Trends in the Use and Outcomes of Mechanical Ventilation among Patients Hospitalized with Acute Exacerbations of COPD in Spain, 2001 to 2015
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Setting, and Participants
2.2. Study Variables
2.3. Statistical Methods
2.4. Ethical Aspects
3. Results
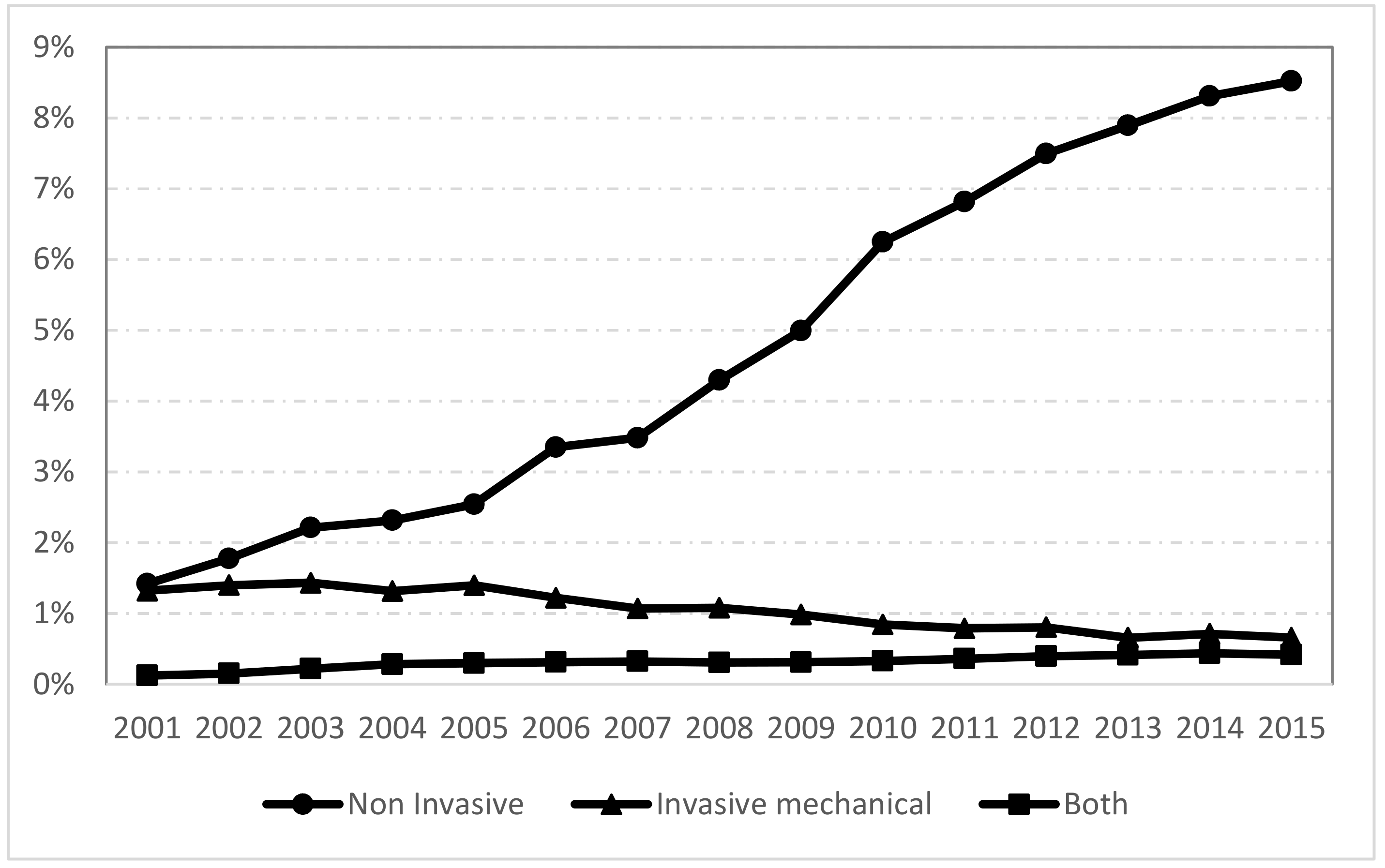
3.1. Trends in the Use of NIV and IMV between 2001 and 2015 and Time Trends of Ventilation Use from 2001 to 2015
3.1.1. Trends in the Use of NIV and IMV between 2001 and 2015
3.1.2. Time Trends of Ventilation Use from 2001 to 2015
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2019. Available online: http://www.goldcopd.org/ (accessed on 11 February 2018).
