Acute Effects of Intermittent Versus Continuous Bilateral Ankle Plantar Flexor Static Stretching on Postural Sway and Plantar Pressures: A Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Procedures
3. Measures
3.1. Variables
3.2. Statistical Analysis
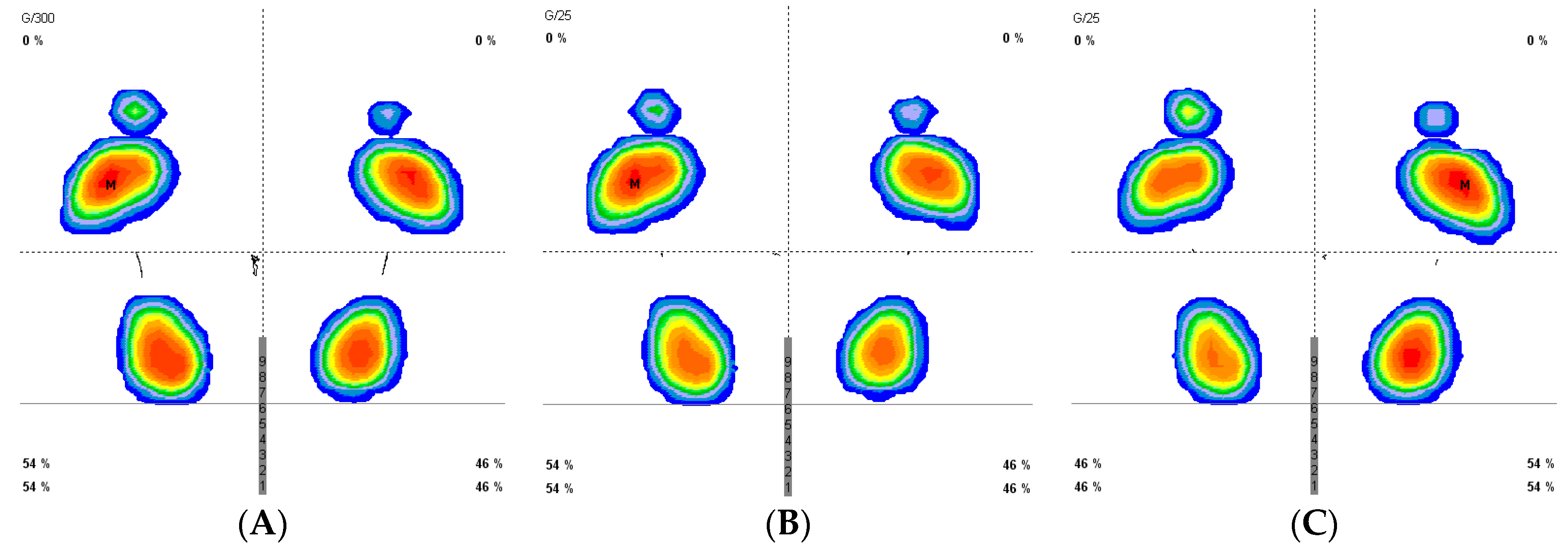
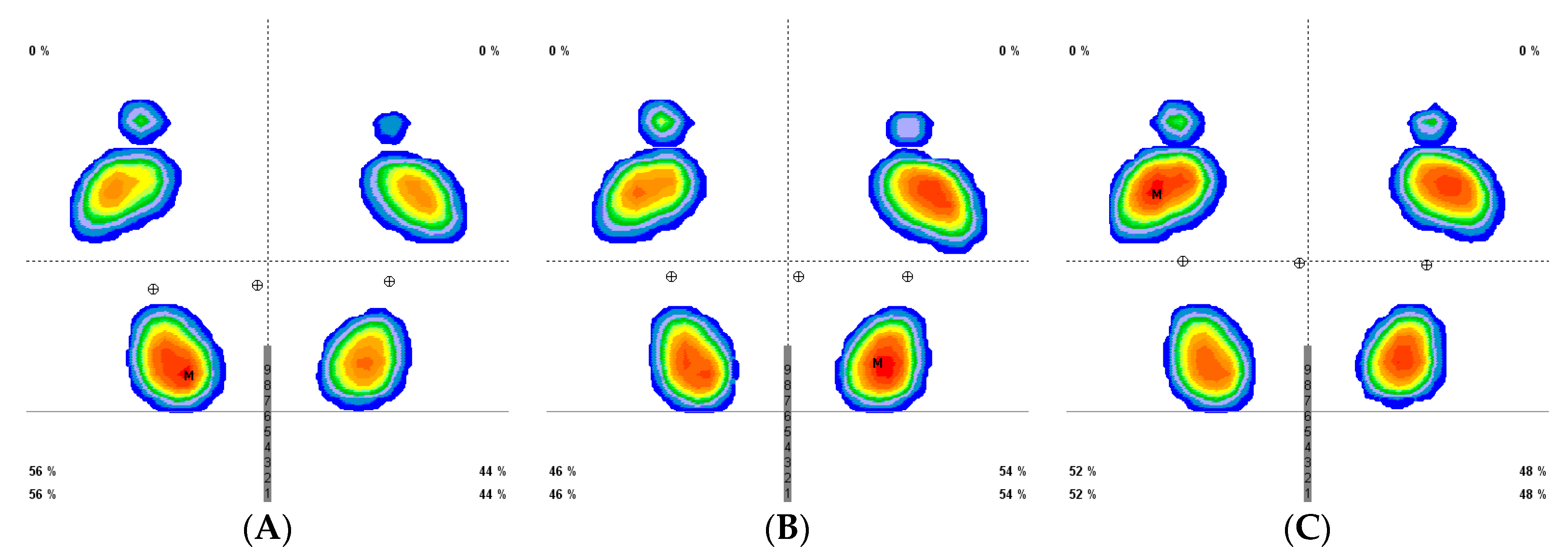
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- ©Falls. Available online: http://www.who.int/news-room/fact-sheets/detail/falls (accessed on 24 May 2018).
- Pua, Y.-H.; Ong, P.-H.; Clark, R.A.; Matcher, D.B.; Lim, E.C.W. Falls efficacy, postural balance, and risk for falls in older adults with falls-related emergency department visits: Prospective cohort study. BMC Geriatr. 2017, 17, 291. [Google Scholar] [CrossRef] [PubMed]
- Avela, J.; Finni, T.; Liikavainio, T.; Niemelä, E.; Komi, P.V. Neural and mechanical responses of the triceps surae muscle group after 1 h of repeated fast passive stretches. J. Appl. Physiol. 2004, 96, 2325–2332. [Google Scholar] [CrossRef] [PubMed]
- Trajano, G.S.; Nosaka, K.B.; Seitz, L.; Blazevich, A.J. Intermittent Stretch Reduces Force and Central Drive more than Continuous Stretch. Med. Sci. Sport Exerc. 2014, 46, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Reid, J.C.; Greene, R.; Young, J.D.; Hodgson, D.D.; Blazevich, A.J.; Behm, D.G. The effects of different durations of static stretching within a comprehensive warm-up on voluntary and evoked contractile properties. Eur. J. Appl. Physiol. 2018, 118, 1427–1445. [Google Scholar] [CrossRef] [PubMed]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. 2), ii7–ii11. [Google Scholar] [CrossRef] [PubMed]
- Jancová, J. Measuring the balance control system-review. Acta Med. 2008, 51, 129–137. [Google Scholar] [CrossRef]
- Muehlbauer, T.; Gollhofer, A.; Granacher, U. Relationship Between Measures of Balance and Strength in Middle-Aged Adults. J. Strength Cond. Res. 2012, 26, 2401–2407. [Google Scholar] [CrossRef] [PubMed]
- Behm, D.G.; Bambury, A.; Cahill, F.; Power, K. Effect of acute static stretching on force, balance, reaction time, and movement time. Med. Sci. Sports Exerc. 2004, 36, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.B.P.; Graves, B.B.S.; Whitehurst, M.; Jacobs, P.L. The Acute Effects of Different Durations of Static Stretching on Dynamic Balance Performance. Strength Cond. 2009, 23, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.-I.; Nam, H.-C.; Jung, K.-S. Effects on Hamstring Muscle Extensibility, Muscle Activity, and Balance of Different Stretching Techniques. J. Phys. Ther. Sci. 2014, 26, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Chatzopoulos, D.; Galazoulas, C.; Patikas, D.; Kotzamanidis, C. Acute effects of static and dynamic stretching on balance, agility, reaction time and movement time. J. Sports Sci. Med. 2014, 13, 403–409. [Google Scholar]
