Multimodal Treatment of Patients with Mental Symptom Load: A Pre–Post Comparison
Abstract
:1. Introduction
2. Methods
2.1. TCM Hospital
2.2. Documentation System
2.3. ICD-10 Diagnosis
2.4. ISR (ICD-10-Symptom-Rating)
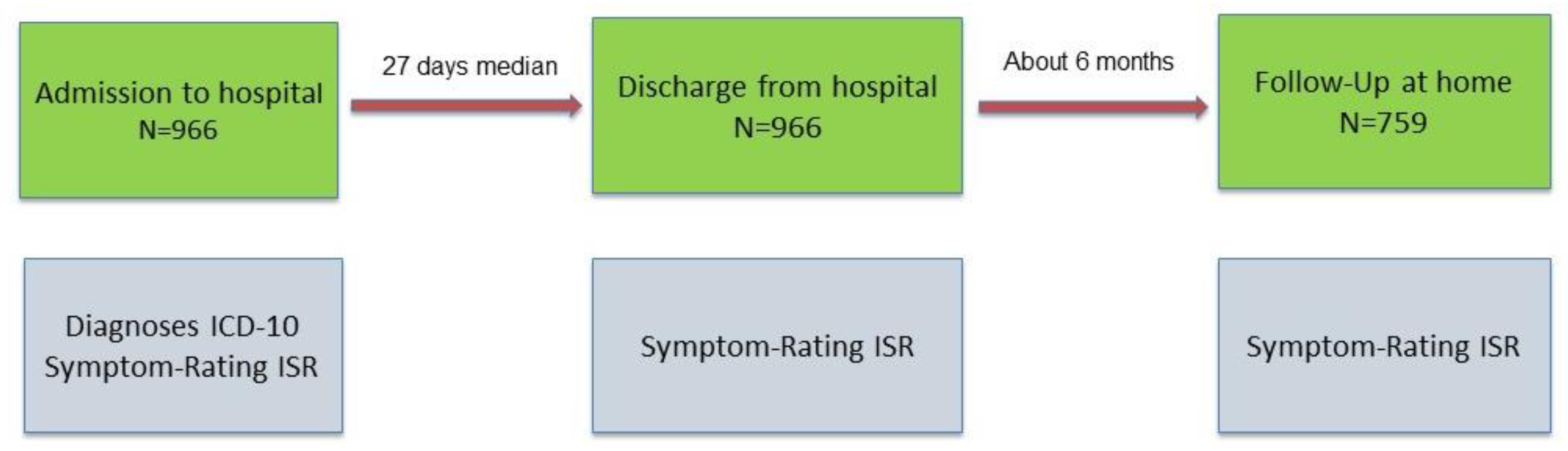
2.5. Study Design
2.6. Patient Admission
2.7. Multimodal Intervention Strategy
2.7.1. TCM Intervention
2.7.2. Psychotherapeutic and Psychoeducational Intervention
2.8. Statistical Analysis
Data Selection
3. Results
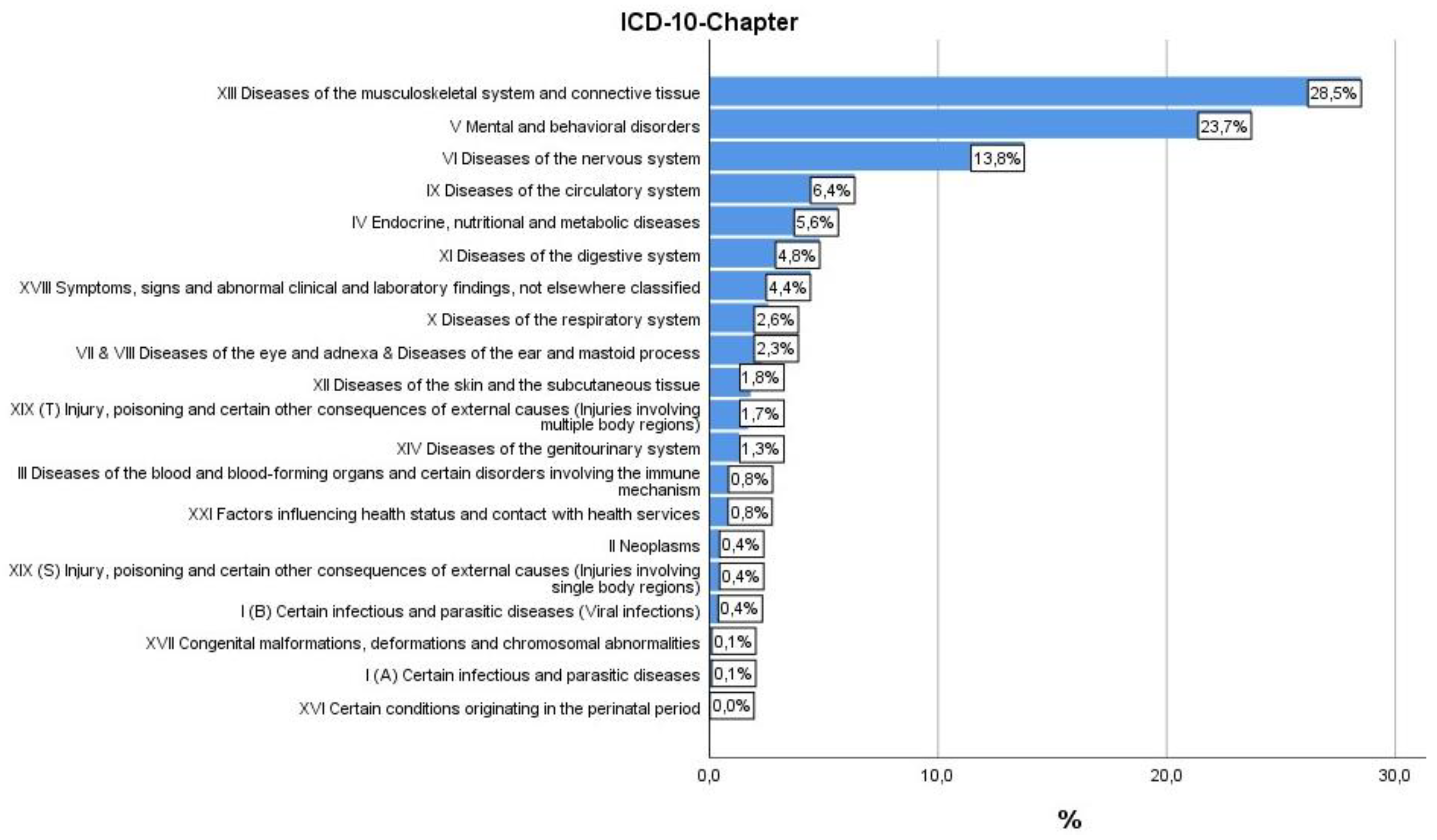
3.1. Sample Description
- Patients who had an ISR diagnosis at admission;
- Valid ISR values were available for all three time points (admission, discharge, and follow up);
- Patients were stationary at the TCM Hospital Bad Kötzting for a minimum of 14 and a maximum of 49 days;
- Patients had a follow-up between 180 and 300 days after discharge from the hospital.
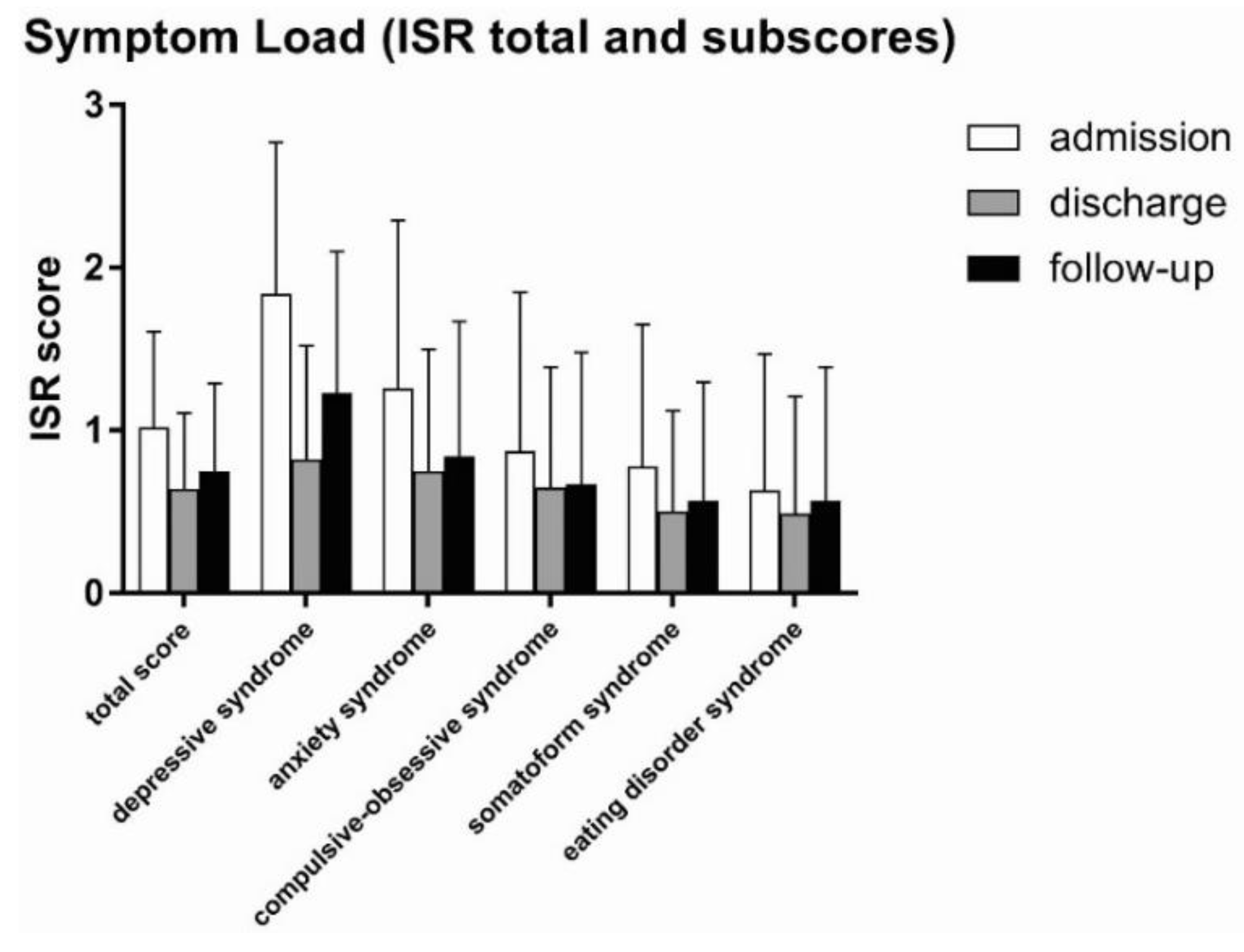
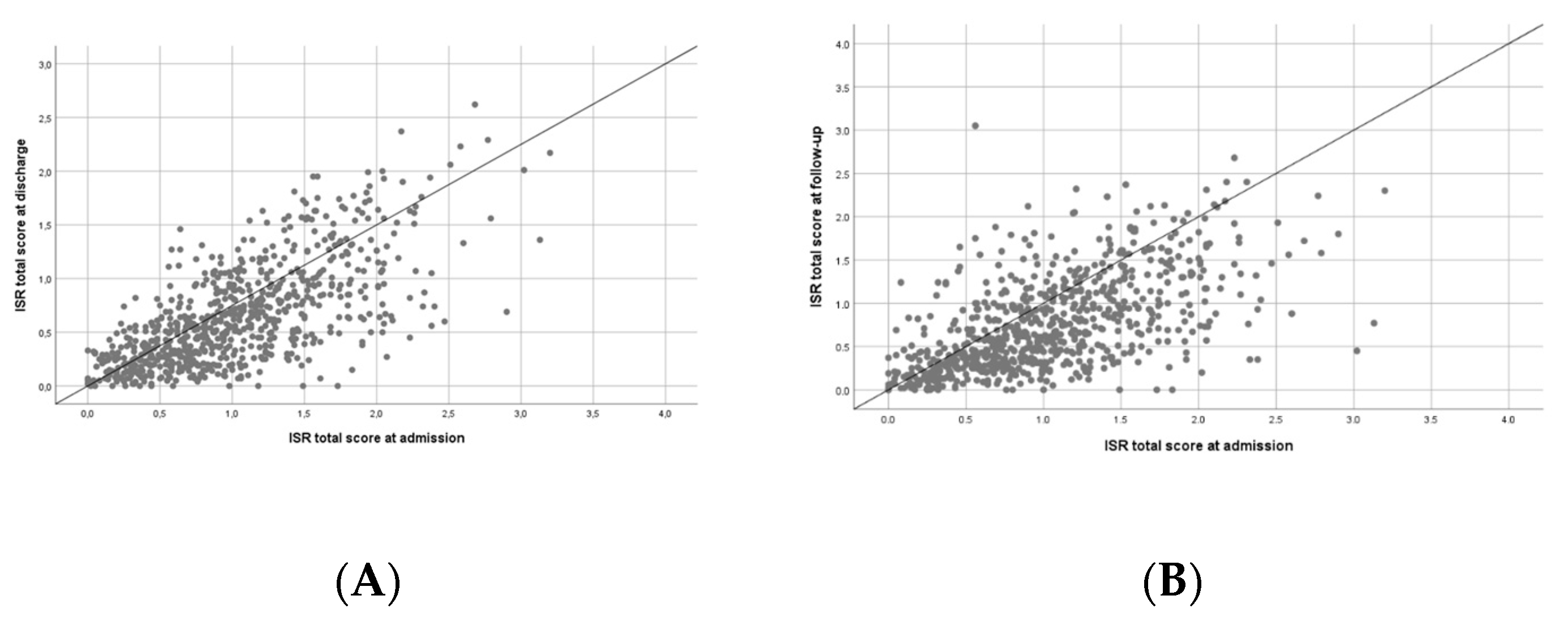
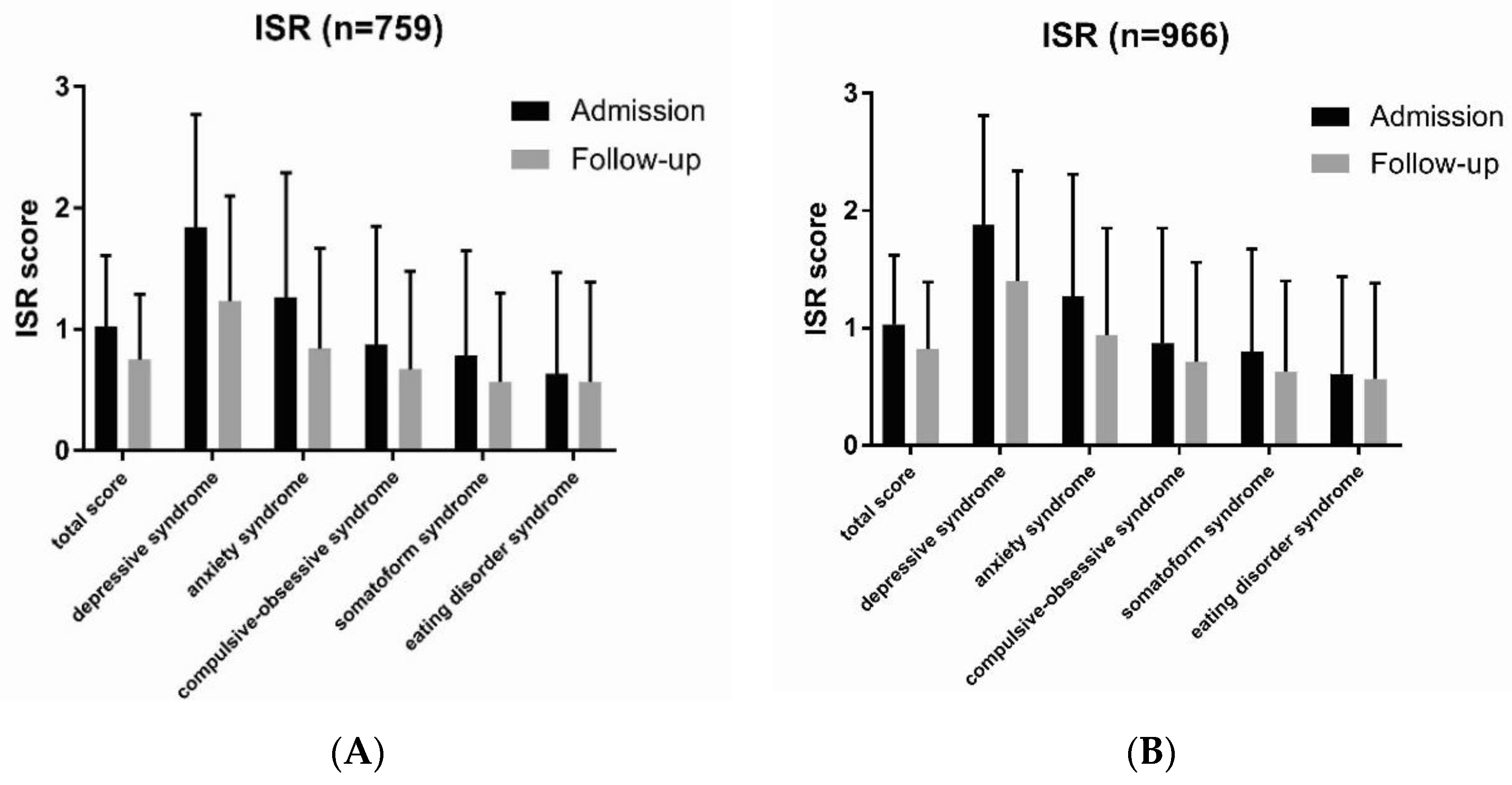
3.2. Symptom Load (ISR Total Score and Subscores) at Admission, Discharge, and Follow-Up
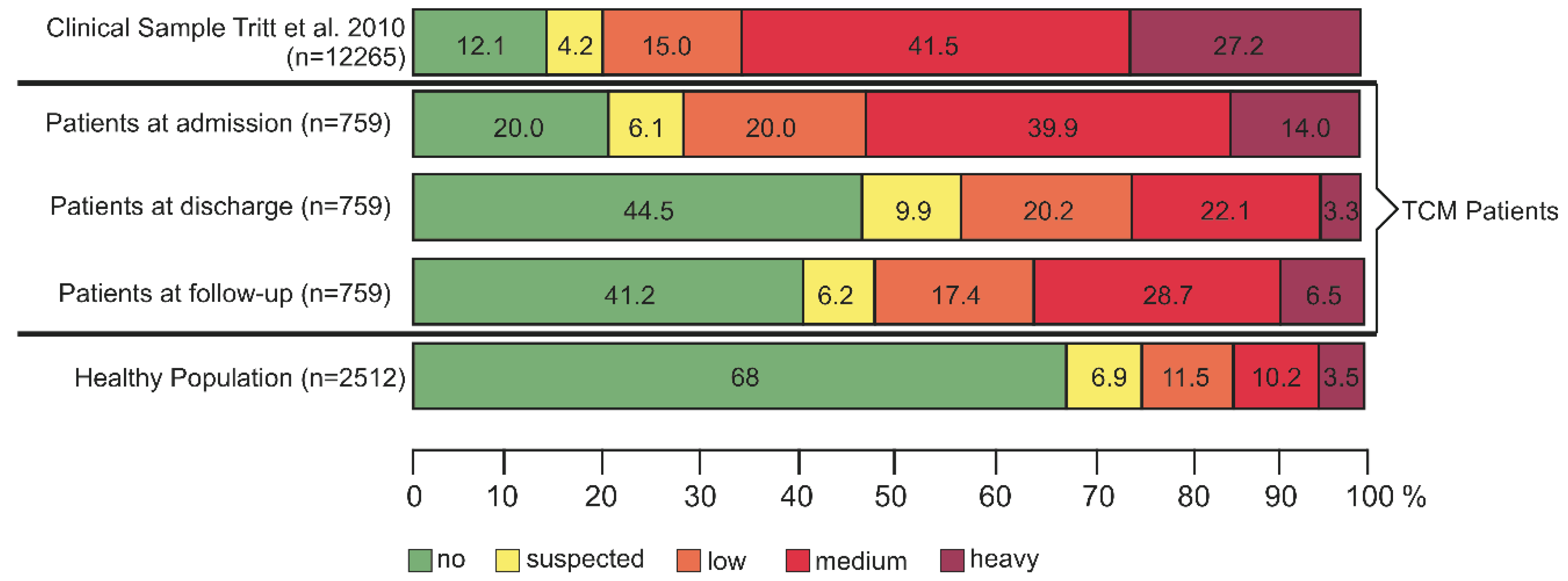
3.3. Percent Distribution of ISR Symptom Loads before and after TCM Intervention
3.4. Loss to Follow-Up
4. Discussion
- The majority of patients suffered from a combination of mental symptoms and chronic somatic disease, mostly pain.
- They had a long history of psychosomatic disease with high degree of chronicity.
- Outpatient conventional therapy did not have any significant beneficial effect.
- Patients had high symptom loads according to ISR classification.
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Fava, G.A.; Sonino, N. Psychosomatic medicine. Int. J. Clin. Pract. 2010, 64, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Katon, W.J.; Walker, E.A. Medically unexplained symptoms in primary care. J. Clin. Psychiatry 1998, 59, 15–21. [Google Scholar] [PubMed]
