A DNA Methylation-Based Test for Breast Cancer Detection in Circulating Cell-Free DNA
Abstract
1. Introduction
2. Experimental Section
2.1. Patients and Samples Collection
2.2. Immunohistochemistry
2.3. DNA Extraction
2.4. Bisulfite Treatment and Whole Genome Amplification (WGA)
2.5. Quantitative Methylation-Specific Polymerase Chain Reaction (QMSP)
2.6. Statistical Analysis
3. Results
3.1. Clinical and Pathological Data of Tissue Cohort
3.2. Assessment of BrC and NBr Tissue Samples Methylation Levels
3.3. Association between Promoter Methylation Levels, Molecular Subtypes and Standard Clinicopathological Parameters in Cohort #1
3.4. Survival Analysis
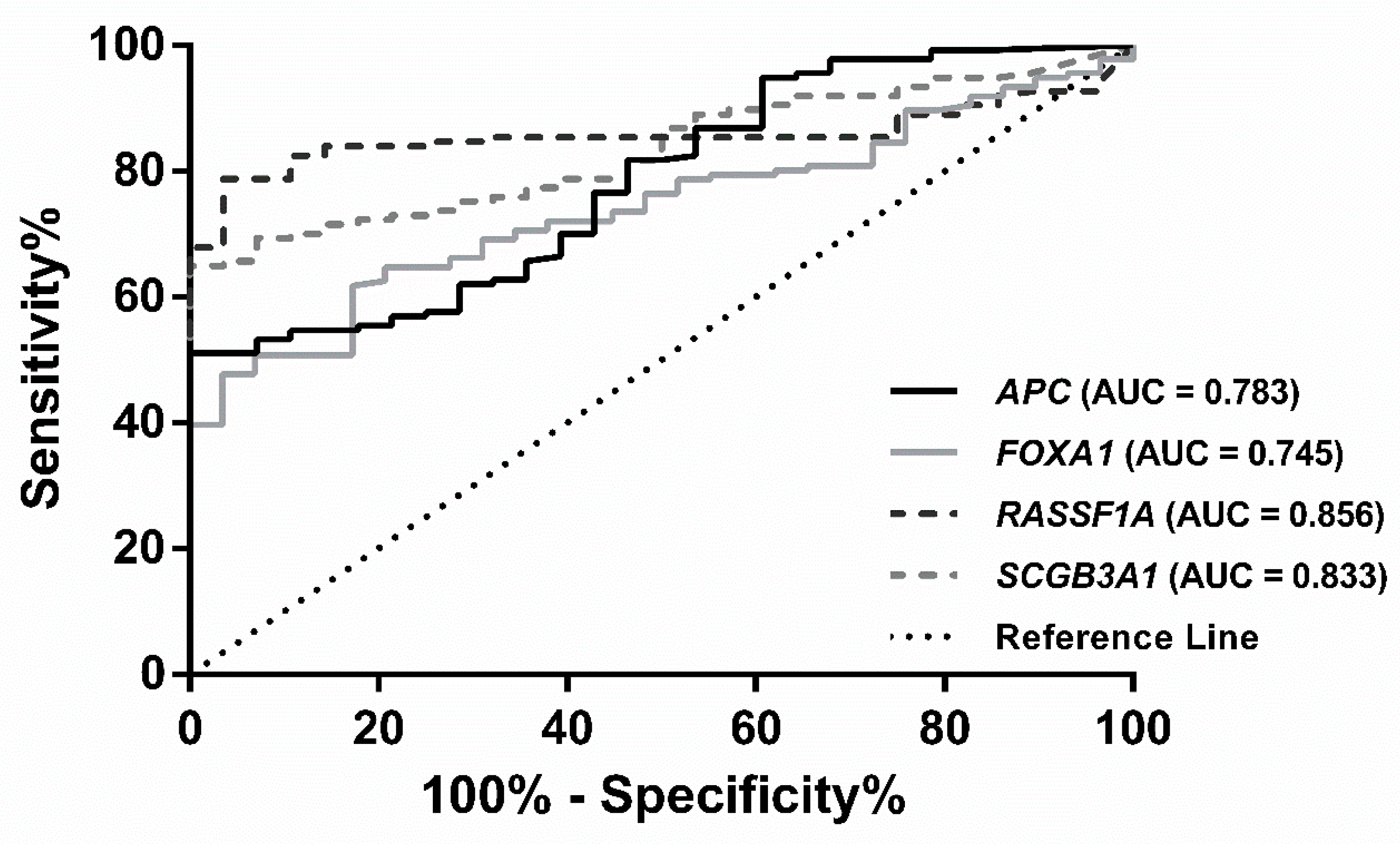
3.5. Biomarker Detection Performance in ccfDNA Liquid Biopsies (Cohort #2)
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Tabar, L.; Vitak, B.; Chen, H.H.; Yen, M.F.; Duffy, S.W.; Smith, R.A. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast carcinoma mortality. Cancer 2001, 91, 1724–1731. [Google Scholar] [CrossRef]
- Pisano, E.D.; Gatsonis, C.; Hendrick, E.; Yaffe, M.; Baum, J.K.; Acharyya, S.; Conant, E.F.; Fajardo, L.L.; Bassett, L.; D’Orsi, C.; et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N. Engl. J. Med. 2005, 353, 1773–1783. [Google Scholar] [CrossRef] [PubMed]
- Warner, E. Clinical practice. Breast-cancer screening. N. Engl. J. Med. 2011, 365, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Sorlie, T.; Perou, C.M.; Tibshirani, R.; Aas, T.; Geisler, S.; Johnsen, H.; Hastie, T.; Eisen, M.B.; van de Rijn, M.; Jeffrey, S.S.; et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc. Nat. Acad. Sci. USA 2001, 98, 10869–10874. [Google Scholar] [CrossRef] [PubMed]
- Senkus, E.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rutgers, E.; Zackrisson, S.; Cardoso, F.; Committee, E.G. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26 (Suppl. 5), v8–v30. [Google Scholar] [CrossRef] [PubMed]
- Jeronimo, C.; Costa, I.; Martins, M.C.; Monteiro, P.; Lisboa, S.; Palmeira, C.; Henrique, R.; Teixeira, M.R.; Lopes, C. Detection of gene promoter hypermethylation in fine needle washings from breast lesions. Clin. Cancer Res. 2003, 9, 3413–3417. [Google Scholar] [PubMed]
- Jeronimo, C.; Monteiro, P.; Henrique, R.; Dinis-Ribeiro, M.; Costa, I.; Costa, V.L.; Filipe, L.; Carvalho, A.L.; Hoque, M.O.; Pais, I.; et al. Quantitative hypermethylation of a small panel of genes augments the diagnostic accuracy in fine-needle aspirate washings of breast lesions. Breast Cancer Res. Treat. 2008, 109, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.T.; Monteiro, P.; Ramalho-Carvalho, J.; Costa, V.L.; Dinis-Ribeiro, M.; Leal, C.; Henrique, R.; Jeronimo, C. High RASSF1A promoter methylation levels are predictive of poor prognosis in fine-needle aspirate washings of breast cancer lesions. Breast Cancer Res. Treat. 2011, 129, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bediaga, N.G.; Acha-Sagredo, A.; Guerra, I.; Viguri, A.; Albaina, C.; Ruiz Diaz, I.; Rezola, R.; Alberdi, M.J.; Dopazo, J.; Montaner, D.; et al. DNA methylation epigenotypes in breast cancer molecular subtypes. Breast Cancer Res. 2010, 12, R77. [Google Scholar] [CrossRef] [PubMed]
- Cancer Genome Atlas, N. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef]