- Raveling, T.; Bladder, G.; Vonk, J.M.; Nieuwenhuis, J.A.; Verdonk-Struik, F.M.; Wijkstra, P.J.; Duiverman, M.L. Improvement in hypercapnia does not predict survival in COPD patients on chronic noninvasive ventilation. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 3625–3634. [Google Scholar] [CrossRef] [PubMed]
- Adeloye, D.; Chua, S.; Lee, C.; Basquill, C.; Papana, A.; Theodoratou, E.; Nair, H.; Gasevic, D.; Sridhar, D.; Campbell, H.; et al. Global and regional estimates of COPD prevalence: Systematic review and meta–analysis. J. Glob. Health 2015, 5, 020415. [Google Scholar] [CrossRef] [PubMed]
- Abroug, F.; Ouanes-Besbes, L.; Fkih-Hassen, M.; Ouanes, I.; Ayed, S.; Dachraoui, F.; Brochard, L.; Elatrous, S. Prednisone in COPD exacerbation requiring ventilatory support: An open-label randomised evaluation. Eur. Respir. J. 2014, 43, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Jinjuvadia, C.; Jinjuvadia, R.; Mandapakala, C.; Durairajan, N.; Liangpunsakul, S.; Soubani, A.O. Trends in outcomes, financial burden, and mortality for acute exacerbation of chronic obstructive pulmonary disease (COPD) in the United States from 2002 to 2010. COPD 2017, 14, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Toy, E.L.; Gallagher, K.F.; Stanley, E.L.; Swensen, A.R.; Duh, M.S. The Economic Impact of Exacerbations of Chronic Obstructive Pulmonary Disease and Exacerbation Definition: A Review. COPD 2010, 7, 214–228. [Google Scholar] [CrossRef] [PubMed]
- Todisco, T.; Baglioni, S.; Eslami, A.; Scoscia, E.; Todisco, C.; Bruni, L.; Dottorini, M. Treatment of acute exacerbations of chronic respiratory failure: Integrated use of negative pressure ventilation and noninvasive positive pressure ventilation. Chest 2004, 125, 2217–2223. [Google Scholar] [CrossRef] [PubMed]
- Duca, A.; Rosti, V.; Brambilla, A.M.; Cosentini, R. Non-invasive ventilation in COPD exacerbation: How and why. Intern. Emerg. Med. 2019, 14, 139–142. [Google Scholar] [CrossRef]
- Bott, J.; Carroll, M.; Conway, J.; Keilty, S.; Ward, E.; Brown, A.; Paul, E.; Elliott, M.; Godfrey, R.; Wedzicha, J.; et al. Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet 1993, 341, 1555–1557. [Google Scholar] [CrossRef]
- Rauss, A.; Gasparetto, A.; Harf, A.; Wysocki, M.; Lemaire, F.; Brochard, L.; Mancebo, J.; Lofaso, F.; Conti, G.; Simonneau, G.; et al. Noninvasive Ventilation for Acute Exacerbations of Chronic Obstructive Pulmonary Disease. N. Engl. J. Med. 1995, 333, 817–822. [Google Scholar]
- Plant, P.; Owen, J.; Elliott, M. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: A multicentre randomised controlled trial. Lancet 2000, 355, 1931–1935. [Google Scholar] [CrossRef]
- Lightowler, J.V.; Wedzicha, J.A.; Elliott, M.W.; Ram, F.S.F. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ 2003, 326, 185. [Google Scholar] [CrossRef] [PubMed]
