The Association between Adult Weight Gain and Insulin Resistance at Middle Age: Mediation by Visceral Fat and Liver Fat
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Study Population
2.2. Data Collection
2.2.1. Weight Change during Adulthood
2.2.2. Visceral Fat and Liver Fat at Middle Age
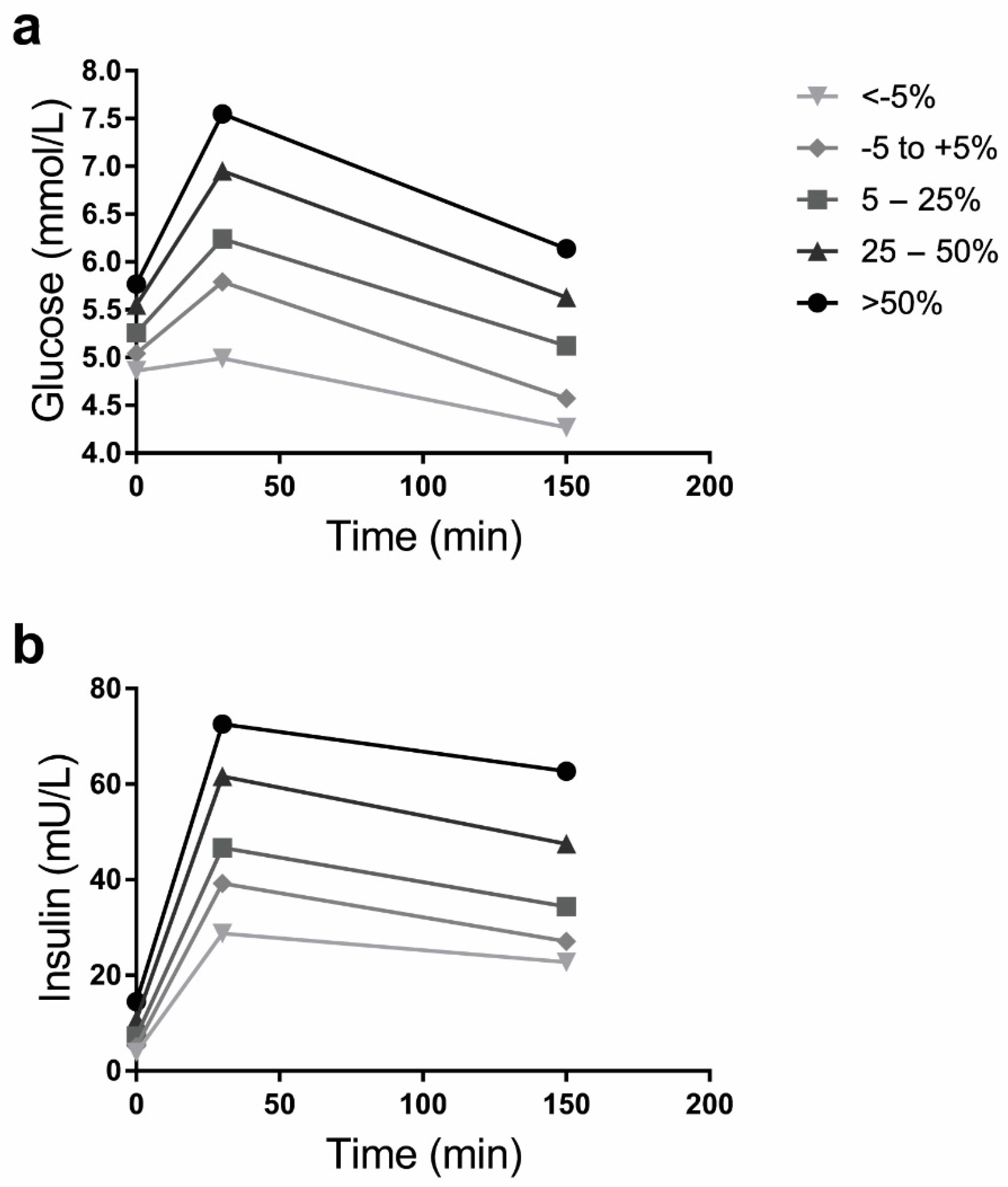
2.2.3. Measures of Insulin Resistance at Middle Age
2.2.4. Covariates
2.3. Statistical Analyses
3. Results
3.1. Characteristics of the Study Population
3.2. Adult Weight Change and Insulin Resistance at Middle Age
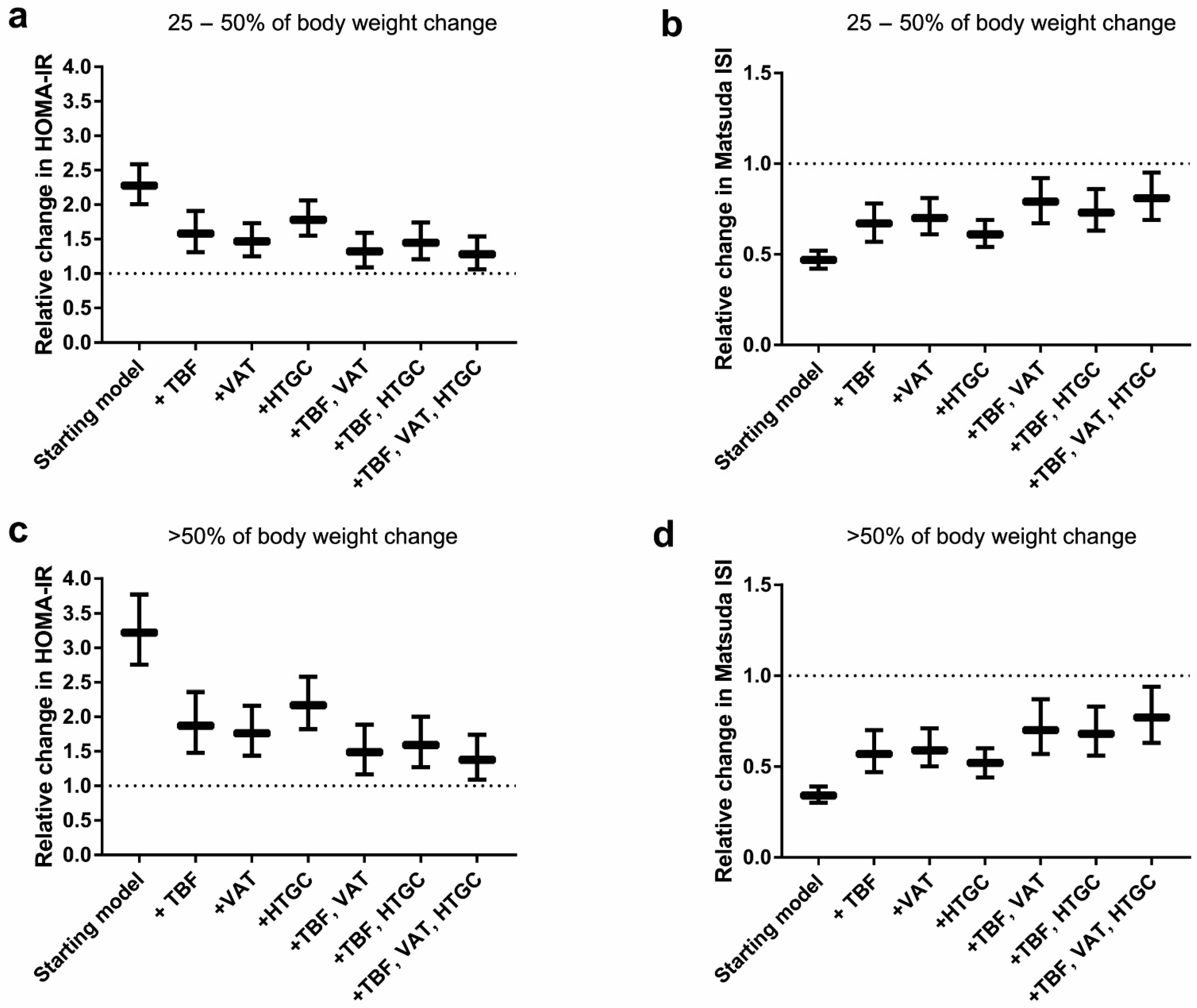
3.3. Mediation Analyses
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tirosh, A.; Shai, I.; Afek, A.; Dubnov-Raz, G.; Ayalon, N.; Gordon, B.; Derazne, E.; Tzur, D.; Shamis, A.; Vinker, S.; et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N. Engl. J. Med. 2011, 364, 1315–1325. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.; Peeters, A.; De Courten, M.; Stoelwinder, J. The magnitude of association between overweight and obesity and the risk of diabetes: A meta-analysis of prospective cohort studies. Diabetes Res. Clin. Pract. 2010, 89, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Dale, C.E.; Fatemifar, G.; Palmer, T.M.; White, J.; Prieto-Merino, D.; Zabaneh, D.; Engmann, J.E.L.; Shah, T.; Wong, A.; Warren, H.R.; et al. Causal Associations of Adiposity and Body Fat Distribution With Coronary Heart Disease, Stroke Subtypes, and Type 2 Diabetes Mellitus: A Mendelian Randomization Analysis. Circulation 2017, 135, 2373–2388. [Google Scholar] [CrossRef] [PubMed]
- De Mutsert, R.; Sun, Q.; Willett, W.C.; Hu, F.B.; van Dam, R.M. Overweight in early adulthood, adult weight change, and risk of type 2 diabetes, cardiovascular diseases, and certain cancers in men: A cohort study. Am. J. Epidemiol. 2014, 179, 1353–1365. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.M.; Rimm, E.B.; Colditz, G.A.; Stampfer, M.J.; Willett, W.C. