Syphilis Trends in the Central Savannah River Area (CSRA) of Georgia and South Carolina, USA
Abstract
:1. Introduction
2. Methods
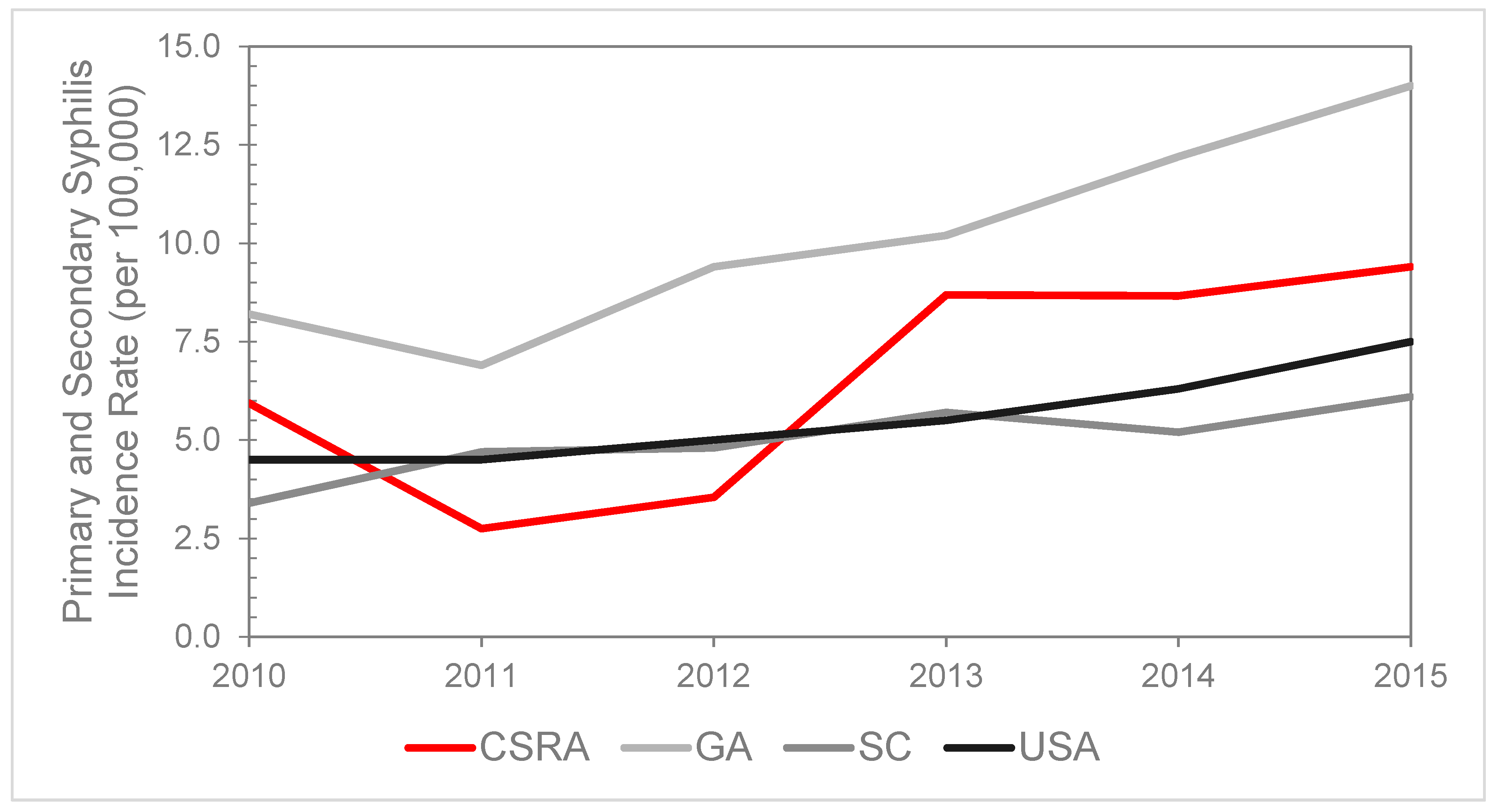
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2015; Department of Health and Human Services: Atlanta, GA, USA, 2016. Available online: https://www.cdc.gov/std/stats15/std-surveillance-2015-print.pdf (accessed on 10 November 2016).
