The Dark Side of Female HIV Patient Care: Sexual and Reproductive Health Risks in Pre- and Post-Clinical Treatments
Abstract
1. Introduction
1.1. The Benefits and Shortcomings of Clinical Treatment
1.2. Sexual and Reproductive Health-Related Rights and Care
2. Methods
2.1. Sample and Study Setting
2.2. Survey
2.3. In-Depth Interviews and Focus Group Discussion
3. Results
3.1. Desciptive Statistics
3.2. Pre- and Post-Clinial Issues
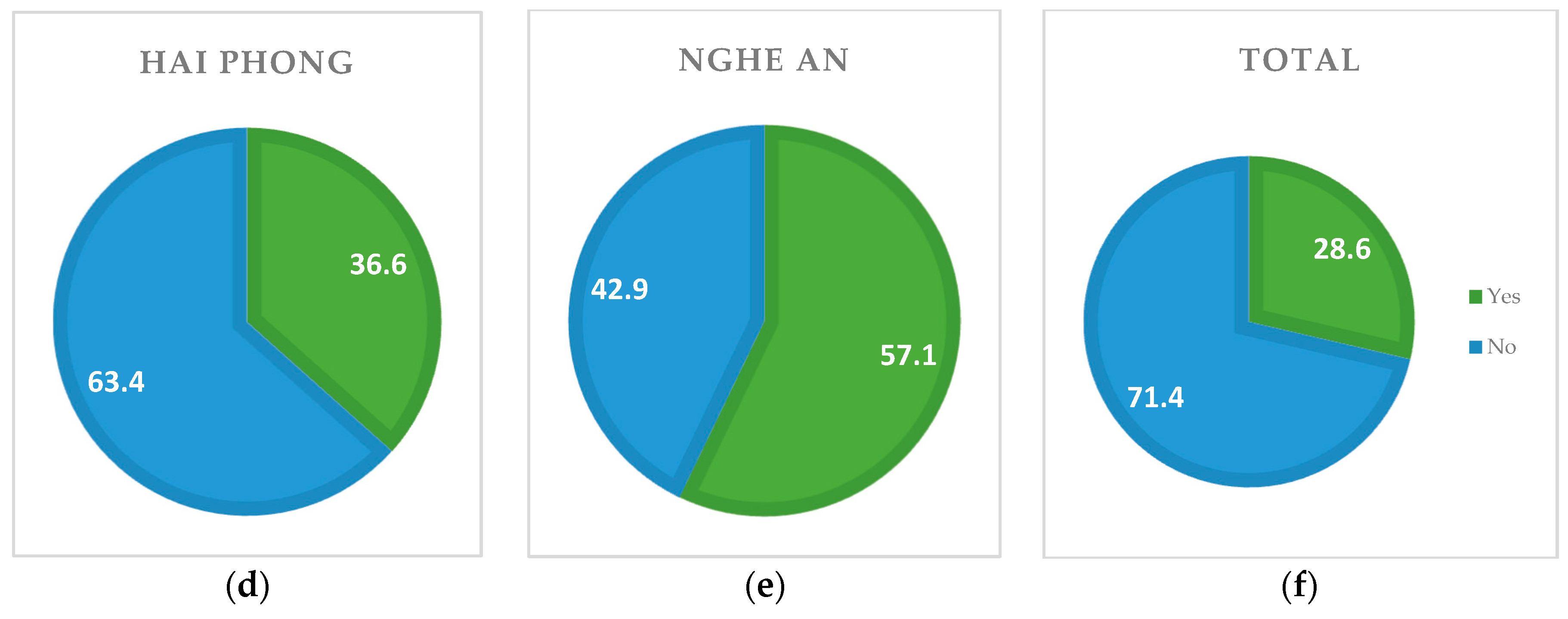
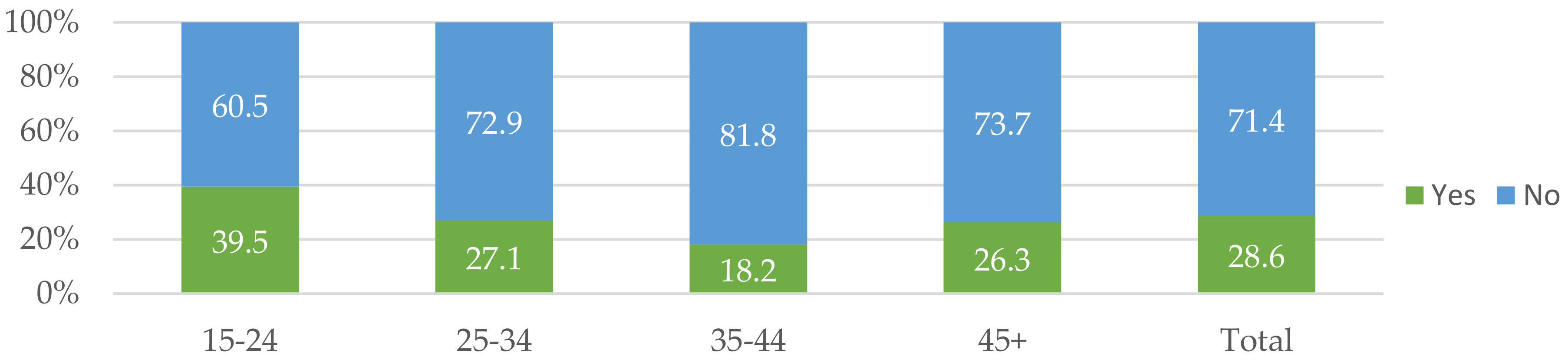
3.2.1. HIV Testing
3.2.2. Sexual and Reproductive Health-Related Issues
Abortion
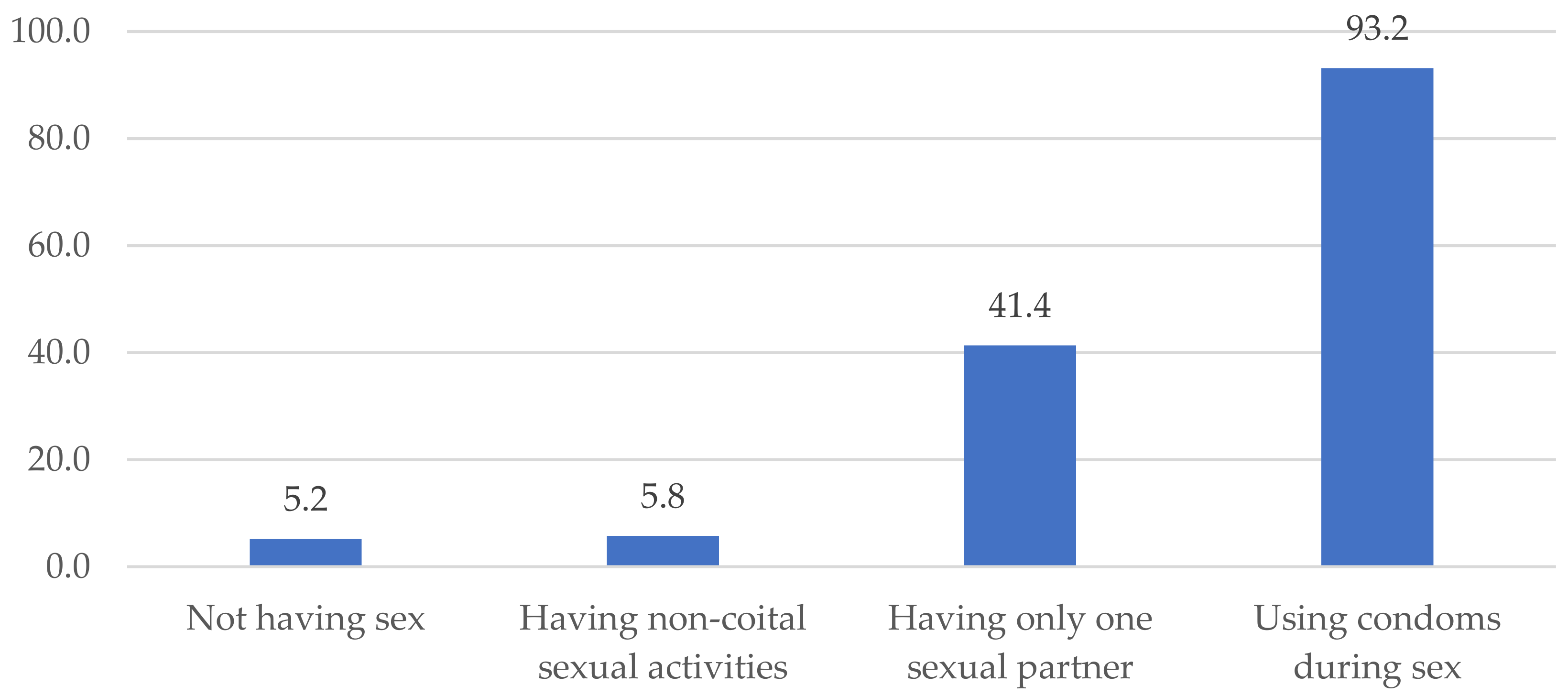
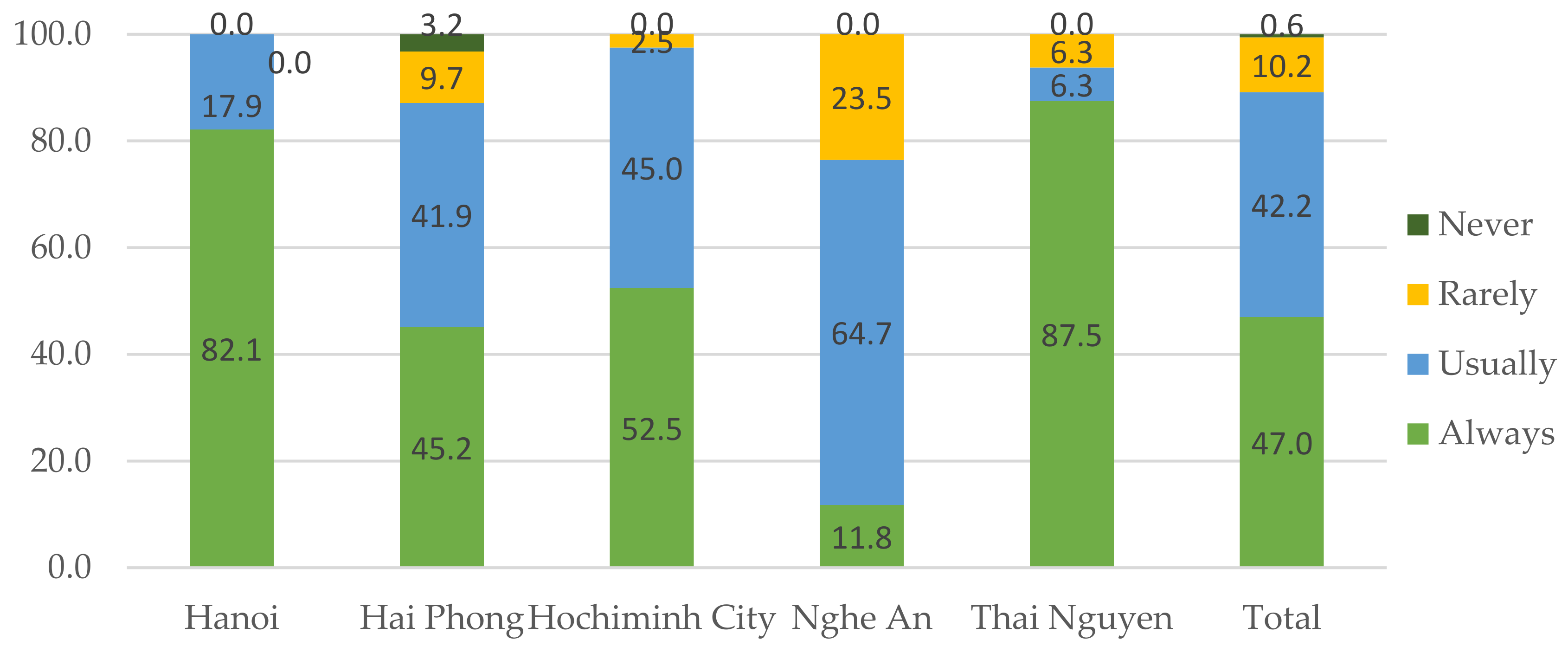
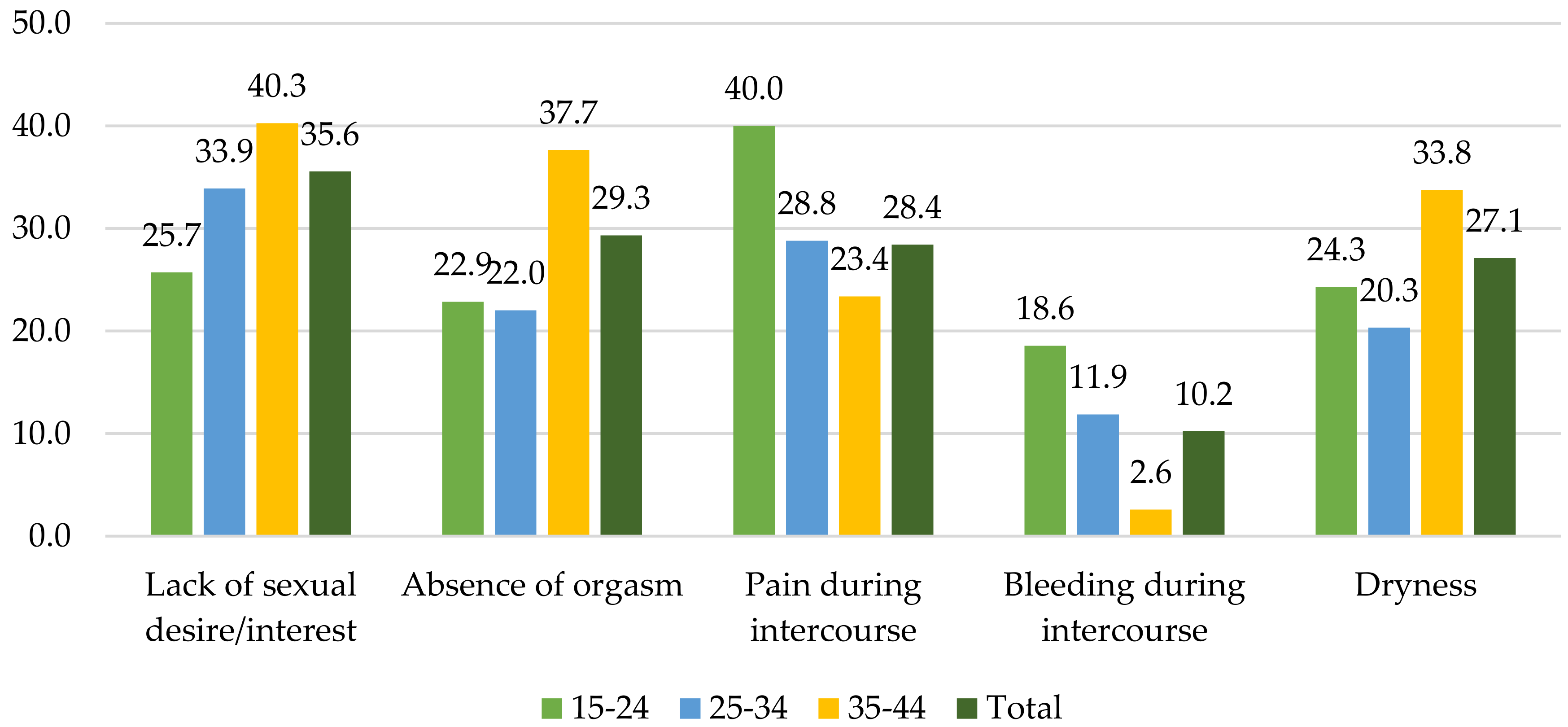
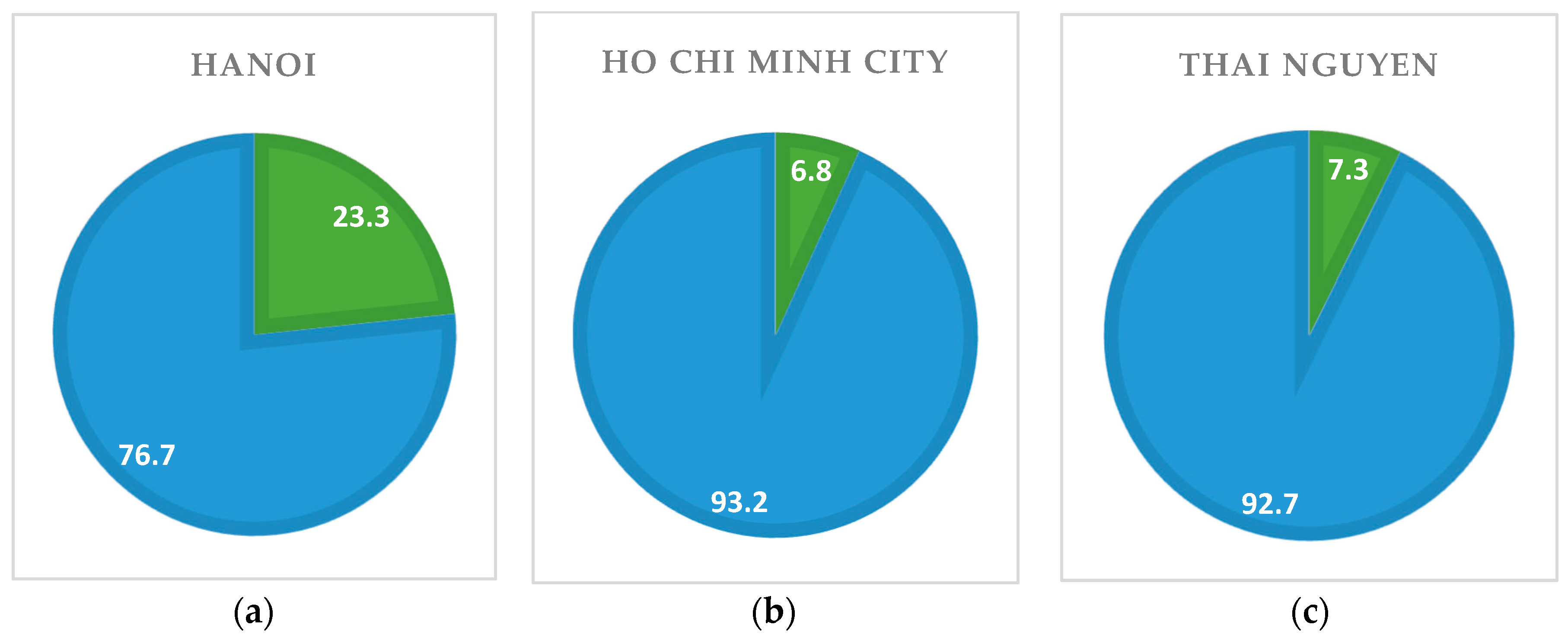
Sexual Health
Physical and Sexual Violence
3.3. Non-Clinical Issues
3.3.1. Services at Healthcare Settings
3.3.2. Health Insurance
4. Discussion
4.1. Limitations
4.2. Policy Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Granich, R.M.; Gilks, C.F.; Dye, C.; de Cock, K.M.; Williams, B.G. Universal voluntary hiv testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: A mathematical model. Lancet 2009, 373, 48–57. [Google Scholar] [CrossRef]