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care 1994, 17, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Colditz, G.A.; Willett, W.C.; Rotnitzky, A.; Manson, J.E. Weight gain as a risk factor for clinical diabetes mellitus in women. Ann. Intern. Med. 1995, 122, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Shi, L.; Ye, Z.; Mu, Y.; Liu, C.; Zhao, J.; Chen, L.; Li, Q.; Yang, T.; Yan, L.; et al. Association between the change in body mass index from early adulthood to midlife and subsequent type 2 diabetes mellitus. Obesity 2016, 24, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Koh-Banerjee, P.; Wang, Y.; Hu, F.B.; Spiegelman, D.; Willett, W.C.; Rimm, E.B. Changes in Body Weight and Body Fat Distribution as Risk Factors for Clinical Diabetes in US Men. Am. J. Epidemiology 2004, 159, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Stefanska, A.; Sypniewska, G.; Blaszkiewicz, B.; Ponikowska, I.; Szternel, L.; Chojnowski, J. Long-term weight gain and metabolic syndrome, adiponectin and C-reactive protein in women aged 50-60 years. Adv. Med. Sci. 2010, 55, 186–190. [Google Scholar] [CrossRef]
- Kissebah, A.H.; Peiris, A.N. Biology of regional body fat distribution: Relationship to non-insulin-dependent diabetes mellitus. Diabetes/Metab. Rev. 1989, 5, 83–109. [Google Scholar] [CrossRef]
- Hartz, A.J.; Rupley, D.C.; Rimm, A.A. The association of girth measurements with disease in 32,856 women. Am. J. Epidemiol. 1984, 119, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Landin, K.; Stigendal, L.; Eriksson, E.; Krotkiewski, M.; Risberg, B.; Tengborn, L.; Smith, U.; Landin-Wilhelmsen, K. Abdominal obesity is associated with an impaired fibrinolytic activity and elevated plasminogen activator inhibitor-1. Metabolism 1990, 39, 1044–1048. [Google Scholar] [CrossRef]
- Kaye, S.A.; Folsom, A.R.; Sprafka, J.; Prineas, R.J.; Wallace, R.B. Increased incidence of diabetes mellitus in relation to abdominal adiposity in older women. J. Clin. Epidemiol. 1991, 44, 329–334. [Google Scholar] [CrossRef]
