Decreased Bioelectrical Impedance Phase Angle in Hospitalized Children and Adolescents with Newly Diagnosed Type 1 Diabetes: A Case-Control Study
Abstract
1. Introduction
2. Experimental Section
2.1. Ethics
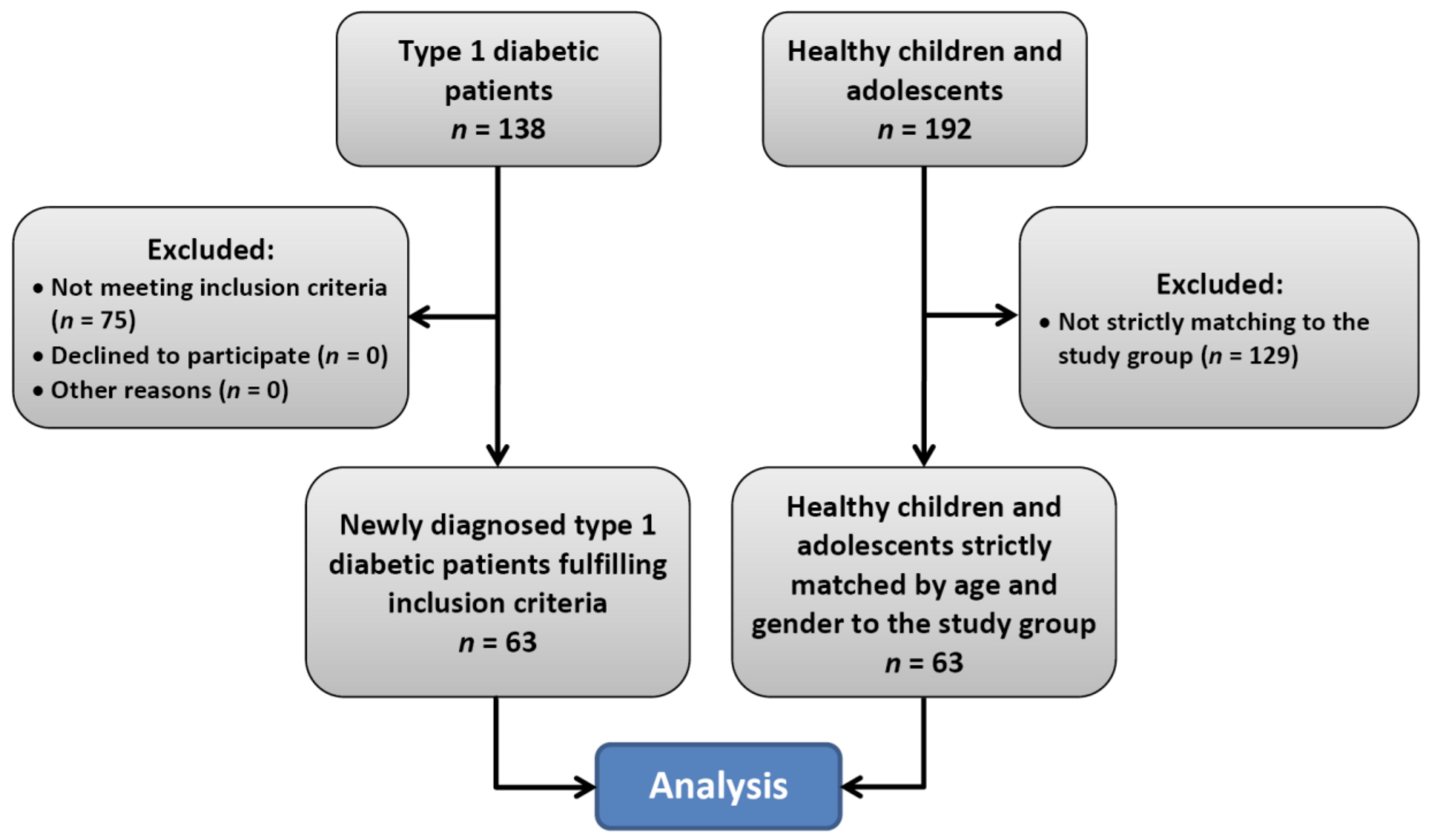
2.2. Subjects
2.3. Assessments
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Baumgartner, R.N.; Chumlea, W.C.; Roche, A.F. Estimation of body composition from bioelectric impedance of body segments. Am. J. Clin. Nutr. 1989, 50, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Shafer, K.J.; Siders, W.A.; Johnson, L.K.; Lukaski, H.C. Validity of segmental multiple-frequency bioelectrical impedance analysis to estimate body composition of adults across a range of body mass indexes. Nutrition 2009, 25, 25–32. [Google Scholar] [CrossRef]
- Stoklossa, C.A.J.; Forhan, M.; Padwal, R.S.; Gonzalez, M.C.; Prado, C.M. Practical considerations for body composition assessment of adults with class II/III obesity using Bioelectrical Impedance Analysis or Dual-Energy, X.-Ray Absorptiometry. Curr. Obes. Rep. 2016, 5, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Wan, C.S.; Ward, L.C.; Halim, J.; Gow, M.L.; Ho, M.; Briody, J.N.; Leung, K.; Cowell, C.T.; Garnett, S.P. Bioelectrical impedance analysis to estimate body composition, and change in adiposity, in overweight and obese adolescents: Comparison with dual-energy x-ray absorptiometry. BMC Pediatr. 2014, 14, 249. [Google Scholar] [CrossRef] [PubMed]
- Böhm, A.; Heitmann, B.L. The use of bioelectrical impedance analysis for body composition in epidemiological studies. Eur. J. Clin. Nutr. 2013, 67, S79. [Google Scholar] [CrossRef] [PubMed]
- Selberg, O.; Selberg, D. Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur. J. Appl. Physiol. 2002, 86, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Huo, X.; Wu, C.; Zhang, C.; Duan, Z. A bioelectrical impedance phase angle measuring system for assessment of nutritional status. Biomed. Mater. Eng. 2014, 24, 3657–3664. [Google Scholar] [CrossRef] [PubMed]
- Khalil, S.F.; Mohktar, M.S.; Ibrahim, F. The theory and fundamentals of bioimpedance analysis in clinical status monitoring and diagnosis of diseases. Sensors 2014, 14, 10895–10928. [Google Scholar] [CrossRef] [PubMed]
- Bosy-Westphal, A.; Danielzik, S.; Dörhöfer, R.P.; Later, W.; Wiese, S.; Müller, M.J. Phase angle from bioelectrical impedance analysis: Population reference values by age, sex, and body mass index. JPEN J. Parenter. Enteral. Nutr. 2006, 30, 309–316. [Google Scholar] [CrossRef]