- Seol, Y.M.; Park, Y.E.; Kim, S.R.; Lee, J.H.; Lee, S.J.; Kim, K.U.; Cho, J.H.; Park, H.K.; Kim, Y.S.; Lee, M.K.; et al. Application of Noninvasive Positive Pressure Ventilation in Patients with Respiratory Failure. Tuberc. Respir. Dis. 2006, 61, 26–33. [Google Scholar] [CrossRef][Green Version]
- Tee, V.S.; Carson-Chahhoud, K.V.; Picot, J.; Wedzicha, J.A.; Smith, B.J.; Osadnik, C.R. Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2017, 2017, CD004104. [Google Scholar]
- Lindenauer, P.K.; Stefan, M.S.; Shieh, M.-S.; Pekow, P.S.; Rothberg, M.B.; Hill, N.S. Outcomes associated with invasive and noninvasive ventilation among patients hospitalized with exacerbations of chronic obstructive pulmonary disease. JAMA Int. Med. 2014, 174, 1982–1993. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Campos, J.L.; Jara-Palomares, L.; Muñoz, X.; Bustamante, V.; Barreiro, E. Lights and shadows of non-invasive mechanical ventilation for chronic obstructive pulmonary disease (COPD) exacerbations. Ann. Thorac. Med. 2015, 10, 87–93. [Google Scholar] [CrossRef]
- Stefan, M.S.; Shieh, M.S.; Pekow, P.S.; Hill, N.; Rothberg, M.B.; Lindenauer, P.K. Trends in mechanical ventilation among patients hospitalized with acute exacerbations of COPD in the United States, 2001 to 2011. Chest 2015, 147, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Toft-Petersen, A.P.; Torp-Pedersen, C.; Weinreich, U.M.; Rasmussen, B.S. Trends in assisted ventilation and outcome for obstructive pulmonary disease exacerbations. A nationwide study. PLoS ONE 2017, 12, e0171713. [Google Scholar] [CrossRef]
- Gadre, S.K.; Duggal, A.; Mireles-Cabodevila, E.; Krishnan, S.; Wang, X.-F.; Zell, K.; Guzmán, J. Acute respiratory failure requiring mechanical ventilation in severe chronic obstructive pulmonary disease (COPD). Medicine 2018, 97, e0487. [Google Scholar] [CrossRef]
- Roberts, C.M.; López-Campos, J.L.; Pozo-Rodriguez, F.; Hartl, S.; Castro-Acosta, A.A.; Abraira-Santos, V.; López-Quílez, A.; Dorado, J.; Burghuber, O.; Kohansal, R.; et al. European hospital adherence to GOLD recommendations for chronic obstructive pulmonary disease (COPD) exacerbation admissions. Thorax 2013, 68, 1169–1171. [Google Scholar] [CrossRef]
- Ministry of Health. Spanish National Hospital Discharge Database (Conjunto Minimo Basico de Datos). Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/cmbdhome.htm (accessed on 15 April 2019).
- Mehta, A.B.; Syeda, S.N.; Wiener, R.S.; Walkey, A.J. Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. J. Crit. Care 2015, 30, 1217–1221. [Google Scholar] [CrossRef]
- Deyo, R. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Chandra, D.; Stamm, J.A.; Taylor, B.; Ramos, R.M.; Satterwhite, L.; Krishnan, J.A.; Mannino, D.; Sciurba, F.C.; Holguin, F. Outcomes of Noninvasive Ventilation for Acute Exacerbations of Chronic Obstructive Pulmonary Disease in the United States, 1998–2008. Am. J. Respir. Crit. Care Med. 2012, 185, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Carpe-Carpe, B.; Hernando-Arizaleta, L.; Ibáñez-Pérez, M.C.; Palomar-Rodríguez, J.A.; Esquinas-Rodríguez, A.M. Evolution of the Use of Noninvasive Mechanical Ventilation in Chronic Obstructive Pulmonary Disease in a Spanish Region, 1997–2010. Arch. Bronconeumol. 