- Després, J.-P.; Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 2006, 444, 881–887. [Google Scholar] [CrossRef] [PubMed]
- De Mutsert, R.; Gast, K.; Widya, R.; de Koning, E.; Jazet, I.; Lamb, H.; le Cessie, S.; de Roos, A.; Smit, J.; Rosendaal, F.; et al. Associations of Abdominal Subcutaneous and Visceral Fat with Insulin Resistance and Secretion Differ Between Men and Women: The Netherlands Epidemiology of Obesity Study. Metab. Syndr. Relat. Disord. 2018, 16, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Verkouter, I.; Noordam, R.; de Roos, A.; Lamb, H.J.; Rosendaal, F.R.; van Heemst, D.; de Mutsert, R. Adult weight change in relation to visceral fat and liver fat at middle age: The Netherlands epidemiology of obesity study. Int. J. Obes. 2019, 43, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Unger, R.H. Lipid overload and overflow: Metabolic trauma and the metabolic syndrome. Trends Endocrinol. Metab. 2003, 14, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Tchernof, A.; Despres, J.P. Pathophysiology of human visceral obesity: An update. Physiol. Rev. 2013, 93, 359–404. [Google Scholar] [CrossRef]
- Klöting, N.; Fasshauer, M.; Dietrich, A.; Kovacs, P.; Schön, M.R.; Kern, M.; Stumvoll, M.; Blüher, M. Insulin-sensitive obesity. Am. J. Physiol. Endocrinol. Metab. 2010, 299, E506–E515. [Google Scholar] [CrossRef]
- Targher, G.; Day, C.P.; Bonora, E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N. Engl. J. Med. 2010, 363, 1341–1350. [Google Scholar] [CrossRef]
- De Mutsert, R.; Den Heijer, M.; Rabelink, T.J.; Smit, J.W.A.; Romijn, J.A.; Jukema, J.W.; de Roos, A.; Cobbaert, C.M.; Kloppenburg, M.; le Cessie, S.; et al. The Netherlands Epidemiology of Obesity (NEO) study: Study design and data collection. Eur. J. Epidemiol. 2013, 28, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Wallace, T.M.; Levy, J.C.; Matthews, D.R. Use and abuse of HOMA modeling. Diabetes Care 2004, 27, 1487–1495. [Google Scholar] [CrossRef] [PubMed]