- Leblebici, H.; Yarar, H.; Aydın, E.M.; Zorlu, Z.; Ertaş, U.; Kıngır, M.E. The Acute Effects of Different Stretching on Dynamic Balance Performance. Int. J. Sport Stud. 2017, 7, 2251–7502. [Google Scholar]
- Gribble, P.A.; Hertel, J. Effect of hip and ankle muscle fatigue on unipedal postural control. J. Electromyogr. Kinesiol. 2004, 14, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanz, D.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Martínez-Jiménez, E.M.; Muñoz-García, D.; Pérez-Boal, E.; Calvo-Lobo, C.; López-López, D. Effects of Compressive Stockings and Standard Stockings in Skin Temperature and Pressure Pain Threshold in Runners with Functional Ankle Equinus Condition. J. Clin. Med. 2018, 7, 454. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanz, D.; Becerro-de-Bengoa-Vallejo, R.; López-López, D.; Calvo-Lobo, C.; Martínez Jiménez, E.M.; Perez-Boal, E.; Losa-Iglesias, M.E.; Palomo-López, P. Slow velocity of the center of pressure and high heel pressures may increase the risk of Sever’s disease: A case-control study. BMC Pediatr. 2018, 18, 357. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Sanz, D.; Losa-Iglesias, M.E.; Becerro de Bengoa-Vallejo, R.; Palomo-Lopez, P.; Beltran-Alacreu, H.; Calvo-Lobo, C.; Navarro-Flores, E.; Lopez-Lopez, D. Skin temperature in youth soccer players with functional equinus and non-equinus condition after running. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 2020–2024. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanz, D.; Losa-Iglesias, M.E.; López-López, D.; Calvo-Lobo, C.; Palomo-López, P.; Becerro-de-Bengoa-Vallejo, R. Infrared thermography applied to lower limb muscles in elite soccer players with functional ankle equinus and non-equinus condition. PeerJ 2017, 5, e3388. [Google Scholar] [CrossRef]
- Romero Morales, C.; Calvo Lobo, C.; Rodríguez Sanz, D.; Sanz Corbalán, I.; Ruiz Ruiz, B.; López López, D. The concurrent validity and reliability of the Leg Motion system for measuring ankle dorsiflexion range of motion in older adults. PeerJ 2017, 5, e2820. [Google Scholar] [CrossRef]
- Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Rodriguez-Sanz, D. Static and dynamic plantar pressures in children with and without sever disease: A case-control study. Phys. Ther. 2014, 94, 818–826. [Google Scholar] [CrossRef]