2013, 49, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Keenan, S.P.; Kernerman, P.D.; Cook, D.J.; Martin, C.M.; McCormack, D.; Sibbald, W.J. Effect of noninvasive positive pressure ventilation on mortality in patients admitted with acute respiratory failure: A meta-analysis. Crit. Care Med. 1997, 25, 1685–1692. [Google Scholar] [CrossRef] [PubMed]
- Demoule, A.; Chevret, S.; Carlucci, A.; Kouatchet, A.; Jaber, S.; Meziani, F.; Schmidt, M.; Schnell, D.; Clergue, C.; Aboab, J.; et al. Changing use of noninvasive ventilation in critically ill patients: Trends over 15 years in francophone countries. Intensive Care Med. 2016, 42, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Davidson, A.C.; Banham, S.; Elliott, M.; Kennedy, D.; Gelder, C.; Glossop, A.; Church, A.C.; Creagh-Brown, B.; Dodd, J.W.; Felton, T.; et al. BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax 2016, 71, ii1–ii35. [Google Scholar] [CrossRef] [PubMed]
- Wedzicha, J.A.; Miravitlles, M.; Hurst, J.R.; Calverley, P.M.; Albert, R.K.; Anzueto, A.; Criner, G.J.; Papi, A.; Rabe, K.F.; Rigau, D.; et al. Management of COPD exacerbations: A European Respiratory Society/American Thoracic Society guideline. Eur. Respir. J. 2017, 49. [Google Scholar] [CrossRef]
- Georges, M.; Vignaux, L.; Janssens, J.-P. Non invasive ventilation outside of the intensive care: Principles and modalities. Rev. Med. Suisse 2010, 6, 2246–2251. [Google Scholar]
- Trevisan, C.E.; Vieira, S.R.; Research Group in Mechanical Ventilation Weaning. Noninvasive mechanical ventilation may be useful in treating patients who fail weaning from invasive mechanical ventilation: A randomized clinical trial. Crit. Care 2008, 12, R51. [Google Scholar] [CrossRef]
- Riario-Sforza, G.G.; Scarpazza, P.; Incorvaia, C.; Casali, W. Role of noninvasive ventilation in elderly patients with hypercapnic respiratory failure. Clin. Ter. 2012, 163, e47–e52. [Google Scholar]
- Nava, S.; Grassi, M.; Fanfulla, F.; Domenighetti, G.; Carlucci, A.; Perren, A.; Dell’Orso, D.; Vitacca, M.; Ceriana, P.; Karakurt, Z.; et al. Non-invasive ventilation in elderly patients with acute hypercapnic respiratory failure: A randomised controlled trial. Age Ageing 2011, 40, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Trethewey, S.P.; Edgar, R.G.; Morlet, J.; Mukherjee, R.; Turner, A.M. Temporal trends in survival following ward-based NIV for acute hypercapnic respiratory failure in patients with COPD. Clin. Respir. J. 2019, 13, 184–188. [Google Scholar] [CrossRef]
- Ciledag, A.; Kaya, A.; Akdogan, B.B.; Kabalak, P.A.; Onen, Z.P.; Gulbay, E.S.B. Early Use of Noninvasive Mechanical Ventilation in Patients with Acute Hypercapnic Respiratory Failure in a Respiratory Ward: A Prospective Study. Arch. Bronconeumol. 2010, 46, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.M.; D’Cruz, R.F.; Murphy, P.B. Update: Non-invasive ventilation in chronic obstructive pulmonary disease. J. Thorac. Dis. 2018, 10, S71–S79. [Google Scholar] [CrossRef] [PubMed]
