The CHA2DS2-VASc Score Predicts Major Bleeding in Non-Valvular Atrial Fibrillation Patients Who Take Oral Anticoagulants
Abstract
:1. Introduction
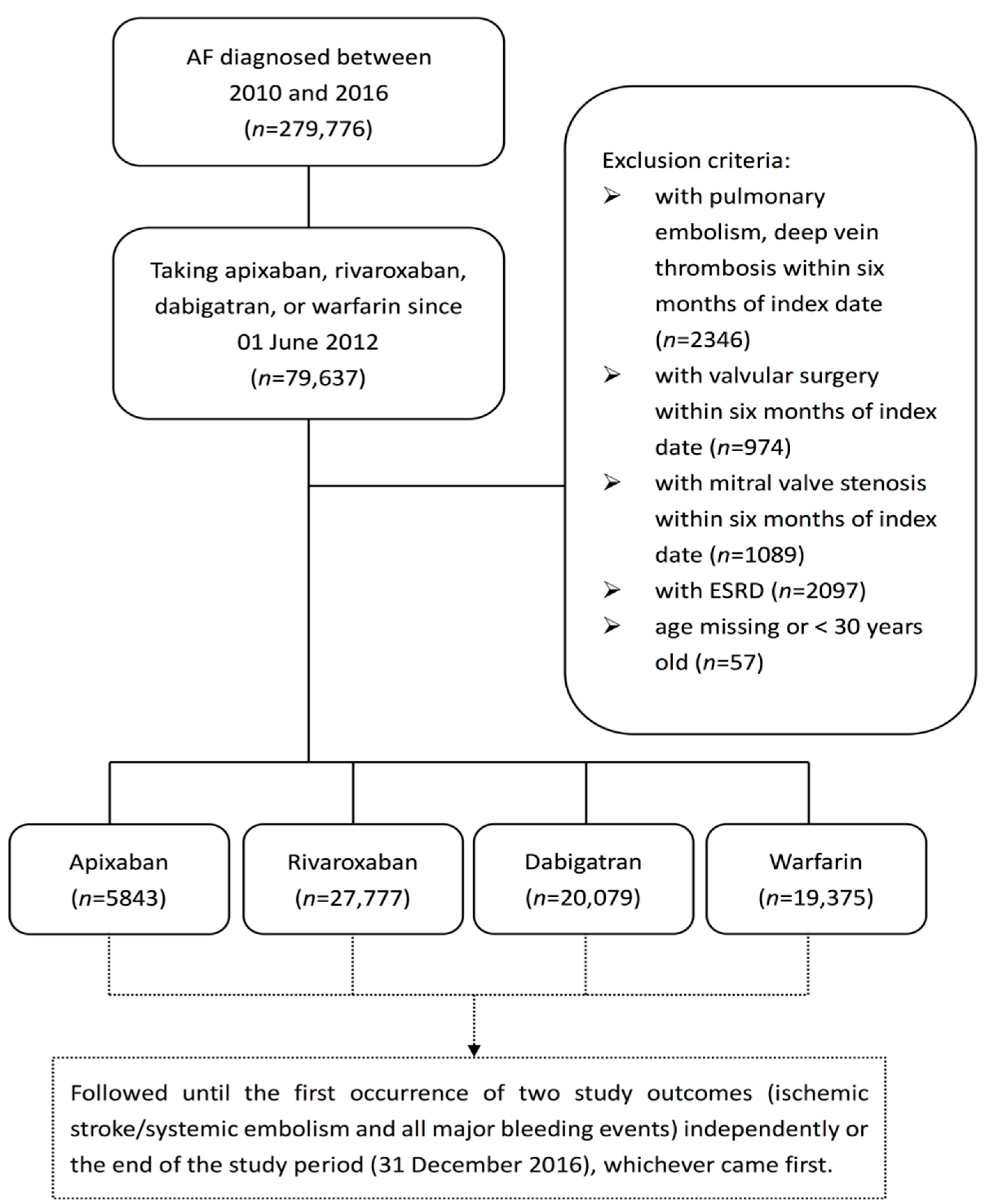
2. Materials and Methods
2.1. Patients
2.2. Outcomes
2.3. Statistical Methods
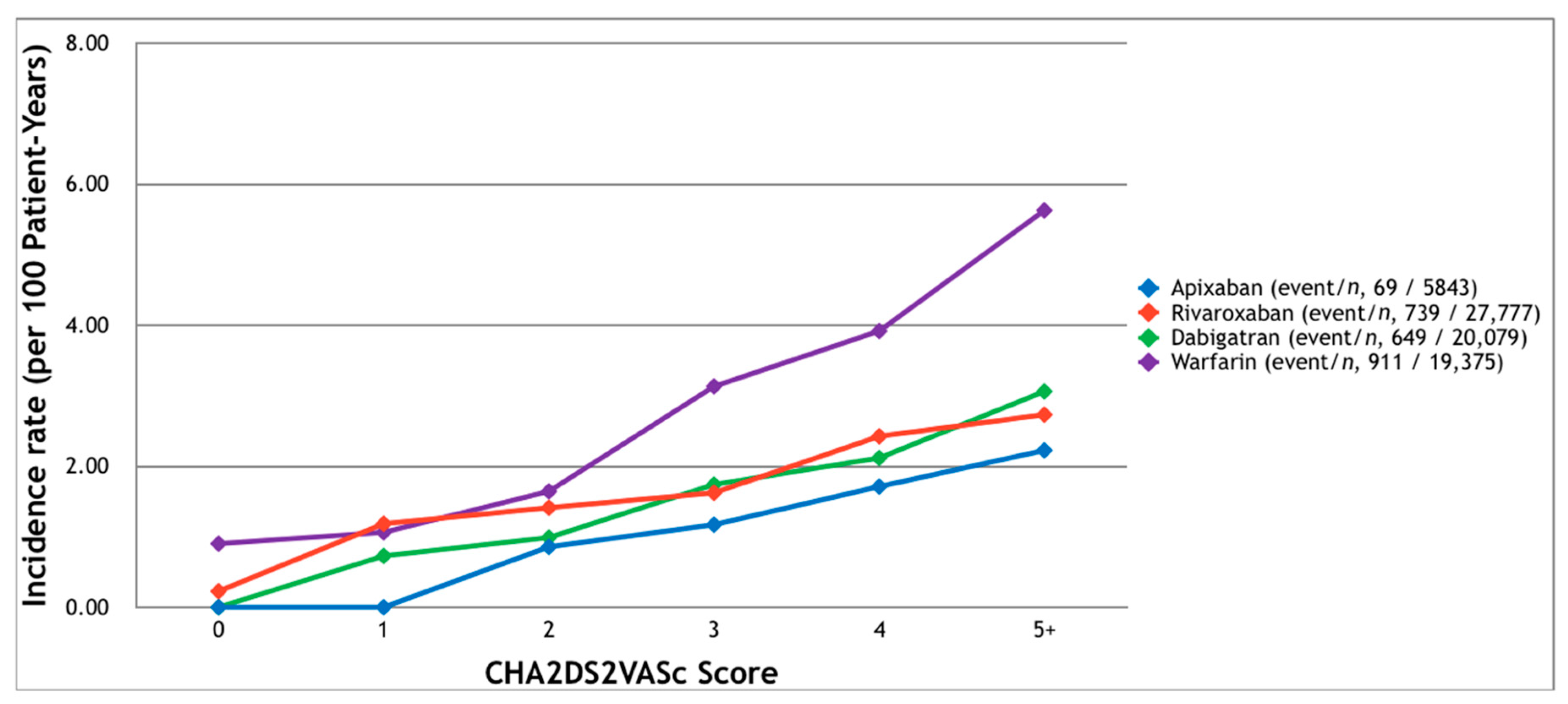
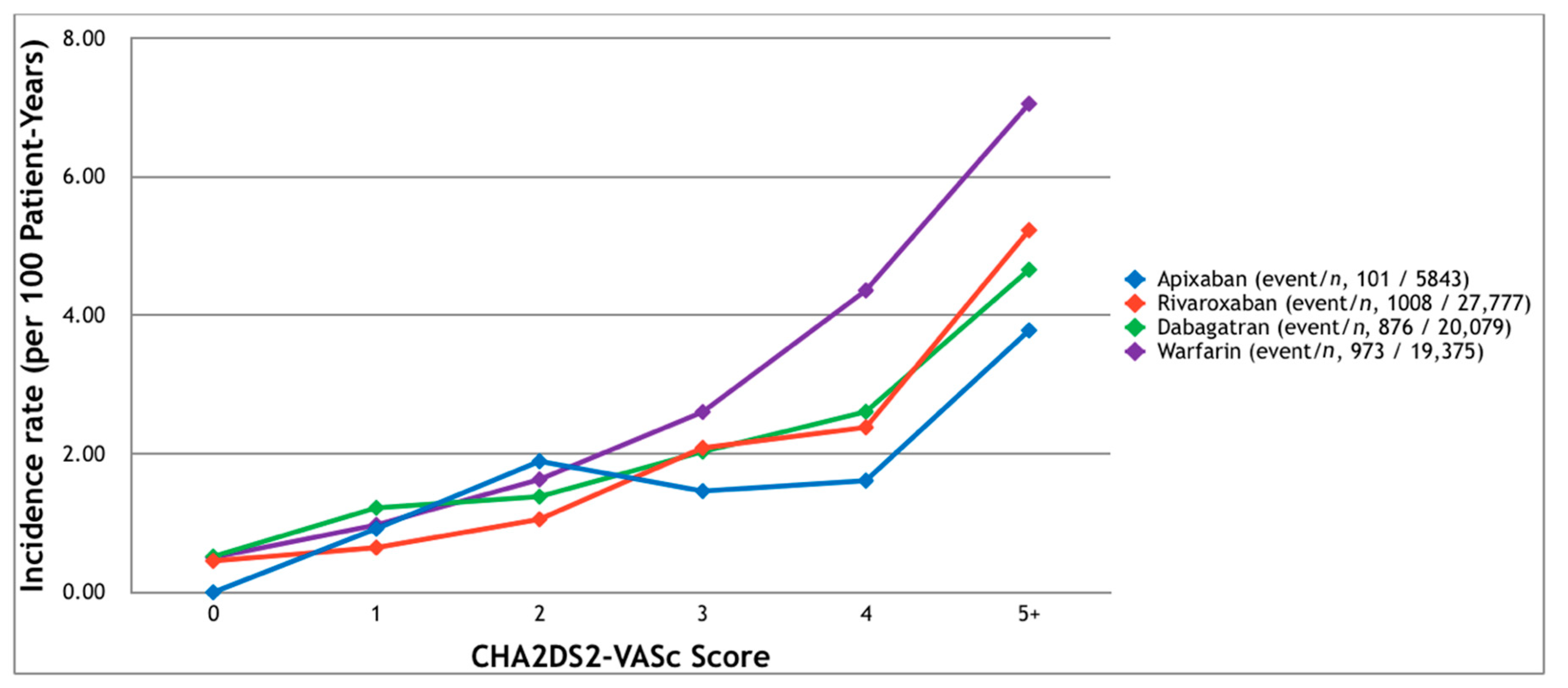
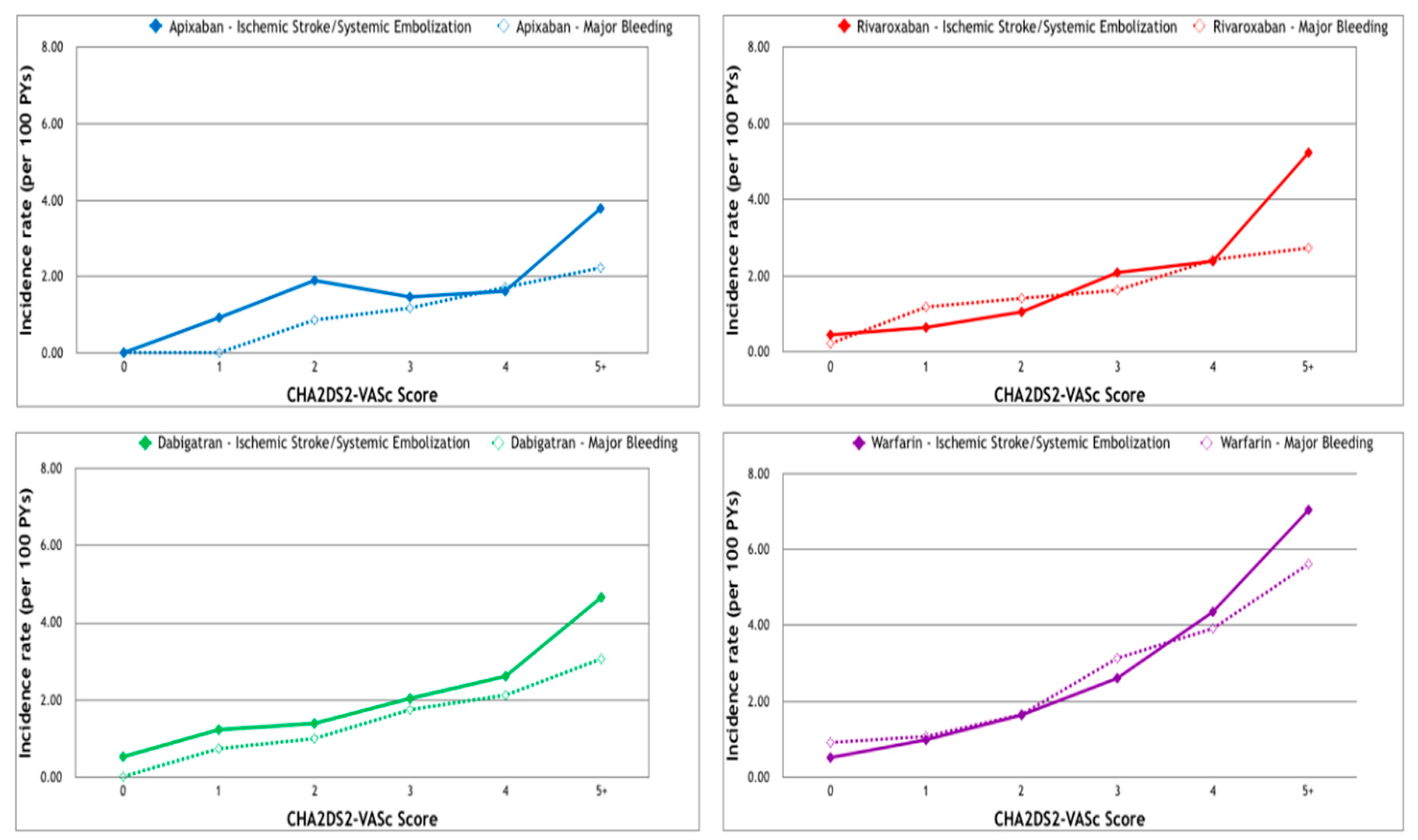
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hart, R.G.; Pearce, L.A.; Aguilar, M.I. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann. Intern. Med. 2007, 146, 857–867. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef] [PubMed]
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Avezum, A.; et al. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef] [PubMed]
- Raunso, J.; Selmer, C.; Olesen, J.B.; Charlot, M.G.; Olsen, A.M.; Bretler, D.M.; Nielsen, J.D.; Dominguez, H.; Gadsboll, N.; Kober, L.; et al. Increased short-term risk of thrombo-embolism or death after interruption of warfarin treatment in patients with atrial fibrillation. Eur. Heart J. 2012, 33, 1886–1892. [Google Scholar] [CrossRef] [PubMed]
- Sjogren, V.; Grzymala-Lubanski, B.; Renlund, H.; Friberg, L.; Lip, G.Y.; Svensson, P.J.; Sjalander, A. Safety and efficacy of well managed warfarin. A report from the Swedish quality register Auricula. Thromb. Haemost. 2015, 113, 1370–1377. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Lane, D.A.; Torp-Pedersen, C.; Lip, G.Y. Net clinical benefit of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus no treatment in a “real world” atrial fibrillation population: A modelling analysis based on a nationwide cohort study. Thromb. Haemost. 