- Engel, G.L. A unified concept of health and disease. Perspect. Biol. Med. 1960, 3, 459–485. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Lipowski, Z.J. Psychosomatic medicine: Past and present. Part III. Current research. Can. J. Psychiatry 1986, 31, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Lipowski, Z.J. Psychosomatic medicine: Past and present. Part II. Current state. Can. J. Psychiatry 1986, 31, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Lipowski, Z.J. Psychosomatic medicine: Past and present. Part I. Historical background. Can. J. Psychiatry 1986, 31, 2–7. [Google Scholar] [CrossRef]
- Fava, G.A.; Sonino, N. Psychosomatic medicine: Emerging trends and perspectives. Psychother. Psychosom. 2000, 69, 184–197. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®), 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Gilmer, W.S.; Trivedi, M.H.; Rush, A.J.; Wisniewski, S.R.; Luther, J.; Howland, R.H.; Yohanna, D.; Khan, A.; Alpert, J. Factors associated with chronic depressive episodes: A preliminary report from the STAR-D project. Acta Psychiatr. Scand. 2005, 112, 425–433. [Google Scholar] [CrossRef]
- Murphy, J.A.; Byrne, G.J. Prevalence and correlates of the proposed DSM-5 diagnosis of chronic depressive disorder. J. Affect. Disord. 2012, 139, 172–180. [Google Scholar] [CrossRef]
- Spijker, J.; de Graaf, R.; Bijl, R.V.; Beekman, A.T.; Ormel, J.; Nolen, W.A. Duration of major depressive episodes in the general population: Results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Br. J. Psychiatry 2002, 181, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A. Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 2017, 166, 514–530. [Google Scholar] [CrossRef] [PubMed]