- Győrffy, B.; Bottai, G.; Fleischer, T.; Munkácsy, G.; Budczies, J.; Paladini, L.; Børresen-Dale, A.L.; Kristensen, V.N.; Santarpia, L. Aberrant DNA methylation impacts gene expression and prognosis in breast cancer subtypes. Int. J. Cancer 2016, 138, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Fackler, M.J.; Lee, J.H.; Choi, C.; Park, M.H.; Yoon, J.H.; Zhang, Z.; Sukumar, S. Basal-like breast cancer displays distinct patterns of promoter methylation. Cancer Biol. Ther. 2010, 9, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Martens, J.W.; Nimmrich, I.; Koenig, T.; Look, M.P.; Harbeck, N.; Model, F.; Kluth, A.; Bolt-de Vries, J.; Sieuwerts, A.M.; Portengen, H.; et al. Association of DNA methylation of phosphoserine aminotransferase with response to endocrine therapy in patients with recurrent breast cancer. Cancer Res. 2005, 65, 4101–4117. [Google Scholar] [CrossRef] [PubMed]
- Esteller, M. Epigenetics in cancer. N. Engl. J. Med. 2008, 358, 1148–1159. [Google Scholar] [CrossRef] [PubMed]
- Van Hoesel, A.Q.; Sato, Y.; Elashoff, D.A.; Turner, R.R.; Giuliano, A.E.; Shamonki, J.M.; Kuppen, P.J.; van de Velde, C.J.; Hoon, D.S. Assessment of DNA methylation status in early stages of breast cancer development. Br. J. Cancer 2013, 108, 2033–2038. [Google Scholar] [CrossRef] [PubMed]
- Muggerud, A.A.; Ronneberg, J.A.; Warnberg, F.; Botling, J.; Busato, F.; Jovanovic, J.; Solvang, H.; Bukholm, I.; Borresen-Dale, A.L.; Kristensen, V.N.; et al. Frequent aberrant DNA methylation of ABCB1, FOXC1, PPP2R2B and PTEN in ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res. 2010, 12, R3. [Google Scholar] [CrossRef] [PubMed]
- Fackler, M.J.; McVeigh, M.; Evron, E.; Garrett, E.; Mehrotra, J.; Polyak, K.; Sukumar, S.; Argani, P. DNA methylation of RASSF1A, HIN-1, RAR-beta, Cyclin D2 and Twist in in situ and invasive lobular breast carcinoma. Int. J. Cancer 2003, 107, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Widschwendter, M.; Jones, P.A. DNA methylation and breast carcinogenesis. Oncogene 2002, 21, 5462–5482. [Google Scholar] [CrossRef] [PubMed]
- Heyn, H.; Esteller, M. DNA methylation profiling in the clinic: Applications and challenges. Nat. Rev.Genet. 2012, 13, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Jeronimo, C.; Henrique, R. Epigenetic biomarkers in urological tumors: A systematic review. Cancer Lett. 2014, 342, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Muller, H.M.; Widschwendter, A.; Fiegl, H.; Ivarsson, L.; Goebel, G.; Perkmann, E.; Marth, C.; Widschwendter, M. DNA methylation in serum of breast cancer patients: An independent prognostic marker. Cancer Res. 2003, 63, 7641–7645. [Google Scholar] [PubMed]
- Gobel, G.; Auer, D.; Gaugg, I.; Schneitter, A.; Lesche, R.; Muller-Holzner, E.; Marth, C.; Daxenbichler, G. Prognostic significance of methylated RASSF1A and PITX2 genes in blood- and bone marrow plasma of breast cancer patients. Breast Cancer Res. Treat. 2011, 130, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.M.; Tsui, D.W.Y. Circulating cell-free DNA for non-invasive cancer management. Cancer Genet. 2018. [Google Scholar] [CrossRef] [PubMed]