2012, 107, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Roskell, N.S.; Samuel, M.; Noack, H.; Monz, B.U. Major bleeding in patients with atrial fibrillation receiving vitamin K antagonists: A systematic review of randomized and observational studies. Europace 2013, 15, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Zhou, M.; Tang, W.; Alexander, G.C.; Singh, S. Risk of gastrointestinal bleeding associated with oral anticoagulants: Population based retrospective cohort study. BMJ 2015, 350, h1585. [Google Scholar] [CrossRef] [PubMed]
- Gage, B.F.; Waterman, A.D.; Shannon, W.; Boechler, M.; Rich, M.W.; Radford, M.J. Validation of clinical classification schemes for predicting stroke: Results from the National Registry of Atrial Fibrillation. JAMA 2001, 285, 2864–2870. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef] [PubMed]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 2014, 130, e199–e267. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gage, B.F.; Yan, Y.; Milligan, P.E.; Waterman, A.D.; Culverhouse, R.; Rich, M.W.; Radford, M.J. Clinical classification schemes for predicting hemorrhage: Results from the National Registry of Atrial Fibrillation (NRAF). Am. Heart J. 2006, 151, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Pisters, R.; Lane, D.A.; Nieuwlaat, R.; de Vos, C.B.; Crijns, H.J.; Lip, G.Y. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest 2010, 138, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Fang, M.C.; Go, A.S.; Chang, Y.; Borowsky, L.H.; Pomernacki, N.K.; Udaltsova, N.; Singer, D.E. A new risk scheme to predict warfarin-associated hemorrhage: The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study. J. Am. Coll. Cardiol. 2011, 58, 395–401. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, E.C.; Simon, D.N.; Thomas, L.E.; Hylek, E.M.; Gersh, B.J.; Ansell, J.E.; Kowey, P.R.; Mahaffey, K.W.; Chang, P.; Fonarow, G.C.; et al. The ORBIT bleeding score: A simple bedside score to assess bleeding risk in atrial fibrillation. Eur. Heart J. 2015, 36, 3258–3264. [Google Scholar] [CrossRef] [PubMed]
- Hijazi, Z.; Oldgren, J.; Lindback, J.; Alexander, J.H.; Connolly, S.J.; Eikelboom, J.W.; Ezekowitz, M.D.; Held, C.; Hylek, E.M.; Lopes, R.D.; et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: A derivation and validation study. Lancet 2016, 387, 2302–2311. [Google Scholar] [CrossRef]
- Roldan, V.; Marin, F.; Manzano-Fernandez, S.; Gallego, P.; Vilchez, J.A.; Valdes, M.; Vicente, V.; Lip, G.Y. The HAS-BLED score has better prediction accuracy for major bleeding than CHADS2 or CHA2DS2-VASc scores in anticoagulated patients with atrial fibrillation. J. Am. Coll. Cardiol. 2013, 62, 2199–2204. [Google Scholar] [CrossRef] [PubMed]
- Peacock, W.F.; Tamayo, S.; Patel, M.; Sicignano, N.; Hopf, K.P.; Yuan, Z. CHA2DS2-VASc scores and major bleeding in patients with nonvalvular atrial fibrillation who are receiving rivaroxaban. Ann. Emerg. Med. 2017, 69, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Russo, V.; Rago, A.; Proietti, R.; Di Meo, F.; Antonio Papa, A.; Calabro, P.; D’Onofrio, A.; Nigro, G.; AlTurki, A. Efficacy and safety of the target-specific oral anticoagulants for stroke prevention in atrial fibrillation: The real-life evidence. Ther. Adv. Drug Saf. 2017, 8, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Russo, V.; Di Napoli, L.; Bianchi, V.; Tavoletta, V.; de Vivo, S.; Cavallaro, C.; Vecchione, F.; Rago, A.; Sarubbi, B.; Calabro, P.; et al. A new integrated strategy for direct current cardioversion in non-valvular atrial fibrillation patients using short term rivaroxaban administration: The MonaldiVert real life experience. Int. J. Cardiol. 2016, 224, 454–455. [Google Scholar] [CrossRef] [PubMed]
