Fibromyalgia and Shoulder Surgery: A Systematic Review and a Critical Appraisal of the Literature
Abstract
1. Introduction
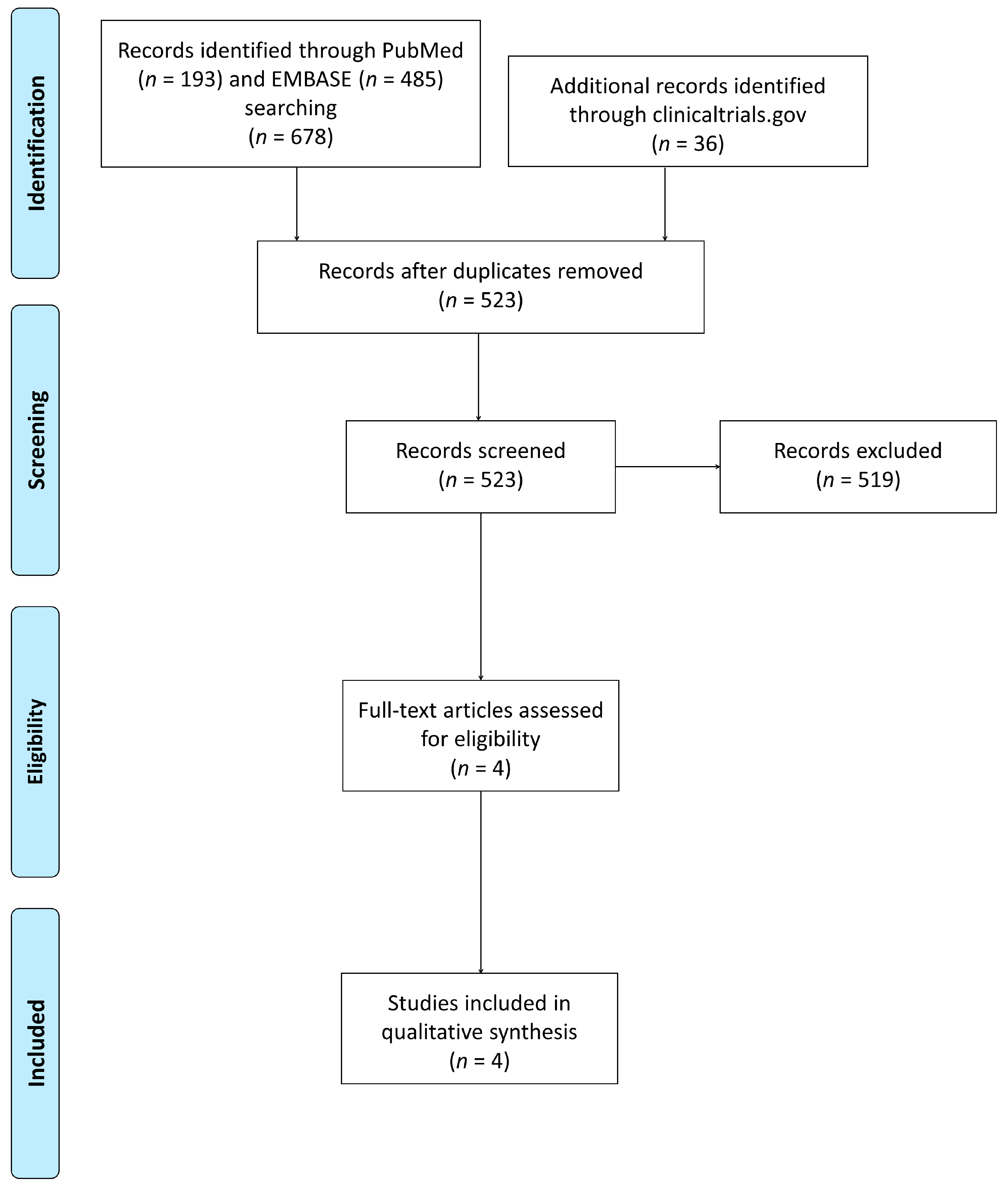
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bigatti, S.M.; Hernandez, A.M.; Cronan, T.A.; Rand, K.L. Sleep disturbances in fibromyalgia syndrome: Relationship to pain and depression. Arthritis Rheum. 2008, 59, 961–967. [Google Scholar] [CrossRef] [PubMed]
- Clauw, D.J. Fibromyalgia: A clinical review. JAMA 2014, 311, 1547–1555. [Google Scholar] [CrossRef]
- Queiroz, L.P. Worldwide epidemiology of fibromyalgia. Curr. Pain Headache Rep. 2013, 17, 356. [Google Scholar] [CrossRef]
- Choy, E.; Perrot, S.; Leon, T.; Kaplan, J.; Petersel, D.; Ginovker, A.; Kramer, E. A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Serv. Res. 2010, 10, 102. [Google Scholar] [CrossRef] [PubMed]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef]
- Napadow, V.; Harris, R.E. What has functional connectivity and chemical neuroimaging in fibromyalgia taught us about the mechanisms and management of ‘centralized’ pain? Arthritis Res. Ther. 2014, 16, 425. [Google Scholar] [CrossRef]
- Caro, X.J.; Winter, E.F. Evidence of abnormal epidermal nerve fiber density in fibromyalgia: Clinical and immunologic implications. Arthritis Rheumatol. 2014, 66, 1945–1954. [Google Scholar] [CrossRef] [PubMed]
- Littlejohn, G.; Guymer, E. Neurogenic inflammation in fibromyalgia. Semin. Immunopathol. 2018, 40, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P.; et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990, 33, 160–172. [Google Scholar] [CrossRef]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Fluss, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef]
- Wolfe, F. Pain extent and diagnosis: Development and validation of the regional pain scale in 12,799 patients with rheumatic disease. J. Rheumatol. 2003, 30, 369–378. [Google Scholar]
