Pre-, Intra-, and Post-Operative Evaluation of Extraocular Muscle Insertions Using Optical Coherence Tomography: A Comparison of Four Devices
Abstract
1. Introduction
2. Experimental Section
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Leffler, C.T.; Vaziri, K.; Schwartz, S.G.; Cavuoto, K.M.; McKeown, C.A.; Kishor, K.S.; Janot, A.C. Rates of Reoperation and Abnormal Binocularity Following Strabismus Surgery in Children. Am. J. Ophthalmol. 2016, 162, 159.e9–166.e9. [Google Scholar] [CrossRef] [PubMed]
- Demer, J.L.; Clark, R.A.; Kono, R.; Wright, W.; Velez, F.; Rosenbaum, A.L. A 12-year, prospective study of extraocular muscle imaging in complex strabismus. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2002, 6, 337–347. [Google Scholar] [CrossRef]
- Ettl, A.; Kramer, J.; Daxer, A.; Koornneef, L. High-resolution magnetic resonance imaging of the normal extraocular musculature. Eye 1997, 11, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Demer, J.L.; Ortube, M.C.; Engle, E.C.; Thacker, N. High-resolution magnetic resonance imaging demonstrates abnormalities of motor nerves and extraocular muscles in patients with neuropathic strabismus. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2006, 10, 135–142. [Google Scholar] [CrossRef][Green Version]
- Demer, J.L.; Dushyanth, A. T2-weighted fast spin-echo magnetic resonance imaging of extraocular muscles. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2011, 15, 17–23. [Google Scholar] [CrossRef]
- Tamburrelli, C.; Salgarello, T.; Vaiano, A.S.; Scullica, L.; Palombi, M.; Bagolini, B. Ultrasound of the horizontal rectus muscle insertion sites: Implications in preoperative assessment of strabismus. Investig. Ophthalmol. Vis. Sci. 2003, 44, 618–622. [Google Scholar] [CrossRef]