- Stabile, G.; Russo, V.; Rapacciuolo, A.; de Divitiis, M.; de Simone, A.; Solimene, F.; D’Onofrio, A.; Iuliano, A.; Maresca, G.; Esposito, F.; et al. Transesophageal echocardiograpy in patients with persistent atrial fibrillation undergoing electrical cardioversion on new oral anticoagulants: A multi-center registry. Int. J. Cardiol. 2015, 184, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Lu, Y.; Qin, Y. A meta-analysis of randomized controlled trials of uninterrupted periprocedural anticoagulation strategy in patients undergoing atrial fibrillation catheter ablation. Int. J. Cardiol. 2018, 270, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Winocour, P.H. Diabetes and chronic kidney disease: An increasingly common multi-morbid disease in need of a paradigm shift in care. Diabet. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Fihn, S.D.; Blankenship, J.C.; Alexander, K.P.; Bittl, J.A.; Byrne, J.G.; Fletcher, B.J.; Fonarow, G.C.; Lange, R.A.; Levine, G.N.; Maddox, T.M.; et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2014, 130, 1749–1767. [Google Scholar] [CrossRef] [PubMed]
- Levine, G.N.; Bates, E.R.; Bittl, J.A.; Brindis, R.G.; Fihn, S.D.; Fleisher, L.A.; Granger, C.B.; Lange, R.A.; Mack, M.J.; Mauri, L.; et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation 2016, 134, e123–e155. [Google Scholar] [CrossRef] [PubMed]