- Lee, Y.C.; Nassikas, N.J.; Clauw, D.J. The role of the central nervous system in the generation and maintenance of chronic pain in rheumatoid arthritis, osteoarthritis and fibromyalgia. Arthritis Res. Ther. 2011, 13, 211. [Google Scholar] [CrossRef]
- Affaitati, G.; Costantini, R.; Fabrizio, A.; Lapenna, D.; Tafuri, E.; Giamberardino, M.A. Effects of treatment of peripheral pain generators in fibromyalgia patients. Eur. J. Pain 2011, 15, 61–69. [Google Scholar] [CrossRef]
- Brummett, C.M.; Janda, A.M.; Schueller, C.M.; Tsodikov, A.; Morris, M.; Williams, D.A.; Clauw, D.J. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: A prospective, observational cohort study. Anesthesiology 2013, 119, 1434–1443. [Google Scholar] [CrossRef]
- Janda, A.M.; As-Sanie, S.; Rajala, B.; Tsodikov, A.; Moser, S.E.; Clauw, D.J.; Brummett, C.M. Fibromyalgia survey criteria are associated with increased postoperative opioid consumption in women undergoing hysterectomy. Anesthesiology 2015, 122, 1103–1111. [Google Scholar] [CrossRef]
- As-Sanie, S.; Till, S.R.; Mowers, E.L.; Lim, C.S.; Skinner, B.D.; Fritsch, L.; Tsodikov, A.; Dalton, V.K.; Clauw, D.J.; Brummett, C.M. Opioid Prescribing Patterns, Patient Use, and Postoperative Pain After Hysterectomy for Benign Indications. Obstet. Gynecol. 2017, 130, 1261–1268. [Google Scholar] [CrossRef]
- Kim, S.C.; Choudhry, N.; Franklin, J.M.; Bykov, K.; Eikermann, M.; Lii, J.; Fischer, M.A.; Bateman, B.T. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthr. Cartil. 2017, 25, 1399–1406. [Google Scholar] [CrossRef]
- Saccomanno, M.F.; Sircana, G.; Cazzato, G.; Donati, F.; Randelli, P.; Milano, G. Prognostic factors influencing the outcome of rotator cuff repair: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3809–3819. [Google Scholar] [CrossRef]
- Spennacchio, P.; Banfi, G.; Cucchi, D.; D’Ambrosi, R.; Cabitza, P.; Randelli, P. Long-term outcome after arthroscopic rotator cuff treatment. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 523–529. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2013. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 16 September 2019).