- Lynn, W.A.; Lightman, S. Syphilis and HIV: A dangerous combination. Lancet Infect. Dis. 2004, 4, 456–466. [Google Scholar] [CrossRef]
- Knaute, D.F.; Graf, N.; Lautenschlager, S.; Weber, R.; Bosshard, P.P. Serological response to treatment of syphilis according to disease stage and HIV status. Clin. Infect. Dis. 2012, 55, 1615–1622. [Google Scholar] [CrossRef] [PubMed]
- University of Wisconsin Population Health Institute. County Health Rankings 2017. Available online: http://www.countyhealthrankings.org/sites/default/files/state/downloads/CHR2017_GA.pdf (accessed on 16 July 2018).
- Centers for Disease Control and Prevention. NCHHSTP AtlasPlus. Available online: https://www.cdc.gov/nchhstp/atlas/index.htm (accessed on 31 July 2017).
- Patton, M.E.; Su, J.R.; Nelson, R.; Weinstock, H.; Centers for Disease Control and Prevention. Primary and secondary syphilis—United States, 2005–2013. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 402–406. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention. 2013 Sexually Transmitted Diseases Surveillance: National Profile—Syphilis. 2014. Available online: https://www.cdc.gov/std/stats13/syphilis.htm (accessed on 21 December 2017).
- Heffelfinger, J.D.; Swint, E.B.; Berman, S.M.; Weinstock, H.S. Trends in primary and secondary syphilis among men who have sex with men in the United States. Am. J. Public Health 2007, 97, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Willeford, W.G.; Bachmann, L.H. Syphilis ascendant: A brief history and modern trends. Trop. Dis. Travel Med. Vaccines 2016, 2, 20. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.; Chaw, J.K.; Kent, C.K.; Klausner, J.D. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sex. Transm. Dis. 2005, 32, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Solomon, M.M.; Mayer, K.H. Evolution of the syphilis epidemic among men who have sex with men. Sex Health 2015, 12, 96–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. Internet use and early syphilis infection among men who have sex with men—San Francisco, California, 1999–2003. MMWR Morb. Mortal. Wkly. Rep. 2003, 52, 1229–1232. [Google Scholar]
- Kim, A.A.; Kent, C.; McFarland, W.; Klausner, J.D. Cruising on the internet highway. J. Acquir. Immune Defic. Syndr. 2001, 28, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Abara, W.; Annang, L.; Spencer, S.M.; Fairchild, A.J.; Billings, D. Understanding internet sex-seeking behaviour and sexual risk among young men who have sex with men: Evidences from a cross-sectional study. Sex. Transm. Infect. 2014, 90, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Abara, W.E.; Hess, K.L.; Fanfair, R.N.; Bernstein, K.T.; Paz-Bailey, G. Syphilis Trends among men who have sex with men in the United States and Western Europe: A systematic review of trend studies published between 2004 and 2015. PLoS ONE 2016, 11, e0159309. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, J.E.; Benson, C.; Holmes, K.K.; Brooks, J.T.; Pau, A.; Masur, H.; Centers for Disease Control and Prevention; National Institutes of Health; HIV Medicine Association (HIVMA) of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm. Rep. 2009, 58, 1–207. [Google Scholar] [PubMed]
