In reviewing scientific databases of the available literature on pain perception and acceptance of illness by patients with cataracts, we did not find papers on this topic. Therefore, the results of our research were compared with results from the studies of other diseases. We believe that the results of this study will be significant for improving the quality of patient care and will be an important element in assessing the treatment process of patients with cataracts after surgery. The presented article may constitute the basis for planning activities aimed at sensitizing healthcare professionals in the discussed area and increasing the professional attitude of these employees towards patients with cataracts. Therefore, it seems advisable to conduct research that takes into account the assessment of pain perception and degree of acceptance of illness by patients with cataracts.
4.1. Acceptance of Illness Scale (AIS)
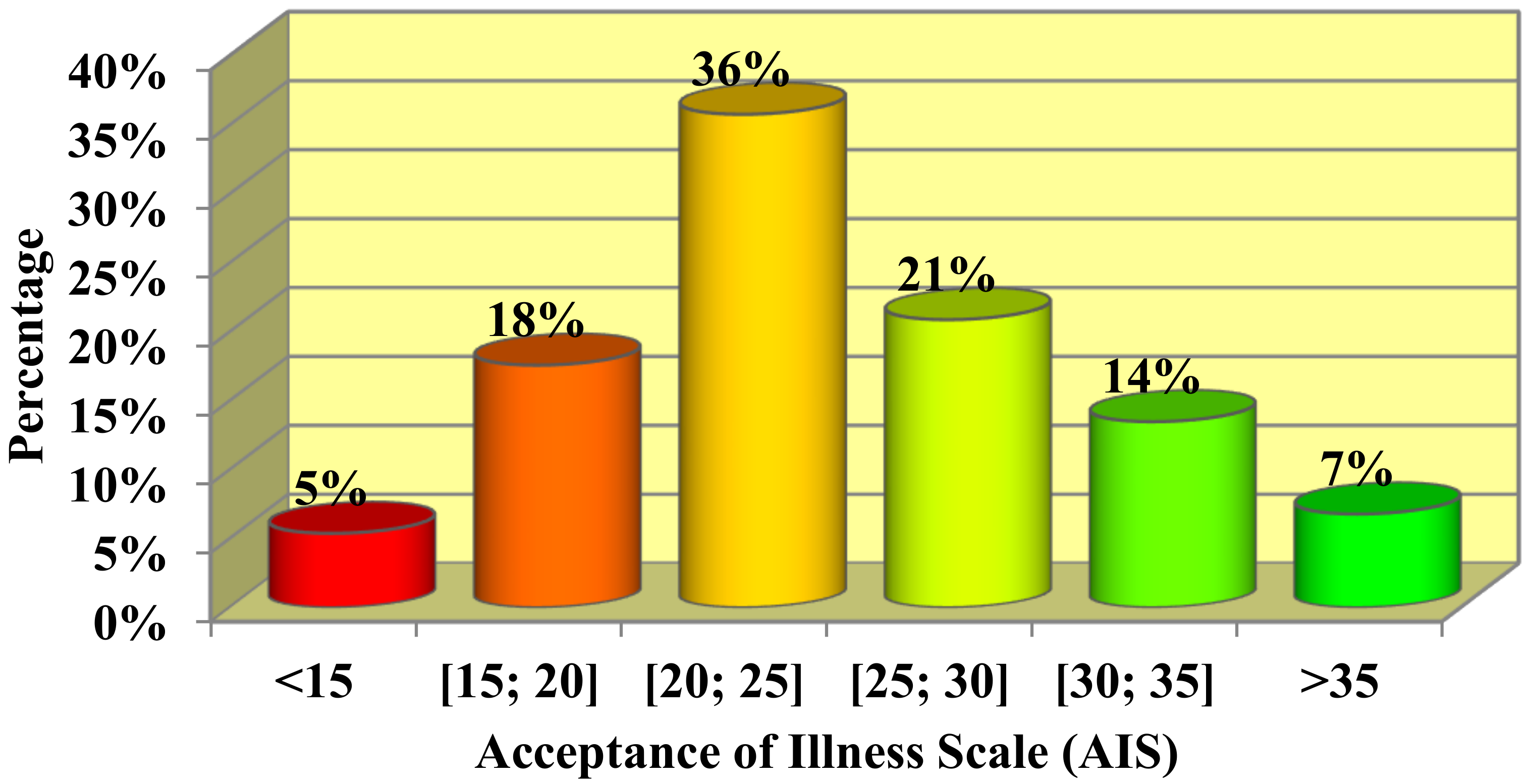
Our study showed that the respondents’ acceptance of the disease was average. The majority of respondents accepted their illness to a medium degree, which was reflected in the average level of the AIS results (the highest percentage of respondents assessed the acceptance of illness in the range of 20–25 points). Van Damme-Ostapowicz et al. [
23] presented quite different results in their study, which included 140 malaria patients treated at the Madonna University Teaching Hospital in Elele (Nigeria). The median value of the AIS in that study was only 10.5 points, indicating that malaria was not accepted. Such large differences could be caused by the severe course of the disease in comparison with cataracts, the high risk of serious malaria complications, as well as sociodemographic factors such as the patients’ financial situation, in addition to the quality of the provided healthcare services.