- Blonna, D.; Bellato, E.; Marini, E.; Barbasetti, N.; Mattei, L.; Fissore, F.; Arrigoni, C.; Castoldi, F. Is fibromyalgia a cause of failure in the treatment of a painful shoulder? Musculoskelet. Surg. 2013, 97, 15–22. [Google Scholar] [CrossRef]
- Cheng, J.; Kahn, R.L.; YaDeau, J.T.; Tsodikov, A.; Goytizolo, E.A.; Guheen, C.R.; Haskins, S.C.; Oxendine, J.A.; Allen, A.A.; Gulotta, L.V.; et al. The Fibromyalgia Survey Score Correlates with Preoperative Pain Phenotypes But Does Not Predict Pain Outcomes after Shoulder Arthroscopy. Clin. J. Pain 2016, 32, 689–694. [Google Scholar] [CrossRef]
- Westermann, R.W.; Anthony, C.A.; Bedard, N.; Glass, N.; Bollier, M.; Hettrich, C.M.; Wolf, B.R. Opioid Consumption After Rotator Cuff Repair. Arthroscopy 2017, 33, 1467–1472. [Google Scholar] [CrossRef]
- Rao, A.G.; Chan, P.H.; Prentice, H.A.; Paxton, E.W.; Navarro, R.A.; Dillon, M.T.; Singh, A. Risk factors for postoperative opioid use after elective shoulder arthroplasty. J. Shoulder Elb. Surg. 2018, 27, 1960–1968. [Google Scholar] [CrossRef]
- Trevisan, C.L.; Klumpp, R.; Recalcati, W.; Compagnoni, R. Influence of personality psychology on outcome of total hip arthroplasty: A cross-sectional study on 69 patients. Musculoskelet. Surg. 2015, 99, 231–236. [Google Scholar] [CrossRef]
| Widespread Pain Index (WPI) | ||||
| Left upper region (Region 1) □ | Right upper region (Region 2) □ | |||
| □ | Jaw * | □ | ||
| □ | Shoulder girdle | □ | ||
| □ | Upper arm | □ | ||
| □ | Lower arm | □ | ||
| Left lower region (Region 3) □ | Right lower region (Region 4) □ | |||
| □ | Hip (buttock, trochanter) | □ | ||
| □ | Upper leg | □ | ||
| □ | Lower leg | □ | ||
| Axial region (Region 5) | ||||
| Neck | □ | |||
| Upper back | □ | |||
| Lower back | □ | |||
| Chest or breast * | □ | |||
| Abdomen * | □ | |||
| Total score (0-19): ______ | ||||
| Symptom Severity Scale (SS) score | ||||
| 0 | 1 | 2 | 3 | |
| Fatigue | □ | □ | □ | □ |
| Waking unrefreshed | □ | □ | □ | □ |
| Cognitive symptoms | □ | □ | □ | □ |
| Present | ||||
| Headaches | □ | |||
| Pain/cramps in lower abdomen | □ | |||
| Depression | □ | |||
| Total score (0-12): ______ | ||||
| Author | Study Design | Sample Size | Type of Intervention | Outcomes | Conclusions | Follow-Up Time |
|---|---|---|---|---|---|---|
| Blonna et al. [24] | Retrospective observational | 286 patients, including 18 with fibromyalgia, of which 5 underwent surgery (11 joints) | Orthopedic evaluation for shoulder pain and shoulder surgery | Diagnosis of fibromyalgia, new OSS, SF-12, and global SOD score | Fibromyalgia may be a cause of failure in the treatment of concomitant painful shoulder. | 15 months (range: 12–27 months) |
| Cheng et al. [25] | Prospective observational | 100 patients | Any type of shoulder arthroscopy | Opioid consumption, pain scores, neuropathic pain (PainDETECT), physical functioning (PROMIS), Quality of Recovery-9 | A higher FSS does not correlate with postoperative opioid consumption, but with a lower 2nd-day postoperative Quality of Recovery-9 score. | 14 days |