- National Center for Complementary and Integrative Health. Complementary, Alternative, or Integrative Health: What’s in a Name; National Center for Complementary and Integrative Health: Bethesda, MD, USA, July 2018. [Google Scholar]
- Melchart, D.; Eustachi, A.; Gronwald, S.; Wuhr, E.; Wifling, K.; Bachmeier, B.E. Introduction of a web portal for an Individual Health Management and observational health data sciences. Patient Relat. Outcome Meas. 2018, 9, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.; Collins, F.S. Patient-Centered Outcomes Research Institute: The intersection of science and health care. Sci. Transl. Med. 2010, 2, 37cm18. [Google Scholar] [CrossRef]
- Brandt, W.A.; Loew, T.; von Heymann, F.; Stadtmüller, G.; Georgi, A.; Tischinger, M.; Strom, F.; Mutschler, F.; Tritt, K. Das ICD-10 symptomrating (ISR): Validierung der depressionsskala an einer klinischen stichprobe. Psychother. Psych. Med. 2015, 65, 234–237. [Google Scholar] [CrossRef]
- Tritt, K.; von Heymann, F.; Zaudig, M.; Zacharias, I.; Sollner, W.; Loew, T. Development of the "ICD-10-Symptom-Rating"(ISR) questionnaire. Z. Psychosom. Med. Psychother. 2008, 54, 409–418. [Google Scholar] [CrossRef]
- Tritt, K.; von Heymann, F.; Zaudig, M.; Söllner, W.; Klapp, B.; Loew, T.; Bühner, M. Der Fragebogen ICD-10-Symptom-Rating (ISR) Kurzdarstellung der Normierung; IQP, Institut für Qualitätsentwicklung in der Psychotherapie und Psychosomatik: München, Germany, 2010; pp. 1–17. [Google Scholar]
- Hager, S.; Dai, J.; Fischer, V.; Luthke, F.; Staudinger, A. East meets west: Synergy through diversity. Complement. Med. Res. 2016, 23 (Suppl. 2), 3–7. [Google Scholar] [CrossRef]
