Long-Term Outcomes in Patients with Incident Chronic Obstructive Pulmonary Disease after Acute Kidney Injury: A Competing-Risk Analysis of a Nationwide Cohort
Abstract
1. Introduction
2. Methods
2.1. Data Sources
2.2. Study Group
2.3. Baseline Characteristics
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
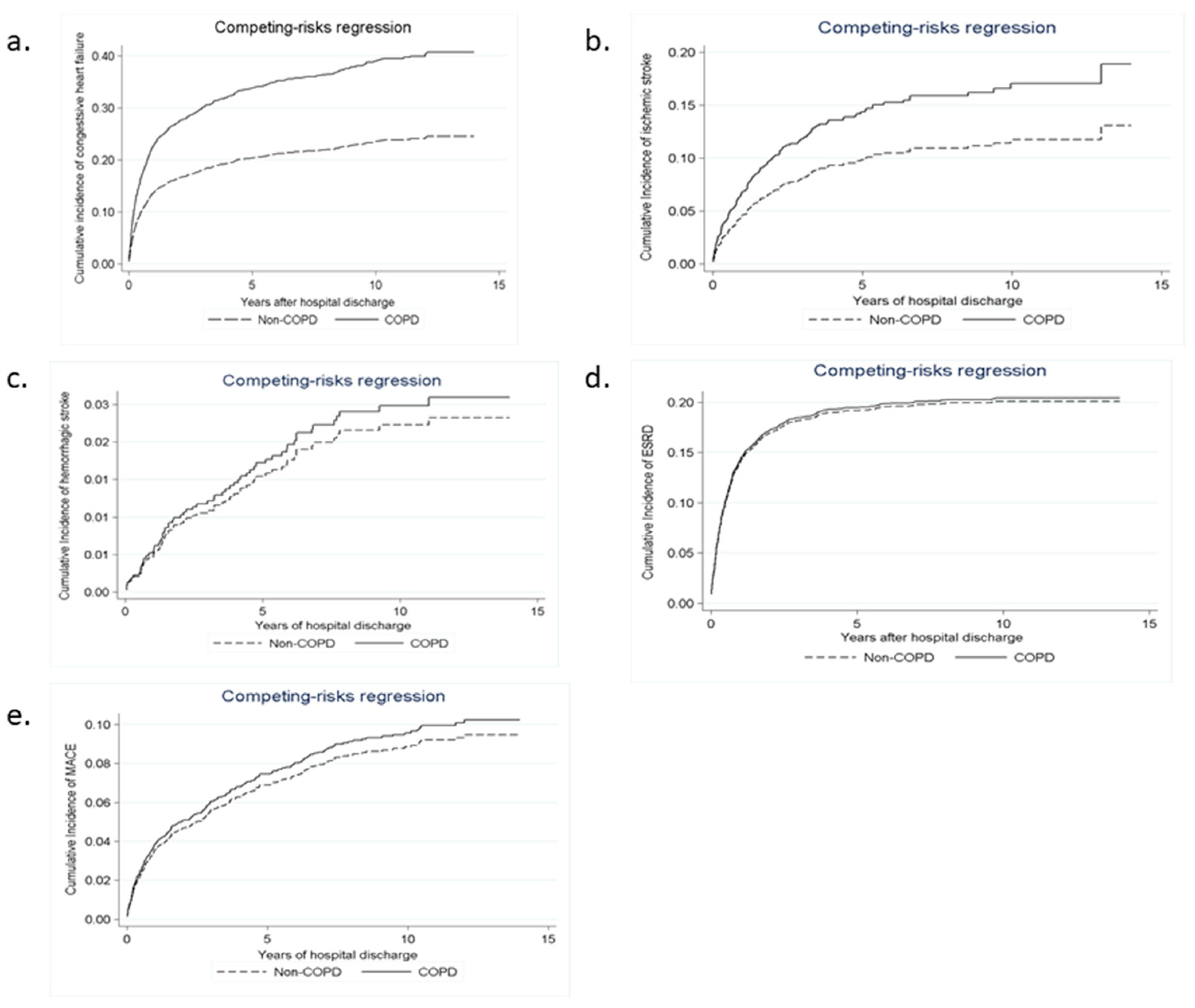
3.2. Long-Term Risks of Death, Stroke, and CHF
3.3. Long-Term Risks of MACE and ESRD
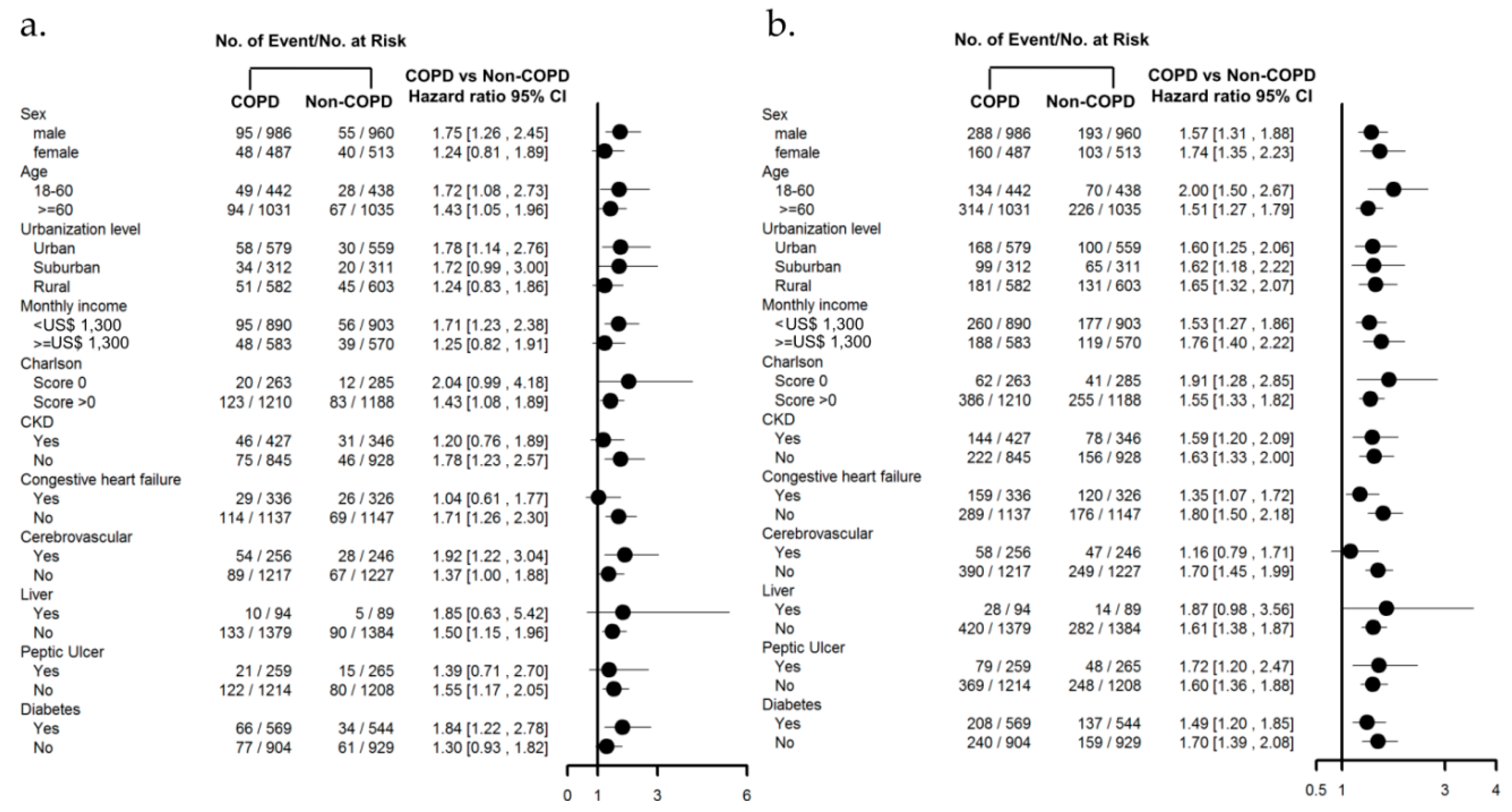
3.4. Subgroup Analysis with Comorbidities
4. Discussion
4.1. Risk of COPD after AKI-D
4.2. Stroke Risk in Patients with COPD after AKI-D
4.3. CHF Risk in Patients with COPD after AKI-D
4.4. Risk of MI and ESRD in Patients with COPD after AKI-D
4.5. Care of Patients with COPD after AKI-D
4.6. Limitation and Strength
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ali, T.; Khan, I.; Simpson, W.; Prescott, G.; Townend, J.; Smith, W.; Macleod, A. Incidence and outcomes in acute kidney injury: A comprehensive population-based study. J. Am. Soc. Nephrol. 2007, 18, 1292–1298. [Google Scholar] [CrossRef] [PubMed]
- Liangos, O.; Wald, R.; O’Bell, J.W.; Price, L.; Pereira, B.J.; Jaber, B.L. Epidemiology and outcomes of acute renal failure in hospitalized patients: A national survey. Clin. J. Am. Soc. Nephrol. 2006, 1, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Ishani, A.; Xue, J.L.; Himmelfarb, J.; Eggers, P.W.; Kimmel, P.L.; Molitoris, B.A.; Collins, A.J. Acute kidney injury increases risk of ESRD among elderly. J. Am. Soc. Nephrol. 2009, 20, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Waikar, S.S.; Winkelmayer, W.C. Chronic on acute renal failure: Long-term implications of severe acute kidney injury. JAMA 2009, 302, 1227–1229. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Wu, C.H.; Huang, T.M.; Wang, C.Y.; Lai, C.F.; Shiao, C.C.; Chang, C.H.; Lin, S.L.; Chen, Y.Y.; Chen, Y.M.; et al. Long-term risk of coronary events after AKI. J. Am. Soc. Nephrol. 2014, 25, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Wu, P.C.; Wu, C.H.; Huang, T.M.; Chang, C.H.; Tsai, P.R.; Ko, W.J.; Chen, L.; Wang, C.Y.; Chu, T.S.; et al. The impact of acute kidney injury on the long-term risk of stroke. J. Am. Heart Assoc. 2014, 3, e000933. [Google Scholar] [CrossRef] [PubMed]
- Husain-Syed, F.; McCullough, P.A.; Birk, H.W.; Renker, M.; Brocca, A.; Seeger, W.; Ronco, C. Cardio-pulmonary-renal interactions: A multidisciplinary approach. J. Am. Coll. Cardiol. 2015, 65, 2433–2448. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Shiao, C.C.; Chang, C.H.; Huang, T.M.; Lai, C.F.; Lin, M.C.; Chiang, W.C.; Chu, T.S.; Wu, K.D.; Ko, W.J.; et al. Long-term outcomes after dialysis-requiring acute kidney injury. Biomed. Res. Int. 2014, 2014, 365186. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, S.L.; Jaber, B.L.; Faubel, S.; Chawla, L.S.; Acute Kidney Injury Advisory Group of American Society of Nephrology. AKI transition of care: A potential opportunity to detect and prevent CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Attanasio, C.; Latancia, M.T.; Otterbein, L.E.; Netti, P.A. Update on renal replacement therapy: Implantable artificial devices and bioengineered organs. Tissue Eng. Part B Rev. 2016, 22, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Anthonisen, N.R.; Connett, J.E.; Enright, P.L.; Manfreda, J.; Lung Health Study Research Group. Hospitalizations and mortality in the lung health study. Am. J. Respir. Crit. Care Med. 2002, 166, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Hansell, A.L.; Walk, J.A.; Soriano, J.B. What do chronic obstructive pulmonary disease patients die from? A multiple cause coding analysis. Eur. Respir. J. 2003, 22, 809–814. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Liao, K.M. Chronic obstructive pulmonary disease is associated with risk of chronic kidney disease: A nationwide case-cohort study. Sci. Rep. 2016, 6, 25855. [Google Scholar] [CrossRef] [PubMed]