- Sacca, S.; Polizzi, A.; Macri, A.; Patrone, G.; Rolando, M. Echographic study of extraocular muscle thickness in children and adults. Eye 2000, 14 Pt 5, 765–769. [Google Scholar] [CrossRef]
- Khan, H.A.; Smith, D.R.; Kraft, S.P. Localising rectus muscle insertions using high frequency wide-field ultrasound biomicroscopy. Br. J. Ophthalmol. 2012, 96, 683–687. [Google Scholar] [CrossRef]
- Watts, P.; Smith, D.; Mackeen, L.; Kraft, S.; Buncic, J.R.; Abdolell, M. Evaluation of the ultrasound biomicroscope in strabismus surgery. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2002, 6, 187–190. [Google Scholar] [CrossRef]
- Dai, S.; Kraft, S.P.; Smith, D.R.; Buncic, J.R. Ultrasound biomicroscopy in strabismus reoperations. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2006, 10, 202–205. [Google Scholar] [CrossRef]
- Solarte, C.E.; Smith, D.R.; Buncic, J.R.; Tehrani, N.N.; Kraft, S.P. Evaluation of vertical rectus muscles using ultrasound biomicroscopy. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2008, 12, 128–131. [Google Scholar] [CrossRef]
- Takkar, B.; Sharma, P.; Singh, A.K.; Sahay, P. Anterior segment optical coherence tomography for identifying muscle status in strabismus surgery. Int. J. Ophthalmol. 2016, 9, 933–934. [Google Scholar] [CrossRef] [PubMed]
- Ngo, C.S.; Smith, D.; Kraft, S.P. The accuracy of anterior segment optical coherence tomography (AS-OCT) in localizing extraocular rectus muscles insertions. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2015, 19, 233–236. [Google Scholar] [CrossRef] [PubMed]
- Pihlblad, M.S.; Erenler, F.; Sharma, A.; Manchandia, A.; Reynolds, J.D. Anterior Segment Optical Coherence Tomography of the Horizontal and Vertical Extraocular Muscles With Measurement of the Insertion to Limbus Distance. J. Pediatric Ophthalmol. Strabismus 2016, 53, 141–145. [Google Scholar] [CrossRef]