- Melchart, D.; Staudinger, A. TCM Klinik Bad Kötzting—20 Jahre Wissenschaftliche Evaluation der Traditionellen Chinesischen Medizin, Klinikbericht 2011; Melchart, D., Staudinger, A., Eds.; Verlag Systemische Medizin: Bad Kötzting, Germany, 2011. [Google Scholar]
- Chaparro, L.E.; Wiffen, P.J.; Moore, R.A.; Gilron, I. Combination pharmacotherapy for the treatment of neuropathic pain in adults. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
- Krollner, B. ICD-10-GM Version 2013 Systematisches Verzeichnis. Internationale Statistische Klassifikation der Krankheiten und Verwandter Gesundheitsprobleme; Deutscher Ärzteverlag GmbH: Cologne, Germany, 2012. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting of observational studies. Internist 2008, 6, 688–693. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Melchart, D.; Eustachi, A.; Wellenhofer-Li, Y.; Doerfler, W.; Bohnes, E. Individual health management—A comprehensive lifestyle counselling programme for health promotion, disease prevention and patient education. Complement. Med. Res. 2016, 23, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Associates, L.E., Ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Lenhard, W.; Lenhard, A. Berechnung von Effektstärken. Available online: https://www.psychometrica.de/effektstaerke.html (accessed on 1 June 2019).
- Dunlap, W.P.; Cortina, J.M.; Vaslow, J.B.; Burke, M.J. Meta-analysis of experiments with matched groups or repeated measures designs. Psychol. Methods 1996, 1, 170–177. [Google Scholar] [CrossRef]
- Weidenhammer, W.; Melchart, D. Quality profiling at the TCM hospital Bad Kotzting—Examples from an ongoing systematic patient documentation. Complement. Med. Res. 2016, 23, 8–15. [Google Scholar] [CrossRef]
- Weidenhammer, W.; Melchart, D.; Hager, S. Treating chronically ill patients with traditional Chinese medicine—Its effects on their quality of life. Qual. Life Res. 1997, 6, 741. [Google Scholar]