- Becerro de Bengoa Vallejo, R.; Losa Iglesias, M.E.; Rodríguez Sanz, D.; Prados Frutos, J.C.; Salvadores Fuentes, P.; Chicharro, J.L. Plantar pressures in children with and without sever’s disease. J. Am. Podiatr. Med. Assoc. 2011, 101, 17–24. [Google Scholar] [CrossRef]
- Lima, B.N.; Lucareli, P.R.G.; Gomes, W.A.; Silva, J.J.; Bley, A.S.; Hartigan, E.H.; Marchetti, P.H. The Acute Effects of Unilateral Ankle Plantar Flexors Static-Stretching on Postural Sway and Gastrocnemius Muscle Activity during Single-Leg Balance Tasks. J. Sport Sci. Med. 2014, 13, 564–570. [Google Scholar]
- Padgett, P.K.; Jacobs, J.V.; Kasser, S.L. Is the BESTest at Its Best? A Suggested Brief Version Based on Interrater Reliability, Validity, Internal Consistency, and Theoretical Construct. Phys. Ther. 2012, 92, 1197–1207. [Google Scholar] [CrossRef] [PubMed]
- Scharfbillig, R.; Scutter, S.D. Measurement of foot dorsiflexion: A modified Lidcombe template. J. Am. Podiatr. Med. Assoc. 2004, 94, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.L.; McPoil, T.G. Reliability of Ankle Goniometric Measurements. J. Am. Podiatr. Med. Assoc. 2005, 95, 564–572. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, M.; Lee, Y.J.; Aruin, A.S. The effect of lateral or medial wedges on control of postural sway in standing. Gait Posture 2014, 39, 899–903. [Google Scholar] [CrossRef] [PubMed]
- Dudek, K.; Drużbicki, M.; Przysada, G.; Śpiewak, D. Assessment of standing balance in patients after ankle fractures. Acta Bioeng. Biomech. 2014, 16, 59–65. [Google Scholar]
- Shim, J.-M.; Jung, J.-H.; Kim, H.-H. The effects of plantar flexor static stretching and dynamic stretching using an aero-step on foot pressure during gait in healthy adults: A preliminary study. J. Phys. Ther. Sci. 2015, 27, 2155–2157. [Google Scholar] [CrossRef]
- Babault, N.; Kouassi, B.Y.L.; Desbrosses, K. Acute effects of 15 min static or contract-relax stretching modalities on plantar flexors neuromuscular properties. J. Sci. Med. Sport 2010, 13, 247–252. [Google Scholar] [CrossRef]
- Zito, M.; Driver, D.; Parker, C.; Bohannon, R. Lasting effects of one bout of two 15 s passive stretches on ankle dorsiflexion range of motion. J. Orthop. Sports Phys. Ther. 1997, 26, 214–221. [Google Scholar] [CrossRef]
- Behm, D.G.; Kibele, A. Effects of differing intensities of static stretching on jump performance. Eur. J. Appl. Physiol. 2007, 101, 587–594. [Google Scholar] [CrossRef]