- Virzi, G.; Day, S.; de Cal, M.; Vescovo, G.; Ronco, C. Heart-kidney crosstalk and role of humoral signaling in critical illness. Crit. Care 2014, 18, 201. [Google Scholar] [CrossRef] [PubMed]
- Andres-Hernando, A.; Altmann, C.; Bhargava, R.; Okamura, K.; Bacalja, J.; Hunter, B.; Ahuja, N.; Soranno, D.; Faubel, S. Prolonged acute kidney injury exacerbates lung inflammation at 7 days post-acute kidney injury. Physiol. Rep. 2014, 2, e12084. [Google Scholar] [CrossRef] [PubMed]
- Chawla, L.S.; Bellomo, R.; Bihorac, A.; Goldstein, S.L.; Siew, E.D.; Bagshaw, S.M.; Bittleman, D.; Cruz, D.; Endre, Z.; Fitzgerald, R.L.; et al. Acute kidney disease and renal recovery: Consensus report of the acute disease quality initiative (ADQI) 16 workgroup. Nat. Rev. Nephrol. 2017, 13, 241–257. [Google Scholar] [CrossRef] [PubMed]
- Chao, C.T.; Hou, C.C.; Wu, V.C.; Lu, H.M.; Wang, C.Y.; Chen, L.; Kao, T.W. The impact of dialysis-requiring acute kidney injury on long-term prognosis of patients requiring prolonged mechanical ventilation: Nationwide population-based study. PLoS ONE 2012, 7, e50675. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.J.; Chao, C.T.; Huang, Y.C.; Wang, C.Y.; Chang, C.H.; Huang, T.M.; Lai, C.F.; Huang, H.Y.; Shiao, C.C.; Chu, T.S.; et al. The impact of acute kidney injury with temporary dialysis on the risk of fracture. J. Bone Miner. Res. 2013, 29, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.C.; Wu, C.J.; Lin, C.J.; Wu, V.C.; National Taiwan University Study Group on Acute Renal Failure Group. Long-term risk of upper gastrointestinal hemorrhage after advanced AKI. Clin. J. Am. Soc. Nephrol. 2015, 10, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Li, C.H.; Chen, W.C.; Liao, W.C.; Tu, C.Y.; Lin, C.L.; Sung, F.C.; Chen, C.H.; Hsu, W.H. The association between chronic obstructive pulmonary disease and Parkinson’s disease: A nationwide population-based retrospective cohort study. QJM 2015, 108, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.Y.; Jian, Z.H.; Nfor, O.N.; Ku, W.Y.; Ko, P.C.; Lung, C.C.; Ho, C.C.; Pan, H.H.; Huang, C.Y.; Liang, Y.C.; et al. The effects of pulmonary diseases on histologic types of lung cancer in both sexes: A population-based study in Taiwan. BMC Cancer 2015, 15, 834. [Google Scholar] [CrossRef] [PubMed]
- Liao, K.M.; Chen, C.Y. Incidence and risk factors of atrial fibrillation in Asian COPD patients. Int. J. Chron. Obstruct. Pulmon. Dis. 2017, 12, 2523–2530. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Hu, Y.H.; Wu, C.H.; Kao, C.C.; Wang, C.Y.; Yang, W.S.; Lee, H.H.; Chang, Y.S.; Lin, Y.H.; Wang, S.M.; et al. Administrative data on diagnosis and mineralocorticoid receptor antagonist prescription identified patients with primary aldosteronism in Taiwan. J. Clin. Epidemiol. 2014, 67, 1139–1149. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.S.; Lai, M.S.; Gau, S.S.; Wang, S.C.; Tsai, H.J. Concordance between patient self-reports and claims data on clinical diagnoses, medication use, and health system utilization in Taiwan. PLoS ONE 2014, 9, e112257. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.T.; Wu, S.C.; Lee, Y.C.; Lai, M.S.; Tam, S.C. Assessing measures of comorbidity using national health insurance databases. Taiwan J. Public Health 2010, 29, 191–200. [Google Scholar]