- So, R.W.L.; Wong, H.S.; Ko, K.M. A traditional Chinese medicine approach in treating depression by promoting liver qi circulation: A western medicine perspective. Chin. Med. 2015, 6, 187–195. [Google Scholar]
- Kim, S.H.; Han, J.; Seog, D.H.; Chung, J.Y.; Kim, N.; Park, Y.H.; Lee, S.K. Antidepressant effect of Chaihu-Shugan-San extract and its constituents in rat models of depression. Life Sci. 2005, 76, 1297–1306. [Google Scholar] [CrossRef]
- Zhang, Z.J.; Tan, Q.R.; Tong, Y.; Wang, X.Y.; Wang, H.H.; Ho, L.M.; Wong, H.K.; Feng, Y.B.; Wang, D.; Ng, R.; et al. An epidemiological study of concomitant use of Chinese medicine and antipsychotics in schizophrenic patients: Implication for herb-drug interaction. PLoS ONE 2011, 6, e17239. [Google Scholar] [CrossRef]
- Kroenke, K. Patients presenting with somatic complaints: Epidemiology, psychiatric comorbidity and management. Int. J. Methods Psychiatr. Res. 2003, 12, 34–43. [Google Scholar] [CrossRef]
- Barkow, K.; Heun, R.; Ustun, T.B.; Berger, M.; Bermejo, I.; Gaebel, W.; Harter, M.; Schneider, F.; Stieglitz, R.D.; Maier, W. Identification of somatic and anxiety symptoms which contribute to the detection of depression in primary health care. Eur. Psychiatry 2004, 19, 250–257. [Google Scholar] [CrossRef]
- Barkow, K.; Heun, R.; Ustun, T.B.; Maier, W. Identification of items which predict later development of depression in primary health care. Eur. Arch. Psychiatry Clin. Neurosci. 2001, 251, 21–26. [Google Scholar] [CrossRef]
- Baune, B.T.; Caniato, R.N.; Garcia-Alcaraz, M.A.; Berger, K. Combined effects of major depression, pain and somatic disorders on general functioning in the general adult population. Pain 2008, 138, 310–317. [Google Scholar] [CrossRef] [PubMed]