- Kloten, V.; Becker, B.; Winner, K.; Schrauder, M.G.; Fasching, P.A.; Anzeneder, T.; Veeck, J.; Hartmann, A.; Knuchel, R.; Dahl, E. Promoter hypermethylation of the tumor-suppressor genes ITIH5, DKK3, and RASSF1A as novel biomarkers for blood-based breast cancer screening. Breast Cancer Res. 2013, 15, R4. [Google Scholar] [CrossRef] [PubMed]
- Radpour, R.; Barekati, Z.; Kohler, C.; Lv, Q.; Burki, N.; Diesch, C.; Bitzer, J.; Zheng, H.; Schmid, S.; Zhong, X.Y. Hypermethylation of tumor suppressor genes involved in critical regulatory pathways for developing a blood-based test in breast cancer. PloS ONE 2011, 6, e16080. [Google Scholar] [CrossRef] [PubMed]
- Avraham, A.; Uhlmann, R.; Shperber, A.; Birnbaum, M.; Sandbank, J.; Sella, A.; Sukumar, S.; Evron, E. Serum DNA methylation for monitoring response to neoadjuvant chemotherapy in breast cancer patients. Int. J. Cancer 2012, 131, E1166–E1172. [Google Scholar] [CrossRef] [PubMed]
- Pasculli, B.; Barbano, R.; Parrella, P. Epigenetics of breast cancer: Biology and clinical implication in the era of precision medicine. Semin. Cancer biol. 2018, 51, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Locke, W.J.; Zotenko, E.; Stirzaker, C.; Robinson, M.D.; Hinshelwood, R.A.; Stone, A.; Reddel, R.R.; Huschtscha, L.I.; Clark, S.J. Coordinated epigenetic remodelling of transcriptional networks occurs during early breast carcinogenesis. Clin. Epigenet. 2015, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- Pearson, H.; Stirling, D. DNA extraction from tissue. Methods Mol. Biol. 2003, 226, 33–34. [Google Scholar] [CrossRef] [PubMed]
- Schisterman, E.F.; Perkins, N.J.; Liu, A.; Bondell, H. Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 2005, 16, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Schuur, E.R.; DeAndrade, J.P. Breast Cancer: Molecular Mechanisms, Diagnosis, and Treatment. In International Manual of Oncology Practice; de Mello, A.R., Tavares, Á., Mountzios, G., Eds.; Springer International Publishing: Cham, Switzerland, 2015; pp. 155–200. [Google Scholar]
- Schnitt, S.J.; Lakhani, S.R. Breast Cancer. In World Cancer Report 2014; Stewart, B., Wild, C.P., Eds.; International Agency for Research on Cancer: Lyon, France, 2014; pp. 362–373. [Google Scholar]
- Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: An independent review. Lancet 2012, 380, 1778–1786. [Google Scholar] [CrossRef]
- Olkhov-Mitsel, E.; Zdravic, D.; Kron, K.; van der Kwast, T.; Fleshner, N.; Bapat, B. Novel multiplex MethyLight protocol for detection of DNA methylation in patient tissues and bodily fluids. Sci. Rep. 2014, 4, 4432. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Chen, H.Y.; Bai, E.Q.; Luo, Y.X.; Fu, R.J.; He, Y.S.; Jiang, J.; Wang, H.Q. Development of a multiplex MethyLight assay for the detection of multigene methylation in human colorectal cancer. Cancer Genet. Cytogenet. 2010, 202, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bu, D.; Lewis, C.M.; Sarode, V.; Chen, M.; Ma, X.; Lazorwitz, A.M.; Rao, R.; Leitch, M.; Moldrem, A.; Andrews, V.; et al. Identification of breast cancer DNA methylation markers optimized for fine-needle aspiration samples. Cancer Epidemiol. Biomark. Prev. 2013, 22, 2212–2221. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.J.; Jain, R.K.; Leung, S.; Choo, J.; Nielsen, T.; Huntsman, D.; Nakshatri, H.; Badve, S. FOXA1 is an independent prognostic marker for ER-positive breast cancer. Breast Cancer Res. Treat. 2012, 131, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Albergaria, A.; Paredes, J.; Sousa, B.; Milanezi, F.; Carneiro, V.; Bastos, J.; Costa, S.; Vieira, D.; Lopes, N.; Lam, E.W.; et al. Expression of FOXA1 and GATA-3 in breast cancer: The prognostic significance in hormone receptor-negative tumours. Breast Cancer Res. 2009, 11, R40. [Google Scholar] [CrossRef] [PubMed]