- Redondo-del-Río, M.P.; Camina-Martín, M.A.; Marugan-de-Miguelsanz, J.M.; de- Mateo-Silleras, B. Bioelectrical impedance vector reference values for assessing body composition in a Spanish child and adolescent population. Am. J. Hum. Biol. 2017, 29, e22978. [Google Scholar] [CrossRef] [PubMed]
- Kuchnia, A.J.; Teigen, L.M.; Cole, A.J.; Mulasi, U.; Gonzalez, M.C.; Heymsfield, S.B.; Vock, D.M.; Earthman, C.P. Phase angle and impedance ratio: Reference cut-points from the United States National Health and Nutrition Examination Survey 1999-2004 from bioimpedance spectroscopy data. JPEN J. Parenter. Enteral. Nutr. 2017, 41, 1310–1315. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Stobäus, N.; Pirlich, M.; Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis--clinical relevance and applicability of impedance parameters. Clin. Nutr. 2012, 31, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Maddocks, M.; Kon, S.S.; Jones, S.E.; Canavan, J.L.; Nolan, C.M.; Higginson, I.J.; Gao, W.; Polkey, M.I.; Man, W.D. Bioelectrical impedance phase angle relates to function, disease severity and prognosis in stable chronic obstructive pulmonary disease. Clin. Nutr. 2015, 34, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Genton, L.; Pichard, C. Low phase angle determined by bioelectrical impedance analysis is associated with malnutrition and nutritional risk at hospital admission. Clin. Nutr. 2013, 32, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Buscemi, S.; Blunda, G.; Maneri, R.; Verga, S. Bioelectrical characteristics of type 1 and type 2 diabetic subjects with reference to body water compartments. Acta. Diabetol. 1998, 35, 220–223. [Google Scholar] [CrossRef]
- Dittmar, M.; Reber, H.; Kahaly, G.J. Bioimpedance phase angle indicates catabolism in Type 2 diabetes. Diabet. Med. 2015, 32, 1177–1185. [Google Scholar] [CrossRef]
- Kułaga, Z.; Różdżyńska-Świątkowska, A.; Grajda, A.; Gurzkowska, B.; Wojtyło, M.; Góźdź, M.; Świąder-Leśniak, A.; Litwin, M. Percentile charts for growth and nutritional status assessment in Polish children and adolescents from birth to 18 year of age. Standard. Med. Ped. 2015, 12, 119–135. [Google Scholar]
- Sun, S.S.; Chumlea, W.C.; Heymsfield, S.B.; Lukaski, H.C.; Schoeller, D.; Friedl, K.; Kuczmarski, R.J.; Flegal, K.M.; Johnson, C.L.; Hubbard, V.S. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am. J. Clin. Nutr. 2003, 77, 331–340. [Google Scholar] [CrossRef]