- American College Health Association. American College Health Association-National College Health Assessment II; American College Health Association: Hannover, MD, USA, 2013. [Google Scholar]
| n | Female (%) | Age (Years) | ||
|---|---|---|---|---|
| Mean | SD | |||
| Admission | 966 | 74.6 | 55.41 | 11.92 |
| Discharge | 966 | 74.6 | 55.41 | 11.92 |
| Follow-up (eligible for outcome analysis) | 759 | 76.2 | 55.74 | 11.55 |
| ISR | Admission | Discharge | Follow-Up | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Cohen’s d | Mean | SD | Cohen’s d | |
| Total Score | 1.02 | 0.59 | 0.64 | 0.47 | 0.815 *** | 0.75 | 0.54 | 0.512 *** |
| Sub-scores | ||||||||
| Depressive Syndrome | 1.84 | 0.93 | 0.82 | 0.70 | 1.115 *** | 1.23 | 0.87 | 0.649 *** |
| Anxiety Syndrome | 1.26 | 1.03 | 0.75 | 0.75 | 0.588 *** | 0.84 | 0.83 | 0.43 *** |
| Compulsive-Obsessive Syndrome | 0.87 | 0.98 | 0.65 | 0.74 | 0.253 *** | 0.67 | 0.81 | 0.219 *** |
| Somatoform Syndrome | 0.78 | 0.87 | 0.50 | 0.62 | 0.352 *** | 0.57 | 0.73 | 0.247 *** |
| Eating Disorder Syndrome | 0.63 | 0.84 | 0.49 | 0.72 | 0.225 *** | 0.57 | 0.82 | 0.085 * |
| ISR Total Discharge | Total | |||||||
|---|---|---|---|---|---|---|---|---|
| No. | Suspected | Low | Medium | Heavy | ||||
| ISR total admission | no | n | 136 | 12 | 4 | 0 | 0 | 152 |
| % | 17.9% | 1.6% | 0.5% | 0.0% | 0.0% | 20.0% | ||
| suspected | n | 32 | 4 | 7 | 3 | 0 | 46 | |
| % | 4.2% | 0.5% | 0.9% | 0.4% | 0.0% | 6.1% | ||
| low | n | 85 | 28 | 23 | 16 | 0 | 152 | |
| % | 11.2% | 3.7% | 3.0% | 2.1% | 0.0% | 20.0% | ||
| medium | n | 78 | 27 | 96 | 96 | 6 | 303 | |
| % | 10.3% | 3.6% | 12.6% | 12.6% | 0.8% | 39.9% | ||
| heavy | n | 7 | 4 | 23 | 53 | 19 | 106 | |
| % | 0.9% | 0.5% | 3.0% | 7.0% | 2.5% | 14.0% | ||
| total | n | 273 | 338 | 75 | 153 | 168 | 25 | |
| % | 44.2% | 44.5% | 9.9% | 20.2% | 22.1% | 3.3% | ||