- Yoo, S.D.; Kim, H.S.; Lee, J.H.; Yun, D.H.; Kim, D.H.; Chon, J.; Lee, S.A.; Han, Y.J.; Soh, Y.S.; Kim, Y.; et al. Biomechanical Parameters in Plantar Fasciitis Measured by Gait Analysis System With Pressure Sensor. Ann. Rehabil. Med. 2017, 41, 979–989. [Google Scholar] [CrossRef]
- Downey, M.; Banks, A. Gastrocnemius recession in the treatment of nonspastic ankle equinus. A retrospective study. J. Am. Podiatr. Med. Assoc. 1989, 79, 159–174. [Google Scholar] [CrossRef]
- Gajdosik, R.L.; Vander Linden, D.W.; McNair, P.J.; Williams, A.K.; Riggin, T.J. Effects of an eight-week stretching program on the passive-elastic properties and function of the calf muscles of older women. Clin. Biomech. 2005, 20, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.-Y.; Tsai, K.-H.; Chen, J.-J. Effects of Prolonged Muscle Stretching With Constant Torque or Constant Angle on Hypertonic Calf Muscles. Arch. Phys. Med. Rehabil. 2005, 86, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Nordez, A.; McNair, P.; Casari, P.; Cornu, C. Acute Changes in Hamstrings Musculo-Articular Dissipative Properties Induced by Cyclic and Static Stretching. Int. J. Sports Med. 2008, 29, 414–418. [Google Scholar] [CrossRef]
- McNair, P.J.; Dombroski, E.W.; Hewson, D.J.; Stanley, S.N. Stretching at the ankle joint: Viscoelastic responses to holds and continuous passive motion. Med. Sci. Sports Exerc. 2001, 33, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Fernando, M.E.; Crowther, R.G.; Lazzarini, P.A.; Sangla, K.S.; Wearing, S.; Buttner, P.; Golledge, J. Plantar pressures are higher in cases with diabetic foot ulcers compared to controls despite a longer stance phase duration. BMC Endocr. Disord. 2016, 16, 51. [Google Scholar] [CrossRef]
- Cortina, R.E.; Morris, B.L.; Vopat, B.G. Gastrocnemius Recession for Metatarsalgia. Foot Ankle Clin. 2018, 23, 57–68. [Google Scholar] [CrossRef]
- Munteanu, S.E.; Barton, C.J. Lower limb biomechanics during running in individuals with achilles tendinopathy: A systematic review. J. Foot Ankle Res. 2011, 4, 15. [Google Scholar] [CrossRef]
- Morrin, N.; Redding, E. Acute effects of warm-up stretch protocols on balance, vertical jump height, and range of motion in dancers. J. Dance Med. Sci. 2013, 17, 34–40. [Google Scholar] [CrossRef]
- Bouvier, T.; Opplert, J.; Cometti, C.; Babault, N. Acute effects of static stretching on muscle–tendon mechanics of quadriceps and plantar flexor muscles. Eur. J. Appl. Physiol. 2017, 117, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Anson, J.; Waddington, G.; Adams, R.; Liu, Y. The Role of Ankle Proprioception for Balance Control in relation to Sports Performance and Injury. Biomed. Res. Int. 2015, 2015, 1–8. [Google Scholar] [CrossRef] [PubMed]