- Liu, X.; Wang, F.; Xiao, Y.; Ye, X.; Hou, L. Measurement of the limbus-insertion distance in adult strabismus patients with anterior segment optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2011, 52, 8370–8373. [Google Scholar] [CrossRef]
- Park, K.A.; Lee, J.Y.; Oh, S.Y. Reproducibility of horizontal extraocular muscle insertion distance in anterior segment optical coherence tomography and the effect of head position. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2014, 18, 15–20. [Google Scholar] [CrossRef]
- Salcedo-Villanueva, G.; Paciuc-Beja, M.; Harasawa, M.; Velez-Montoya, R.; Olson, J.L.; Oliver, S.C.; Mandava, N.; Quiroz-Mercado, H. Identification and biometry of horizontal extraocular muscle tendons using optical coherence tomography. Graefe’s Arch. Clin. Exp. Ophthalmol. 2015, 253, 477–485. [Google Scholar] [CrossRef]
- Haner, N.U.; Dysli, M.; Abegg, M.; Zinkernagel, M.S. Enhanced-depth optical coherence tomography for imaging horizontal rectus muscles in Graves’ orbitopathy. Graefe’s Arch. Clin. Exp. Ophthalmol. 2015, 253, 1569–1573. [Google Scholar] [CrossRef][Green Version]
- Radhakrishnan, S.; Rollins, A.M.; Roth, J.E.; Yazdanfar, S.; Westphal, V.; Bardenstein, D.S.; Izatt, J.A. Real-time optical coherence tomography of the anterior segment at 1310 nm. Arch. Ophthalmol. 2001, 119, 1179–1185. [Google Scholar] [CrossRef]
- De-Pablo-Gomez-de-Liano, L.; Fernandez-Vigo, J.I.; Ventura-Abreu, N.; Morales-Fernandez, L.; Fernandez-Perez, C.; Garcia-Feijoo, J.; Gomez-de-Liano, R. Spectral domain optical coherence tomography to assess the insertion of extraocular rectus muscles. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2016, 20, 201–205. [Google Scholar] [CrossRef]
