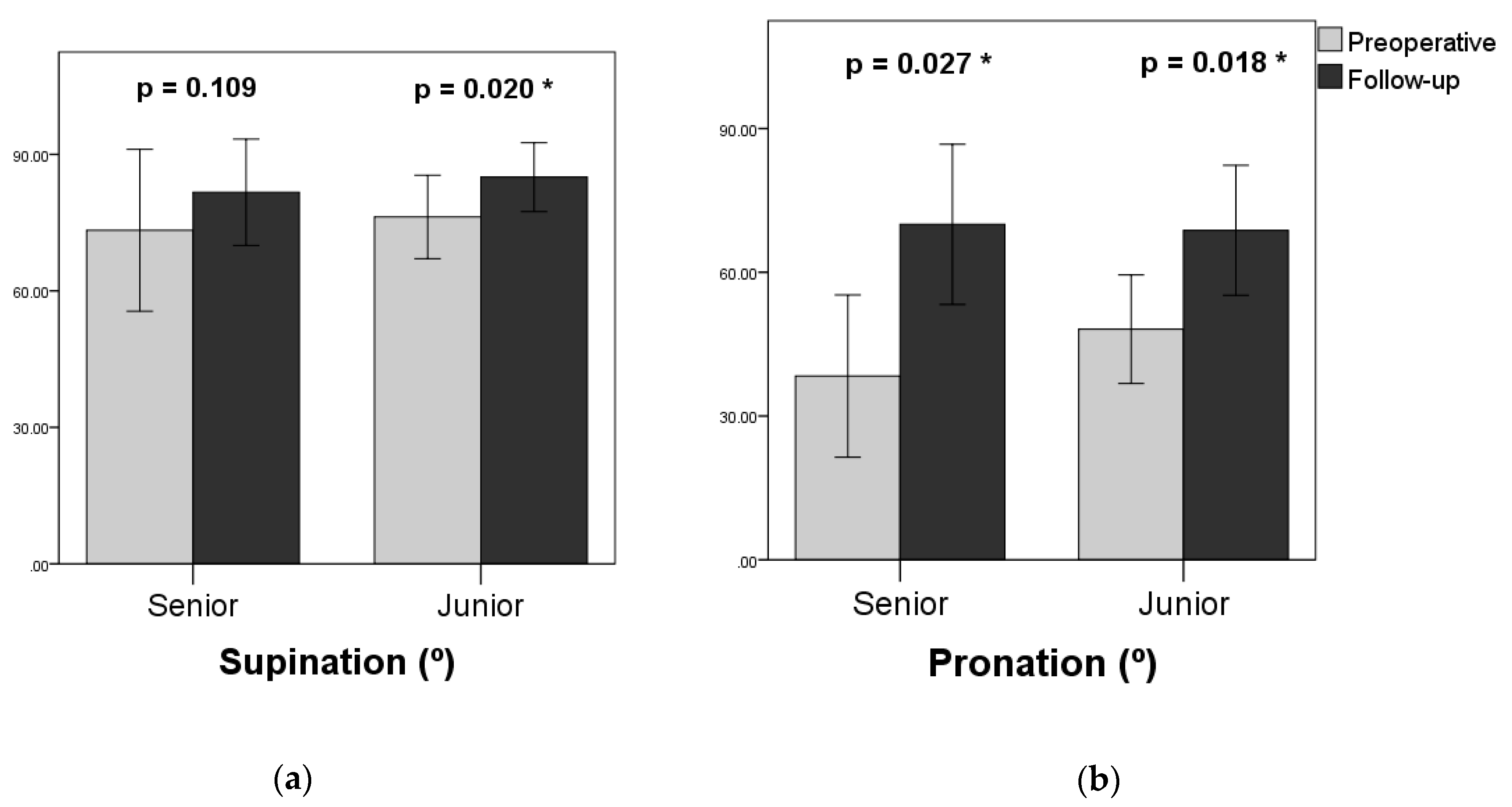
| Supination | |||
| Preoperative | 73.3° ± 16.2° | 76.3° ± 8.6° | 0.95 |
| Follow-up | 81.7° ± 10.7° | 85.0° ± 7.1° | 0.61 |
| Gained | 8.3° ± 11.1° | 8.8° ± 6.0° | 0.59 |
| Pronation | |||
| Preoperative | 38.3° ± 15.5° | 48.1° ± 10.6° | 0.29 |
| Follow-up | 70.0° ± 15.3° | 68.8° ± 12.7° | 0.89 |
| Gained | 31.7° ± 17.5° | 20.6° ± 14.2° | 0.30 |
| The Senior Group (n = 6) | The Junior Group (n = 8) | p Value | |
|---|---|---|---|
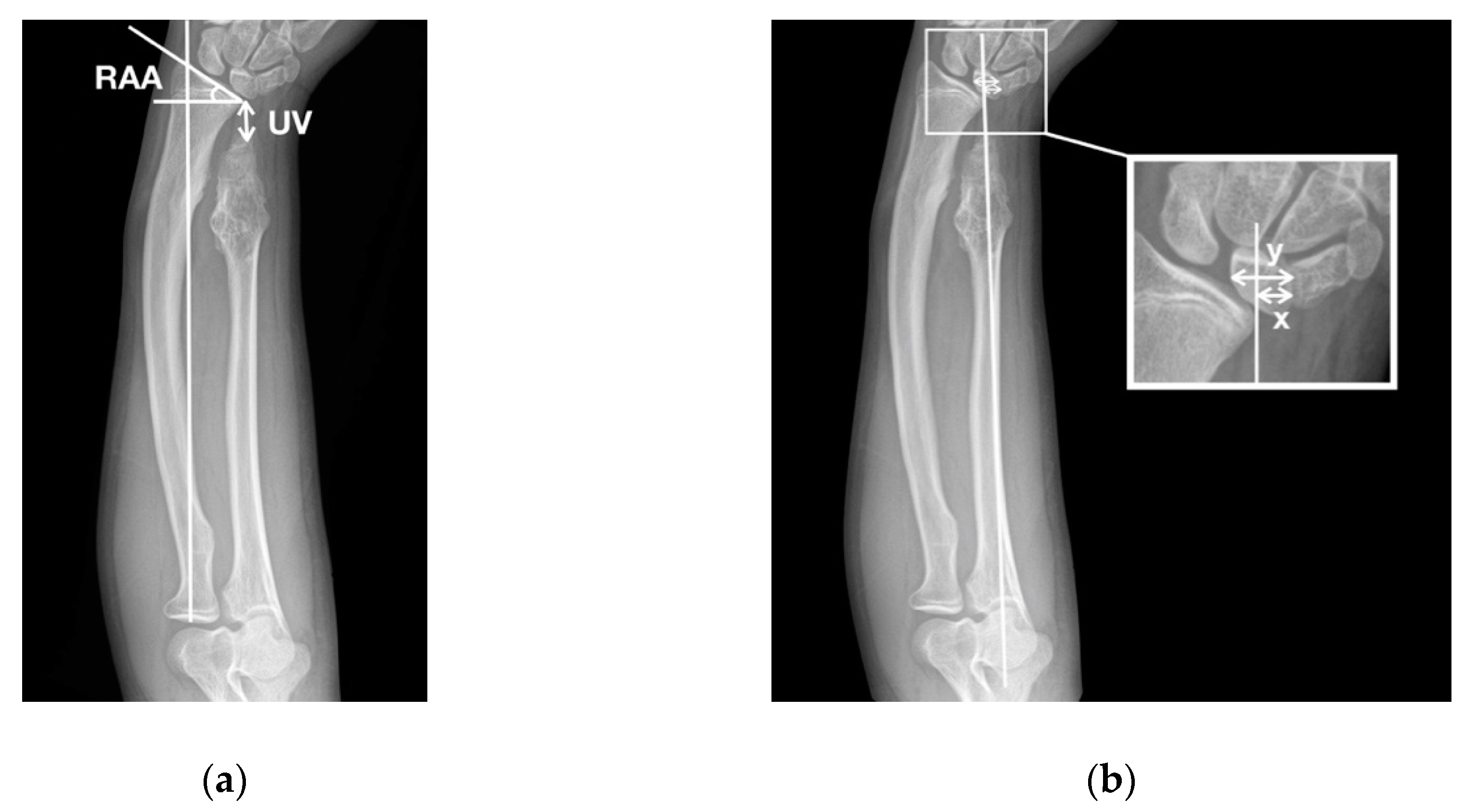
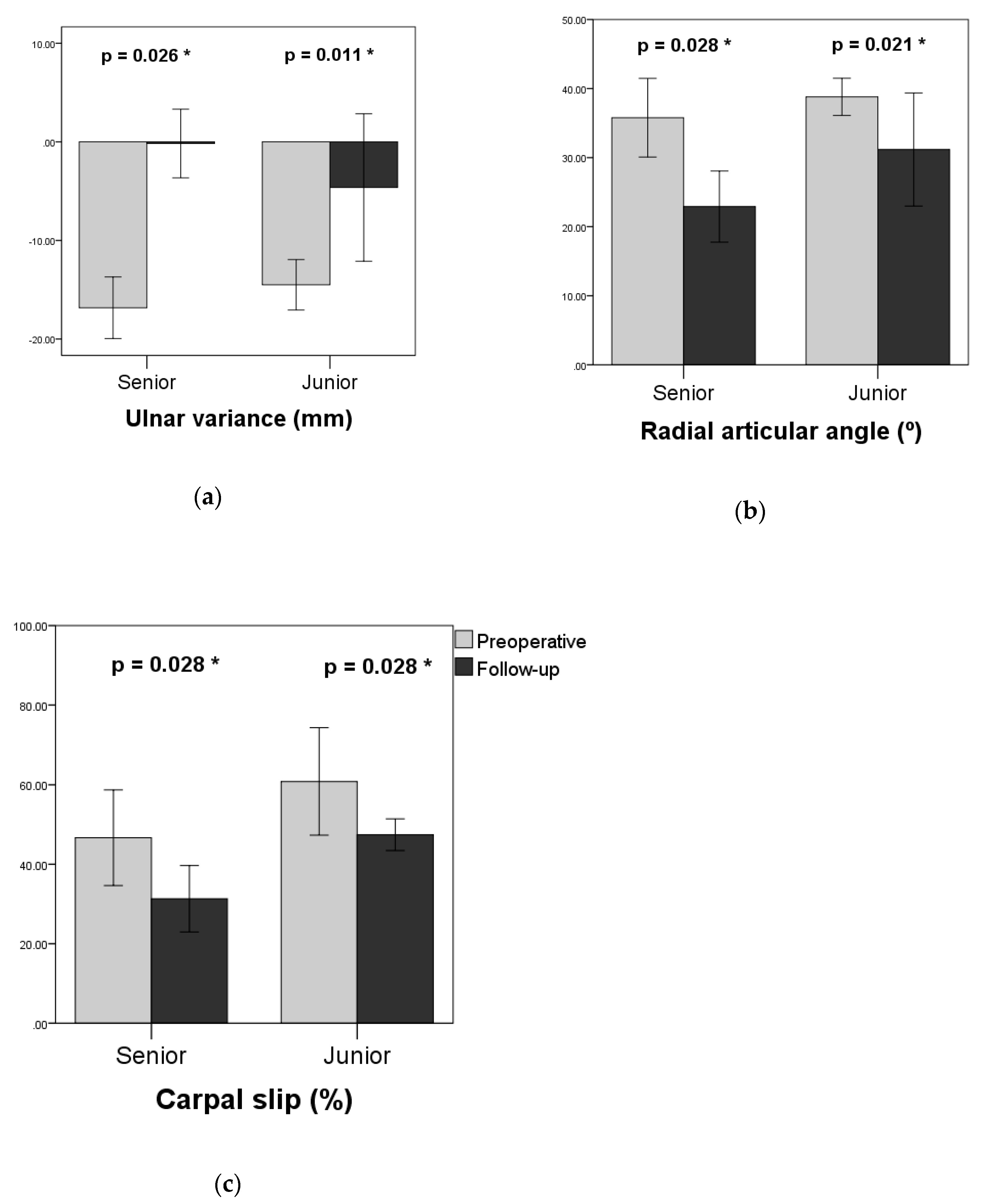
| UV (mm) | |||
| Preoperative | −16.8 ± 2.9 | −14.5 ± 2.4 | 0.11 |
| Follow-up | −0.2 ± 3.2 | −4.6 ± 7.0 | 0.32 |
| RAA (°) | |||
| Preoperative | 35.8 ± 5.2 | 38.8 ± 2.5 | 0.44 |