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients with Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2017, 135, e726–e779. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Ogden, L.G.; Bazzano, L.A.; Vupputuri, S.; Loria, C.; Whelton, P.K. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch. Intern. Med. 2001, 161, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.C., Jr.; Benjamin, E.J.; Bonow, R.O.; Braun, L.T.; Creager, M.A.; Franklin, B.A.; Gibbons, R.J.; Grundy, S.M.; Hiratzka, L.F.; Jones, D.W.; et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: A guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 2011, 124, 2458–2473. [Google Scholar] [CrossRef] [PubMed]
- Yao, X.; Abraham, N.S.; Sangaralingham, L.R.; Bellolio, M.F.; McBane, R.D.; Shah, N.D.; Noseworthy, P.A. Effectiveness and safety of dabigatran, rivaroxaban, and apixaban versus warfarin in nonvalvular atrial fibrillation. J. Am. Heart Assoc. 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Hankey, G.J.; Stevens, S.R.; Piccini, J.P.; Lokhnygina, Y.; Mahaffey, K.W.; Halperin, J.L.; Patel, M.R.; Breithardt, G.; Singer, D.E.; Becker, R.C.; et al. Intracranial hemorrhage among patients with atrial fibrillation anticoagulated with warfarin or rivaroxaban: The rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation. Stroke 2014, 45, 1304–1312. [Google Scholar] [CrossRef] [PubMed]
- Hori, M.; Connolly, S.J.; Zhu, J.; Liu, L.S.; Lau, C.P.; Pais, P.; Xavier, D.; Kim, S.S.; Omar, R.; Dans, A.L.; et al. Dabigatran versus warfarin: Effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke 2013, 44, 1891–1896. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.S.; Zhang, L.; He, Q.; Li, Y.B.; Dai, Z.L.; Zheng, J.R.; Cheng, P.Q.; He, Y.S. DNA sensors to assess the effect of VKORC1 and CYP2C9 gene polymorphisms on warfarin dose requirement in Chinese patients with atrial fibrillation. Australas. Phys. Eng. Sci. Med. 2017, 40, 249–258. [Google Scholar] [CrossRef] [PubMed]