- Pihlblad, M.S.; Reynolds, J.D. Anterior Segment Optical Coherence Tomography of Previously Operated Extraocular Muscles. Am. Orthopt. J. 2017, 67, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Ocak, O.B.; Inal, A.; Yilmaz, I.; Aygit, E.D.; Ocak, S.Y.; Celik, S.; Taskapili, M.; Gokyigit, B. Measurement of extraocular horizontal muscle insertion distance via anterior segment optical coherence tomography of healthy children and comparison with healthy adults. Int. Ophthalmol. 2019, 39, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- De-Pablo-Gomez-de-Liano, L.; Fernandez-Vigo, J.I.; Ventura-Abreu, N.; Troyano-Rivas, J.; Nino-Rueda, C.; Romo-Lopez, A.; Gomez-de-Liano, R. Optical Coherence Tomography Thickness Measurements of the Extraocular Rectus Muscle Tendons in Graves’ Ophthalmopathy. J. Pediatric Ophthalmol. Strabismus 2018, 55, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Han, J.Y.; Lee, D.C.; Lee, S.Y. Horizontal Extraocular Muscle and Scleral Anatomy in Children: A Swept-Source Anterior Segment Optical Coherence Tomography Study. Korean J. Ophthalmol. 2018, 32, 83–88. [Google Scholar] [CrossRef]
- Venincasa, M.J.; Osigian, C.J.; Cavuoto, K.M.; Rossetto, J.D.; Capo, H. Combination of anterior segment optical coherence tomography modalities to improve accuracy of rectus muscle insertion location. J. Aapos Off. Publ. Am. Assoc. Pediatric Ophthalmol. Strabismus 2017, 21, 243–246. [Google Scholar] [CrossRef]
- Lee, J.Y.; Park, K.A.; Lyu, I.J.; Oh, S.Y. Postoperative change in lateral rectus muscle insertion measured by anterior segment optical coherence tomography. Eye 2017, 31, 1556–1561. [Google Scholar] [CrossRef]
- Rossetto, J.D.; Cavuoto, K.M.; Allemann, N.; McKeown, C.A.; Capo, H. Accuracy of Optical Coherence Tomography Measurements of Rectus Muscle Insertions in Adult Patients Undergoing Strabismus Surgery. Am. J. Ophthalmol. 2017, 176, 236–243. [Google Scholar] [CrossRef]