- Cheng, C.L.; Kao, Y.H.; Lin, S.J.; Lee, C.H.; Lai, M.L. Validation of the national health insurance research database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug Saf. 2011, 20, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.H.; Yang, Y.W.; Hung, S.C.; Kuo, K.L.; Wu, K.D.; Wu, V.C.; Hsieh, T.C.; National Taiwan University Study Group on Acute Renal Failure. Ketoanalogues supplementation decreases dialysis and mortality risk in patients with anemic advanced chronic kidney disease. PLoS ONE 2017, 12, e0176847. [Google Scholar]
- Ou, S.M.; Chen, Y.T.; Chao, P.W.; Lee, Y.J.; Liu, C.J.; Yeh, C.M.; Chen, T.J.; Chen, T.W.; Yang, W.C.; Li, S.Y. Nonsteroidal anti-inflammatory drug use is associated with cancer risk reduction in chronic dialysis patients. Kidney Int. 2013, 84, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.J.; Bai, C.H.; Yeh, W.T.; Chiu, H.C.; Pan, W.H. Influence of metabolic syndrome and general obesity on the risk of ischemic stroke. Stroke 2006, 37, 1060–1064. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Lee, W.Y.; Yang, J.; Lo, J.C.; Gurwitz, J.H. Statin therapy and risks for death and hospitalization in chronic heart failure. JAMA 2006, 296, 2105–2111. [Google Scholar] [CrossRef] [PubMed]
- Kip, K.E.; Hollabaugh, K.; Marroquin, O.C.; Williams, D.O. The problem with composite end points in cardiovascular studies: The story of major adverse cardiac events and percutaneous coronary intervention. J. Am. Coll. Cardiol. 2008, 51, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Chang, C.H.; Wang, C.Y.; Lin, Y.H.; Kao, T.W.; Lin, P.C.; Chu, T.S.; Chang, Y.S.; Chen, L.; Wu, K.D.; et al. Risk of fracture in primary aldosteronism: A population-based cohort study. J. Bone Miner. Res. 2017, 32, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Chueh, S.J.; Chen, L.; Chang, C.H.; Hu, Y.H.; Lin, Y.H.; Wu, K.D.; Yang, W.S.; Taiwan Primary Aldosteronism Investigation Study Group. Risk of new-onset diabetes mellitus in primary aldosteronism: A population study over 5 years. J. Hypertens. 2017, 35, 1698–1708. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Abajobir, A.A.; Abate, K.H.; Abera, S.F.; Agrawal, A.; Ahmed, M.B.; Aichour, A.N.; Aichour, I.; Aichour, M.T.E.; Alam, K.; et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet Respi. Med. 2017, 5, 691–706. [Google Scholar] [CrossRef]
- Baty, F.; Putora, P.M.; Isenring, B.; Blum, T.; Brutsche, M. Comorbidities and burden of COPD: A population based case-control study. PLoS ONE 2013, 8, e63285. [Google Scholar] [CrossRef] [PubMed]
- Faubel, S.; Edelstein, C.L. Mechanisms and mediators of lung injury after acute kidney injury. Nat. Rev. Nephrol. 2016, 12, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Lie, M.L.; White, L.E.; Santora, R.J.; Park, J.M.; Rabb, H.; Hassoun, H.T. Lung T lymphocyte trafficking and activation during ischemic acute kidney injury. J. Immunol. 2012, 189, 2843–2851. [Google Scholar] [CrossRef] [PubMed]