- Horlick, M.; Arpadi, S.M.; Bethel, J.; Wang, J.; Moye, J. Jr.; Cuff, P.; Pierson, R.N.Jr.; Kotler, D. Bioelectrical impedance analysis models for prediction of total body water and fat-free mass in healthy and HIV-infected children and adolescents. Am. J. Clin. Nutr. 2002, 76, 991–999. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis—part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef] [PubMed]
- Davis, N.L.; Bursell, J.D.; Evans, W.D.; Warner, J.T.; Gregory, J.W. Body composition in children with type 1 diabetes in the first year after diagnosis: Relationship to glycaemic control and cardiovascular risk. Arch. Dis. Child. 2012, 97, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Galli-Tsinopoulou, A.; Grammatikopoulou, M.G.; Stylianou, C.; Kokka, P.; Emmanouilidou, E. A preliminary case-control study on nutritional status, body composition, and glycemic control of Greek children and adolescents with type 1 diabetes. J. Diabetes. 2009, 1, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Szadkowska, A.; Madej, A.; Ziółkowska, K.; Szymańska, M.; Jeziorny, K.; Mianowska, B.; Pietrzak, I. Gender and Age—Dependent effect of type 1 diabetes on obesity and altered body composition in young adults. Ann. Agric. Environ. Med. 2015, 22, 124–128. [Google Scholar] [CrossRef] [PubMed]
- DCCT Research Group. Weight gain associated with intensive therapy in the Diabetes Control and Complications Trial. Diabetes Care 1988, 11, 567–573. [Google Scholar] [CrossRef]
- Purnell, J.Q.; Zinman, B.; Brunzell, J.D.; DCCT/EDIC Research Group. The effect of excess weight gain with intensive diabetes mellitus treatment on cardiovascular disease risk factors and atherosclerosis in type 1 diabetes mellitus: Results from the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study (DCCT/EDIC) study. Circulation. 2013, 127, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Gubitosi-Klug, R.A.; DCCT/EDIC Research Group. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study at 30 years: Summary and future directions. Diabetes Care. 2014, 37, 44–49. [Google Scholar] [CrossRef]
- Wierzbicka, E.; Swiercz, A.; Pludowski, P.; Jaworski, M.; Szalecki, M. Skeletal Status, Body Composition, and Glycaemic Control in Adolescents with Type 1 Diabetes Mellitus. J. Diabetes Res. 2018, 2018, 8121634. [Google Scholar] [CrossRef]
- Maratova, K.; Soucek, O.; Matyskova, J.; Hlavka, Z.; Petruzelkova, L.; Obermannova, B.; Pruhova, S.; Kolouskova, S.; Sumnik, Z. Muscle functions and bone strength are impaired in adolescents with type 1 diabetes. Bone 2018, 106, 22–27. [Google Scholar] [CrossRef]