- Parrella, P. Epigenetic Signatures in Breast Cancer: Clinical Perspective. Breast Care 2010, 5, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Maisonneuve, P.; Disalvatore, D.; Rotmensz, N.; Curigliano, G.; Colleoni, M.; Dellapasqua, S.; Pruneri, G.; Mastropasqua, M.G.; Luini, A.; Bassi, F.; et al. Proposed new clinicopathological surrogate definitions of luminal A and luminal B (HER2-negative) intrinsic breast cancer subtypes. Breast Cancer Res. 2014, 16, R65. [Google Scholar] [CrossRef] [PubMed]
- Prat, A.; Cheang, M.C.; Martin, M.; Parker, J.S.; Carrasco, E.; Caballero, R.; Tyldesley, S.; Gelmon, K.; Bernard, P.S.; Nielsen, T.O.; et al. Prognostic significance of progesterone receptor-positive tumor cells within immunohistochemically defined luminal a breast cancer. J. Clin. Oncol. 2013, 31, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Coates, A.S.; Winer, E.P.; Goldhirsch, A.; Gelber, R.D.; Gnant, M.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.-J.; André, F.; Baselga, J. Tailoring therapies—Improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann. Oncol. 2015, 26, 1533–1546. [Google Scholar] [CrossRef] [PubMed]
- Stefansson, O.A.; Jonasson, J.G.; Olafsdottir, K.; Hilmarsdottir, H.; Olafsdottir, G.; Esteller, M.; Johannsson, O.T.; Eyfjord, J.E. CpG island hypermethylation of BRCA1 and loss of pRb as co-occurring events in basal/triple-negative breast cancer. Epigenetics 2011, 6, 638–649. [Google Scholar] [CrossRef] [PubMed]
- Sunami, E.; Shinozaki, M.; Sim, M.S.; Nguyen, S.L.; Vu, A.T.; Giuliano, A.E.; Hoon, D.S. Estrogen receptor and HER2/neu status affect epigenetic differences of tumor-related genes in primary breast tumors. Breast Cancer Res. 2008, 10, R46. [Google Scholar] [CrossRef] [PubMed]
- Stirzaker, C.; Zotenko, E.; Clark, S.J. Genome-wide DNA methylation profiling in triple-negative breast cancer reveals epigenetic signatures with important clinical value. Mol. Cell Oncol. 2016, 3, e1038424. [Google Scholar] [CrossRef] [PubMed]
- Stefansson, O.A.; Moran, S.; Gomez, A.; Sayols, S.; Arribas-Jorba, C.; Sandoval, J.; Hilmarsdottir, H.; Olafsdottir, E.; Tryggvadottir, L.; Jonasson, J.G.; et al. A DNA methylation-based definition of biologically distinct breast cancer subtypes. Mol. Oncol. 2015, 9, 555–568. [Google Scholar] [CrossRef] [PubMed]
- Tisserand, P.; Fouquet, C.; Barrois, M.; Gallou, C.; Dendale, R.; Stoppa-Lyonnet, D.; Sastre-Garau, X.; Fourquet, A.; Soussi, T. Lack of HIN-1 methylation defines specific breast tumor subtypes including medullary carcinoma of the breast and BRCA1-linked tumors. Cancer Biol. Ther. 2003, 2, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Benevolenskaya, E.V.; Islam, A.B.; Ahsan, H.; Kibriya, M.G.; Jasmine, F.; Wolff, B.; Al-Alem, U.; Wiley, E.; Kajdacsy-Balla, A.; Macias, V.; et al. DNA methylation and hormone receptor status in breast cancer. Clin. Epigenet. 2016, 8, 17. [Google Scholar] [CrossRef] [PubMed]