- Altmann, C.; Andres-Hernando, A.; McMahan, R.H.; Ahuja, N.; He, Z.; Rivard, C.J.; Edelstein, C.L.; Barthel, L.; Janssen, W.J.; Faubel, S. Macrophages mediate lung inflammation in a mouse model of ischemic acute kidney injury. Am. J. Physiol. Ren. Physiol. 2012, 302, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Caramori, G.; Adcock, I.M.; Di Stefano, A.; Chung, K.F. Cytokine inhibition in the treatment of COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2014, 9, 397–412. [Google Scholar] [PubMed]
- Pandey, K.C.; De, S.; Mishra, P.K. Role of proteases in chronic obstructive pulmonary disease. Front. Pharmacol. 2017, 8, 512. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Aguilar, N.E.; Vargas-Camano, M.E.; Hernandez-Pliego, R.R.; Chaia-Semerena, G.M.; Perez-Chavira, M.R. Immunopathology of chronic obstructive pulmonary disease. Rev. Alerg. Mex. 2017, 64, 327–346. [Google Scholar] [PubMed]
- Polosa, R.; Malerba, M.; Cacciola, R.R.; Morjaria, J.B.; Maugeri, C.; Prosperini, G.; Gullo, R.; Spicuzza, L.; Radaeli, A.; Di Maria, G.U. Effect of acute exacerbations on circulating endothelial, clotting and fibrinolytic markers in COPD patients. Intern. Emerg. Med. 2013, 8, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Muir, K.W.; Tyrrell, P.; Sattar, N.; Warburton, E. Inflammation and ischaemic stroke. Curr. Opin. Neurol. 2007, 20, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Young, G.H.; Huang, P.H.; Lo, S.C.; Wang, K.C.; Sun, C.Y.; Liang, C.J.; Huang, T.M.; Chen, J.H.; Chang, F.C.; et al. In acute kidney injury, indoxyl sulfate impairs human endothelial progenitor cells: Modulation by statin. Angiogenesis 2013, 16, 609–624. [Google Scholar] [CrossRef] [PubMed]
- Bonventre, J.V. Pathophysiology of AKI: Injury and normal and abnormal repair. Contrib. Nephrol. 2010, 165, 9–17. [Google Scholar] [PubMed]
- Hosohata, K. Role of oxidative stress in drug-induced kidney injury. Int. J. Mol. Sci. 2016, 17, 1826. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.H. Acidemia and blood free fatty acids: Analysis of cardiovascular risk factors in a new context. Discov. Med. 2017, 23, 183–188. [Google Scholar] [PubMed]
- Gorter, K.A.; Stehouwer, M.C.; Van Putte, B.P.; Vlot, E.A.; Urbanus, R.T. Acidosis induced by carbon dioxide insufflation decreases heparin potency: A risk factor for thrombus formation. Perfusion 2017, 32, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Checherita, I.A.; David, C.; Ciocalteu, A.; Lascar, I.; Budala, L. Oral treatment of metabolic acidosis in hemodialyzed patients and the implications on the hemodynamic status. Rom. J. Morphol. Embryol. 2013, 54, 539–543. [Google Scholar] [PubMed]
- Hu, M.C.; Shiizaki, K.; Kuro-o, M.; Moe, O.W. Fibroblast growth factor 23 and Klotho: Physiology and pathophysiology of an endocrine network of mineral metabolism. Annu. Rev. Physiol. 2013, 75, 503–533. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.C.; Shi, M.; Cho, H.J.; Adams-Huet, B.; Paek, J.; Hill, K.; Shelton, J.; Amaral, A.P.; Faul, C.; Taniguchi, M.; et al. Klotho and phosphate are modulators of pathologic uremic cardiac remodeling. J. Am. Soc. Nephrol. 2015, 26, 1290–1302. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wang, Y.; Gao, W.; Yuan, C.; Zhang, S.; Zhou, H.; Huang, M.; Yao, X. Klotho reduction in alveolar macrophages contributes to cigarette smoke extract-induced inflammation in chronic obstructive pulmonary disease. J. Biol. Chem. 2015, 290, 27890–27900. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, V.; Nagaraja, D.; Christopher, R. Association of the functional kL-VS variant of Klotho gene with early-onset ischemic stroke. Biochem. Biophys. Res. Commun. 2010, 403, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Yoon, J.; An, S.W.; Kuro-o, M.; Huang, C.L. Soluble Klotho protects against uremic cardiomyopathy independently of fibroblast growth factor 23 and phosphate. J. Am. Soc. Nephrol. 2015, 26, 1150–1160. [Google Scholar] [CrossRef] [PubMed]