- Coleman, S.K.; Rebalka, I.A.; D’Souza, D.M.; Hawke, T.J. Skeletal muscle as a therapeutic target for delaying type 1 diabetic complications. World J. Diabetes 2015, 6, 1323–1336. [Google Scholar] [CrossRef]
- Mameli, C.; Mazzantini, S.; Nasr, M.B.; Fiorina, P.; Scaramuzza, A.E.; Zuccotti, G.V. Explaining the increased mortality in type 1 diabetes. World J. Diabetes 2015, 6, 889–895. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Type 1 Diabetes Group | Control Group | p-Value |
|---|---|---|---|
| Age (years) | 10.78 ± 3.72 | 10.80 ± 3.73 | 0.967 |
| Girls | 10.93 ± 3.55 | 10.96 ± 3.56 | 0.947 |
| Boys | 10.66 ± 3.90 | 10.66 ± 3.90 | 1.000 |
| Body weight (kg) | 42.15 ± 21.08 | 39.93 ± 14.97 | 0.907 |
| Girls | 38.71 ± 16.69 | 38.53 ± 11.92 | 0.962 |
| Percentile * (n): | |||
| <3 | 2 | 1 | 0.613 |
| 3–10 | 4 | 1 | |
| 10–90 | 20 | 23 | |
| 90–97 | 1 | 1 | |
| >97 | 1 | 2 | |
| Boys | 44.89 ± 23.91 | 41.05 ± 17.11 | 0.720 |
| Percentile * (n): | |||
| <3 | 0 | 1 | 0.400 |
| 3–10 | 4 | 2 | |
| 10–90 | 24 | 26 | |
| 90–97 | 3 | 5 | |
| >97 | 4 | 1 | |
| Height (cm) | 145.80 ± 22.16 | 144.12 ± 19.63 | 0.653 |
| Girls | 143.93 ± 19.64 | 143.66 ± 18.60 | 0.958 |
| Low-to-age * | 1 | 1 | 0.354 |
| Normal * | 27 | 25 | |
| High-to-age * | 0 | 2 | |
| Boys | 147.30 ± 24.17 | 144.49 ± 20.68 | 0.602 |
| Low-to-age * | 0 | 0 | 0.673 |
| Normal * | 31 | 33 | |
| High-to-age * | 4 | 2 | |
| BMI (kg/m2) | 18.56 ± 4.57 | 18.52 ± 3.30 | 0.460 |
| Girls | 17.76 ± 3.40 | 18.26 ± 3.08 | 0.244 |
| Underweight * | 10 | 5 | 0.371 |
| Normal weight * | 15 | 19 | |
| Overweight * | 3 | 3 | |
| Obesity * | 0 | 1 | |
| Boys | 19.21 ± 4.94 | 18.72 ± 3.49 | 0.939 |
| Underweight * | 1 | 1 | 0.573 |
| Normal weight * | 27 | 24 | |
| Overweight * | 6 | 10 | |
| Obesity * | 1 | 0 |
| Parameter | Type 1 Diabetes Group (N = 63) | Control group (N = 63) | p-Value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Fat mass (kg) | 10.84 ± 8.33 | 9.07 ± 5.20 | 0.481 |
| Fat mass (% of body mass) | 23.96 ± 9.50 | 22.49 ± 9.44 | 0.386 |
| Fat mass index (kg/m2) | 4.66 ± 2.78 | 4.24 ± 2.33 | 0.364 |
| Fat free mass (kg) | 31.31 ± 14.49 | 30.86 ± 12.26 | 0.840 |
| Fat free mass (% of body mass) | 76.04 ± 9.50 | 77.51 ± 9.44 | 0.386 |
| Fat free mass index (kg/m2) | 13.81 ± 2.74 | 14.20 ± 2.26 | 0.218 |
| Muscle mass (kg) | 18.87 ± 10.01 | 20.03 ± 9.17 | 0.341 |
| Muscle mass (% of body mass) | 44.61 ± 6.58 | 49.40 ± 7.59 | <0.001 |
| Total body water (L) | 24.48 ± 10.61 | 24.28 ± 9.10 | 0.903 |
| Total body water (% of body mass) | 59.95 ± 8.62 | 61.36 ± 8.56 | 0.359 |
| Extracellular water (L) | 11.10 ± 4.44 | 10.57 ± 3.85 | 0.707 |
