Abnormal Plasma Cell Disorders in Refinery Waste Workers
Abstract
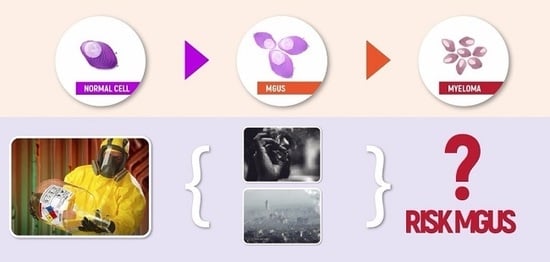
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Laboratory Analysis
2.3. Waste Characterization
2.4. Environmental Monitoring
2.5. Biological Monitoring
2.5.1. t,t-Muconic Acid
2.5.2. Heavy Metal Monitoring
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kyle, R.A.; Rajkumar, S.V. Monoclonal gammopathy of undetermined significance and smouldering multiple myeloma: Emphasis on risk factors for progression. Br. J. Haematol. 2007, 139, 730–743. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.A.; Child, J.A.; Anderson, K.; Barlogie, B.; Bataille, R.; Bensinger, W. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: A report of the International Myeloma Working Group. Br. J. Haematol. 2003, 121, 749–757. [Google Scholar]
- Kyle, R.A. Monoclonal gammopathy of undetermined significance. Natural history in 241 cases. Am. J. Med. 1978, 64, 814–826. [Google Scholar] [CrossRef]
- Kyle, R.A.; Buadi, F.; Rajkumar, S.V. Management of monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM). Oncology 2011, 25, 578–586. [Google Scholar] [PubMed]
- Van de Donk, N.W.C.J.; Mutis, T.; Poddighe, P.J.; Lokhorst, H.M.; Zweegman, S. Diagnosis, risk stratification and management of monoclonal gammopathy of undetermined significance and smoldering multiple myeloma. Int. J. Lab. Hematol. 2016, 38, 110–122. [Google Scholar] [CrossRef] [PubMed]
- Dispenzieri, A.; Katzmann, J.A.; Kyle, R.A.; Larson, D.R.; Melton, L.J.; Colby, C.L. Prevalence and risk of progression of light-chain monoclonal gammopathy of undetermined significance: A retrospective population-based cohort study. Lancet 2010, 375, 1721–1728. [Google Scholar] [CrossRef]
- Kyle, R.A.; Therneau, T.M.; Rajkumar, S.V.; Larson, D.R.; Plevak, M.F.; Offord, J.R. Prevalence of monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 2006, 354, 1362–1369. [Google Scholar] [CrossRef] [PubMed]
- Eisele, L.; Dürig, J.; Hüttmann, A.; Dührsen, U.; Assert, R.; Bokhof, B. Prevalence and progression of monoclonal gammopathy of undetermined significance and light-chain MGUS in Germany. Ann. Hematol. 2012, 91, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.A.; Therneau, T.M.; Vincent Rajkumar, S.; Offord, J.R.; Larson, D.R.; Plevak, M.F. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 2002, 346, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Bladé, J.; Rosiñol, L.; Cibeira, M.T.; De Larrea, C.F. Pathogenesis and progression of monoclonal gammopathy of undetermined significance. Leukemia 2008, 22, 1651–1657. [Google Scholar] [CrossRef] [PubMed]
- Landgren, O.; Kyle, R.A.; Pfeiffer, R.M.; Katzmann, J.A.; Caporaso, N.E.; Hayes, R.B. Monoclonal gammopathy of undetermined significance (MGUS) consistently precedes multiple myeloma: A. prospective study. Blood 2009, 113, 5412–5417. [Google Scholar] [CrossRef] [PubMed]
- Weiss, B.M.; Abadie, J.; Verma, P. Howard RS, Kuehl WM. A monoclonal gammopathy precedes multiple myeloma in most patients. Blood 2009, 113, 5418–5422. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.A.; Gertz, M.A.; Witzig, T.E.; Lust, J.A.; Lacy, M.Q.; Dispenzieri, A. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin. Proc. 2003, 78, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, S.V.; Kumar, S. Multiple myeloma: Diagnosis and treatment. Mayo Clin. Proc. 2016, 91, 101–119. [Google Scholar] [CrossRef] [PubMed]