- Retnakaran, R.; Shen, S.; Hanley, A.J.; Vuksan, V.; Hamilton, J.K.; Zinman, B. Hyperbolic relationship between insulin secretion and sensitivity on oral glucose tolerance test. Obesity 2008, 16, 1901–1907. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, M.; DeFronzo, R.A. Insulin sensitivity indices obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care 1999, 22, 1462–1470. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Matsuda, M. Reduced time points to calculate the composite index. Diabetes Care 2010, 33, e93. [Google Scholar] [CrossRef] [PubMed]
- Verkleij-Hagoort, A.C.; de Vries, J.H.; Stegers, M.P.; Lindemans, J.; Ursem, N.T.; Steegers-Theunissen, R.P. Validation of the assessment of folate and vitamin B12 intake in women of reproductive age: The method of triads. Eur. J. Clin. Nutr. 2007, 61, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Wendel-Vos, G.W.; Schuit, A.J.; Saris, W.H.; Kromhout, D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J. Clin. Epidemiol. 2003, 56, 1163–1169. [Google Scholar] [CrossRef] [Green Version]
- De Hollander, E.L.; Zwart, L.; de Vries, S.I.; Wendel-Vos, W. The SQUASH was a more valid tool than the OBiN for categorizing adults according to the Dutch physical activity and the combined guideline. J. Clin. Epidemiol. 2012, 65, 73–81. [Google Scholar] [CrossRef]
- Korn, E.L.; Graubard, B.I. Epidemiologic studies utilizing surveys: Accounting for the sampling design. Am. J. Public Health 1991, 81, 1166–1173. [Google Scholar] [CrossRef]
- Lumley, T. Analysis of complex survey samples. J. Statist. Softw. 2004, 9, 1–19. [Google Scholar] [CrossRef]
- Ministerie van Volksgezondheid, Welzijn en Sport. Nederland de Maat Genomen. Available online: www.rivm.nl/Onderwerpen/N/Nederland_de_Maat_Genomen (accessed on 13 August 2019).