- De-Pablo-Gomez-de-Liano, L.; Fernandez-Vigo, J.I.; Ventura-Abreu, N.; Garcia-Feijoo, J.; Fernandez-Vigo, J.A.; Gomez-de-Liano, R. Agreement Between Three Optical Coherence Tomography Devices to Assess the Insertion Distance and Thickness of Horizontal Rectus Muscles. J. Pediatric Ophthalmol. Strabismus 2017, 54, 168–176. [Google Scholar] [CrossRef]
- De-Pablo-Gomez-de-Liano, L.; Fernandez-Vigo, J.I.; Ventura-Abreu, N.; Morales-Fernandez, L.; Garcia-Feijoo, J.; Gomez-de-Liano, R. Agreement between intraoperative measurements and optical coherence tomography of the limbus-insertion distance of the extraocular muscles. Arch. De La Soc. Esp. De Oftalmol. 2016, 91, 567–572. [Google Scholar] [CrossRef]


| Bioptigen | Rescan | Spectralis | Visante | |
|---|---|---|---|---|
| Able to image muscle insertion | 24/34 (71%) | 25/28 (89%) | 22/38 (58%) | 31/40 (78%) |
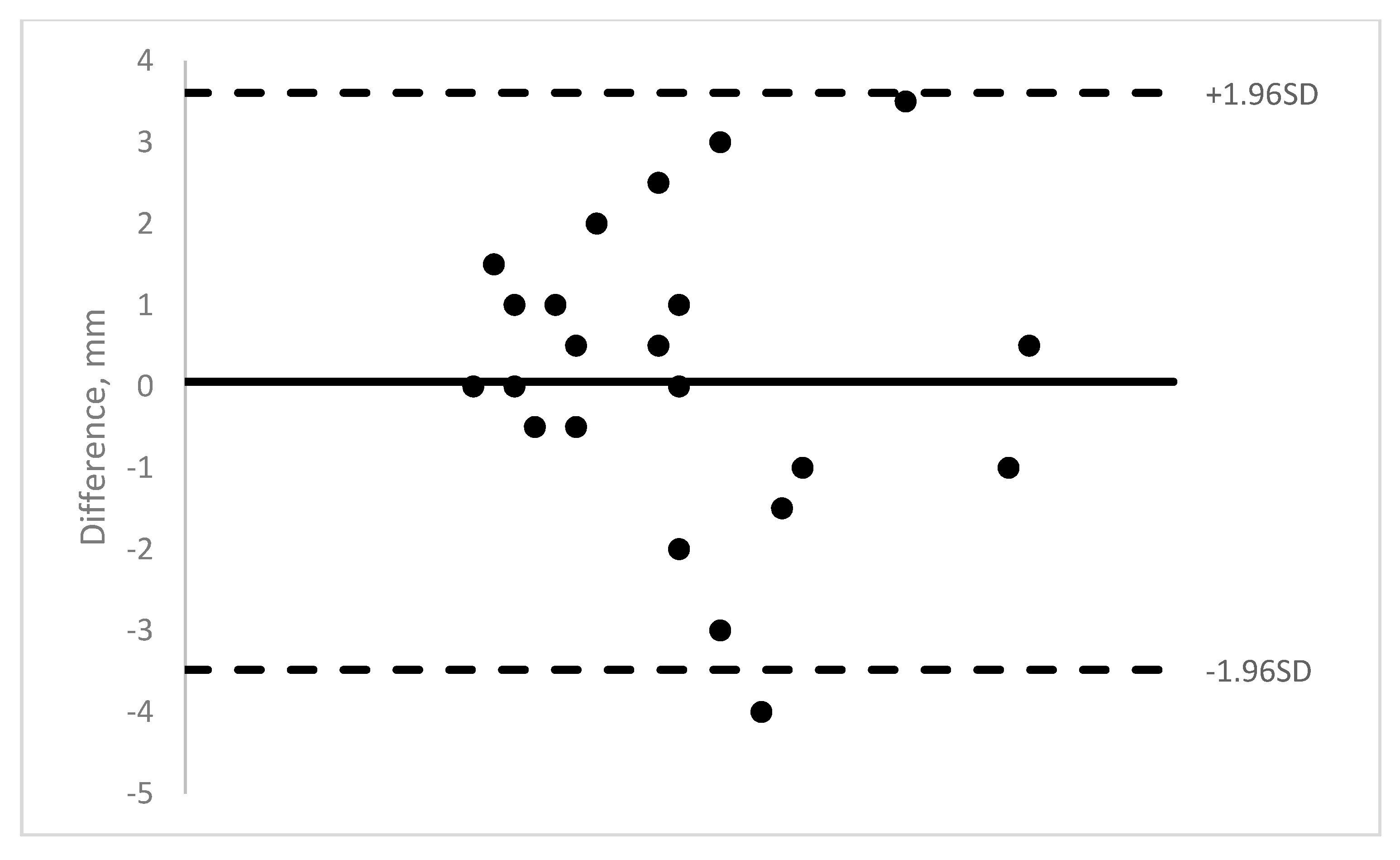
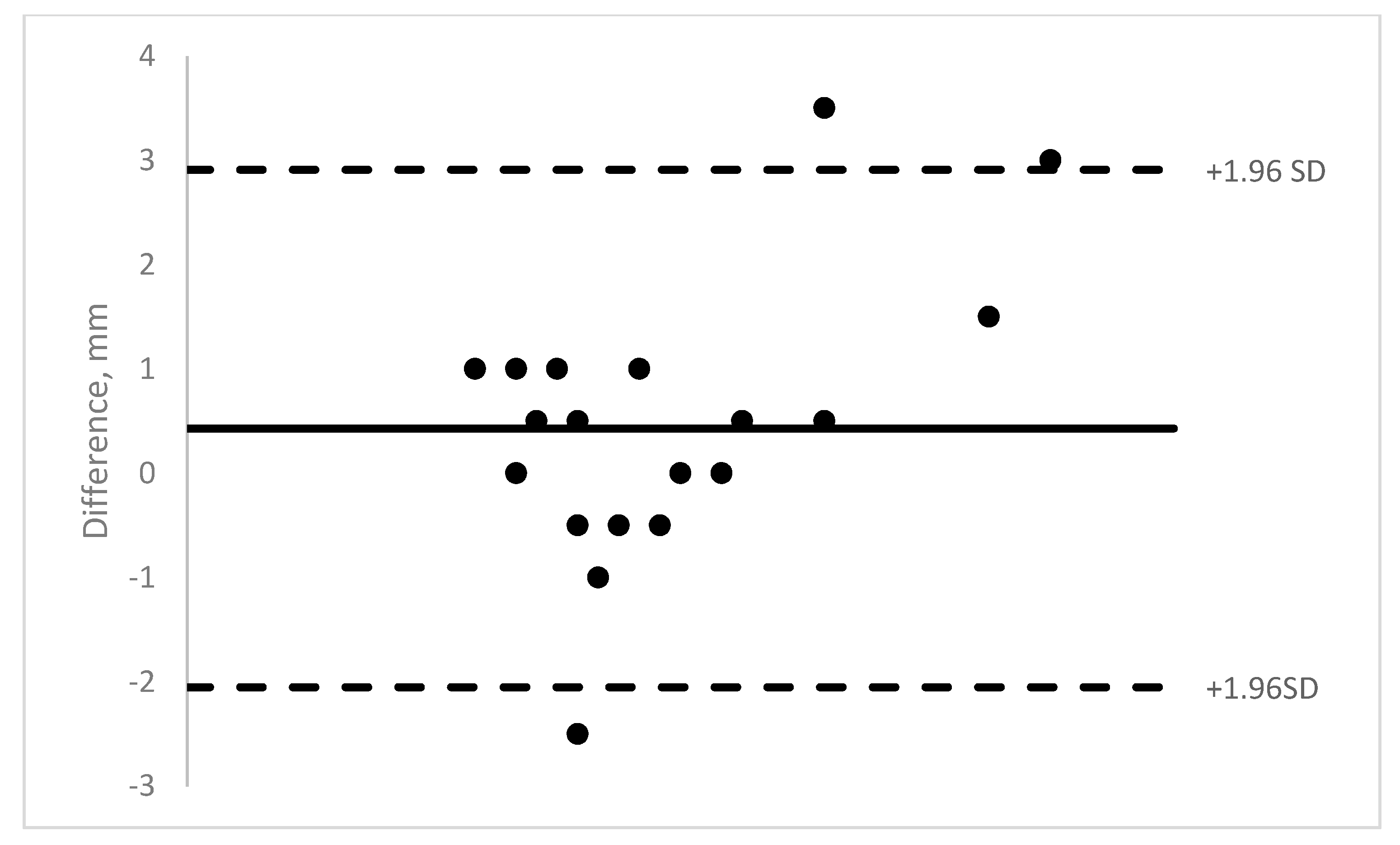
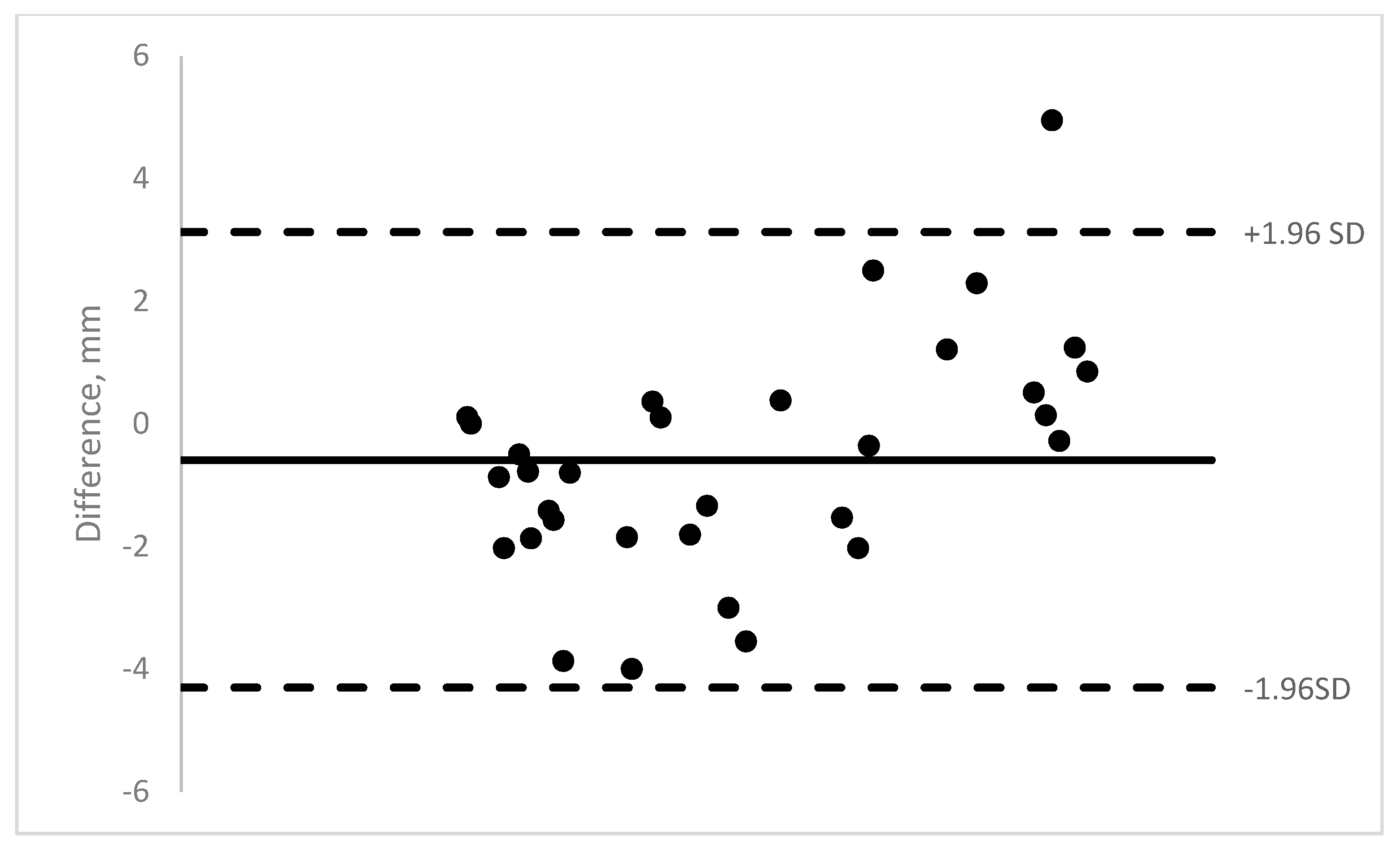
| Mean difference between OCT measurement and caliper (SD) | 0.06 mm (1.81) range −4.0 to +3.5 | 0.43 mm (1.27) range −2.5 to +3.5 | 0.47 mm (1.54) range −3.7 to +4.3 | −0.56 mm (1.9) range −4.0 to +5.0 |
| Intraclass correlation coefficient (ICC) | 0.62 | 0.83 | 0.85 | 0.88 |
| p-value | <0.01 | <0.001 | <0.001 | <0.001 |
| ≤1 mm | 13/24 (54%) | 21/25 (84%) | 15/22 (68%) | 13/31 (42%) |
| ≤2 mm | 18/24 (75%) | 21/25 (84%) | 20/22 (91%) | 22/31 (71%) |
| Pre-op or before surgery on unoperated muscles: ≤1 mm | 10/29 (34%) | 19/24 (79%) | 8/9 (89%) | 5/11 (45%) |
| Post-op: ≤1 mm | a | a | 7/13 (54%) | 5/16 (31%) |
| Muscles imaged with all four machines (% ≤ 1 mm) | 37.5% (3/8) | 75% (6/8) | 62.5% (5/8) | 37.5% (3/8) |