| Westermann et al. [26] | Retrospective case control | 35,155 shoulder arthroscopies, including 7884 with myalgia or fibromyalgia | Arthroscopy for rotator cuff repair | Postoperative opioid prescriptions | Significantly more opioid prescriptions in fibromyalgia patients | 12 months |
| Rao et al. [27] | Retrospective large database analysis | 4243 surgery procedures in 3996 patients, including 92 with fibromyalgia | Elective shoulder arthroplasty | Postoperative opioid consumption | Higher opioid prescription in patients with fibromyalgia in the later rehabilitation period | 360 days |
| Newcastle–Ottawa Quality Assessment Scale | ||||||||
|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Outcome | ||||||
| Author | Representativeness of the Exposed Cohort | Selection of the Non-Exposed Cohort | Ascertainment of Exposure | Demonstration that Outcome of Interest Was Not Present at the Start of Study | Comparability of Cohorts on the Basis of the Design or Analysis | Assessment of Outcome | Was Follow-Up Long Enough for Outcome to Occur? | Adequacy of Follow Up of Cohorts |
| Blonna et al. [24] | Truly representative ★ | n/a | Surgical records ★ | Yes ★ | n/a | Self-reported outcomes and medical records ★ | Yes ★ | n/a |
| Cheng et al. [25] | Truly representative ★ | n/a | Surgical records ★ | Yes ★ | n/a | Self-reported outcomes and medical records ★ | No | n/a |
| Westermann et al. [26] | Fibromyalgia diagnosis based on ICD-9 | n/a | Surgical records ★ | Yes ★ | n/a | Medical records ★ | Yes ★ | n/a |
| Rao et al. [27] | No description of fibromyalgia criteria | n/a | Surgical records ★ | Yes ★ | n/a | Medical records ★ | Yes ★ | n/a |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Compagnoni, R.; Gualtierotti, R.; Luceri, F.; Sciancalepore, F.; Randelli, P.S. Fibromyalgia and Shoulder Surgery: A Systematic Review and a Critical Appraisal of the Literature. J. Clin. Med. 2019, 8, 1518. https://doi.org/10.3390/jcm8101518
Compagnoni R, Gualtierotti R, Luceri F, Sciancalepore F, Randelli PS. Fibromyalgia and Shoulder Surgery: A Systematic Review and a Critical Appraisal of the Literature. Journal of Clinical Medicine. 2019; 8(10):1518. https://doi.org/10.3390/jcm8101518
Chicago/Turabian StyleCompagnoni, Riccardo, Roberta Gualtierotti, Francesco Luceri, Fabio Sciancalepore, and Pietro Simone Randelli. 2019. "Fibromyalgia and Shoulder Surgery: A Systematic Review and a Critical Appraisal of the Literature" Journal of Clinical Medicine 8, no. 10: 1518. https://doi.org/10.3390/jcm8101518
APA StyleCompagnoni, R., Gualtierotti, R., Luceri, F., Sciancalepore, F., & Randelli, P. S. (2019). Fibromyalgia and Shoulder Surgery: A Systematic Review and a Critical Appraisal of the Literature. Journal of Clinical Medicine, 8(10), 1518. https://doi.org/10.3390/jcm8101518