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Gunzler, D.; Chen, T.; Wu, P.; Zhang, H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch. Psychiatry 2013, 25, 390–394. [Google Scholar] [PubMed]
- Kodama, S.; Horikawa, C.; Fujihara, K.; Yoshizawa, S.; Yachi, Y.; Tanaka, S.; Ohara, N.; Matsunaga, S.; Yamada, T.; Hanyu, O.; et al. Quantitative relationship between body weight gain in adulthood and incident type 2 diabetes: A meta-analysis. Obes. Rev. 2014, 15, 202–214. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Pham, N.M.; Yasuda, K.; Nanri, A.; Kurotani, K.; Kuwahara, K.; Akter, S.; Sato, M.; Hayabuchi, H.; Mizoue, T. Association of adulthood weight gain with circulating adipokine and insulin resistance in the Japanese population. Eur. J. Clin. Nutr. 2015, 69, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Spalding, K.L.; Arner, E.; Westermark, P.O.; Bernard, S.; Buchholz, B.A.; Bergmann, O.; Blomqvist, L.; Hoffstedt, J.; Näslund, E.; Britton, T.; et al. Dynamics of fat cell turnover in humans. Nature 2008, 453, 783. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, B. Adipose tissue, inflammation and atherosclerosis. J. Atheroscler. Thromb. 2010, 17, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.N.; Kim, S.P.; Catalano, K.J.; Hsu, I.R.; Chiu, J.D.; Kabir, M.; Hucking, K.; Ader, M. Why visceral fat is bad: Mechanisms of the metabolic syndrome. Obesity 2006, 14, 16S–19S. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.D. Is visceral fat involved in the pathogenesis of the metabolic syndrome? Human model. Obesity. 2006, 14, 20S–24S. [Google Scholar] [CrossRef]
- Kahn, S.E.; Hull, R.L.; Utzschneider, K.M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006, 444, 840–846. [Google Scholar] [CrossRef]
- Frayn, K. Adipose tissue as a buffer for daily lipid flux. Diabetologia 2002, 45, 1201–1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeFronzo, R.A.; Tobin, J.D.; Andres, R. Glucose clamp technique: A method for quantifying insulin secretion and resistance. Am. J. Physiol. 1979, 237, E214–E223. [Google Scholar] [CrossRef] [PubMed]
- Bonora, E.; Targher, G.; Alberiche, M.; Bonadonna, R.; Saggiani, F.; Zenere, M.B.; Monauni, T.; Muggeo, M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: Studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 2000, 23, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Casey, V.A.; Dwyer, J.T.; Berkey, C.S.; Coleman, K.A.; Gardner, J.; Valadian, I. Long-term memory of body weight and past weight satisfaction: A longitudinal follow-up study. Am. J. Clin. Nutr. 1991, 53, 1493–1498. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity and Overweight. Available online: www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 9 September 2019).
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef] [PubMed]