- Stein, B.D.; Bautista, A.; Schumock, G.T.; Lee, T.A.; Charbeneau, J.T.; Lauderdale, D.S.; Naureckas, E.T.; Meltzer, D.O.; Krishnan, J.A. The validity of International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes for identifying patients hospitalized for COPD exacerbations. Chest 2012, 141, 87–93. [Google Scholar] [CrossRef]
| 2001–2003 | 2004–2006 | 2007–2009 | 2010–2012 | 2013–2015 | Total | p | ||
|---|---|---|---|---|---|---|---|---|
| Sex, n (%) | Male | 227,159 (84.77) | 244,122 (85.62) | 262,861 (85.39) | 243,934 (84.49) | 234,464 (83.05) | 1,212,540 (84.68) | <0.001 |
| Female | 40,815 (15.23) | 41,007 (14.38) | 44,968 (14.61) | 44,769 (15.51) | 47,836 (16.95) | 219,395 (15.32) | ||
| Age | Mean (SD) | 73.6 (9.85) | 74.24 (9.96) | 74.72 (10.25) | 75.24 (10.46) | 75.26 (10.71) | 74.63 (10.27) | <0.001 |
| Age groups in years, n (%) | 40–64 | 43,592 (16.27) | 45,053 (15.8) | 49,955 (16.23) | 45,997 (15.93) | 46,486 (16.47) | 231,083 (16.14) | <0.001 |
| 65–74 | 89,012 (33.22) | 86,832 (30.45) | 83,077 (26.99) | 71,382(24.73) | 70,830 (25.09) | 401,133 (28.01) | ||
| 75–84 | 103,098 (38.47) | 115,080 (40.36) | 125,418 (40.74) | 118,041 (40.89) | 109,007 (38.61) | 570,644 (39.85) | ||
| ≥85 | 32,272 (12.04) | 38,164 (13.38) | 49 379 (16.04) | 53,283 (18.46) | 55,977 (19.83) | 229,075 (16) | ||
| Charlson comorbidity index, n (%) | 1 | 144,016 (53.74) | 137,056 (48.07) | 135 531 (44.03) | 114,458 (39.65) | 105,536 (37.38) | 636,597 (44.46) | <0.001 |
| 2 | 72,471 (27.04) | 80,072 (28.08) | 86,132 (27.98) | 80,587 (27.91) | 77,274 (27.37) | 396,536 (27.69) | ||
| ≥3 | 51,487 (19.21) | 68,001 (23.85) | 86,166 (27.99) | 93,658 (32.44) | 99,490 (35.24) | 398,802 (27.85) | ||
| Pneumonia, n (%) | Yes | 47,426 (17.7) | 53,678 (18.83) | 58,416 (18.98) | 61,497 (21.3) | 66,808 (23.67) | 287,825 (20.1) | <0.001 |
| Ventilation type, n (%) | NV | 258,932 (96.63) | 272,759 (95.66) | 290,577 (94.4) | 265,526 (91.97) | 255,912 (90.65) | 1,343,706 (93.84) | <0.001 |
| NIV | 4881 (1.82) | 7776 (2.73) | 13,072 (4.25) | 19,789 (6.85) | 23,293 (8.25) | 68,811 (4.81) | ||
| IMV | 3716 (1.39) | 3747 (1.31) | 3216 (1.04) | 2346 (0.81) | 1904 (0.67) | 14,929 (1.04) | ||
| NIV + IMV | 445 (0.17) | 847 (0.3) | 964 (0.31) | 1042 (0.36) | 1191 (0.42) | 4489 (0.31) | ||
| Length of hospital stay | Mean (sd) | 9.57 (8.32) | 9.25 (7.94) | 8.88 (7.98) | 8.33 (7.63) | 8.04 (6.89) | 8.81 (7.79) | <0.001 |
| In-hospital mortality, n (%) | Yes | 18,436 (6.88) | 20,170 (7.07) | 21,289 (6.92) | 19,866 (6.88) | 18,667 (6.61) | 98,428 (6.87) | <0.001 |
| Type | 2001–2003 | 2004–2006 | 2007–2009 | 2010–2012 | 2013–2015 | Total | |
|---|---|---|---|---|---|---|---|
| Male Sex, n (%) | NV* | 219,352 (84.71) | 233,526 (85.62) | 248,336 (85.46) | 224,806 (84.66) | 213,329 (83.36) | 1,139,349 (84.79) |