| ISR Total Follow-Up | Total | |||||||
|---|---|---|---|---|---|---|---|---|
| No | Suspected | Low | Medium | Heavy | ||||
| ISR total admission | no | n | 129 | 4 | 10 | 9 | 0 | 152 |
| % | 17.0% | 0.5% | 1.3% | 1.2% | 0.0% | 20.0% | ||
| suspected | n | 29 | 3 | 7 | 5 | 2 | 46 | |
| % | 3.8% | 0.4% | 0.9% | 0.7% | 0.3% | 6.1% | ||
| low | n | 72 | 16 | 29 | 32 | 3 | 152 | |
| % | 9.5% | 2.1% | 3.8% | 4.2% | 0.4% | 20.0% | ||
| medium | n | 74 | 20 | 69 | 121 | 19 | 303 | |
| % | 9.7% | 2.6% | 9.1% | 15.9% | 2.5% | 39.9% | ||
| heavy | n | 9 | 4 | 17 | 51 | 25 | 106 | |
| % | 1.2% | 0.5% | 2.2% | 6.7% | 3.3% | 14.0% | ||
| total | n | 253 | 313 | 47 | 132 | 218 | 49 | |
| % | 40.9% | 41.2% | 6.2% | 17.4% | 28.7% | 6.5% | ||
| Complete Datasets (n = 759) | Loss-to-Follow-Up (n = 207) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ICD-10-Symptom-Rating ISR | Admission | Discharge | Admission | Discharge | ||||||
| Mean | SD | Mean | SD | Cohen’s d | Mean | SD | Mean | SD | Cohen’s d | |
| Total score | 1.02 | 0.59 | 0.64 | 0.47 | 0.815 *** | 1.07 | 0.61 | 0.73 | 0.49 | 0.645 *** |
| Sub-scores | ||||||||||
| Depressive Syndrome | 1.84 | 0.93 | 0.82 | 0.70 | 1.115 *** | 2.03 | 0.93 | 1.07 | 0.82 | 1.041 *** |
| Anxiety Syndrome | 1.26 | 1.03 | 0.75 | 0.75 | 0.588 *** | 1.30 | 1.08 | 0.87 | 0.83 | 0.425 *** |
| Compulsive-Obsessive Syndrome | 0.87 | 0.98 | 0.65 | 0.74 | 0.253 *** | 0.85 | 0.99 | 0.67 | 0.76 | 0.193 ** |
| Somatoform Syndrome | 0.78 | 0.87 | 0.50 | 0.62 | 0.352 *** | 0.85 | 0.88 | 0.57 | 0.68 | 0.339 *** |
| Eating Disorder Syndrome | 0.63 | 0.84 | 0.49 | 0.72 | 0.225 *** | 0.55 | 0.79 | 0.48 | 0.67 | 0.113 |
| ICD-10-Symptom-Rating ISR | Complete Datasets (n = 759) | Baseline-Observation-Carried- Forward (n = 966) | ||||
|---|---|---|---|---|---|---|