| Loss of >5% | Weight Maintenance −5% to <5% | Gain of ≥5% to <25% | Gain of ≥25% to <50% | Gain of ≥50% | |
|---|---|---|---|---|---|
| Proportion of population (%) | 4.5 | 11.2 | 55.0 | 24.7 | 4.6 |
| Sex (% men) | 22 | 39 | 50 | 46 | 38 |
| Body weight at age 20 | |||||
| Recalled weight at age 20 (kg) | 73.7 (8.0) | 67.2 (7.6) | 66.2 (9.3) | 64.5 (14.1) | 59.0 (14.5) |
| BMI at age 20 (kg/m2) | 25.1 (2.1) | 22.6 (1.9) | 21.7 (1.9) | 21.3 (3.3) | 19.9 (4.1) |
| Change in weight (%, range) | −7.6 (−32.2; −5.8) | 1.9 (−4.9; 4.8) | 14.9 (5.0; 24.9) | 32.3(25.0; 49.8) | 57.2 (50.0;102.8) |
| Characteristics at middle age | |||||
| Age (years) | 53 (3) | 57 (4) | 55 (5) | 55 (7) | 56 (8) |
| Ethnicity (% Caucasian) | 100 | 96 | 96 | 98 | 91 |
| Education (% high) | 45 | 53 | 51 | 37 | 31 |
| Smoking (% current) | 19 | 21 | 13 | 13 | 11 |
| Alcohol (g/day) | 4 (1–21) | 10 (4–16) | 11 (3–23) | 8 (2–21) | 8 (1–21) |
| Physical activity (MET-hours/week) | 27 (19–58) | 42 (28–56) | 31 (17–53) | 26 (14–44) | 20 (10–42) |
| Body weight (kg) | 66.0 (6.2) | 67.9 (7.8) | 76.0 (11.2) | 86.3 (18.7) | 94.6 (23.3) |
| BMI (kg/m2) | 22.4 (1.4) | 22.8 (1.9) | 25.0 (2.4) | 28.5 (4.6) | 31.9 (6.6) |
| Waist circumference (cm, M/W) | 90(5)/76(5) | 87(6)/77(7) | 96(7)/82(7) | 105(12)/93(13) | 110(14) /103(16) |
| Total body fat (%, M/W) | 18(3)/32(3) | 20(3)/31(4) | 24(3)/35(4) | 28(7)/41(6) | 31(8)/44(10) |
| Visceral adipose tissue (cm2, M/W) | 50(44–66)/21(14–37) | 50(19–79)/36(24–47) | 98(76–133)/49(35–69) | 135(104–173)/88(59–113) | 158(131–210)/118(94–156) |
| Hepatic triglyceride content (%, M/W) | 2.2(0.9–2.6)/0.9(0.7–1.6) | 1.8(1.0–3.6)/1.2(0.7–1.7) | 3.5(2.0–7.0)/1.6(1.1–3.6) | 6.0(3.5–14.0)/3.4(1.6–8.4) | 11.8(3.8–20.8)/7.7(3.7–18.8) |
| In women a: | |||||
| Postmenopausal (% yes) | 37 | 78 | 51 | 66 | 69 |
| Current use of sex hormones b (%) | 4 | 3 | 11 | 7 | 3 |
| Insulin resistance at middle age | |||||
| Family history of diabetes (% yes) | 31 | 22 | 26 | 24 | 31 |
| Family history of myocardial infarction (% yes) | 26 | 34 | 39 | 47 | 48 |
| Fasted plasma glucose (mmol/L) | 4.8 (4.5–5.1) | 5.1 (4.8–5.3) | 5.2 (4.9–5.6) | 5.5 (5.2–5.9) | 5.6 (5.3–6.1) |
| Fasted serum insulin (mU/L) | 5.5 (4.1–6.5) | 5.4 (3.6–7.1) | 7.3 (5.2–9.9) | 10.5 (7.6–14.7) | 13.0 (8.6–21.6) |
| HOMA-IR | 1.1 (0.8–1.5) | 1.2 (0.8–1.6) | 1.7 (1.2–2.4) | 2.6 (1.8–3.7) | 3.2 (2.1–5.5) |
| Matsuda ISI | 2.4 (2.1–2.7) | 2.1 (1.8–2.5) | 1.8 (1.5–2.1) | 1.4 (1.0–1.8) | 1.1 (0.6–1.6) |
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Ratio | 95% CI | Ratio | 95% CI | Ratio | 95% CI | |
| HOMA-IR | ||||||
| < −5.0% | 0.85 | 0.56; 1.30 | 0.85 | 0.56; 1.30 | 0.73 | 0.47; 1.12 |
| −5% to 5% (ref) | 1 | 1 | 1 | |||
| 5–25% | 1.38 | 1.21; 1.57 | 1.37 | 1.20; 1.56 | 1.47 | 1.30; 1.67 |
| 25–50% | 2.14 | 1.87; 2.44 | 2.04 | 1.79; 2.34 | 2.28 | 2.01; 2.59 |