| Apixaban (n = 5843) | Rivaroxaban (n = 27,777) | Dabagatran (n = 20,079) | Warfarin (n = 19,375) | p-Value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (year) | 76 ± 10 | 75 ± 10 | 75 ± 10 | 71 ± 13 | <0.0001 |
| Male gender | 3214 (55.01%) | 15,374 (55.35%) | 12,061 (60.07%) | 11,221 (57.91%) | <0.0001 |
| CHA2DS2-VASc score | 3.89 ± 1.56 | 3.83 ± 1.57 | 3.74 ± 1.52 | 3.26 ± 1.81 | <0.0001 |
| Comorbidities | |||||
| Hypertension | 5055 (86.51%) | 23,766 (85.56%) | 16,863 (83.98%) | 15,099 (77.93%) | <0.0001 |
| Diabetes mellitus | 2389 (40.89%) | 10,752 (38.71%) | 7647 (38.08%) | 6948 (35.86%) | <0.0001 |
| PAOD | 4 (0.07%) | 19 (0.07%) | 11 (0.05%) | 16 (0.08%) | 0.7736 |
| Ischemic heart disease | 733 (12.54%) | 3399 (12.24%) | 1961 (9.77%) | 2098 (10.83%) | <0.0001 |
| PCI | 415 (7.1%) | 1750 (6.3%) | 916 (4.56%) | 1051 (5.42%) | <0.0001 |
| CABG | 31 (0.53%) | 104 (0.37%) | 40 (0.2%) | 143 (0.74%) | <0.0001 |
| Heart failure | 735 (12.58%) | 3582 (12.9%) | 2172 (10.82%) | 2699 (13.93%) | <0.0001 |
| Chronic kidney disease | 1671 (28.6%) | 6786 (24.43%) | 3922 (19.53%) | 4702 (24.27%) | <0.0001 |
| Chronic liver disease | 929 (15.9%) | 4421 (15.92%) | 2831 (14.1%) | 3048 (15.73%) | <0.0001 |
| TIA | 167 (2.86%) | 667 (2.4%) | 573 (2.85%) | 344 (1.78%) | <0.0001 |
| Stroke | 1173 (20.08%) | 5675 (20.43%) | 4778 (23.8%) | 2936 (15.15%) | <0.0001 |
| History of bleeding | 113 (1.93%) | 644 (2.32%) | 415 (2.07%) | 451 (2.33%) | 0.0841 |
| Medication used | |||||
| NSAID | 1556 (26.63%) | 6657 (23.97%) | 4401 (21.92%) | 4792 (24.73%) | <0.0001 |