- Widschwendter, M.; Siegmund, K.D.; Müller, H.M.; Fiegl, H.; Marth, C.; Müller-Holzner, E.; Jones, P.A.; Laird, P.W. Association of breast cancer DNA methylation profiles with hormone receptor status and response to tamoxifen. Cancer Res. 2004, 64, 3807–3813. [Google Scholar] [CrossRef] [PubMed]
- Gong, C.; Fujino, K.; Monteiro, L.; Gomes, A.; Drost, R.; Davidson-Smith, H.; Takeda, S.; Khoo, U.; Jonkers, J.; Sproul, D.; et al. FOXA1 repression is associated with loss of BRCA1 and increased promoter methylation and chromatin silencing in breast cancer. Oncogene 2014, 34, 5012–5024. [Google Scholar] [CrossRef] [PubMed]
- Sturgeon, S.R.; Balasubramanian, R.; Schairer, C.; Muss, H.B.; Ziegler, R.G.; Arcaro, K.F. Detection of promoter methylation of tumor suppressor genes in serum DNA of breast cancer cases and benign breast disease controls. Epigenetics 2012, 7, 1258–1267. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Shin, M.-H.; Kweon, S.-S.; Park, M.H.; Yoon, J.H.; Lee, J.S.; Choi, C.; Fackler, M.J.; Sukumar, S. Evaluation of promoter hypermethylation detection in serum as a diagnostic tool for breast carcinoma in Korean women. Gynecol. Oncol. 2010, 118, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Hoque, M.O.; Feng, Q.; Toure, P.; Dem, A.; Critchlow, C.W.; Hawes, S.E.; Wood, T.; Jeronimo, C.; Rosenbaum, E.; Stern, J.; et al. Detection of aberrant methylation of four genes in plasma DNA for the detection of breast cancer. J. Clin. Oncol. 2006, 24, 4262–4269. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Galán, J.; Torres, B.; del Moral, R.; Muñoz-Gámez, J.A.; Martín-Oliva, D.; Villalobos, M.; Núñez, M.I.; Luna, J.D.D.; Oliver, F.J.; Almodóvar, J.M.R.D. Quantitative detection of methylated ESR1 and 14-3-3-σ gene promoters in serum as candidate biomarkers for diagnosis of breast cancer and evaluation of treatment efficacy. Cancer Biol. Ther. 2008, 7, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Nandi, K.; Yadav, P.; Mir, R.; Khurana, N.; Agarwal, P.; Saxena, A. The Clinical Significance of Rassf1a and Cdh1 Hypermethylation in Breast Cancer Patients. Int. J. Sci. Res. 2008, in press. [Google Scholar]
- Papadopoulou, E.; Davilas, E.; Sotiriou, V.; Georgakopoulos, E.; Georgakopoulou, S.; Koliopanos, A.; Aggelakis, F.; Dardoufas, K.; Agnanti, N.J.; Karydas, I. Cell-free DNA and RNA in Plasma as a New Molecular Marker for Prostate and Breast Cancer. Ann. N. Y. Acad. Sci. 2006, 1075, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Shan, M.; Yin, H.; Li, J.; Li, X.; Wang, D.; Su, Y.; Niu, M.; Zhong, Z.; Wang, J.; Zhang, X.; et al. Detection of aberrant methylation of a six-gene panel in serum DNA for diagnosis of breast cancer. Oncotarget 2016, 7, 18485–18494. [Google Scholar] [CrossRef] [PubMed]
- Skvortsova, T.E.; Rykova, E.Y.; Tamkovich, S.N.; Bryzgunova, O.E.; Starikov, A.V.; Kuznetsova, N.P.; Vlassov, V.V.; Laktionov, P.P. Cell-free and cell-bound circulating DNA in breast tumours: DNA quantification and analysis of tumour-related gene methylation. Br. J. Cancer 2006, 94, 1492–1495. [Google Scholar] [CrossRef] [PubMed]