- Control, C.F. Achievements in public health. Reduction in perinatal transmission of HIV infection--united states, 1985–2005. Morb. Mortal. Wkly. Rep. 2006, 55, 592. [Google Scholar]
- Attia, S.; Egger, M.; Müller, M.; Zwahlen, M.; Low, N. Sexual transmission of HIV according to viral load and antiretroviral therapy: Systematic review and meta-analysis. Aids 2009, 23, 1397–1404. [Google Scholar] [CrossRef] [PubMed]
- Cohen, M.S.; Chen, Y.Q.; McCauley, M.; Gamble, T.; Hosseinipour, M.C.; Kumarasamy, N.; Hakim, J.G.; Kumwenda, J.; Grinsztejn, B.; Pilotto, J.H. Prevention of HIV-1 infection with early antiretroviral therapy. N. Engl. J. Med. 2011, 365, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Grinsztejn, B.; Hosseinipour, M.C.; Ribaudo, H.J.; Swindells, S.; Eron, J.; Chen, Y.Q.; Wang, L.; Ou, S.-S.; Anderson, M.; McCauley, M. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: Results from the phase 3 hptn 052 randomised controlled trial. Lancet Infect. Dis. 2014, 14, 281–290. [Google Scholar] [CrossRef]
- Kitahata, M.M.; Gange, S.J.; Abraham, A.G.; Merriman, B.; Saag, M.S.; Justice, A.C.; Hogg, R.S.; Deeks, S.G.; Eron, J.J.; Brooks, J.T. Effect of early versus deferred antiretroviral therapy for HIV on survival. N. Engl. J. Med. 2009, 360, 1815–1826. [Google Scholar] [CrossRef] [PubMed]
- Farmer, P.; Léandre, F.; Mukherjee, J.S.; Claude, M.S.; Nevil, P.; Smith-Fawzi, M.C.; Koenig, S.P.; Castro, A.; Becerra, M.C.; Sachs, J.; et al. Community-based approaches to HIV treatment in resource-poor settings. Lancet 2001, 358, 404–409. [Google Scholar] [CrossRef]
- Hegdahl, H.K.; Fylkesnes, K.M.; Sandøy, I.F. Sex differences in hiv prevalence persist over time: Evidence from 18 countries in sub-Saharan Africa. PLoS ONE 2016, 11, e0148502. [Google Scholar] [CrossRef] [PubMed]
- UN Women. Facts and Figures: HIV and AIDS. Available online: http://www.unwomen.org/en/what-we-do/hiv-and-aids/facts-and-figures (accessed on 5 September 2018).
- UNICEF. Girls, Hiv/Aids and Education. Available online: https://www.unicef.org/lifeskills/index_8657.html (accessed on 7 September 2018).
- Farmer, P.; Connors, M.; Simmons, J. Women, Poverty, and Aids: Sex, Drugs, and Structural Violence; Common Courage Press: Monroe, ME, USA, 1996. [Google Scholar]