- Druml, W. Acute renal failure is not a “cute” renal failure! Intensive. Care Med. 2004, 30, 1886–1890. [Google Scholar] [CrossRef] [PubMed]
- Griffo, R.; Spanevello, A.; Temporelli, P.L.; Faggiano, P.; Carone, M.; Magni, G.; Ambrosino, N.; Tavazzi, L.; Investigators, S. Frequent coexistence of chronic heart failure and chronic obstructive pulmonary disease in respiratory and cardiac outpatients: Evidence from suspirium, a multicentre Italian survey. Eur. J. Prev. Cardiol. 2017, 24, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Macchia, A.; Rodriguez Moncalvo, J.J.; Kleinert, M.; Comignani, P.D.; Gimeno, G.; Arakaki, D.; Laffaye, N.; Fuselli, J.J.; Massolin, H.P.; Gambarte, J.; et al. Unrecognised ventricular dysfunction in COPD. Eur. Respir. J. 2012, 39, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, M.; Agrawal, S.; Garg, L.; Garg, A.; Bhatia, N.; Kadaria, D.; Reed, G. Effect of chronic obstructive pulmonary disease on in-hospital mortality and clinical outcomes after ST-segment elevation myocardial infarction. Am. J. Cardiol. 2017, 119, 1555–1559. [Google Scholar] [CrossRef] [PubMed]
- Anand, I.S.; Chandrashekhar, Y.; Rao, S.K.; Malhotra, R.M.; Ferrari, R.; Chandana, J.; Ramesh, B.; Shetty, K.J.; Boparai, M.S. Body fluid compartments, renal blood flow, and hormones at 6000 m in normal subjects. J. Appl. Physiol. 1993, 74, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Walley, K.R.; Lewis, T.H.; Wood, L.D. Acute respiratory acidosis decreases left ventricular contractility but increases cardiac output in dogs. Circ. Res. 1990, 67, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Mishra, J.; Ma, Q.; Prada, A.; Mitsnefes, M.; Zahedi, K.; Yang, J.; Barasch, J.; Devarajan, P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J. Am. Soc. Nephrol. 2003, 14, 2534–2543. [Google Scholar] [CrossRef] [PubMed]
- Solak, Y.; Yilmaz, M.I.; Siriopol, D.; Saglam, M.; Unal, H.U.; Yaman, H.; Gok, M.; Cetinkaya, H.; Gaipov, A.; Eyileten, T.; et al. Serum neutrophil gelatinase-associated lipocalin is associated with cardiovascular events in patients with chronic kidney disease. Int. Urol. Nephrol. 2015, 47, 1993–2001. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Jia, M.; Yan, X.; Cao, L.; Barnes, P.J.; Adcock, I.M.; Huang, M.; Yao, X. Increased neutrophil gelatinase-associated lipocalin (NGAL) promotes airway remodelling in chronic obstructive pulmonary disease. Clin. Sci. (Lond). 2017, 131, 1147–1159. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, M.; Ishii, J.; Kitagawa, F.; Takahashi, H.; Sugiyama, K.; Tada, M.; Kanayama, K.; Takahashi, K.; Hayashi, H.; Koide, S.; et al. Plasma neutrophil gelatinase-associated lipocalin as a predictor of cardiovascular events in patients with chronic kidney disease. BioMed Res. Int. 2016, 2016, 8761475. [Google Scholar] [CrossRef] [PubMed]