| Anti-platelets | 3231 (55.3%) | 15,450 (55.62%) | 10,906 (54.32%) | 11,907 (61.46%) | <0.0001 |
| H2 blocker | 1810 (30.98%) | 8175 (29.43%) | 5772 (28.75%) | 6200 (32%) | <0.0001 |
| PPI | 655 (11.21%) | 2906 (10.46%) | 1654 (8.24%) | 2421 (12.5%) | <0.0001 |
| Amiodarone | 1649 (28.22%) | 7370 (26.53%) | 4498 (22.4%) | 7472 (38.57%) | <0.0001 |
| Beta-blocker | 3451 (59.06%) | 15,782 (56.82%) | 10,839 (53.98%) | 11,824 (61.03%) | <0.0001 |
| Statin | 229 (3.92%) | 3949 (14.22%) | 4101 (20.42%) | 3322 (17.15%) | <0.0001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.-T.; Chang, S.-H.; Yeh, Y.-H.; Tu, H.-T.; Chan, Y.-H.; Kuo, C.-T.; See, L.-C. The CHA2DS2-VASc Score Predicts Major Bleeding in Non-Valvular Atrial Fibrillation Patients Who Take Oral Anticoagulants. J. Clin. Med. 2018, 7, 338. https://doi.org/10.3390/jcm7100338
Lee K-T, Chang S-H, Yeh Y-H, Tu H-T, Chan Y-H, Kuo C-T, See L-C. The CHA2DS2-VASc Score Predicts Major Bleeding in Non-Valvular Atrial Fibrillation Patients Who Take Oral Anticoagulants. Journal of Clinical Medicine. 2018; 7(10):338. https://doi.org/10.3390/jcm7100338
Chicago/Turabian StyleLee, Kuang-Tso, Shang-Hung Chang, Yung-Hsin Yeh, Hui-Tzu Tu, Yi-Hsin Chan, Chi-Tai Kuo, and Lai-Chu See. 2018. "The CHA2DS2-VASc Score Predicts Major Bleeding in Non-Valvular Atrial Fibrillation Patients Who Take Oral Anticoagulants" Journal of Clinical Medicine 7, no. 10: 338. https://doi.org/10.3390/jcm7100338
APA StyleLee, K.-T., Chang, S.-H., Yeh, Y.-H., Tu, H.-T., Chan, Y.-H., Kuo, C.-T., & See, L.-C. (2018). The CHA2DS2-VASc Score Predicts Major Bleeding in Non-Valvular Atrial Fibrillation Patients Who Take Oral Anticoagulants. Journal of Clinical Medicine, 7(10), 338. https://doi.org/10.3390/jcm7100338