| Variable Total (n = 24) | Total Group Mean ± SD (CI 95%) | Continuous Group Mean ± SD (CI 95%) | Intermittent Group Mean ± SD (CI 95%) | p-Value * |
|---|---|---|---|---|
| Age (years) | 32.12 ± 7.60 (29.08–35.16) | 32.20 ± 8.08 (28.97–35.44) | 32.04 ± 7.28 (29.18–34.89) | 0.940 |
| Weight (kg) | 62.72 ± 8.97 (59.14–66.31) | 62.77 ± 9.52 (58.96–66.57) | 62.68 ± 8.58 (59.32–66.05) | 0.975 |
| Height (cm) | 166.64 ± 8.13 (163.39–169.90) | 166.20 ± 8.43 (162.83–169.58) | 167.08 ± 7.98 (163.95–170.21) | 0.714 |
| BMI (kg/m2) | 22.58 ± 2.75 (21.48–23.69) | 22.71 ± 2.90 (21.55–23.87) | 22.46 ± 2.66 (21.41–23.50) | 0.753 |
| Size of shoe | 38.87 ± 2.32 (37.94–39.80) | 38.81 ± 2.26 (37.90–39.72) | 38.93 ± 2.43 (37.98–39.89) | 0.855 |
| Specification | Description |
|---|---|
| Size (length × width × height) | 530 × 600 × 45 mm |
| Thickness | 4 mm |
| Active surface | 400 × 400 mm |
| Weight | 6.8 kg |
| Sensors | Calibrated resistive |
| Sensor | 8 × 8 mm |
| Sensor thickness | 0.15 mm |
| No. of sensors | 2304 (48 × 48) |
| Permissible temperature | −40 °C to 85 °C |
| Sensor pressure (minimum/maximum) | 0.4 N/m2 (0.0004 kPa)/100 N/m2 (0.1 kPa) |
| Type of PC interface/platform | Universal Serial Bus (USB) |
| Supply | USB cable |
| Data acquisition frequency | 200 images/s |
| Vertical force recording | 60 Hz |
| Operating system required | Windows XP, Vista, or 7 |
| Variable | Intermittent Group Pretest Values (n = 20) Mean ± SD (CI 95%) | Continuous Group Pretest Values (n = 20) Mean ± SD (CI 95%) | p-value * |
|---|---|---|---|
| Rearfoot maximum pressure (kPa) | 106.24 ± 21.36 (97.00–115.48) | 105.52 ± 24.08 (95.02–105.93) | 0.918 |
| Rearfoot medium pressure (kPa) | 39.61 ± 6.51 (36.79–42.43) | 41.59 ± 8.96 (37.71–45.46) | 0.483 |
| Rearfoot surface (cm2) | 85.84 ± 10.51 (81.30–90.39) | 84.71 ± 10.33 (80.25–89.18) | 0.828 |
| Midfoot maximum pressure (kPa) | 13.05 ± 14.82 (6.64–19.46) | 11.18 ± 11.69 (6.12–16.23) | 0.865 |
| Midfoot medium pressure (kPa) | 5.72 ± 6.10 (3.08–8.36) | 5.63 ± 5.68 (3.17–8.09) | 0.966 |
| Midfoot surface (cm2) | 16.71 ± 19.08 (8.46–24.96) | 17.93 ± 20.07 (9.25–26.61) | 0.787 |
| Forefoot maximum pressure (kPa) | 69.41 ± 13.19 (63.71–75.12) | 70.16 ± 10.36 (65.68–74.64) | 0.606 |
| Forefoot medium pressure (kPa) | 25.54 ± 6.07 (22.91–28.16) | 25.23 ± 2.77 (24.03–26.43) | 0.338 |