Interestingly, the mean point value on the AIS among breast cancer patients in studies conducted by Polish authors was significantly higher than in our study [
24,
25]. A higher mean point value was also recorded among 117 patients on dialysis, with an average age of 29.5 years (25.32 points) in a study by Adamczuk et al. [
26]. In this case, the higher level of illness acceptance—in comparison to the group included in our study—could be due to the younger age of the patients as well as the large percentage of patients that had prior kidney transplantation, which significantly reduces the burden associated with the disease.
Patients with ulcerative colitis had an even higher mean value of illness acceptance using the AIS [
27]. The was an average level of illness acceptance, and the mean point value on the AIS was 29.65 points. Similarly, a higher mean point value on the AIS was demonstrated by patients with lung diseases, such as asthma, chronic obstructive pulmonary disease, and obstructive sleep apnea (26.1 points) [
28], than the cataract patients in our study.
An assessment of illness acceptance using the AIS, conducted among patients with chronic obstructive pulmonary disease by Uchmanowicz et al. [
29], showed that the respondents were mainly characterized by a moderate level of acceptance, with a tendency to not accept their disease (20.6 points). In this case, the average value obtained on the AIS was lower than in our study. Cybulski et al., who studied people over 60 years of age, showed that the average level of acceptance of illness was 26.21 points. Rosińczuk et al. obtained similar point values for the acceptance of Parkinson’s disease in a group of 50 patients (25.28 points) [
30]. Sierakowska et al. obtained almost identical results in their study [
31]. The average level of illness acceptance in a group of patients with osteoarthritis was 25.75 points, which indicates an average level. Nevertheless, it should be emphasized that the compared groups differed in size, as well as in the diseases they had.
The statistical analysis conducted in our study did not show a correlation between sex and acceptance of illness. The study by Chrobak-Bień et al. also reached the same conclusion [
27]. These results are also in line with other results that did not confirm a higher level of acceptance of illness by men or women [
32]. The analysis carried out by Staniszewska et al. [
33] also did not show a statistically significant correlation between the patients’ sex and the level of acceptance of illness. In studies performed on surgery ward patients, an inverse correlation was found. According to these studies, men felt less psychological discomfort due to illness [
34].
The statistical analysis also included age. Our study indicated a statistically significant negative correlation between age and the level of average values for the AIS. The older the patients, the lower the average level of illness acceptance. Cipora et al. [
25] and Sierakowska et al. [
31] demonstrated an identical correlation in their studies. Chrobak-Bień et al. [
27] and Staniszewska et al. [
33], however, did not find an effect of age on the acceptance of illness. Similarly, no such correlation was observed by Polish researchers from Toruń who conducted an analysis of women treated for pathological cervical lesions [
35], nor by a research team from Rzeszów studying women after mastectomy [
36]. Glińska et al. [
32] determined that older patients adapted better to living with inflammatory bowel disease. The authors attributed this phenomenon to the more financially stable economic situation and professional status of older people. This observation was not confirmed by our research.
When studying the effect of education level on the acceptance of illness, no statistically significant correlation was found. Chrobak-Bień et al. [
27] showed that patients with a higher education showed a higher level of acceptance of illness than people with a secondary or vocational education. Andrzejewska et al. [
37] also showed higher point values of illness acceptance among people with a higher education. Glińska et al. [
32] described the strong influence of higher education on the acceptance of illness. We noted a completely different correlation in our study. Data from the study of Cipora et al. [
25] showed that women with a higher education had a higher level of illness acceptance compared with respondents with a lower level of education. The average AIS values did not differ significantly (
p = 0.12). An analysis of the results of the study by Staniszewska et al. [
33] did not show a significant correlation between illness acceptance and the respondents’ education. Similarly, Kaźmierczak et al. [
35], who studied disease acceptance in women treated for pathological cervical lesions, and Pawlik et al. [
36], who studied cancer acceptance in women after mastectomy, did not observe any effect of education level on illness acceptance. However, Niedzielski et al. [
17] and Szafraniec et al. [
38], who examined illness acceptance in patients with rheumatoid arthritis, obtained a negative level of acceptance of illness in people with a lower level of education. People with a higher education are characterized by a higher awareness of the risks associated with noncompliance with medical recommendations, and are, thus, more likely to learn to cope with the disease, which results in a greater acceptance.