| NIV * | 4198 (86.01) | 6611 (85.02) | 10,959 (83.84) | 16,328 (82.51) | 18,656 (80.09) | 56,752 (82.48) | |
| IMV * | 3230 (86.92) | 3235 (86.34) | 2738 (85.14) | 1940 (82.69) | 1543 (81.04) | 12,686 (84.98) | |
| NIV + IMV * | 379 (85.17) | 750 (88.55) | 828 (85.89) | 860 (82.53) | 936 (78.59) | 3753 (83.6) | |
| Age, mean (sd) | NV * | 73.75 (9.82) | 74.43 (9.91) | 74.97 (10.21) | 75.56 (10.4) | 75.63 (10.65) | 74.87 (10.22) |
| NIV * | 69.76 (9.71) | 70.31 (10.2) | 70.98 (10.21) | 72.13 (10.49) | 72.16 (10.6) | 71.55 (10.42) | |
| IMV * | 68.73 (9.47) | 69.44 (9.5) | 69.75 (9.88) | 68.67 (10.2) | 68.69 (10.08) | 69.12 (9.77) | |
| NIV + IMV * | 68.34 (9.16) | 69.37 (9.4) | 68.29 (9.79) | 68.49 (9.75) | 68.07 (10.02) | 68.49 (9.71) | |
| CCI 1, n (%) | NV * | 139,286 (53.79) | 131,316 (48.14) | 128,147 (44.1) | 105,453 (39.71) | 95,592 (37.35) | 599,794 (44.64) |
| CCI 2, n (%) | 69,919 (27) | 76,253 (27.96) | 80,898 (27.84) | 73,505 (27.68) | 69,421 (27.13) | 369,996 (27.54) | |
| CCI ≥3, n (%) | 49,727 (19.2) | 65,190 (23.9) | 81,532 (28.06) | 86,568 (32.6) | 90,899 (35.52) | 373,916 (27.83) | |
| CCI 1, n (%) | NIV * | 2684 (54.99) | 3716 (47.79) | 5660 (43.3) | 7653 (38.67) | 8703 (37.36) | 28,416 (41.3) |
| CCI 2, n (%) | 1331 (27.27) | 2438 (31.35) | 4023 (30.78) | 6117 (30.91) | 6992 (30.02) | 20,901 (30.37) | |
| CCI ≥3, n (%) | 866 (17.74) | 1622 (20.86) | 3389 (25.93) | 6019 (30.42) | 7598 (32.62) | 19,494 (28.33) | |
| CCI 1, n (%) | IMV * | 1844 (49.62) | 1665 (44.44) | 1305 (40.58) | 940 (40.07) | 759 (39.86) | 6513 (43.63) |
| CCI 2, n (%) | 1074 (28.9) | 1103 (29.44) | 923 (28.7) | 653 (27.83) | 514 (27) | 4267 (28.58) | |
| CCI ≥3, n (%) | 798 (21.47) | 979 (26.13) | 988 (30.72) | 753 (32.1) | 631 (33.14) | 4149 (27.79) | |
| CCI 1, n (%) | NIV + IMV * | 202(45.39) | 359 (42.38) | 419 (43.46) | 412 (39.54) | 482 (40.47) | 1874 (41.75) |
| CCI 2, n (%) | 147 (33.03) | 278 (32.82) | 288 (29.88) | 312 (29.94) | 347 (29.14) | 1372 (30.56) | |
| CCI ≥3, n (%) | 96 (21.57) | 210 (24.79) | 257 (26.66) | 318 (30.52) | 362 (30.39) | 1243 (27.69) | |
| Pneumonia n (%) | NV * | 45,902 (17.73) | 51,789 (18.99) | 56,277 (19.37) | 58,429 (22.01) | 62,703 (24.5) | 275,100 (20.47) |
| NIV * | 507 (10.39) | 808 (10.39) | 1272 (9.73) | 2276 (11.5) | 3342 (14.35) | 8205 (11.92) | |
| IMV * | 927 (24.95) | 928 (24.77) | 697 (21.67) | 576 (24.55) | 482 (25.32) | 3610 (24.18) | |
| NIV + IMV * | 90 (20.22) | 153 (18.06) | 170 (17.63) | 216 (20.73) | 281 (23.59) | 910 (20.27) | |
| LOHS, mean (sd) | NV * | 9.4 (8.11) | 9.05 (7.7) | 8.66 (7.66) | 8.08 (7.37) | 7.77 (6.57) | 8.6 (7.53) |
| NIV * | 12.03 (9.7) | 11.52 (8.96) | 11.22 (10.02) | 10.42 (8.71) | 10.07 (8.19) | 10.69 (8.93) | |
| IMV * | 16.67 (13.97) | 16.26 (13.59) | 15.96 (14.52) | 15.07 (12.04) | 14.45 (12.09) | 15.88 (13.5) | |
| NIV + IMV * | 19.94 (14.75) | 19.39 (14.54) | 18.34 (14.37) | 18.87 (14.3) | 17.22 (12.86) | 18.52 (14.06) | |