- Glasier, A.; Gülmezoglu, A.M.; Schmid, G.P.; Moreno, C.G.; Van Look, P.F. Sexual and reproductive health: A matter of life and death. Lancet 2006, 368, 1595–1607. [Google Scholar] [CrossRef]
- Askew, I.; Berer, M. The contribution of sexual and reproductive health services to the fight against HIV/AIDS: A review. Reprod. Health Matters 2003, 11, 51–73. [Google Scholar] [CrossRef]
- Gruskin, S.; Ferguson, L.; O’Malley, J. Ensuring sexual and reproductive health for people living with hiv: An overview of key human rights, policy and health systems issues. Reprod. Health Matters 2007, 15, 4–26. [Google Scholar] [CrossRef]
- Pallas, C.L.; Nguyen, L. Donor withdrawal and local civil society organizations: An analysis of the hiv/aids sector in Vietnam. Dev. Policy Rev. 2018, 36, 131–151. [Google Scholar] [CrossRef]
- Ministry of Planning and Investment. Country Report: 15 Years Achieving the Viet Nam Millennium Development Goals; Ministry of Planning and Investment: Hanoi, Vietnam, 2015. [Google Scholar]
- UNAIDS. Fact Sheet-July 2018. Available online: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf (accessed on 5 September 2018).