- Sundaramoorthy, P.; Gasparetto, C.; Kang, Y. The combination of a sphingosine kinase 2 inhibitor (ABC294640) and a bcl-2 inhibitor (ABT-199) displays synergistic anti-myeloma effects in myeloma cells without a t(11;14) translocation. Cancer Med 2018, 7, 3257–3268. [Google Scholar] [CrossRef] [PubMed]
- Landgren, O.; Shim, Y.K.; Michalek, J.; Costello, R.; Burton, D.; Ketchum, N. Agent Orange Exposure and Monoclonal Gammopathy of Undetermined Significance: An Operation Ranch Hand Veteran Cohort Study. JAMA Oncol. 2015, 1, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Landgren, O.; Kyle, R.A.; Hoppin, J.A.; Beane Freeman, L.E.; Cerhan, J.R.; Katzmann, J.A. Pesticide exposure and risk of monoclonal gammopathy of undetermined significance in the Agricultural Health Study. Blood 2009, 113, 6386–6391. [Google Scholar] [CrossRef] [PubMed]
- Sirohi, B.; Powles, R. Epidemiology and outcomes research for MGUS, myeloma and amyloidosis. Eur. J. Cancer 2006, 42, 1671–1683. [Google Scholar] [CrossRef] [PubMed]
- Pasqualetti, P.; Collacciani, A.; Casale, R. Risk of monoclonal gammopathy of undetermined significance: A case-referent study. Am. J. Hematol. 1996, 52, 217–220. [Google Scholar] [CrossRef]
- Wong, O.; Raabe, G.K. Multiple myeloma and benzene exposure in a multinational cohort of more than 250,000 petroleum workers. Regul. Toxicol. Pharmacol. 1997, 26, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Steineck, G.; Wiklund, K. Multiple myeloma in Swedish agricultural workers. Int. J. Epidemiol. 1986, 15, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Baris, D.; Järvholm, B.; Silverman, D.T.; Bergdahl, I.A.; Blair, A. Multiple myeloma and diesel and other occupational exposures in Swedish construction workers. Int. J. Cancer 2003, 107, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Kirkeleit, J.; Riise, T.; Bråtveit, M.; Moen, B.E. Increased risk of acute myelogenous leukemia and multiple myeloma in a historical cohort of upstream petroleum workers exposed to crude oil. Cancer Causes Control 2008, 19, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Mayo Medical Laboratories. Available online: http://www.mayomedicallaboratories.com (accessed on 21 July 2018).
- Directive 2008/98/EC of the European Parliament and of the council of 19 November 2008 on waste and repealing certain Directives. Available online: https://eur-lex.europa.eu/legal-content/FRF/TXT/?uri=celex:32008L0098 (accessed on 21 July 2018).
- Commission Regulation (EU) No 1357/2014 of 18 December 2014 replacing Annex III to Directive 2008/98/EC of the European Parliament and of the Council on waste and repealing certain Directives. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex:32014R1357 (accessed on 21 July 2018).
- European Standard (EN) 481: Workplace atmospheres—Size fraction definitions for measurement of airborne particles; Comité Européen de Normalisation: Brussels, Belgium, 1993.
- M.U. 13: Ambienti di lavoro—Determinazione della frazione inalabile delle particelle aerodisperse—Metodo gravimetrico; UNICHIM: Milan, Italy, 1998.
- M.U. 11: Ambienti di lavoro—Determinazione della frazione respirabile delle particelle aerodisperse—Metodo gravimetrico; UNICHIM: Milan, Italy, 2010.