| Forefoot surface(cm2) | 94.15 ± 17.75 (86.47–101.82) | 90.02 ± 12.02 (84.81–95.22) | 0.496 |
| X displacement eyes open (mm) | 6.91 ± 6.14 (4.26–9.57) | 8.34 ± 9.01 (6.49–10.19) | 0.083 |
| Y displacement eyes open (mm) | 16.68 ± 9.89 (12.40–20.95) | 19.32 ± 9.01 (15.43–23.22) | 0.359 |
| Surface Eyes Open (mm2) | 13.35 ± 9.58 (9.21–17.50) | 9.83 ± 7.12 (6.75–12.92) | 0.180 |
| Medium speed of the laterolateral displacement. Eyes open (mm/s) | 1.20 ± 0.27 (1.08–1.32) | 1.16 ± 0.28 (1.03–1.28) | 0.657 |
| Medium speed of the anteroposterior displacement. Eyes open (mm/s) | 0.98 ± 0.26 (0.87–1.10) | 1.04 ± 0.39 (0.87–1.21) | 0.542 |
| X displacement eyes closed (mm) | 7.74 ± 5.05 (5.55–9.92) | 7.61 ± 4.40 (5.71–9.52) | 0.926 |
| Y displacement eyes closed (mm) | 17.08 ± 9.93 (12.78–21.37) | 21.34 ± 9.46 (17.24–25.43) | 0.164 |
| Surface eyes closed (mm2) | 25.96 ± 14.77 (19.57–32.34) | 32.44 ± 52.54 (9.71–55.16) | 0.599 |
| Medium speed of the laterolateral displacement. Eyes closed (mm/s) | 1.39 ± 0.36 (1.23–1.55) | 1.37 ± 0.42 (1.19–1.56) | 0.788 |
| Medium speed of the anteroposterior displacement. Eyes closed (mm/s) | 1.48 ± 0.58 (1.22–1.73) | 1.41 ± 0.70 (1.10–1.72) | 0.332 |
| Variable | Intermittent Group Posttest Values (n = 20) Mean ± SD (CI 95%) | Continuous Group Posttest Values (n = 20) Mean ± SD (CI 95%) | p-Value * |
|---|---|---|---|
| Rearfoot maximum pressure (kPa) | 87.56 ± 22.77 (77.71–97.41) | 99.39 ± 18.76 (91.28–107.51) | 0.019 |
| Rearfoot medium pressure (kPa) | 33.84 ± 7.44 (30.62–37.06) | 37.19 ± 5.38 (34.86–39.51) | 0.105 |
| Rearfoot surface (cm2) | 81.86 ± 12.11 (76.62–87.10) | 83.54 ± 13.11 (77.87–89.21) | 0.703 |
| Midfoot maximum pressure (kPa) | 14.73 ± 13.98 (8.68–20.78) | 15.58 ± 14.85 (9.16–22.01) | 0.983 |
| Midfoot medium pressure (kPa) | 7.05 ± 6.55 (4.21–9.88) | 7.54 ± 6.22 (4.85–10.23) | 0.761 |
| Midfoot surface (cm2) | 20.78 ± 18.67 (12.70–28.85) | 20.56 ± 19.08 (12.31–28.81) | 0.957 |
| Forefoot maximum pressure (kPa) | 74.16 ± 15.62 (67.41–80.92) | 73.14 ± 15.38 (66.48–79.79) | 0.332 |
| Forefoot medium pressure (kPa) | 26.98 ± 4.29 (25.12–28.84) | 26.72 ± 6.73 (23.81–29.63) | 0.322 |
| Forefoot surface (cm2) | 105.23 ± 18.32) (97.31–113.16) | 97.36 ± 12.98 (91.75–102.98) | 0.038 |
| X displacement eyes open (mm) | 8.48 ± 5.23 (6.22–10.75) | 7.32 ± 4.89 (5.20–9.44) | 0.353 |
| Y displacement eyes open (mm) | 15.89 ± 8.39 (12.26–19.51) | 18.29 ± 10.84 (13.60–22.98) | 0.409 |
| Surface eyes open (mm2) | 6.34 ± 4.08 (4.57–8.10) | 11.02 ± 8.58 (7.31–14.74) | 0.031 |