| >50% | 2.78 | 2.34; 3.30 | 2.65 | 2.24; 3.14 | 3.22 | 2.76; 3.77 |
| Matsuda ISI | ||||||
| < −5.0% | 1.22 | 0.92; 1.63 | 1.23 | 0.92; 1.63 | 1.40 | 1.05; 1.86 |
| −5 to 5% (ref) | 1 | 1 | 1 | |||
| 5–25% | 0.75 | 0.67; 0.84 | 0.76 | 0.68; 0.84 | 0.71 | 0.64; 0.79 |
| 25–50% | 0.49 | 0.44; 0.55 | 0.51 | 0.46; 0.58 | 0.47 | 0.42; 0.52 |
| >50% | 0.38 | 0.32; 0.44 | 0.40 | 0.34; 0.47 | 0.34 | 0.30; 0.39 |
| All (N = 1758) | Men (N = 913) | Women (N = 845) | |||||
|---|---|---|---|---|---|---|---|
| % of Total Effect | 95% CI | % of Total Effect | 95% CI | % of Total Effect | 95% CI | ||
| Total effect | 100 | 100 | 100 | ||||
| Indirect effect through: | |||||||
| TBF alone | 34.2 | 16.6; 51.9 | 42.2 | 20.6; 63.9 | 27.3 | −0.4; 55.0 | |
| VAT alone | 44.1 | 31.3; 56.9 | 31.9 | 19.3; 44.6 | 51.2 | 29.6; 72.8 | |
| HTGC alone | 28.3 | 20.9; 35.8 | 25.8 | 14.9; 36.8 | 29.1 | 19.1; 39.1 | |
| TBF + VAT | TBF | 13.0 | −4.4; 30.3 | 29.8 | 9.0; 50.6 | −1.7 | −0.29.9; 26.5 |
| VAT | 41.6 | 28.7; 54.4 | 28.5 | 16.1; 41.0 | 51.7 | 29.4; 73.9 | |
| TBF + HTGC | TBF | 22.5 | 4.5; 40.5 | 28.6 | 7.6; 49.7 | 16.6 | −12.3; 45.5 |
| HTGC | 27.0 | 19.4; 34.6 | 24.2 | 13.4; 35.0 | 28.1 | 17.4; 38.8 | |
| TBF + VAT + HTGC | TBF | 8.1 | −9.2; 25.4 | 20.2 | −0.4; 40.9 | −3.2 | −30.8; 24.4 |
| VAT | 32.0 | 18.6; 45.4 | 22.5 | 10.2; 34.7 | 39.5 | 15.5; 63.4 | |
| HTGC | 22.5 | 15.0; 30.1 | 21.8 | 11.6; 32.0 | 21.9 | 10.6; 33.3 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verkouter, I.; Noordam, R.; le Cessie, S.; van Dam, R.M.; Lamb, H.J.; Rosendaal, F.R.; van Heemst, D.; de Mutsert, R. The Association between Adult Weight Gain and Insulin Resistance at Middle Age: Mediation by Visceral Fat and Liver Fat. J. Clin. Med. 2019, 8, 1559. https://doi.org/10.3390/jcm8101559
Verkouter I, Noordam R, le Cessie S, van Dam RM, Lamb HJ, Rosendaal FR, van Heemst D, de Mutsert R. The Association between Adult Weight Gain and Insulin Resistance at Middle Age: Mediation by Visceral Fat and Liver Fat. Journal of Clinical Medicine. 2019; 8(10):1559. https://doi.org/10.3390/jcm8101559
Chicago/Turabian StyleVerkouter, Inge, Raymond Noordam, Saskia le Cessie, Rob M. van Dam, Hildo J. Lamb, Frits R. Rosendaal, Diana van Heemst, and Renée de Mutsert. 2019. "The Association between Adult Weight Gain and Insulin Resistance at Middle Age: Mediation by Visceral Fat and Liver Fat" Journal of Clinical Medicine 8, no. 10: 1559. https://doi.org/10.3390/jcm8101559
APA StyleVerkouter, I., Noordam, R., le Cessie, S., van Dam, R. M., Lamb, H. J., Rosendaal, F. R., van Heemst, D., & de Mutsert, R. (2019). The Association between Adult Weight Gain and Insulin Resistance at Middle Age: Mediation by Visceral Fat and Liver Fat. Journal of Clinical Medicine, 8(10), 1559. https://doi.org/10.3390/jcm8101559