- Inter-Parliamentary Union. Hiv and Aids in Viet Nam—Facing the Challenges. Available online: http://archive.ipu.org/pdf/publications/hiv-vietnam-en.pdf (accessed on 5 September 2018).
- Plana, M.; García, F.; Gallart, T.; Tortajada, C.; Soriano, A.; Palou, E.; Maleno, M.J.; Barceló, J.J.; Vidal, C.; Cruceta, A. Immunological benefits of antiretroviral therapy in very early stages of asymptomatic chronic HIV-1 infection. Aids 2000, 14, 1921–1933. [Google Scholar] [CrossRef] [PubMed]
- Chiappini, E.; Galli, L.; Tovo, P.-A.; Gabiano, C.; Gattinara, G.C.; Guarino, A.; Baddato, R.; Giaquinto, C.; Lisi, C.; de Martino, M. Virologic, immunologic, and clinical benefits from early combined antiretroviral therapy in infants with perinatal HIV-1 infection. Aids 2006, 20, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Johansson, K.A.; Robberstad, B.; Norheim, O.F. Further benefits by early start of hiv treatment in low income countries: Survival estimates of early versus deferred antiretroviral therapy. AIDS Res. Ther. 2010, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Bijker, R.; Jiamsakul, A.; Siwale, M.; Kiertiburanakul, S.; Kityo, C.; Phanuphak, P.; de Wit, T.F.R.; Ng, O.T.; Hamers, R.L.; Collaboration, P.-T.C. Determinants of adherence to antiretroviral therapy di er between Africa and Asia. AGE 2015, 18, 1. [Google Scholar]
- Bijker, R.; Jiamsakul, A.; Kityo, C.; Kiertiburanakul, S.; Siwale, M.; Phanuphak, P.; Akanmu, S.; Chaiwarith, R.; Wit, F.W.; Sim, B.L. Adherence to antiretroviral therapy for HIV in sub-Saharan Africa and Asia: A comparative analysis of two regional cohorts. J. Int. AIDS Soc. 2017, 20, 21218. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Gerver, S.M.; Fidler, S.; Ward, H. Adherence to antiretroviral therapy in adolescents living with HIV: Systematic review and meta-analysis. AIDS (Lond. Engl.) 2014, 28, 1945. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.; Halperin, D.T. “Know your epidemic, know your response”: A useful approach, if we get it right. Lancet 2008, 372, 423–426. [Google Scholar] [CrossRef]
- Tanser, F.; de Oliveira, T.; Maheu-Giroux, M.; Bärnighausen, T. Concentrated HIV sub-epidemics in generalized epidemic settings. Curr. Opin. HIV AIDS 2014, 9, 115. [Google Scholar] [CrossRef] [PubMed]
- Kisesa, A.; Chamla, D. Getting to 90–90–90 targets for children and adolescents HIV in low and concentrated epidemics: Bottlenecks, opportunities, and solutions. Curr. Opin. HIV AIDS 2016, 11, S1. [Google Scholar] [CrossRef] [PubMed]
- Kumarasamy, N.; Safren, S.A.; Raminani, S.R.; Pickard, R.; James, R.; Krishnan, A.S.; Solomon, S.; Mayer, K.H. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: A qualitative study. AIDS Patient Care STDs 2005, 19, 526–537. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, D.; Carrieri, M.P.; Shepard, D. Treatment and care for injecting drug users with HIV infection: A review of barriers and ways forward. Lancet 2010, 376, 355–366. [Google Scholar] [CrossRef]
- Posse, M.; Meheus, F.; Van Asten, H.; Van Der Ven, A.; Baltussen, R. Barriers to access to antiretroviral treatment in developing countries: A review. Trop. Med. Int. Health 2008, 13, 904–913. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.A.; Oosterhoff, P.; Ngoc, Y.P.; Wright, P.; Hardon, A. Barriers to access prevention of mother-to-child transmission for HIV positive women in a well-resourced setting in Vietnam. AIDS Res. Ther. 2008, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Nhan Dan. Tăng tỷ lệ Người Nhiễm HIV Điều Trị Bằng Thuốc Kháng Vi-Rút [Raising the Rate of HIV-Infected People Receiving Arv]. Available online: http://nhandan.com.vn/suckhoe/item/36307802-tang-ty-le-nguoi-nhiem-hiv-dieu-tri-bang-thuoc-khang-vi-rut.html (accessed on 7 September 2018).
- Tieng Chuong. 73% Cơ Sở Sẵn Sàng Thanh Toán Các Chi Phí Điều Trị Hiv/Aids Thông Qua Bhyt [73% of Medical Establishments Ready to Pay for Hiv/Aids Treatment via Health Insurance]. Available online: http://tiengchuong.vn/Trao-doi-gop-y/73-co-so-san-sang-thanh-toan-cac-chi-phi-dieu-tri-HIVAIDS-thong-qua-BHYT/25982.vgp (accessed on 7 September 2018).