- Inoue, O.; Seiji, K.; Nakatsuka, H.; Watanabe, T.; Yin, S.N.; Li, G.L.; Jin, C.; Ikeda, M. Urinary t,t-muconic acid as an indicator of exposure to benzene. Br. J. Ind. Med. 1989, 46, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Goullé, J.-; Mahieu, L.; Castermant, J.; Neveu, N.; Bonneau, L.; Lainé, G. Metal and metalloid multi-elementary ICP-MS validation in whole blood, plasma, urine and hair: Reference values. Forensic. Sci. Int. 2005, 153, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Iavicoli, I.; Bracci, M.; Avola, R.; Senia, P.; Santarelli, L. Serum lipid, lipoprotein and apolipoprotein profiles in workers exposed to low arsenic levels: Lipid profiles and occupational arsenic exposure. Toxicol. Lett 2018, 282, 49–56. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Biological Monitoring of Chemical Exposure in the Workplace; World Health Organization: Geneva, Switherland, 1996. [Google Scholar]
- Kyle, R.A.; Rajkumar, S.V. Epidemiology of the plasma-cell disorders. Best Pract. Res. Clin. Haematol. 2007, 20, 637–664. [Google Scholar] [CrossRef] [PubMed]
- Wadhera, R.K.; Rajkumar, S.V. Prevalence of monoclonal gammopathy of undetermined significance: A. systematic review. Mayo Clin. Proc. 2010, 85, 933–942. [Google Scholar] [CrossRef] [PubMed]
- Landgren, O.; Gridley, G.; Turesson, I.; Caporaso, N.E.; Goldin, L.R.; Baris, D. Risk of monoclonal gammopathy of undetermined significance (MGUS) and subsequent multiple myeloma among African American and white veterans in the United States. Blood 2006, 107, 904–906. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, U.; Hällén, J. Review of fifty-four subjects with monoclonal gammopathy. Br. J. Haematol. 1968, 15, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Saleun, J.P.; Vicariot, M.; Deroff, P.; Morin, J.F. Monoclonal gammopathies in the adult population of Finistere, France. J. Clin. Pathol. 1982, 35, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.A.; Finkelstein, S.; Elveback, L.R. Kurland LT. Incidence of monoclonal proteins in a Minnesota community with a cluster of multiple myeloma. Blood 1972, 40, 719–724. [Google Scholar] [PubMed]
- Kyle, R.A.; Therneau, T.M.; Rajkumar, S.V.; Larson, D.R.; Plevak, M.F.; Melton, L.J., III. Long-term follow-up of 241 patients with monoclonal gammopathy of undetermined significance: The original Mayo Clinic series 25 years later. Mayo Clin. Proc. 2004, 79, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Baris, D.; Silverman, D.T.; Brown, L.M.; Swanson, G.M.; Hayes, R.B.; Schwatz, A.G. Occupation, pesticide exposure and risk of multiple myeloma. Scand. J. Work Environ. Health 2004, 30, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Cerhan, J.R.; Cantor, K.P.; Williamson, K.; Lynch, C.F.; Torner, J.C.; Burmeister, L.F. Cancer mortality among Iowa farmers: Recent results, time trends, and lifestyle factors (United States). Cancer Causes Control 1998, 9, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Pukkala, E.; Notkola, V. Cancer incidence among Finnish farmers, 1979–1993. Cancer Causes Control 1997, 8, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Blade, J.; Lopez-Guillermo, A.; Rozman, C.; Cervantes, F.; Salgado, C.; Aguilar, J.L. Malignant transformation and life expectancy in monoclonal gammopathy of undetermined significance. Br. J. Haematol. 1992, 81, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Cesana, C.; Klersy, C.; Barbarano, L.; Nosari, A.M.; Crugnola, M.; Pungolino, E. Prognostic factors for malignant transformation in monoclonal gammopathy of undetermined significance and smoldering multiple myeloma. J. Clin. Oncol. 2002, 20, 1625–1634. [Google Scholar] [CrossRef] [PubMed]