| Patients | Intra-Op Measurment | Bioptigen | Rescan | Spectralis | Visante |
|---|---|---|---|---|---|
| Patient 1: LR a | 12 mm | Unable | 9.0 mm | Unable | 9.5 mm |
| Patient 2: MR | 4.5 mm | Unable | 3.5 mm | 5.2 mm | 6.4 mm |
| Patient 2: LR | 7.0 mm | 10.0 mm | 8.0 mm | 7.3 mm | 10.7 mm |
| Patient 3: MR a | 9.5 mm | 10.5 mm | 6.0 mm | Unable | 9.1 mm |
| Patient 3: LR | 6.0 mm | 6.0 mm | 5.0 mm | 6.0 mm | 6.1 mm |
| Patient 4: MR | 5.0 mm | 4.5 mm | 4.5 mm | 4.1 mm | 6.6 mm |
| Patient 4: LR | 6.0 mm | unable | 6.0 mm | 6.4 mm | 7.9 mm |
| Patient 4: IR | 5.0 mm | unable | 4.0 mm | Unable | 5.8 mm |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pihlblad, M.S.; Troia, A.; Tibrewal, S.; Shah, P.R. Pre-, Intra-, and Post-Operative Evaluation of Extraocular Muscle Insertions Using Optical Coherence Tomography: A Comparison of Four Devices. J. Clin. Med. 2019, 8, 1732. https://doi.org/10.3390/jcm8101732
Pihlblad MS, Troia A, Tibrewal S, Shah PR. Pre-, Intra-, and Post-Operative Evaluation of Extraocular Muscle Insertions Using Optical Coherence Tomography: A Comparison of Four Devices. Journal of Clinical Medicine. 2019; 8(10):1732. https://doi.org/10.3390/jcm8101732
Chicago/Turabian StylePihlblad, Matthew S., Andrew Troia, Sapna Tibrewal, and Parth R. Shah. 2019. "Pre-, Intra-, and Post-Operative Evaluation of Extraocular Muscle Insertions Using Optical Coherence Tomography: A Comparison of Four Devices" Journal of Clinical Medicine 8, no. 10: 1732. https://doi.org/10.3390/jcm8101732
APA StylePihlblad, M. S., Troia, A., Tibrewal, S., & Shah, P. R. (2019). Pre-, Intra-, and Post-Operative Evaluation of Extraocular Muscle Insertions Using Optical Coherence Tomography: A Comparison of Four Devices. Journal of Clinical Medicine, 8(10), 1732. https://doi.org/10.3390/jcm8101732