- Van Tam, V.; Pharris, A.; Thorson, A.; Alfven, T.; Larsson, M. “It is not that i forget, it’s just that i don’t want other people to know”: Barriers to and strategies for adherence to antiretroviral therapy among HIV patients in northern Vietnam. AIDS Care 2011, 23, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Maher, L.; Coupland, H.; Musson, R. Scaling up HIV treatment, care and support for injecting drug users in Vietnam. Int. J. Drug Policy 2007, 18, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Van Tam, V.; Larsson, M.; Pharris, A.; Diedrichs, B.; Nguyen, H.P.; Nguyen, C.T.K.; Ho, P.D.; Marrone, G.; Thorson, A. Peer support and improved quality of life among persons living with HIV on antiretroviral treatment: A randomised controlled trial from north-eastern Vietnam. Health Qual. Life Outcomes 2012, 10, 53. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X. Quality of life outcomes of antiretroviral treatment for HIV/AIDS patients in Vietnam. PLoS ONE 2012, 7, e41062. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Granich, R.; Bui, D.D.; Tran, H.V.; Nadol, P.; Jacka, D.; Sabin, K.; Suthar, A.B.; Mesquita, F.; Lo, Y.R. The potential impact of expanding antiretroviral therapy and combination prevention in Vietnam: Towards elimination of HIV transmission. J. Acquir. Immune Defic. Syndr. 2013, 63, e142. [Google Scholar] [CrossRef] [PubMed]
- Ruxrungtham, K.; Brown, T.; Phanuphak, P. HIV/AIDS in Asia. Lancet 2004, 364, 69–82. [Google Scholar] [CrossRef]
- Goldsamt, L.A.; Clatts, M.C.; Giang, L.M.; Le, B.Q.; Colby, D.J.; Yu, G. Hiv and other stis in male sex workers: Findings from a sexual health promotion intervention in Vietnam. Int. J. STD AIDS 2018, 29, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Nadol, P.; Hoang, T.V.; Le, L.-V.; Nguyen, T.A.; Kaldor, J.; Law, M. High HIV prevalence and risk among male clients of female sex workers in Hanoi and Ho Chi Minh City, Vietnam. AIDS Behav. 2017, 21, 2381–2393. [Google Scholar] [CrossRef] [PubMed]
- Duong, H.T.; Des Jarlais, D.; Khuat, O.H.T.; Arasteh, K.; Feelemyer, J.; Khue, P.M.; Giang, H.T.; Laureillard, D.; Hai, V.V.; Vallo, R.J.A.; et al. Risk behaviors for HIV and HCV infection among people who inject drugs in Hai Phong, Viet Nam, 2014. AIDS Behav. 2018, 22, 2161–2171. [Google Scholar] [CrossRef] [PubMed]
- WHO. The Risks of Unsafe Sex and Aids: The World Health Organization’s Response. Available online: http://www.who.int/whr/media_centre/factsheet1/en/ (accessed on 7 September 2018).
- Olley, B.O.; Gxamza, F.; Seedat, S.; Theron, H.; Taljaard, J.; Reid, E.; Reuter, H.; Stein, D.J. Psychopathology and coping in recently diagnosed HIV/AIDS patients-the role of gender. S. Afr. Med. J. 2003, 93, 928–931. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.; Moodley, J.; Zweigenthal, V.; Bekker, L.-G.; Shah, I.; Myer, L. Fertility intentions and reproductive health care needs of people living with HIV in cape town, south africa: Implications for integrating reproductive health and HIV care services. AIDS Behav. 2009, 13, 38. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.; Harries, J.; Myer, L.; Orner, P.; Bracken, H. “Life is still going on”: Reproductive intentions among HIV-positive women and men in South Africa. Soc. Sci. Med. 2007, 65, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Watt, M.H.; Dennis, A.C.; Choi, K.W.; Ciya, N.; Joska, J.A.; Robertson, C.; Sikkema, K.J. Impact of sexual trauma on HIV care engagement: Perspectives of female patients with trauma histories in Cape Town, South Africa. AIDS Behav. 2017, 21, 3209–3218. [Google Scholar] [CrossRef] [PubMed]
- Speizer, I.S.; Magnani, R.J.; Colvin, C.E. The effectiveness of adolescent reproductive health interventions in developing countries: A review of the evidence. J. Adolesc. Health 2003, 33, 324–348. [Google Scholar] [CrossRef]
- Bao, A.; Colby, D.J.; Trang, T.; Le, B.Q.; Dinh, T.D.; Nguyen, Q.H.; Hoang, H.T.; Friedman, M.R.; Stall, R. Correlates of HIV testing among transgender women in Ho Chi Minh, Vietnam. AIDS Behav. 2016, 20, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Nguyen, L.H.; Nguyen, C.T.; Phan, H.T.T.; Latkin, C.A. Alcohol abuse increases the risk of HIV infection and diminishes health status of clients attending HIV testing services in Vietnam. Harm Reduct. J. 2016, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.T.; Nguyen, H.T.; Nguyen, Q.C.; Duong, P.T.B.; West, G. Expenditure analysis of HIV testing and counseling services using the cascade framework in Vietnam. PLoS ONE 2015, 10, e0126659. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Tran, B.X.; Nguyen, N.P.; Phan, H.T.T.; Bui, T.T.; Latkin, C.A. Mobilization for HIV voluntary counseling and testing services in Vietnam: Clients’ risk behaviors, attitudes and willingness to pay. AIDS Behav. 2016, 20, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Goldsamt, L.; Clatts, M.; Giang, L.; Le, B.; Colby, D. Sexual health promotion intervention for male sex workers in Vietnam in-creases knowledge of STI/HIV transmission risk. J. AIDS Clin. Res. 2017, 4. [Google Scholar] [CrossRef]
- Nguyen, M.X.; Krishnan, A.; Le, G.M.; Nguyen, Q.T.; Bhadra, N.M.; Nguyen, S.M.; Miller, W.C.; Go, V.F. The use of technology to find sexual health information online among men who have sex with men in Hanoi, Vietnam, 2016. Int. J. STD AIDS 2018, 29, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Vu, N.T.T.; Holt, M.; Phan, H.T.T.; La, L.T.; Tran, G.M.; Doan, T.T.; Nguyen, T.N.N.; de Wit, J. The relationship between methamphetamine use, sexual sensation seeking and condomless anal intercourse among men who have sex with men in Vietnam: Results of a community-based, cross-sectional study. AIDS Behav. 2017, 21, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- Patterson, S.; Cescon, A.; Samji, H.; Chan, K.; Zhang, W.; Raboud, J.; Burchell, A.N.; Cooper, C.; Klein, M.B.; Rourke, S.B. Life expectancy of HIV-positive individuals on combination antiretroviral therapy in Canada. BMC Infect. Dis. 2015, 15, 274. [Google Scholar] [CrossRef] [PubMed]
- Kaida, A.; Carter, A. High mortality among women living with HIV enrolled in Canada’s largest community-based cohort study. Trans Gend. Identity 2018, 63, 4. [Google Scholar]
- VTV. Hà nội: Gần 20.000 Người Nhiễm HIV/AIDS. Available online: https://vtv.vn/suc-khoe/ha-noi-gan-20000-nguoi-nhiem-hiv-aids-20180623214344631.htm (accessed on 26 September 2018).