| Extracellular water (% of body mass) | 46.89 ± 7.34 | 44.05 ± 3.67 | 0.064 |
| Intracellular water (L) | 13.70 ± 6.49 | 13.76 ± 5.44 | 0.946 |
| Intracellular water (% of body mass) | 53.11 ± 7.34 | 55.95 ± 3.67 | 0.064 |
| Body cell mass (kg) | 15.14 ± 8.27 | 16.23 ± 7.57 | 0.308 |
| Body cell mass (% of body mass) | 46.89 ± 5.67 | 51.40 ± 4.19 | <0.001 |
| Body cell mass index (kg/m2) | 6.57 ± 1.80 | 7.37 ± 1.72 | 0.004 |
| Resistance (ohm) | 684.92 ± 99.29 | 659.98 ± 94.10 | 0.150 |
| Reactance (ohm) | 57.62 ± 10.41 | 63.83 ± 6.93 | <0.001 |
| Phase angle (−) | 4.85 ± 0.86 | 5.62 ± 0.81 | <0.001 |
| Parameter | Girls | p-Value | Boys | p-Value | ||
|---|---|---|---|---|---|---|
| Diabetes (N = 28) | Control (N = 28) | Diabetes (N = 35) | Control (N = 35) | |||
| Fat mass (kg) | 9.98 ± 6.53 | 9.77 ± 4.53 | 0.891 | 11.53 ± 9.57 | 8.50 ± 5.67 | 0.215 |
| Fat mass (% of body mass) | 23.65 ± 9.72 | 25.12 ± 8.56 | 0.555 | 24.21 ± 9.46 | 20.38 ± 9.47 | 0.072 |
| Fat mass index (kg/m2) | 4.37 ± 2.40 | 4.71 ± 2.39 | 0.611 | 4.90 ± 3.06 | 3.86 ± 2.25 | 0.079 |
| Fat free mass (kg) | 28.74 ± 11.00 | 28.76 ± 9.52 | 0.994 | 33.37 ± 16.63 | 32.55 ± 13.98 | 0.930 |
| Fat free mass (% of body mass) | 76.35 ± 9.72 | 74.88 ± 8.86 | 0.555 | 75.79 ± 9.46 | 79.62 ± 9.47 | 0.072 |
| Fat free mass index (kg/m2) | 13.18 ± 2.52 | 13.46 ± 1.78 | 0.628 | 14.32 ± 2.84 | 14.78 ± 2.45 | 0.247 |
| Muscle mass (kg) | 16.79 ± 7.25 | 18.29 ± 6.59 | 0.421 | 20.53 ± 11.60 | 21.42 ± 10.70 | 0.597 |
| Muscle mass (% of body mass) | 43.62 ± 5.70 | 47.20 ± 6.17 | 0.028 | 45.41 ± 7.19 | 51.15 ± 8.23 | 0.003 |
| Total body water (L) | 22.25 ± 7.82 | 22.35 ± 6.92 | 0.958 | 26.25 ± 12.23 | 25.81 ± 10.37 | 0.893 |
| Total body water (% of body mass) | 59.75 ± 9.02 | 58.55 ± 7.54 | 0.590 | 60.11 ± 8.42 | 63.61 ± 8.77 | 0.093 |
| Extracellular water (L) | 10.48 ± 3.64 | 9.85 ± 3.12 | 0.629 | 11.59 ± 4.98 | 11.15 ± 4.30 | 0.930 |
| Extracellular water (% of body mass) | 48.31 ± 8.70 | 44.25 ± 3.08 | 0.119 | 45.76 ± 5.92 | 43.89 ± 4.12 | 0.131 |
| Intracellular water (L) | 12.13 ± 4.99 | 12.65 ± 4.05 | 0.793 | 14.95 ± 7.31 | 14.65 ± 6.25 | 0.995 |
| Intracellular water (% of body mass) | 51.69 ± 8.70 | 55.75 ± 3.08 | 0.119 | 54.24 ± 5.92 | 56.11 ± 4.12 | 0.131 |
| Body cell mass (kg) | 13.39 ± 5.99 | 14.79 ± 5.38 | 0.362 | 16.55 ± 9.57 | 17.37 ± 8.86 | 0.565 |
| Body cell mass (% of body mass) | 45.60 ± 6.30 | 50.90 ± 3.05 | <0.001 | 47.91 ± 4.96 | 51.79 ± 4.93 | 0.002 |
| Body cell mass index (kg/m2) | 6.11 ± 1.50 | 6.91 ± 1.27 | 0.037 | 6.93 ± 1.95 | 7.73 ± 1.96 | 0.039 |