- Van der Auwera, I.; Elst, H.; Van Laere, S.; Maes, H.; Huget, P.; Van Dam, P.; Van Marck, E.; Vermeulen, P.; Dirix, L. The presence of circulating total DNA and methylated genes is associated with circulating tumour cells in blood from breast cancer patients. Br. J. Cancer 2009, 100, 1277. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Nakayama, T.; Kajita, M.; Miyake, T.; Iwamoto, T.; Kim, S.J.; Sakai, A.; Ishihara, H.; Tamaki, Y.; Noguchi, S. Detection of aberrant promoter methylation of GSTP1, RASSF1A, and RARβ2 in serum DNA of patients with breast cancer by a newly established one-step methylation-specific PCR assay. Breast Cancer Res. Treat. 2012, 132, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.A.; Pusch, C.M.; Hamed, T.; Rashad, H.; Idris, A.; El-Fadle, A.A.; Blin, N. Epigenetic alterations by methylation of RASSF1A and DAPK1 promoter sequences in mammary carcinoma detected in extracellular tumor DNA. Cancer Genet. Cytogenet. 2010, 199, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Roperch, J.P.; Incitti, R.; Forbin, S.; Bard, F.; Mansour, H.; Mesli, F.; Baumgaertner, I.; Brunetti, F.; Sobhani, I. Aberrant methylation of NPY, PENK, and WIF1 as a promising marker for blood-based diagnosis of colorectal cancer. BMC Cancer 2013, 13, 566. [Google Scholar] [CrossRef] [PubMed]
- Fackler, M.J.; McVeigh, M.; Mehrotra, J.; Blum, M.A.; Lange, J.; Lapides, A.; Garrett, E.; Argani, P.; Sukumar, S. Quantitative multiplex methylation-specific PCR assay for the detection of promoter hypermethylation in multiple genes in breast cancer. Cancer Res. 2004, 64, 4442–4452. [Google Scholar] [CrossRef] [PubMed]
- Melnikov, A.A.; Scholtens, D.M.; Wiley, E.L.; Khan, S.A.; Levenson, V.V. Array-based multiplex analysis of DNA methylation in breast cancer tissues. J. Mol. Diagn. 2008, 10, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Liao, K.-M.; Chao, T.-B.; Tian, Y.-F.; Lin, C.-Y.; Lee, S.-W.; Chuang, H.-Y.; Chan, T.-C.; Chen, T.-J.; Hsing, C.-H.; Sheu, M.-J. Overexpression of the PSAT1 Gene in Nasopharyngeal Carcinoma Is an Indicator of Poor Prognosis. J. Cancer 2016, 7, 1088–1094. [Google Scholar] [CrossRef] [PubMed]
- Klajic, J.; Fleischer, T.; Dejeux, E.; Edvardsen, H.; Warnberg, F.; Bukholm, I.; Lonning, P.E.; Solvang, H.; Borresen-Dale, A.L.; Tost, J.; et al. Quantitative DNA methylation analyses reveal stage dependent DNA methylation and association to clinico-pathological factors in breast tumors. BMC Cancer 2013, 13, 456. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Mirza, S.; Yang, Y.H.; Parshad, R.; Hazrah, P.; Datta Gupta, S.; Ralhan, R. Prognostic relevance of promoter hypermethylation of multiple genes in breast cancer patients. Cell Oncol. 2009, 31, 487–500. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.H.; Shen, J.; Gammon, M.D.; Zhang, Y.J.; Wang, Q.; Gonzalez, K.; Xu, X.; Bradshaw, P.T.; Teitelbaum, S.L.; Garbowski, G.; et al. Prognostic significance of gene-specific promoter hypermethylation in breast cancer patients. Breast Cancer Res. Treat. 2012, 131, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Buhmeida, A.; Merdad, A.; El-Maghrabi, J.; Al-Thobaiti, F.; Ata, M.; Bugis, A.; Syrjänen, K.; Abuzenadah, A.; Chaudhary, A.; Gari, M. RASSF1A methylation is predictive of poor prognosis in female breast cancer in a background of overall low methylation frequency. Anticancer Res. 2011, 31, 2975–2981. [Google Scholar] [PubMed]