- Nymo, S.H.; Ueland, T.; Askevold, E.T.; Flo, T.H.; Kjekshus, J.; Hulthe, J.; Wikstrand, J.; McMurray, J.; Van Veldhuisen, D.J.; Gullestad, L.; et al. The association between neutrophil gelatinase-associated lipocalin and clinical outcome in chronic heart failure: Results from CORONA*. J. Intern. Med. 2012, 271, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, G.C.; Hurst, J.R.; Smith, C.J.; Hubbard, R.B.; Wedzicha, J.A. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest 2010, 137, 1091–1097. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Wilt, T.J.; Weinberger, S.E.; Hanania, N.A.; Criner, G.; van der Molen, T.; Marciniuk, D.D.; Denberg, T.; Schunemann, H.; Wedzicha, W.; et al. Diagnosis and management of stable chronic obstructive pulmonary disease: A clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann. Int. Med. 2011, 155, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Suissa, S.; Dell’Aniello, S.; Ernst, P. Concurrent use of long-acting bronchodilators in COPD and the risk of adverse cardiovascular events. Eur. Respir. J. 2017, 49. [Google Scholar] [CrossRef] [PubMed]

| Before Matching | After Matching | |||||
|---|---|---|---|---|---|---|
| Non COPD | COPD | p-Value | Non COPD | COPD | p-Value | |
| (n = 12,779) | (n = 1535) | (n = 1473) | (n = 1473) | |||
| Age (year, SD) | 63.63 ± 16.39 | 74.02 ± 11.31 | <0.001 | 73.95 ± 11.28 | 73.91 ± 11.25 | 0.888 |
| Male gender | 6715 (52.55%) | 1044 (68.01%) | <0.001 | 960 (65.17%) | 986 (66.94%) | 0.331 |
| Monthly income, US dollars | ||||||
| <600 | 7865 (61.55%) | 923 (60.13%) | 0.004 | 903 (61.30%) | 890 (60.42%) | 0.304 |
| 600–1300 | 4484 (35.09%) | 581 (37.85%) | 530 (35.98%) | 554 (37.61%) | ||
| ≥1300 | 430 (3.36%) | 31 (2.02%) | 40 (2.72%) | 29 (1.97%) | ||
| Hospital location | ||||||
| Urban | 5276 (41.29%) | 604 (39.35%) | 0.005 | 559 (37.95%) | 579 (39.31%) | 0.696 |
| Suburban | 2947 (23.06%) | 320 (20.85%) | 311 (21.11%) | 312 (21.18%) | ||
| Rural | 4556 (35.65%) | 611 (39.80%) | 603 (40.94%) | 582 (39.51%) | ||
| Baseline comorbidities | ||||||
| Charlson comorbidity index | 2.17 ± 2.03 | 2.61 ± 2.06 | <0.001 | 2.59 ± 2.09 | 2.61 ± 2.08 | 0.736 |
| Myocardial infarction | 542 (4.24%) | 75 (4.89%) | 0.232 | 68 (4.62%) | 75 (5.09%) | 0.607 |
| Congestive heart failure | 1956 (15.31%) | 349 (22.74%) | <0.001 | 326 (22.13%) | 336 (22.81%) | 0.691 |
| Peripheral vascular disease | 244 (1.91%) | 25 (1.63%) | 0.487 | 29 (1.97%) | 25 (1.70%) | 0.681 |
| Cerebrovascular disease | 1382 (10.81%) | 276 (17.98%) | <0.001 | 246 (16.70%) | 256 (17.38%) | 0.659 |
| Dementia | 315 (2.46%) | 98 (6.38%) | <0.001 | 91 (6.18%) | 91 (6.18%) | 0.999 |
| Reumatologic disease | 243 (1.90%) | 18 (1.17%) | 0.043 | 16 (1.09%) | 18 (1.22%) | 0.863 |
| Peptic ulcer disease | 1791 (14.02%) | 273 (17.79%) | <0.001 | 265 (17.99%) | 259 (17.58%) | 0.81 |
| Hemiplegia or paraplegia | 117 (0.92%) | 26 (1.69%) | 0.006 | 16 (1.09%) | 26 (1.77%) | 0.161 |
| Diabetes | 4956 (38.78%) | 582 (37.92%) | 0.524 | 544 (36.93%) | 569 (38.63%) | 0.362 |
| Moderate or severe liver disease | 1036 (8.11%) | 98 (6.38%) | 0.019 | 89 (6.04%) | 94 (6.38%) | 0.76 |
| Chronic kidney disease | 4034 (31.57%) | 445 (28.99%) | 0.041 | 447 (30.35%) | 437 (29.67%) | 0.718 |
| Hypertension | 6630 (51.88%) | 950 (61.89%) | <0.001 | 889 (60.35%) | 911 (61.85%) | 0.427 |
| Dyslipidemia | 1765 (13.81%) | 167 (10.88%) | 0.001 | 185 (12.56%) | 164 (11.13%) | 0.254 |
| Medication for hypertension before index hospitalization | ||||||
| Alpha-blocker | 1326 (10.38%) | 206 (13.42%) | <0.001 | 201 (13.65%) | 201 (13.65%) | 0.999 |
| Beta-blocker | 4696 (36.75%) | 509 (33.16%) | 0.006 | 507 (34.42%) | 494 (33.54%) | 0.641 |