- Hai Phong Newspaper. Hải Phòng có hơn 9 Nghìn Người Nghiện Ma Túy [haiphong Has over 9000 Heroin Addicts]. Available online: http://baohaiphong.com.vn/baohp/vn/home/InfoDetail.jsp?ID=12459&cat=24 (accessed on 26 September 2018).
- Zing News. 42% người nhiễm hiv ở sài gòn không rõ nguyên nhân [42% of HIV infected patients in saigon don’t know the cause]. Available online: https://news.zing.vn/42-nguoi-nhiem-hiv-o-sai-gon-khong-ro-nguyen-nhan-post846555.html (accessed on 26 September 2018).
- Thai Nguyen Newspaper. Khó Khăn Trong Phòng, Chống Hiv ở Tuyến cơ sở [Difficulties in Fighting, Preventing HIV at the Grassroots Level]. Available online: http://m.baothainguyen.vn/tin-tuc/suc-khoe-cong-dong/kho-khan-trong-phong-chong-hivaids-o-tuyen-co-so-253471-46249.html (accessed on 26 September 2018).
- VnExpress. Nghệ an có Hơn 9.000 Người Nhiễm HIV [Nghe an Has over 9000 HIV-Infected People]. Available online: https://suckhoe.vnexpress.net/tin-tuc/suc-khoe/nghe-an-co-hon-9-000-nguoi-nhiem-hiv-3720875.html (accessed on 27 September 2018).
- Fielding, N.G. Triangulation and mixed methods designs: Data integration with new research technologies. J. Mixed Methods Res. 2012, 6, 124–136. [Google Scholar] [CrossRef]
- Vuong, Q.-H.; La, V.-P.; Vuong, T.-T.; Ho, M.-T.; Nguyen, H.-K.T.; Nguyen, V.-H.; Pham, H.-H.; Ho, M.-T. An open database of productivity in Vietnam’s social sciences and humanities for public use. Sci. Data 2018, 5, 180188. [Google Scholar] [CrossRef] [PubMed]
- Gill, P.; Stewart, K.; Treasure, E.; Chadwick, B. Methods of data collection in qualitative research: Interviews and focus groups. Br. Dent. J. 2008, 204, 291. [Google Scholar] [CrossRef] [PubMed]
- Downward, P.; Mearman, A. Retroduction as mixed-methods triangulation in economic research: Reorienting economics into social science. Camb. J. Econ. 2006, 31, 77–99. [Google Scholar] [CrossRef]
- Heckathorn, D.D. Comment: Snowball versus respondent-driven sampling. Sociol. Methodol. 2011, 41, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Magnani, R.; Sabin, K.; Saidel, T.; Heckathorn, D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. Aids 2005, 19, S67–S72. [Google Scholar] [CrossRef] [PubMed]
- Bernhed, J.; Mollstedt, M.; Rosengren, K. Dare to care: A qualitative content analysis regarding nursing students’ view on HIV in Vietnam. Home Health Care Manag. Pract. 2018, 30, 187–194. [Google Scholar] [CrossRef]
- Stringer, K.L.; Turan, B.; McCormick, L.; Durojaiye, M.; Nyblade, L.; Kempf, M.-C.; Lichtenstein, B.; Turan, J.M. HIV-related stigma among healthcare providers in the deep south. AIDS Behav. 2016, 20, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Katz, I.T.; Ryu, A.E.; Onuegbu, A.G.; Psaros, C.; Weiser, S.D.; Bangsberg, D.R.; Tsai, A.C. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J. Int. AIDS Soc. 2013, 16, 18640. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, W.R.; Weiser, S.; Bangsberg, D.; Thior, I.; Makhema, J.; Dickinson, D.; Mompati, K.; Marlink, R. Effects of HIV-related stigma among an early sample of patients receiving antiretroviral therapy in Botswana. AIDS Care 2006, 18, 931–933. [Google Scholar] [CrossRef] [PubMed]
- Oanh, K.T.H.; Ashburn, K.; Pulerwitz, J.; Ogden, J.; Nyblade, L. Improving Hospital-Based Quality of Care in Vietnam by Reducing HIV-Related Stigma and Discrimination; Horizons Final Report; Population Council: Washington, DC, USA, 2008. [Google Scholar]
- Pulerwitz, J.; Oanh, K.T.H.; Akinwolemiwa, D.; Ashburn, K.; Nyblade, L. Improving hospital-based quality of care by reducing HIV-related stigma: Evaluation results from Vietnam. AIDS Behav. 2015, 19, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Vuong, Q.-H.; Ho, T.-M.; Nguyen, H.-K.; Vuong, T.-T. Healthcare consumers’ sensitivity to costs: A reflection on behavioural economics from an emerging market. Palgrave Commun. 2018, 4, 70. [Google Scholar] [CrossRef]
- Vuong, Q.-H. Sociodemographic factors influencing Vietnamese patient satisfaction with healthcare services and some meaningful empirical thresholds. Iran. J. Public Health 2018, 47, 119. [Google Scholar] [PubMed]
- Vuong, Q.-H.; Vuong, T.-T.; Ho, T.M.; Nguyen, H.V. Psychological and socio-economic factors affecting social sustainability through impacts on perceived health care quality and public health: The case of Vietnam. Sustainability 2017, 9, 1456. [Google Scholar] [CrossRef]
- General Statistics Office Vietnam; National Institute of Hygiene and Epidemiology Vietnam. Vietnam Population Aids Indicator Survey (Vpais): 2005; ORC Macro: Calverton, MD, USA, 2006. [Google Scholar]
- Pharris, A.; Chuc, N.T.K.; Tishelman, C.; Brugha, R.; Hoa, N.P.; Thorson, A. Expanding hiv testing efforts in concentrated epidemic settings: A population-based survey from rural Vietnam. PLoS ONE 2011, 1, e16017. [Google Scholar] [CrossRef] [PubMed]
- Long, T. HIV/AIDS Tại Việt Nam Ước Tính Và Dự Báo: Giai đoạn 2011-2015 [HIV/AIDS in Vietnam, Estimation and Forecast: 2011–2015]. Available online: https://www.fhi360.org/sites/default/files/media/documents/FHI-Layout Uoc tinh va Du bao 2011-2015_FINAL.pdf (accessed on 22 July 2018).