- Vlaanderen, J.; Lan, Q.; Kromhout, H.; Rothman, N.; Vermeulen, R. Occupational benzene exposure and the risk of lymphoma subtypes: A meta-analysis of cohort studies incorporating three study quality dimensions. Environ. Health Perspect. 2011, 119, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Cocco, P.; T’Mannetje, A.; Fadda, D.; Melis, M.; Becker, N.; De Sanjosé, S. Occupational exposure to solvents and risk of lymphoma subtypes: Results from the Epilymph case-control study. Occup. Environ. Med. 2010, 67, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Costantini, A.S.; Benvenuti, A.; Vineis, P.; Kriebel, D.; Tumino, R.; Ramazzotti, V. Risk of leukemia and multiple myeloma associated with exposure to benzene and other organic solvents: Evidence from the Italian multicenter case-control study. Am. J. Ind. Med. 2008, 51, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, A.J.; Rajkumar, S.V.; Vachon, C.M. Familial monoclonal gammopathy of undetermined significance and multiple myeloma: Epidemiology, risk factors, and biological characteristics. Blood 2012, 119, 5359–5366. [Google Scholar] [CrossRef] [PubMed]
- Bida, J.P.; Kyle, R.A.; Therneau, T.M.; Melton, L.J., III; Plevak, M.F.; Larson, D.R. Disease associations with monoclonal gammopathy of undetermined significance: A population-based study of 17,398 patients. Mayo Clin. Proc. 2009, 84, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Khuder, S.A.; Mutgi, A.B. Meta-analyses of multiple myeloma and farming. Am. J. Ind. Med. 1997, 32, 510–516. [Google Scholar] [CrossRef]
- Landgren, O. Monoclonal gammopathy of undetermined significance and smoldering multiple myeloma: Biological insights and early treatment strategies. Hematol. Am. Soc. Hematol. Educ. Program 2013, 2013, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Lathrop, G.D.; Wolfe, W.H.; Albanese, R.A.; Moynahan, P.M. An Epidemiologic Investigation of Health Effects in Air Force Personnel Following Exposure to Herbicides: Baseline Morbidity Results 1984. Available online: https://www.vietnam.ttu.edu/star/images/455/4550214001A.pdf (accessed on 16 August 2018).
- Michalek, J.E.; Robinson, J.; Fox, K. The Air Force Health Study: An epidemiologic investigation of health effects in air force personnel following exposure to herbicides 2002 Follow-Up Examination Results 2005. Available online: https://www.dtic.mil/dtic/tr/fulltext/u2/a438835.pdf (accessed on 8 June 2018).
- Patterson, D.G.; Hampton, L.; Lapeza, C.R.; Belser, W.T.; Green, V.; Alexander, L. High-resolution gas chromatographic/high-resolution mass spectrometric analysis of human serum on a whole-weight and lipid basis for 2,3,7,8-Tetrachlorodibenzo-p-dioxin. Anal. Chem. 1987, 59, 2000–2005. [Google Scholar] [CrossRef] [PubMed]