| Resistance (ohm) | 712.75 ± 102.10 | 700.57 ± 79.01 | 0.620 | 662.66 ± 92.47 | 627.51 ± 93.53 | 0.119 |
| Reactance (ohm) | 58.07 ± 12.66 | 66.71 ± 5.14 | 0.003 | 57.26 ± 8.38 | 61.51 ± 7.36 | 0.027 |
| Phase angle (−) | 4.66 ± 0.84 | 5.49 ± 0.56 | <0.001 | 5.00 ± 0.85 | 5.72 ± 0.97 | 0.001 |
| Age Range (years) | Phase Angle Percentiles | Girls | Boys | ||
|---|---|---|---|---|---|
| Diabetes | Control | Diabetes | Control | ||
| All (n) | 28 | 28 | 35 | 35 | |
| ≥10th percentile | 14 | 27 | 20 | 30 | |
| <10th percentile | 14 | 1 | 15 | 5 | |
| <5th percentile | 13 | 1 | 11 | 1 | |
| 4–9 (n) | 10 | 10 | 13 | 13 | |
| ≥10th percentile | 3 | 10 | 7 | 10 | |
| <10th percentile | 7 | 0 | 6 | 3 | |
| <5th percentile | 7 | 0 | 5 | 0 | |
| 10–13 (n) | 13 | 13 | 16 | 16 | |
| ≥10th percentile | 9 | 13 | 10 | 14 | |
| <10th percentile | 4 | 0 | 6 | 2 | |
| <5th percentile | 3 | 0 | 5 | 1 | |
| 14–18 (n) | 5 | 5 | 6 | 6 | |
| ≥10th percentile | 2 | 4 | 3 | 6 | |
| <10th percentile | 3 | 1 | 3 | 0 | |
| <5th percentile | 3 | 1 | 1 | 0 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Więch, P.; Bazaliński, D.; Sałacińska, I.; Binkowska-Bury, M.; Korczowski, B.; Mazur, A.; Kózka, M.; Dąbrowski, M. Decreased Bioelectrical Impedance Phase Angle in Hospitalized Children and Adolescents with Newly Diagnosed Type 1 Diabetes: A Case-Control Study. J. Clin. Med. 2018, 7, 516. https://doi.org/10.3390/jcm7120516
Więch P, Bazaliński D, Sałacińska I, Binkowska-Bury M, Korczowski B, Mazur A, Kózka M, Dąbrowski M. Decreased Bioelectrical Impedance Phase Angle in Hospitalized Children and Adolescents with Newly Diagnosed Type 1 Diabetes: A Case-Control Study. Journal of Clinical Medicine. 2018; 7(12):516. https://doi.org/10.3390/jcm7120516
Chicago/Turabian StyleWięch, Paweł, Dariusz Bazaliński, Izabela Sałacińska, Monika Binkowska-Bury, Bartosz Korczowski, Artur Mazur, Maria Kózka, and Mariusz Dąbrowski. 2018. "Decreased Bioelectrical Impedance Phase Angle in Hospitalized Children and Adolescents with Newly Diagnosed Type 1 Diabetes: A Case-Control Study" Journal of Clinical Medicine 7, no. 12: 516. https://doi.org/10.3390/jcm7120516
APA StyleWięch, P., Bazaliński, D., Sałacińska, I., Binkowska-Bury, M., Korczowski, B., Mazur, A., Kózka, M., & Dąbrowski, M. (2018). Decreased Bioelectrical Impedance Phase Angle in Hospitalized Children and Adolescents with Newly Diagnosed Type 1 Diabetes: A Case-Control Study. Journal of Clinical Medicine, 7(12), 516. https://doi.org/10.3390/jcm7120516