- Morales, J.A. The ‘Middle-Income Effect’ on HIV/Aids Programs in Vietnam; Devex: Washington, DC, USA, 2013. [Google Scholar]
- Kates, J.; Wexler, A.; Lief, E. Financing the Response to HIV in Low and Middle-Income Countries; Kaiser Family Foundation: Menlo Park, CA, USA, 2014. [Google Scholar]
- Manning, R.; Sterck, O. Rethinking international and domestic financing for HIV in low-and middle-income countries. Dev. Policy Rev. 2018, 36, 433–444. [Google Scholar] [CrossRef]

| Geographical Location | Total Population | Number of PLWH (End-2017) | Percentage of Vietnam’s PLWH Population | |
|---|---|---|---|---|
| Hanoi | Northern | 7.65 million | 19,904 | 9.5% |
| Thai Nguyen | Northern | 1.15 million | 6252 | 3.0% |
| Hai Phong | Northeastern | 1.96 million | 7635 | 3.6% |
| Nghe An | North-central | 3.11 million | 5647 | 2.7% |
| Ho Chi Minh City | Southern | 8.43 million | 46,853 | 22.4% |
| Number of Respondents | Percentage | |
|---|---|---|
| Location | ||
| Hanoi | 30 | 12.4% |
| Hai Phong | 41 | 17.0% |
| Ho Chi Minh City | 59 | 24.5% |
| Nghe An | 70 | 29.0% |
| Thai Nguyen | 41 | 17.0% |
| Age group | ||
| 15–24 | 86 | 35.7% |
| 25–34 | 59 | 24.5% |
| 35–44 | 77 | 32.0% |
| 45 and above | 19 | 7.9% |
| Marital status | ||
| Married | 55 | 22.8% |
| Widowed | 21 | 8.7% |
| Divorced | 40 | 16.6% |
| Separate | 7 | 2.9% |
| Cohabiting | 13 | 5.4% |
| Never married | 105 | 43.6% |
| Highest educational level | ||
| Primary school | 45 | 18.7% |
| Lower secondary school | 101 | 41.9% |
| Upper secondary school | 93 | 38.6% |
| Vocational training-college-university | 2 | 0.8% |
| Total | 241 |
| Hanoi | Hai Phong | Nghe An | Thai Nguyen | Ho Chi Minh City | Total | |
|---|---|---|---|---|---|---|
| In-depth interview | 48 | |||||
| FSW | 1 | 1 | 1 | 1 | 1 | 5 |
| WLHIV | 1 | 1 | 1 | 1 | 1 | 5 |
| PSP of PLHIV/IDU | 2 | 2 | 2 | 2 | 2 | 10 |
| IDU woman | 1 | 1 | 1 | 1 | 1 | 5 |
| Woman 3 in 1 * | 1 | 1 | 1 | 1 | 1 | 5 |
| Adolescent girl | 3 | 1 | 2 | 1 | 1 | 8 |
| Health care worker | 2 | 2 | 2 | 2 | 2 | 10 |
| Focus group discussion | 4 | |||||
| Adolescent girl | ||||||
| FSW | 1 | 1 | ||||
| FSW and IDU woman | 1 | 1 | ||||
| PSP of PLHIV/IDU | 1 | 1 | ||||
| WLHIV | 1 | 1 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khuat, T.H.; Do, T.T.; Nguyen, V.A.T.; Vu, X.T.; Nguyen, P.T.T.; Tran, K.; Ho, M.T.; T. Nguyen, H.K.; Vuong, T.T.; La, V.P.; et al. The Dark Side of Female HIV Patient Care: Sexual and Reproductive Health Risks in Pre- and Post-Clinical Treatments. J. Clin. Med. 2018, 7, 402. https://doi.org/10.3390/jcm7110402
Khuat TH, Do TT, Nguyen VAT, Vu XT, Nguyen PTT, Tran K, Ho MT, T. Nguyen HK, Vuong TT, La VP, et al. The Dark Side of Female HIV Patient Care: Sexual and Reproductive Health Risks in Pre- and Post-Clinical Treatments. Journal of Clinical Medicine. 2018; 7(11):402. https://doi.org/10.3390/jcm7110402
Chicago/Turabian StyleKhuat, Thu Hong, Thu Trang Do, Van Anh T. Nguyen, Xuan Thai Vu, Phuong Thao T. Nguyen, Kien Tran, Manh Tung Ho, Hong Kong T. Nguyen, Thu Trang Vuong, Viet Phuong La, and et al. 2018. "The Dark Side of Female HIV Patient Care: Sexual and Reproductive Health Risks in Pre- and Post-Clinical Treatments" Journal of Clinical Medicine 7, no. 11: 402. https://doi.org/10.3390/jcm7110402
APA StyleKhuat, T. H., Do, T. T., Nguyen, V. A. T., Vu, X. T., Nguyen, P. T. T., Tran, K., Ho, M. T., T. Nguyen, H. K., Vuong, T. T., La, V. P., & Vuong, Q. H. (2018). The Dark Side of Female HIV Patient Care: Sexual and Reproductive Health Risks in Pre- and Post-Clinical Treatments. Journal of Clinical Medicine, 7(11), 402. https://doi.org/10.3390/jcm7110402