In our study, we did not find any statistically significant differences in the level of illness acceptance depending on the place of residence. Cipora et al. noted a similar relationship [
25]. However, it should be noted that urban residents had a slightly higher level of illness acceptance than patients from rural areas.
4.2. Perception of Pain
Patients have different strategies for reducing pain. Our study showed that the respondents’ perception of pain was average. Most of the respondents assessed the effect of all three measures on pain control included in the BPCQ similarly. The BPCQ results in the study by Czerw et al. [
24] showed that patients with breast cancer mainly believed that doctors had the greatest influence on pain control and internal factors had the least influence. In addition, the same authors showed that in the case of pain management strategies, breast cancer patients most often preferred a strategy of coping with it, and least often, catastrophizing [
24]. Rosenstiel and Keefe [
22] and Juczyński [
39] drew similar conclusions. We obtained completely different results in our study of cataract patients; the most frequently adopted strategy was praying/hoping, while the rarest was increased behavioral activity. Similar results in the case of praying/hoping, as one of the most common strategies for coping with pain, have been noted in many other publications studying cancer patients [
40,
41,
42,
43,
44].
In the case of older people, Cybulski et al. [
45] showed that the influence of internal factors and doctors on pain control in the BPCQ was higher than in our study among patients with cataracts, whereas in the case of random events, the same result was obtained. In a group of 100 patients with peripheral artery disease in the study by Kadłubowska et al. [
46], the median of the influence of internal factors was 18 points, the influence of doctors was 19 points, and the effect of chance events was 16 points. The same study also included 100 patients with rheumatoid arthritis. In this group of patients, all three groups of factors affecting the perception of pain scored lower than those in patients with peripheral artery disease (internal factors 14 points, doctors 16 points, random events 15 points).
Our research showed that sex statistically significantly differentiated the level of pain experienced during the procedure. It was significantly higher in the group of women. However, there was no significant correlation between the level of pain and the patients’ age. Cybulski et al. [
45] found no statistically significant differences between men and women, as well as between age groups in terms of the point values of individual scales and their subscales. In the study by Krajewski et al. [
40], patients’ age also did not have a significant impact on the results of the CSQ, although there are studies in the literature in which age statistically significantly influenced the strategies for coping with pain [
47].
Our study showed that people who were better educated perceived pain as more severe; however, there was no statistically significant correlation in this case. Krajewski et al. came to the same conclusions in their study [
40], while Czerw et al. obtained completely different results [
24,
41]. The correlation we obtained may be illusory because women and people from younger age groups were better educated. To answer the question about the real impact of education, it would be necessary to perform multivariate analysis, e.g., regression analysis or analysis of variance, but the asymmetric distribution of the pain rating scale causes some difficulty, which makes it impossible to fully apply these analytical techniques.
When analyzing the place of residence, we found that patients in rural areas had significantly higher pain reduction abilities compared with patients living in urban areas. Krajewski et al. drew similar conclusions [
40]. However, these results were in contrast to the results of other authors [
24,
43].
The effect of the waiting time for treatment on the subjective feeling of pain was close to the level of statistical significance, whereas the nature of this effect was complex. A higher level of pain was felt by people waiting for surgery for periods that were both relatively short (perhaps due to the course of the disease, they qualified for surgery faster, and this could have been related to the level of pain) and relatively long (perhaps the “fatigue” of waiting for the procedure and, thus, a negative evaluation of its course were at play here).
The conducted study showed that the respondents experienced more pain during the operation of the first eye than the second eye. Gayadine-Harricham et al. [
48] reported similar results. Out of 69 patients enrolled in the study, only 13 people (19%) experienced more pain after the second-eye surgery. Shi et al. [
49] obtained completely different results in their meta-analysis, which examined eight published studies. The authors showed that patients experienced a greater pain intensity during surgery of the second eye than during first-eye surgery. This fact may be associated with various types of anxieties after first-eye surgery, as well as previous experiences during the first operation. The differing results obtained in our study could also be due to the fact that the vast majority of respondents were people who had already undergone surgery of the first eye.
4.3. Impact of Conducted Research on the Quality of Patient Care and their Clinical Significance
The study showed that a longer waiting time for surgery enhances the perception of pain, and first-eye surgery is felt to be more painful than second-eye surgery. Therefore, in order to improve the quality of patient care, the waiting time for first-eye surgery should be reduced as much as possible, while the waiting period for second-eye surgery may be a little longer.
Clinically, the study showed that the ideal solution would be a controlled administration of anesthetic drugs during phacoemulsification, depending on the patient’s pain. Currently, at the University Clinical Hospital in Białystok, anesthetics are administered only immediately before the procedure, which may affect the level of pain sensation after the surgery.