- Pasqualetti, P.; Casale, R.; Colantonio, D.; Collacciani, A. Occupational risk for hematological malignancies. Am. J. Hematol. 1991, 38, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Pasqualetti, P.; Festuccia, V.; Acitelli, P.; Collacciani, A.; Giusti, A.; Casale, R. Tobacco smoking and risk of haematological malignancies in adults: A. case-control study. Br. J. Haematol. 1997, 97, 659–662. [Google Scholar] [CrossRef] [PubMed]
- Wallin, A.; Larsson, S.C. Body mass index and risk of multiple myeloma: A meta-analysis of prospective studies. Eur. J. Cancer 2011, 47, 1606–1615. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.T.; Caporaso, N.E.; Kyle, R.A.; Katzmann, J.A.; Dispenzieri, A.; Hayes, R.B. Evidence of serum immunoglobulin abnormalities up to 9.8 years before diagnosis of chronic lymphocytic leukemia: A. prospective study. Blood 2009, 114, 4928–4932. [Google Scholar] [CrossRef] [PubMed]
- Alavanja, M.C.R.; Blair, A.; Merkle, S.; Teske, J.; Eaton, B. Mortality among agricultural extension agents. Am. J. Ind. Med. 1988, 14, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Burnett, C.A.; Lalich, N.; Cameron, L.L.; Sestito, J.P. Proportionate mortality of crop and livestock farmers in the United States, 1984–1993. Am. J. Ind. Med. 2002, 42, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Nandakumar, A.; English, D.R.; Dougan, L.E.; Armstrong, B.K. Incidence and outcome of multiple myeloma in western Australia, 1960 to 1984. Aust. New Zealand J. Med. 1988, 18, 774–779. [Google Scholar] [CrossRef]
- Stark, A.D.; Chang, H.G.; Fitzgerald, E.F.; Riccardi, K.; Stone, R.R. A retrospective cohort study of cancer incidence among New York state farm bureau members. Arch. Environ. Health 1990, 45, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Boffetta, P.; Stellman, S.D.; Garfinkel, L. A case-control study of multiple myeloma nested in the American cancer society prospective study. Int. J. Cancer 1989, 43, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Brownson, R.C.; Reif, J.S.; Chang, J.C.; Davis, J.R. Cancer risks among Missouri farmers. Cancer 1989, 64, 2381–2386. [Google Scholar] [CrossRef]
- Burmeister, L.F. Cancer in Iowa farmers: Recent results. Am. J. Ind. Med. 1990, 18, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Cantor, K.P.; Blair, A. Farming and mortality from multiple myeloma: A case-control study with the use of death certificates. J. Natl. Cancer Inst. 1984, 72, 251–255. [Google Scholar] [PubMed]
- Seniori Costantini, A.; Miligi, L.; Kriebel, D.; Ramazzotti, V.; Rodella, S.; Scarpi, E. A multicenter case-control study in Italy on hematolymphopoietic neoplasms and occupation. Epidemiology 2001, 12, 78–87. [Google Scholar] [CrossRef]
- Cuzick, J.; De Stavola, B. Multiple myeloma a case-control study. Br. J. Cancer 1988, 57, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Demers, P.A.; Vaughan, T.L.; Koepsell, T.D.; Lyon, J.L.; Swanson, G.M.; Greenberg, R.S. A case-control study of multiple myeloma and occupation. Am. J. Ind. Med. 1993, 23, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Karlsson, M. Occupational and other environmental factors and multiple myeloma: A population based case-control study. Br. J. Ind. Med. 1992, 49, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Figgs, L.W.; Dosemeci, M.; Blair, A. Risk of multiple myeloma by occupation and industry among men and women: A 24-state death certificate study. J. Occup. Med. 1994, 36, 1210–1221. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, S.; Barbone, F.; Bidoli, E.; Guarneri, S.; Serraino, D.; Talamini, R. Cancer risk in farmers: Results from a multi-site case-control study in north-eastern Italy. Int. J. Cancer 1993, 53, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Heineman, E.F.; Olsen, J.H.; Pottern, L.M.; Gomez, M.; Raffn, E.; Blair, A. Occupational risk factors for multiple myeloma among Danish men. Cancer Causes Control 1992, 3, 555–568. [Google Scholar] [CrossRef] [PubMed]
- Vecchia, C.L.; Negri, E.; D’Avanzo, B.; Franceschi, S. Occupation and lymphoid neoplasms. Br. J. Cancer 1989, 60, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Milham, S. Leukemia and multiple myeloma in farmers. Am. J. Epidemiol. 1971, 94, 307–310. [Google Scholar] [CrossRef]
- Pearce, N.; Reif, J.S. Epidemiologic studies of cancer in agricultural workers. Am. J. Ind. Med. 1990, 18, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Blair, A.; Dosemeci, M.; Heineman, E.F. Cancer and other causes of death among male and female farmers from twenty-three states. Am. J. Ind. Med. 1993, 23, 729–742. [Google Scholar] [CrossRef] [PubMed]
- Blair, A.; Zahm, S.H.; Pearce, N.E.; Heineman, E.F.; Fraumeni, J.F., Jr. Clues to cancer etiology from studies of farmers. Scand. J. Work Environ. Health 1992, 18, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.M.; Burmeister, L.F.; Everett, G.D.; Blair, A. Pesticide exposures and multiple myeloma in Iowa men. Cancer Causes Control 1993, 4, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Manzella, N.; Bracci, M.; Strafella, E.; Staffolani, S.; Ciarapica, V.; Copertaro, A. Circadian modulation of 8-oxoguanine DNA damage repair. Sci. Rep. 2015, 5, 13752. [Google Scholar] [CrossRef] [PubMed]
- Rapisarda, V.; Ledda, C.; Ferrante, M.; Fiore, M.; Cocuzza, S.; Bracci, M. Blood pressure and occupational exposure to noise and lead (Pb): A cross-sectional study. Toxicol Ind. Health 2016, 32, 1729–1736. [Google Scholar] [CrossRef] [PubMed]
- Rapisarda, V.; Miozzi, E.; Loreto, C.; Matera, S.; Fenga, C.; Avola, R. Cadmium exposure and prostate cancer: Insights, mechanisms and perspectives. Front Biosci. Landmark 2018, 23, 1687–1700. [Google Scholar]
- Rapisarda, V.; Ledda, C.; Matera, S.; Fago, L.; Arrabito, G.; Falzone, L.; Marconi, A.; Libra, M.; Loreto, C. Absence of t (14; 18) chromosome translocation in agricultural workers after short-term exposure to pesticides. Mol. Med. Rep. 2017, 15, 3379–3382. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, C.A.; Landgren, O. Polyclonal immunoglobulin free light chains as a potential biomarker of immune stimulation and inflammation. Clin. Chem. 2011, 57, 1387–1389. [Google Scholar] [CrossRef] [PubMed]
- Korde, N.; Kristinsson, S.Y.; Landgren, O. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM): Novel biological insights and development of early treatment strategies. Blood 2011, 117, 5573–5581. [Google Scholar] [CrossRef] [PubMed]
| Sample | Hazard Properties (HP) |
|---|---|
| A |
|
| B |
|
| C |
|
| Area | Inhaled Airborne Dust (mg/m3) | Breathable Fraction (mg/m3) | ||
|---|---|---|---|---|
| 1 | 0.08 ± 0.02 | TLV-TWA 10 mg/m3 | <0.05 | TLV-TWA 3 mg/m3 |