| Follow-up | 22.9 ± 4.7 | 31.2 ± 7.7 | 0.07 |
| CS (%) | |||
| Preoperative | 46.7 ± 11.0 | 60.8 ± 12.3 | 0.11 |
| Follow-up | 31.3 ± 7.6 | 47.4 ± 3.6 | 0.01 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, P.-J.; Wu, K.-W.; Lee, C.-C.; Kuo, K.N.; Chang, J.-F.; Wang, T.-M. Less Is More: Ulnar Lengthening Alone without Radial Corrective Osteotomy in Forearm Deformity Secondary to Hereditary Multiple Exostoses. J. Clin. Med. 2019, 8, 1765. https://doi.org/10.3390/jcm8111765
Hsu P-J, Wu K-W, Lee C-C, Kuo KN, Chang J-F, Wang T-M. Less Is More: Ulnar Lengthening Alone without Radial Corrective Osteotomy in Forearm Deformity Secondary to Hereditary Multiple Exostoses. Journal of Clinical Medicine. 2019; 8(11):1765. https://doi.org/10.3390/jcm8111765
Chicago/Turabian StyleHsu, Po-Jen, Kuan-Wen Wu, Chia-Che Lee, Ken N. Kuo, Jia-Feng Chang, and Ting-Ming Wang. 2019. "Less Is More: Ulnar Lengthening Alone without Radial Corrective Osteotomy in Forearm Deformity Secondary to Hereditary Multiple Exostoses" Journal of Clinical Medicine 8, no. 11: 1765. https://doi.org/10.3390/jcm8111765
APA StyleHsu, P.-J., Wu, K.-W., Lee, C.-C., Kuo, K. N., Chang, J.-F., & Wang, T.-M. (2019). Less Is More: Ulnar Lengthening Alone without Radial Corrective Osteotomy in Forearm Deformity Secondary to Hereditary Multiple Exostoses. Journal of Clinical Medicine, 8(11), 1765. https://doi.org/10.3390/jcm8111765