| IHM, n (%) | NV * | 16,513 (6.38) | 17,756 (6.51) | 18,378 (6.32) | 16,470 (6.2) | 14,883 (5.82) | 84,000 (6.25) |
| NIV | 559 (11.45) | 932 (11.99) | 1579 (12.08) | 2375 (12) | 2895 (12.43) | 8340 (12.12) | |
| IMV | 1227 (33.02) | 1264 (33.73) | 1046 (32.52) | 734 (31.29) | 601 (31.57) | 4872 (32.63) | |
| NIV + IMV * | 137 (30.79) | 218 (25.74) | 286 (29.67) | 287 (27.54) | 288 (24.18) | 1216 (27.09) |
| NIV/No Ventilation | IMV/No Ventilation | NIV + IMV/No Ventilation | |
|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Year | 1.147 (1.145–1.149) | 0.953 (0.950–0.957) | 1.084 (1.077–1.091) |
| Female sex | 1.137 (1.114–1.161) | 1.137 (1.092–1.185) | 1.140 (1.061–1.226) |
| 65–74 years old | 0.767 (0.751–0.784) | 0.664 (0.640–0.688) | 0.645 (0.605–0.688) |
| 75–84 years old | 0.543 (0.531–0.554) | 0.359 (0.346–0.373) | 0.310 (0.289–0.333) |
| ≥85 years old | 0.321 (0.311–0.330) | 0.075 (0.068–0.082) | 0.049 (0.040–0.0605) |
| CCI 2 | 1.205 (1.183–1.228) | 1.171 (1.131–1.213) | 1.242 (1.165–1.324) |
| CCI ≥3 | 1.078 (1.057–1.098) | 1.255 (1.210–1.301) | 1.145 (1.071–1.224) |
| Pneumonia | 0.520 (0.508–0.533) | 1.425 (1.377–1.474) | 1.082 (1.013–1.156) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Miguel-Diez, J.; Jiménez-García, R.; Hernández-Barrera, V.; Puente-Maestu, L.; Girón-Matute, W.I.; de Miguel-Yanes, J.M.; Méndez-Bailón, M.; Villanueva-Orbaiz, R.; Albaladejo-Vicente, R.; López-de-Andrés, A. Trends in the Use and Outcomes of Mechanical Ventilation among Patients Hospitalized with Acute Exacerbations of COPD in Spain, 2001 to 2015. J. Clin. Med. 2019, 8, 1621. https://doi.org/10.3390/jcm8101621
de Miguel-Diez J, Jiménez-García R, Hernández-Barrera V, Puente-Maestu L, Girón-Matute WI, de Miguel-Yanes JM, Méndez-Bailón M, Villanueva-Orbaiz R, Albaladejo-Vicente R, López-de-Andrés A. Trends in the Use and Outcomes of Mechanical Ventilation among Patients Hospitalized with Acute Exacerbations of COPD in Spain, 2001 to 2015. Journal of Clinical Medicine. 2019; 8(10):1621. https://doi.org/10.3390/jcm8101621
Chicago/Turabian Stylede Miguel-Diez, Javier, Rodrigo Jiménez-García, Valentin Hernández-Barrera, Luis Puente-Maestu, Walther Iván Girón-Matute, José M. de Miguel-Yanes, Manuel Méndez-Bailón, Rosa Villanueva-Orbaiz, Romana Albaladejo-Vicente, and Ana López-de-Andrés. 2019. "Trends in the Use and Outcomes of Mechanical Ventilation among Patients Hospitalized with Acute Exacerbations of COPD in Spain, 2001 to 2015" Journal of Clinical Medicine 8, no. 10: 1621. https://doi.org/10.3390/jcm8101621
APA Stylede Miguel-Diez, J., Jiménez-García, R., Hernández-Barrera, V., Puente-Maestu, L., Girón-Matute, W. I., de Miguel-Yanes, J. M., Méndez-Bailón, M., Villanueva-Orbaiz, R., Albaladejo-Vicente, R., & López-de-Andrés, A. (2019). Trends in the Use and Outcomes of Mechanical Ventilation among Patients Hospitalized with Acute Exacerbations of COPD in Spain, 2001 to 2015. Journal of Clinical Medicine, 8(10), 1621. https://doi.org/10.3390/jcm8101621