- Shockman, S.; Buescher, L.S.; Stone, S.P. Syphilis in the United States. Clin. Dermatol. 2014, 32, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Peterman, T.A.; Su, J.; Bernstein, K.T.; Weinstock, H. Syphilis in the United States: On the rise? Expert Rev. Anti Infect. Ther. 2015, 13, 161–168. [Google Scholar] [CrossRef] [PubMed]
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | |
| Age in years | ||||||||||||
| 15–19 | 6 | 11.2 | 4 | 7.9 | 1 | 2.0 | 2 | 4.1 | 6 | 12.6 | 3 | 6.3 |
| 20–24 | 11 | 22.4 | 5 | 9.8 | 12 | 22.8 | 15 | 28.3 | 16 | 30.1 | 18 | 34.5 |
| 25–29 | 4 | 8.28 | 2 | 4.1 | 5 | 10.1 | 8 | 16.0 | 17 | 33.3 | 13 | 24.8 |
| 30–34 | 5 | 11.3 | 5 | 11.0 | 3 | 6.4 | 10 | 21.0 | 7 | 14.6 | 12 | 24.9 |
| 35–39 | 3 | 6.8 | 0 | 0 | 2 | 4.7 | 11 | 25.8 | 3 | 7.0 | 7 | 15.8 |
| 40–44 | 0 | 0 | 0 | 0 | 1 | 2.2 | 6 | 13.2 | 3 | 6.7 | 3 | 6.8 |
| 45–54 | 9 | 8.5 | 4 | 3.8 | 0 | 0 | 10 | 9.9 | 8 | 8.1 | 9 | 9.2 |
| 55–64 | 5 | 5.5 | 0 | 0 | 1 | 1.1 | 1 | 1.0 | 2 | 2.1 | 5 | 5.0 |
| 65 + | 0 | 0 | 0 | 0 | 1 | 1.0 | 0 | 0 | 1 | 0.9 | 0 | 0.0 |
| Race/ethnicity | ||||||||||||
| White, non-Hispanic | 6 | 1.5 | 4 | 1.0 | 5 | 1.2 | 15 | 3.7 | 12 | 3.0 | 20 | 4.9 |
| Black, non-Hispanic | 37 | 13.3 | 15 | 5.4 | 19 | 6.8 | 49 | 17.3 | 49 | 17.3 | 48 | 16.9 |
| Asian/Pacific Islander | 0 | 0 | 1 | 7.9 | 0 | 0 | 0 | 0 | 1 | 7.2 | 0 | 0.0 |
| Am. Indian/Alaskan Native | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 |
| Hispanic | 0 | 0 | 0 | 0 | 2 | 5.9 | 0 | 0 | 2 | 5.5 | 1 | 2.7 |
| Unknown | - | - | - | - | - | - | - | - | - | - | 1 | NA |
| Sex | ||||||||||||
| Male | 36 | 10.2 | 14 | 3.94 | 22 | 6.13 | 46 | 12.7 | 55 | 15.2 | 58 | 15.9 |
| Female | 7 | 1.9 | 6 | 1.61 | 4 | 1.07 | 18 | 4.8 | 9 | 2.4 | 12 | 3.2 |
| Total | 43 | 5.9 | 20 | 2.7 | 26 | 3.5 | 64 | 8.7 | 64 | 8.7 | 70 | 9.4 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stone, R.B.; Chung, Y.; Ansa, B.E. Syphilis Trends in the Central Savannah River Area (CSRA) of Georgia and South Carolina, USA. J. Clin. Med. 2018, 7, 190. https://doi.org/10.3390/jcm7080190
Stone RB, Chung Y, Ansa BE. Syphilis Trends in the Central Savannah River Area (CSRA) of Georgia and South Carolina, USA. Journal of Clinical Medicine. 2018; 7(8):190. https://doi.org/10.3390/jcm7080190
Chicago/Turabian StyleStone, Rebecca B., Yunmi Chung, and Benjamin E. Ansa. 2018. "Syphilis Trends in the Central Savannah River Area (CSRA) of Georgia and South Carolina, USA" Journal of Clinical Medicine 7, no. 8: 190. https://doi.org/10.3390/jcm7080190
APA StyleStone, R. B., Chung, Y., & Ansa, B. E. (2018). Syphilis Trends in the Central Savannah River Area (CSRA) of Georgia and South Carolina, USA. Journal of Clinical Medicine, 7(8), 190. https://doi.org/10.3390/jcm7080190