| Medium speed of the laterolateral displacement. Eyes open (mm/s) | 1.19 ± 0.31 (1.05–1.32) | 1.35 ± 0.71 (1.04–1.66) | 0.910 |
| Medium speed of the anteroposterior displacement. Eyes open (mm/s) | 1.15 ± 0.65 (0.87–1.43) | 1.02 ± 0.57 (0.77–1.27) | 0.474 |
| X displacement eyes closed (mm) | 7.97 ± 5.86 (5.43–10.50) | 6.51 ± 4.09 (4.74–8.29) | 0.557 |
| Y displacement eyes closed (mm) | 15.54 ± 9.53 (11.42–19.66) | 16.90 ± 9.62 (12.74–21.06) | 0.640 |
| Surface eyes closed (mm2) | 18.24 ± 12.29 (12.93–23.56) | 23.17 ± 16.36 (16.09–30.24) | 0.167 |
| Medium speed of the laterolateral displacement. Eyes closed (mm/s) | 1.54 ± 0.47 (1.34–1.75) | 1.43 ± 0.85 (1.07–1.80) | 0.051 |
| Medium speed of the anteroposterior displacement. Eyes closed (mm/s) | 1.79 ± 0.87 (1.42–2.17) | 1.89 ± 2.31 (0.89–2.89) | 0.083 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Jiménez, E.M.; Losa-Iglesias, M.E.; Díaz-Velázquez, J.I.; Becerro-De-Bengoa-Vallejo, R.; Palomo-López, P.; Calvo-Lobo, C.; López-López, D.; Rodríguez-Sanz, D. Acute Effects of Intermittent Versus Continuous Bilateral Ankle Plantar Flexor Static Stretching on Postural Sway and Plantar Pressures: A Randomized Clinical Trial. J. Clin. Med. 2019, 8, 52. https://doi.org/10.3390/jcm8010052
Martínez-Jiménez EM, Losa-Iglesias ME, Díaz-Velázquez JI, Becerro-De-Bengoa-Vallejo R, Palomo-López P, Calvo-Lobo C, López-López D, Rodríguez-Sanz D. Acute Effects of Intermittent Versus Continuous Bilateral Ankle Plantar Flexor Static Stretching on Postural Sway and Plantar Pressures: A Randomized Clinical Trial. Journal of Clinical Medicine. 2019; 8(1):52. https://doi.org/10.3390/jcm8010052
Chicago/Turabian StyleMartínez-Jiménez, Eva María, Marta Elena Losa-Iglesias, Jose Ignacio Díaz-Velázquez, Ricardo Becerro-De-Bengoa-Vallejo, Patricia Palomo-López, César Calvo-Lobo, Daniel López-López, and David Rodríguez-Sanz. 2019. "Acute Effects of Intermittent Versus Continuous Bilateral Ankle Plantar Flexor Static Stretching on Postural Sway and Plantar Pressures: A Randomized Clinical Trial" Journal of Clinical Medicine 8, no. 1: 52. https://doi.org/10.3390/jcm8010052
APA StyleMartínez-Jiménez, E. M., Losa-Iglesias, M. E., Díaz-Velázquez, J. I., Becerro-De-Bengoa-Vallejo, R., Palomo-López, P., Calvo-Lobo, C., López-López, D., & Rodríguez-Sanz, D. (2019). Acute Effects of Intermittent Versus Continuous Bilateral Ankle Plantar Flexor Static Stretching on Postural Sway and Plantar Pressures: A Randomized Clinical Trial. Journal of Clinical Medicine, 8(1), 52. https://doi.org/10.3390/jcm8010052