- Jiang, Y.; Cui, L.; Chen, W.D.; Shen, S.H.; Ding, L.D. The prognostic role of RASSF1A promoter methylation in breast cancer: A meta-analysis of published data. PloS ONE 2012, 7, e36780. [Google Scholar] [CrossRef] [PubMed]

| Genes | Sensitivity % | Specificity % | PPV a % | NPV b % | Accuracy % |
|---|---|---|---|---|---|
| APC | 51.09 | 100.0 | 100.0 | 29.47 | 59.39 |
| CCND2 | 72.26 | 92.86 | 98.02 | 40.63 | 75.76 |
| FOXA1 | 62.04 | 82.14 | 94.44 | 30.67 | 65.45 |
| PSAT1 | 91.24 | 50.00 | 89.93 | 53.85 | 84.24 |
| RASSF1A | 78.83 | 96.43 | 99.08 | 48.21 | 81.82 |
| SCGB3A1 | 64.96 | 100.0 | 100.0 | 36.84 | 70.91 |
| APC/FOXA1 RASSF1A/SCGB3A1 | 97.81 | 78.57 | 95.71 | 88.00 | 94.55 |
| Disease-Free Survival | Variable | HR a | CI b (95%) | p Value |
|---|---|---|---|---|
| Univariable | Grade | |||
| G1 | 1 | |||
| G2 c & G3 | 2.054 | 1.029–4.098 | 0.041 | |
| pN Stage | ||||
| N0 d & N1 | 1 | |||
| N2 & N3 | 3.894 | 1.940–7.812 | <0.001 | |
| PSAT1 | ||||
| >P75 e | 1 | |||
| ≤P75 | 3.707 | 1.133–12.127 | 0.030 | |
| Multivariable | Grade | |||
| G1 | 1 | |||
| G2 & G3 | 1.490 | 0.717–3.096 | 0.286 | |
| pN Stage | ||||
| N0 & N1 | 1 | |||
| N2 & N3 | 4.345 | 2.114–8.930 | <0.001 | |
| PSAT1 | ||||
| >P75 e | 1 | |||
| ≤P75 | 3.613 | 1.077–12.123 | 0.038 | |
| Disease-Specific Survival | Variable | HR a | CI b (95%) | pValue |
| Univariable | Grade | |||
| G1 | 1 | |||
| G2 & G3 | 2.725 | 1.155–6.428 | 0.022 | |
| pN Stage | ||||
| N0 & N1 | 1 | |||
| N2 & N3 | 4.061 | 1.814–9.089 | 0.001 | |
| FOXA1 | ||||
| ≤P75 f | 1 | |||
| >P75 | 2.678 | 1.200–5.978 | 0.016 | |
| Multivariable | Grade | |||
| G1 | 1 | |||
| G2 & G3 | 2.005 | 0.082–4.866 | 0.124 | |
| pN Stage | ||||
| N0 & N1 | 1 | |||
| N2 & N3 | 4.855 | 1.981–10.611 | <0.001 | |
| FOXA1 | ||||
| ≤P75 f | 1 | |||
| >P75 | 2.710 | 1.161–6.324 | 0.021 |
| Genes | Sensitivity % | Specificity % | PPV a % | NPV b % | Accuracy % |
|---|---|---|---|---|---|
| APC | 27.27 | 94.87 | 85.71 | 53.62 | 59.04 |
| FOXA1 | 68.18 | 82.05 | 81.08 | 69.57 | 74.70 |
| RASSF1A | 13.64 | 100.0 | 100.0 | 50.65 | 54.22 |
| APC/FOXA1/RASSF1A | 81.82 | 76.92 | 80.00 | 78.95 | 79.52 |
| Genes/Panel | Controls (Healthy Donors) | Patients | References | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| HIC-1/RARβ2/RASSF1Aa | 0/10 | 0% | 18/20 | 90% | [60] |
| APC | 0/38 | 0% | 8/47 | 17% | [55] |
| GSTP1 | 0/38 | 0% | 12/47 | 26% | |
| RARβ2 | 3/38 | 8% | 12/47 | 26% | |
| RASSF1A | 2/38 | 5% | 15/47 | 32% | |
| APC/GSTP1/RARβ2/RASSF1A | 5/38 | 13% | 29/47 | 62% | |
| ATM | 0/14 | 0% | 13/50 | 26% | [58] |
| RASSF1A | 0/14 | 0% | 7/50 | 14% | |
| ATM/RASSF1A | 0/14 | 0% | 18/50 | 36% | |
| RARβ2 | 8/125 | 6% | 103/119 | 87% | [54] |
| RASSF1A | 6/125 | 5% | 39/119 | 33% | |
| SCGB3A1 | 0/125 | 0% | 36/119 | 30% | |
| Twist | 10/125 | 8% | 65/119 | 55% | |
| RARβ2/RASSF1A/SCGB3A1/Twist | 23/125 | 18% | 117/119 | 98% | |
| ITIH5 | 7/135 | 6% | 19/138 | 14% | [25] |
| DKK3 | 2/135 | 2% | 41/138 | 30% | |
| RASSF1A | 25/135 | 26% | 64/138 | 47% | |
| ITIH5/DKK3/RASSF1A | 42/135 | 31% | 92/138 | 67% | |
| CDH1 | 0/25 | 0% | 24/50 | 48% | [57] |
| RASSF1A | 0/25 | 0% | 32/50 | 64% | |
| CDH1/RASSF1A | 0/25 | 0% | 38/50 | 76% | |
| SFN | 143/245 | 58% | 197/268 | 74% | [59] |