| 2 | 0.10 ± 0.02 | <0.05 | ||
| 3 | 0.06 ± 0.01 | <0.05 | ||
| 4 | 0.06 ± 0.01 | <0.05 | ||
| 5 | 0.08 ± 0.02 | <0.05 | ||
| 6 | 0.06 ± 0.01 | <0.05 | ||
| 7 | 0.08 ± 0.02 | <0.05 | ||
| 8 | 0.06 ± 0.01 | <0.05 | ||
| 9 | 0.08 ± 0.02 | <0.05 | ||
| 10 | 0.06 ± 0.01 | <0.05 | ||
| Workers (No. 77) | Mean ± SD | Reference Values |
|---|---|---|
| General characteristics | ||
| Age (years) | 36 ± 11 | |
| Duration of employment (years) | 18.5 ± 6.4 | |
| Duration of employment in refinery waste (years) | 9.1 ± 3.9 | |
| Smoking habits | 41 (53%) | |
| Pack/years | 301 ± 36 | |
| Living close industrial area | 63 (82%) | |
| BMI (Body Mass Index) (kg/m2) | 22.1 ± 2.5 | 18.5–24.99 |
| Hematology | ||
| WBC (Haemochrome for leukocytes) | 7.3 ± 1.7 | 4–10 × 103/µL |
| RBC (erythrocytes) | 5.1 ± 1.6 | 4–6 × 106/µL |
| HGB (hemoglobin) | 15.4 ± 1.2 | 13.0–17.5 g/dL |
| PLT (platelets) | 251 ± 74 | 150–450 × 103/µL |
| Biochemical parameter | ||
| TP (total protein) | 6.9 ± 0.5 | 6.3–7.9 g/dL |
| γ-GT (γ-glutamyltranspeptidase) | 21 ± 12 | 9–40 U/L |
| ALT (alanine aminotransferase) | 25 ± 15 | 7–55 U/L |
| AST (aspartate aminotransferase) | 26 ± 18 | 8–48 U/L |
| CHOL (total cholesterol) | 187 ± 23 | <200 mg/dL |
| TRIG (triglycerides) | 95 ± 26 | <150 mg/dL |
| HDL (high-density lipoprotein) | 63 ± 12 | ≥40 mg/dL |
| LDL (low-density lipoprotein) | 110 ± 18 | ≤129 mg/dL |
| BUN (blood urea nitrogen) | 15 ± 5 | 8–24 mg/dL |
| URIC (uric acid) | 5.9 ± 2.1 | 3.7–8.0 mg/dL |
| GLURA (fasting glucose) | 95 ± 16 | 70–126 mg/dL |
| Biological Monitoring | ||
| t,t-muconic acid | 278.8 ± 78.3 | 500 µg/L |
| As | 24.3 ± 8.9 | <50.0 µg/g creu |
| Cd | 1.2 ± 0.8 | <3.0 µg/g creu |
| Hg | 19.7 ± 3.5 | <35.0 µg/g creu |
| Pb | 3.1 ± 1.7 | <5.0 µg/g creu |
| MGUS Prevalence No. (%) | Frequency of Ig Sub-Types No. (%) | ||||
|---|---|---|---|---|---|
| IgG | IgA | IgM | IgD | Oligoclonal | |
| 12 (16%) | 8 (67%) | 1 (8%) | 2 (17%) | 0 | 1 (8%) |
| MGUS | ||
|---|---|---|
| OR (95%CI) | p-Value | |
| Duration of employment | 1.04 (0.91–1.17) | n.s. |
| Duration of employment in refinery waste | 0.99 (0.95–1.04) | n.s. |
| Smoking habits | 1.08 (1.05–1.13) | <0.001 |
| Living close industrial area | 1.10 (1.07–1.15) | <0.001 |
| BMI | 1.03 (0.97–1.09) | n.s. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ledda, C.; Loreto, C.; Filetti, V.; Matera, S.; Vitale, E.; Bracci, M.; Rapisarda, V. Abnormal Plasma Cell Disorders in Refinery Waste Workers. J. Clin. Med. 2018, 7, 221. https://doi.org/10.3390/jcm7080221
Ledda C, Loreto C, Filetti V, Matera S, Vitale E, Bracci M, Rapisarda V. Abnormal Plasma Cell Disorders in Refinery Waste Workers. Journal of Clinical Medicine. 2018; 7(8):221. https://doi.org/10.3390/jcm7080221
Chicago/Turabian StyleLedda, Caterina, Carla Loreto, Vera Filetti, Serena Matera, Ermanno Vitale, Massimo Bracci, and Venerando Rapisarda. 2018. "Abnormal Plasma Cell Disorders in Refinery Waste Workers" Journal of Clinical Medicine 7, no. 8: 221. https://doi.org/10.3390/jcm7080221
APA StyleLedda, C., Loreto, C., Filetti, V., Matera, S., Vitale, E., Bracci, M., & Rapisarda, V. (2018). Abnormal Plasma Cell Disorders in Refinery Waste Workers. Journal of Clinical Medicine, 7(8), 221. https://doi.org/10.3390/jcm7080221