| Admission Mean (SD) | Follow-Up Mean (SD) | Cohen’s d | Admission Mean (SD) | Follow-Up Mean (SD) | Cohen’s d | |
| Total score | 1.02 (0.59) | 0.75 (0.54) | 0.512 *** | 1.03 (0.59) | 0.82 (0.57) | 0.448 *** |
| Sub-scores | ||||||
| Depressive Syndrome | 1.84 (0.93) | 1.23 (0.87) | 0.649 *** | 1.88 (0.93) | 1.40 (0.94) | 0.572 *** |
| Anxiety Syndrome | 1.26 (1.03) | 0.84 (0.83) | 0.43 *** | 1.27 (1.04) | 0.94 (0.91) | 0.384 *** |
| Compulsive-obsessive Syndrome | 0.87 (0.98) | 0.67 (0.81) | 0.219 *** | 0.87 (0.98) | 0.71 (0.85) | 0.201 *** |
| Somatoform Syndrome | 0.78 (0.87) | 0.57 (0.73) | 0.247 *** | 0.80 (0.87) | 0.63 (0.77) | 0.229 *** |
| Eating disorder Syndrome | 0.63 (0.84) | 0.57 (0.82) | 0.085 * | 0.61 (0.83) | 0.57 (0.81) | 0.064 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melchart, D.; Fischer, V.; Dai, J.; Hager, S.; Dersch, L.; Bachmeier, B.E. Multimodal Treatment of Patients with Mental Symptom Load: A Pre–Post Comparison. J. Clin. Med. 2019, 8, 1610. https://doi.org/10.3390/jcm8101610
Melchart D, Fischer V, Dai J, Hager S, Dersch L, Bachmeier BE. Multimodal Treatment of Patients with Mental Symptom Load: A Pre–Post Comparison. Journal of Clinical Medicine. 2019; 8(10):1610. https://doi.org/10.3390/jcm8101610
Chicago/Turabian StyleMelchart, Dieter, Volker Fischer, Jingzhang Dai, Stefan Hager, Lisa Dersch, and Beatrice E. Bachmeier. 2019. "Multimodal Treatment of Patients with Mental Symptom Load: A Pre–Post Comparison" Journal of Clinical Medicine 8, no. 10: 1610. https://doi.org/10.3390/jcm8101610
APA StyleMelchart, D., Fischer, V., Dai, J., Hager, S., Dersch, L., & Bachmeier, B. E. (2019). Multimodal Treatment of Patients with Mental Symptom Load: A Pre–Post Comparison. Journal of Clinical Medicine, 8(10), 1610. https://doi.org/10.3390/jcm8101610