| P16 | 41/245 | 17% | 60/268 | 33% | |
| hMLH1 | 35/245 | 14% | 75/268 | 28% | |
| HOXD13 | 6/245 | 2% | 37/268 | 14% | |
| PCDHGB7 | 116/245 | 48% | 149/268 | 56% | |
| RASSF1A | 25/245 | 10% | 46/248 | 17% | |
| SFN/P16/hMLH1/HOXD13/PCDHGB7/RASSF1Ab | 68/245 | 28% | 213/268 | 80% | |
| ESR1 | 35/74 | 47% | 80/106 | 75% | [56] |
| 14-3-3-σ | 28/74 | 38% | 69/106 | 65% | |
| ESR1/14-3-3-σb | 33/74 | 45% | 86/106 | 81% | |
| GSTP1 | 2/87 | 2% | 4/101 | 4% | [62] |
| RARβ2 | 0/87 | 0% | 7/101 | 7% | |
| RASSF1A | 4/87 | 5% | 12/101 | 12% | |
| GSTP1/RARβ2/RASSF1A | 6/87 | 7% | 22/101 | 22% | |
| DAPK1 | 0/12 | 0% | 23/26 | 88% | [63] |
| RASSF1A | 1/12 | 8% | 18/26 | 69% | |
| DAPK1/RASSF1A | 1/12 | 8% | 25/26 | 96% | |
| APC | 1/19 | 5% | 23/79 | 30% | [61] |
| ESR1 | 2/19 | 11% | 16/79 | 20% | |
| RASSF1A | 0/19 | 0% | 28/79 | 35% | |
| APC/ESR1/RASSF1A | 3/19 | 16% | 42/79 | 53% | |
| APC | 2/39 | 5% | 12/44 | 27% | --- |
| FOXA1 | 7/39 | 18% | 30/44 | 68% | |
| RASSF1A | 0/39 | 0% | 6/44 | 14% | |
| APC/FOXA1/RASSF1A | 9/39 | 23% | 36/44 | 82% | |
| Panels | Sensitivity (%) | Specificity (%) | Specimen Type | Methods | References |
|---|---|---|---|---|---|
| HIC-1/RARβ2/RASSF1A | 90 | 100 | Plasma | MSP a | [60] |
| APC/GSTP1/RARβ2/RASSF1A | 62 | 87 | Plasma | QMSP b | [55] |
| ATM/RASSF1A | 36 | 100 | Plasma | QMSP b | [58] |
| RARβ2/RASSF1A/SCGB3A1/ Twist | 98.3 | 81.6 | Serum | Two-steps QMSP b | [54] |
| ITIH5/DKK3/RASSF1A | 67 | 72 | Serum | QMSP b | [25] |
| CDH1/RASSF1A | 76 | 90 | Serum | MSP a | [57] |
| SFN/P16/hMLH1/HOXD13/PCDHGB7/RASSF1A | 79.6 | 72.4 | Serum | QMSP b | [59] |
| ESR1/14-3-3-σ | 81 | 55 | Serum | QMSP b | [56] |
| GSTP1/RARβ2/RASSF1A | 22 | 93 | Serum | One-step MSP a | [62] |
| DAPK1/RASSF1A | 96 | 71 | Serum | MSP a | [63] |
| APC/ESR1/RASSF1A | 53 | 84 | Serum | QMSP b | [61] |
| APC/FOXA1/RASSF1A | 81.82 | 76.92 | Plasma | Multiplex QMSP b | --- |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salta, S.; P. Nunes, S.; Fontes-Sousa, M.; Lopes, P.; Freitas, M.; Caldas, M.; Antunes, L.; Castro, F.; Antunes, P.; Palma de Sousa, S.; et al. A DNA Methylation-Based Test for Breast Cancer Detection in Circulating Cell-Free DNA. J. Clin. Med. 2018, 7, 420. https://doi.org/10.3390/jcm7110420
Salta S, P. Nunes S, Fontes-Sousa M, Lopes P, Freitas M, Caldas M, Antunes L, Castro F, Antunes P, Palma de Sousa S, et al. A DNA Methylation-Based Test for Breast Cancer Detection in Circulating Cell-Free DNA. Journal of Clinical Medicine. 2018; 7(11):420. https://doi.org/10.3390/jcm7110420
Chicago/Turabian StyleSalta, Sofia, Sandra P. Nunes, Mário Fontes-Sousa, Paula Lopes, Micaela Freitas, Margarida Caldas, Luís Antunes, Fernando Castro, Pedro Antunes, Susana Palma de Sousa, and et al. 2018. "A DNA Methylation-Based Test for Breast Cancer Detection in Circulating Cell-Free DNA" Journal of Clinical Medicine 7, no. 11: 420. https://doi.org/10.3390/jcm7110420
APA StyleSalta, S., P. Nunes, S., Fontes-Sousa, M., Lopes, P., Freitas, M., Caldas, M., Antunes, L., Castro, F., Antunes, P., Palma de Sousa, S., Henrique, R., & Jerónimo, C. (2018). A DNA Methylation-Based Test for Breast Cancer Detection in Circulating Cell-Free DNA. Journal of Clinical Medicine, 7(11), 420. https://doi.org/10.3390/jcm7110420