| CCB | 6807 (53.27%) | 946 (61.63%) | <0.001 | 881 (59.81%) | 903 (61.30%) | 0.429 |
| Diuretic | 6657 (52.09%) | 926 (60.33%) | <0.001 | 859 (58.32%) | 887 (60.22%) | 0.311 |
| ACEI or ARB | 5577 (43.64%) | 767 (49.97%) | <0.001 | 719 (48.81%) | 744 (50.51%) | 0.376 |
| Other medication | ||||||
| Aspirin | 1107 (8.66%) | 163 (10.62%) | 0.013 | 171 (11.61%) | 156 (10.59%) | 0.412 |
| Clopidogrel | 640 (5.01%) | 107 (6.97%) | 0.002 | 97 (6.59%) | 105 (7.13%) | 0.61 |
| Ticlopidine | 471 (3.69%) | 76 (4.95%) | 0.017 | 70 (4.75%) | 74 (5.02%) | 0.798 |
| Dipyridamole | 2851 (22.31%) | 357 (23.26%) | 0.4 | 358 (24.30%) | 348 (23.63%) | 0.698 |
| Nitrate | 93 (0.73%) | 22 (1.43%) | 0.006 | 19 (1.29%) | 19 (1.29%) | 0.999 |
| Statin | 2009 (15.72%) | 191 (12.44%) | 0.001 | 209 (14.19%) | 184 (12.49%) | 0.193 |
| NSAID | 6375 (49.89%) | 859 (55.96%) | <0.001 | 822 (55.80%) | 819 (55.60%) | 0.941 |
| PPI | 1214 (9.50%) | 201 (13.09%) | <0.001 | 165 (11.20%) | 191 (12.97%) | 0.158 |
| Index hospital comorbidity | ||||||
| Cardiovascular | 1148 (8.98%) | 150 (9.77%) | 0.301 | 153 (10.39%) | 142 (9.64%) | 0.539 |
| Respiratory | 2819 (22.06%) | 635 (41.37%) | <0.001 | 602 (40.87%) | 582 (39.51%) | 0.475 |
| Hepatic | 267 (2.09%) | 15 (0.98%) | 0.002 | 22 (1.49%) | 14 (0.95%) | 0.24 |
| Neurologic | 250 (1.96%) | 37 (2.41%) | 0.247 | 35 (2.38%) | 35 (2.38%) | 0.999 |
| Hematologic | 201 (1.57%) | 16 (1.04%) | 0.121 | 17 (1.15%) | 15 (1.02%) | 0.859 |
| Metabolic | 365 (2.86%) | 35 (2.28%) | 0.219 | 41 (2.78%) | 35 (2.38%) | 0.561 |
| ICU admission | 8492 (66.45%) | 1189 (77.46%) | <0.001 | 1141 (77.46%) | 1130 (76.71%) | 0.661 |
| Operation | 1314 (10.28%) | 151 (9.84%) | 0.624 | 136 (9.23%) | 139 (9.44%) | 0.899 |
| Renal function status at AKD periods (1 year after index hospitalization) | ||||||
| CKD | 4958 (38.80%) | 642 (41.82%) | 0.023 | 532 (36.12%) | 622 (42.23%) | 0.001 |
| Advanced CKD | 2410 (18.86%) | 206 (13.42%) | <0.001 | 199 (13.51%) | 201 (13.65%) | 0.957 |
| Events | Before Matching | After Matching | ||||
|---|---|---|---|---|---|---|
| Non-COPD (n = 12,779) | COPD (n = 1535) | p-Value | Non-COPD (n = 1473) | COPD (n = 1473) | p-Value | |
| All-cause death | 6931 (54.24%) | 1096 (71.40%) | <0.001 | 971 (65.92%) | 1050 (71.28%) | 0.002 |
| Stroke | 1044 (8.17%) | 172 (11.21%) | <0.001 | 121 (8.21%) | 170 (11.54%) | 0.003 |
| Ischemic stroke | 774 (6.06%) | 144 (9.38%) | <0.001 | 95 (6.45%) | 143 (9.71%) | 0.001 |
| Hemorrhagic stroke | 327 (2.56%) | 36 (2.35%) | 0.668 | 30 (2.04%) | 35 (2.38%) | 0.616 |
| CHF | 2541 (19.88%) | 458 (29.84%) | <0.001 | 296 (20.10%) | 448 (30.41%) | <0.001 |
| MACE * | 802 (6.28%) | 96 (6.25%) | 0.999 | 87 (5.91%) | 95 (6.45%) | 0.592 |
| ESRD | 3362 (26.31%) | 311 (20.26%) | <0.001 | 299 (20.30%) | 302 (20.50%) | 0.927 |
| COPD | Non-COPD | Crude | Adjusted † | Compete Risk †† | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Event | Person-Year | Incidence Rate (per 1000 Person-Years) | Event | Person-Year | Incidence Rate (per 1000 Person-Years) | HR (95%CI) | p Value | HR (95%CI) | p Value | sHR (95%CI) | p Value | |
| Before Propensity Score Matching | ||||||||||||
| All-cause death | 1096 | 4848.71 | 226.0 | 6931 | 57,368.8 | 120.8 | 1.55 [1.45,1.65] | <0.001 | 0.96 [0.90,1.04] | 0.323 | NA | NA |
| Stroke | 172 | 4368.39 | 39.4 | 1044 | 53,890 | 19.4 | 1.70 [1.45,2.00] | <0.001 | 1.27 [1.06,1.53] | 0.009 | 1.30 [1.07,1.56] | 0.007 |
| Ischemic stroke | 144 | 4413.14 | 32.6 | 774 | 54,369.5 | 14.2 | 1.88 [1.57,2.24] | <0.001 | 1.33 [1.09,1.63] | 0.006 | 1.37 [1.11,1.69] | 0.004 |
| Hemorrhagic stroke | 36 | 4783.3 | 7.5 | 327 | 56,658.6 | 5.8 | 1.18 [0.84,1.67] | 0.349 | 1.08 [0.74,1.57] | 0.691 | 1.05 [0.72,1.54] | 0.8 |
| CHF | 458 | 3769.6 | 121.5 | 2541 | 50,533.8 | 50.3 | 1.89 [1.71,2.09] | <0.001 | 1.37 [1.22,1.53] | <0.001 | 1.39 [1.24,1.56] | <0.001 |
| MACE | 127 | 4595.71 | 27.6 | 1127 | 54,737.5 | 20.6 | 1.20 [1.00,1.44] | 0.055 | 0.89 [0.73,1.09] | 0.270 | 0.89 [0.72,1.08] | 0.240 |
| ESRD | 311 | 4073.25 | 76.4 | 3362 | 45,620.2 | 73.7 | 0.81 [0.72,0.91] | <0.001 | 0.90 [0.80,1.02] | 0.102 | 0.91 [0.80,1.03] | 0.120 |
| After Propensity Score Matching | ||||||||||||
| All-cause death | 1050 | 4633.13 | 226.6 | 971 | 5159.11 | 188.2 | 1.08 [0.99,1.17] | 0.104 | 1.04 [0.96,1.14] | 0.331 | NA | NA |
| Stroke | 170 | 4156.28 | 40.9 | 121 | 4788.18 | 25.3 | 1.45 [1.14,1.83] | 0.002 | 1.42 [1.12,1.79] | 0.004 | 1.43 [1.13,1.81] | 0.003 |
| Ischemic stroke | 143 | 4201.03 | 34.0 | 95 | 4831.49 | 19.7 | 1.52 [1.17,1.97] | 0.002 | 1.48 [1.14,1.92] | 0.003 | 1.52 [1.17,1.97] | 0.002 |
| Hemorrhagic stroke | 35 | 4567.72 | 7.7 | 30 | 5107.35 | 5.9 | 1.26 [0.77,2.05] | 0.362 | 1.26 [0.77,2.05] | 0.361 | 1.19 [0.73,1.96] | 0.480 |
| CHF | 448 | 3583.99 | 125.0 | 296 | 4547.46 | 65.1 | 1.62 [1.40,1.88] | <0.001 | 1.59 [1.37,1.84] | <0.001 | 1.61 [1.39,1.86] | <0.001 |
| MACE * | 126 | 4391.31 | 28.7 | 116 | 4871.23 | 23.8 | 1.13 [0.87,1.45] | 0.357 | 1.12 [0.87,1.44] | 0.396 | 1.09 [0.84,1.40] | 0.520 |
| ESRD | 302 | 3870.54 | 78.0 | 299 | 4367.31 | 68.5 | 0.97 [0.83,1.14] | 0.695 | 0.96 [0.81,1.12] | 0.579 | 0.95 [0.81,1.12] | 0.550 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.-H.; Chang, H.-M.; Wang, C.-Y.; Chen, L.; Chen, L.-W.; Lai, C.-H.; Kuo, S.-W.; Wang, H.-C.; Wu, V.-C.; The National Taiwan University Study Group on Acute Renal Failure. Long-Term Outcomes in Patients with Incident Chronic Obstructive Pulmonary Disease after Acute Kidney Injury: A Competing-Risk Analysis of a Nationwide Cohort. J. Clin. Med. 2018, 7, 237. https://doi.org/10.3390/jcm7090237
Wu C-H, Chang H-M, Wang C-Y, Chen L, Chen L-W, Lai C-H, Kuo S-W, Wang H-C, Wu V-C, The National Taiwan University Study Group on Acute Renal Failure. Long-Term Outcomes in Patients with Incident Chronic Obstructive Pulmonary Disease after Acute Kidney Injury: A Competing-Risk Analysis of a Nationwide Cohort. Journal of Clinical Medicine. 2018; 7(9):237. https://doi.org/10.3390/jcm7090237
Chicago/Turabian StyleWu, Che-Hsiung, Huang-Ming Chang, Cheng-Yi Wang, Likwang Chen, Liang-Wen Chen, Chien-Heng Lai, Shuenn-Wen Kuo, Hao-Chien Wang, Vin-Cent Wu, and The National Taiwan University Study Group on Acute Renal Failure. 2018. "Long-Term Outcomes in Patients with Incident Chronic Obstructive Pulmonary Disease after Acute Kidney Injury: A Competing-Risk Analysis of a Nationwide Cohort" Journal of Clinical Medicine 7, no. 9: 237. https://doi.org/10.3390/jcm7090237
APA StyleWu, C.-H., Chang, H.-M., Wang, C.-Y., Chen, L., Chen, L.-W., Lai, C.-H., Kuo, S.-W., Wang, H.-C., Wu, V.-C., & The National Taiwan University Study Group on Acute Renal Failure. (2018). Long-Term Outcomes in Patients with Incident Chronic Obstructive Pulmonary Disease after Acute Kidney Injury: A Competing-Risk Analysis of a Nationwide Cohort. Journal of Clinical Medicine, 7(9), 237. https://doi.org/10.3390/jcm7090237






