Effectiveness and Safety of Direct Oral Anticoagulants versus Vitamin K Antagonists for People Aged 75 Years and over with Atrial Fibrillation: A Systematic Review and Meta-Analyses of Observational Studies
Abstract
1. Introduction
2. Experimental Section
2.1. Search Strategy and Selection Criteria
2.2. Data Analysis
3. Results
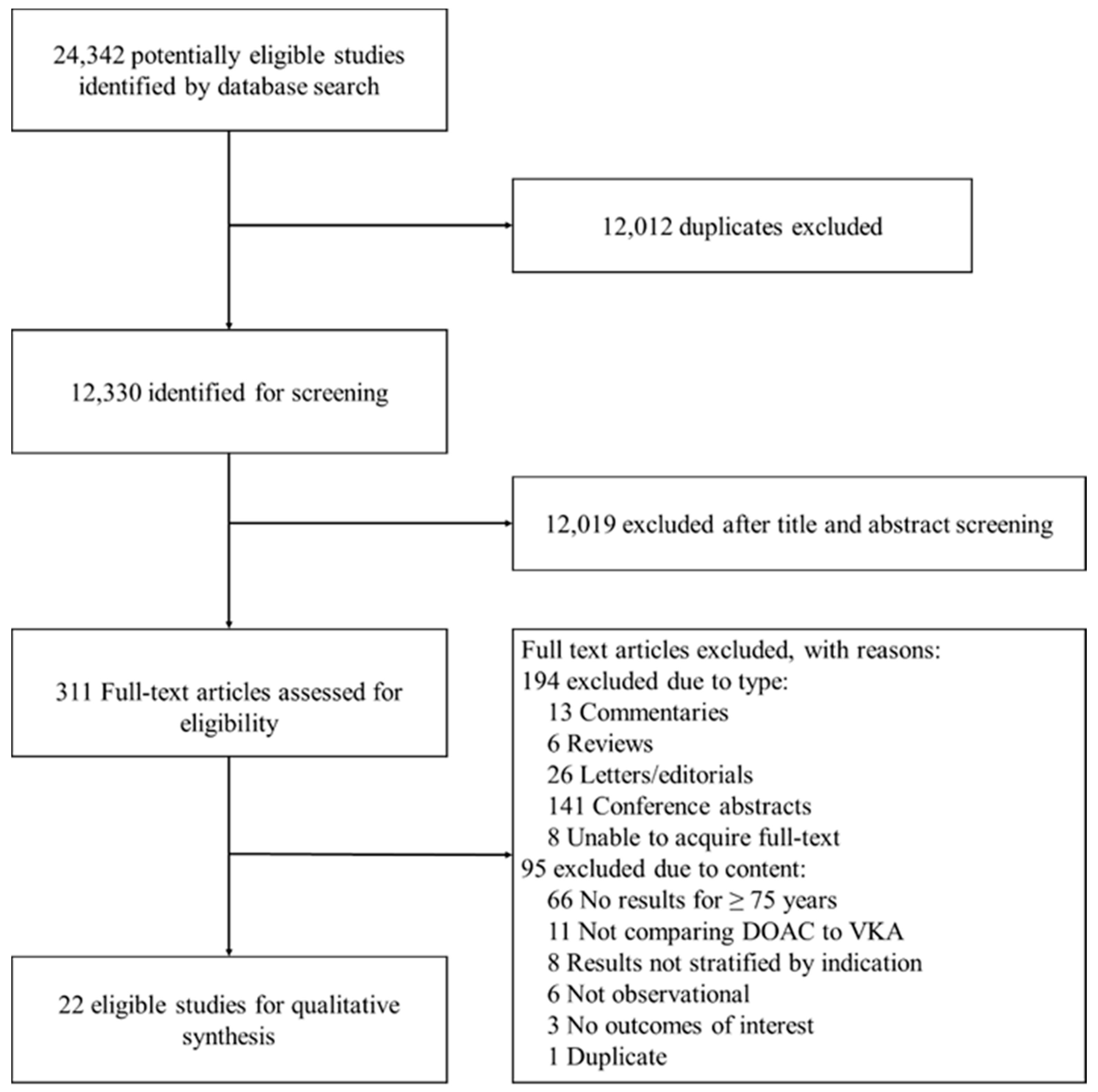
3.1. Study Identification
3.2. Characteristics of Included Studies
3.3. Risk of Bias
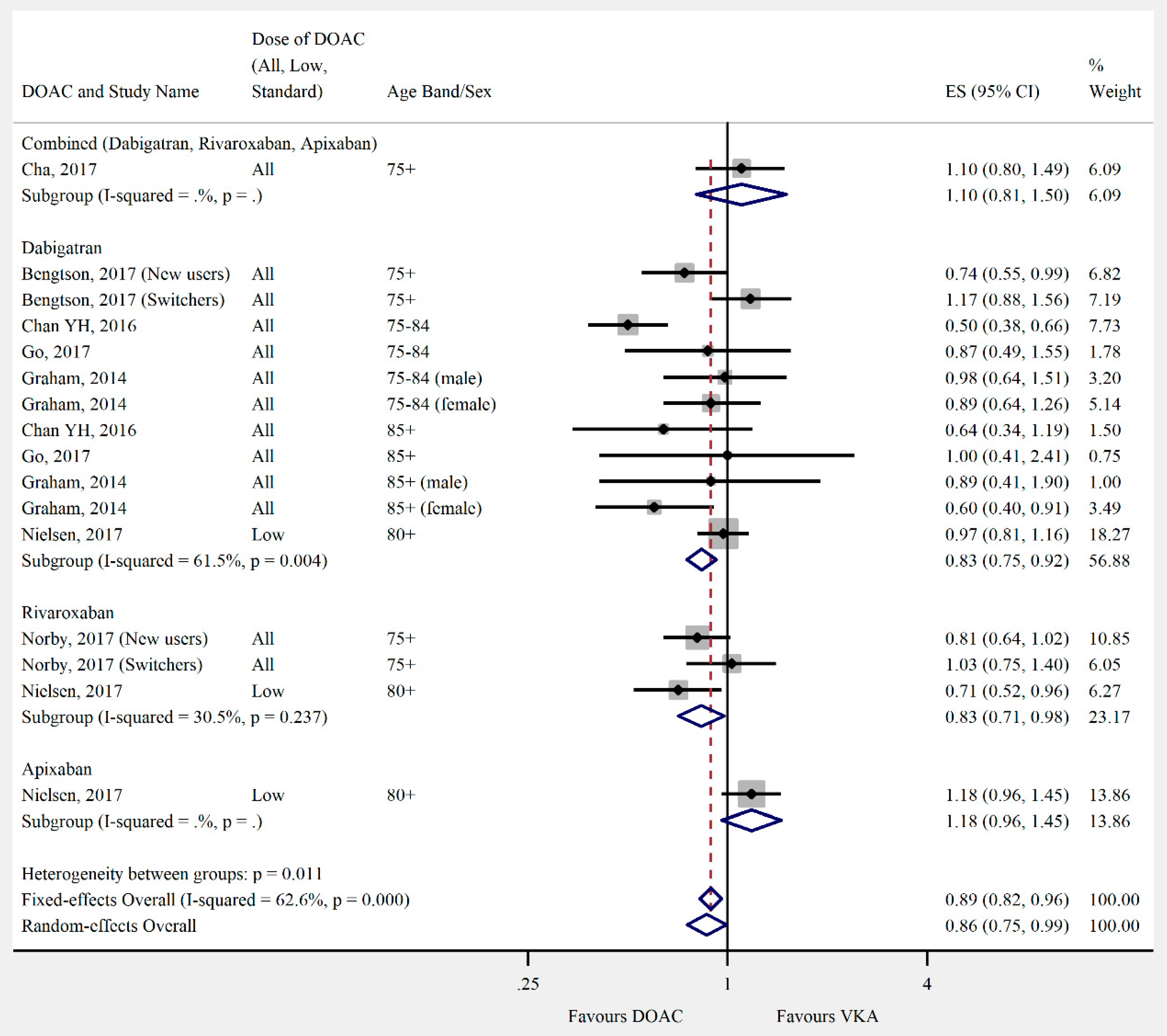
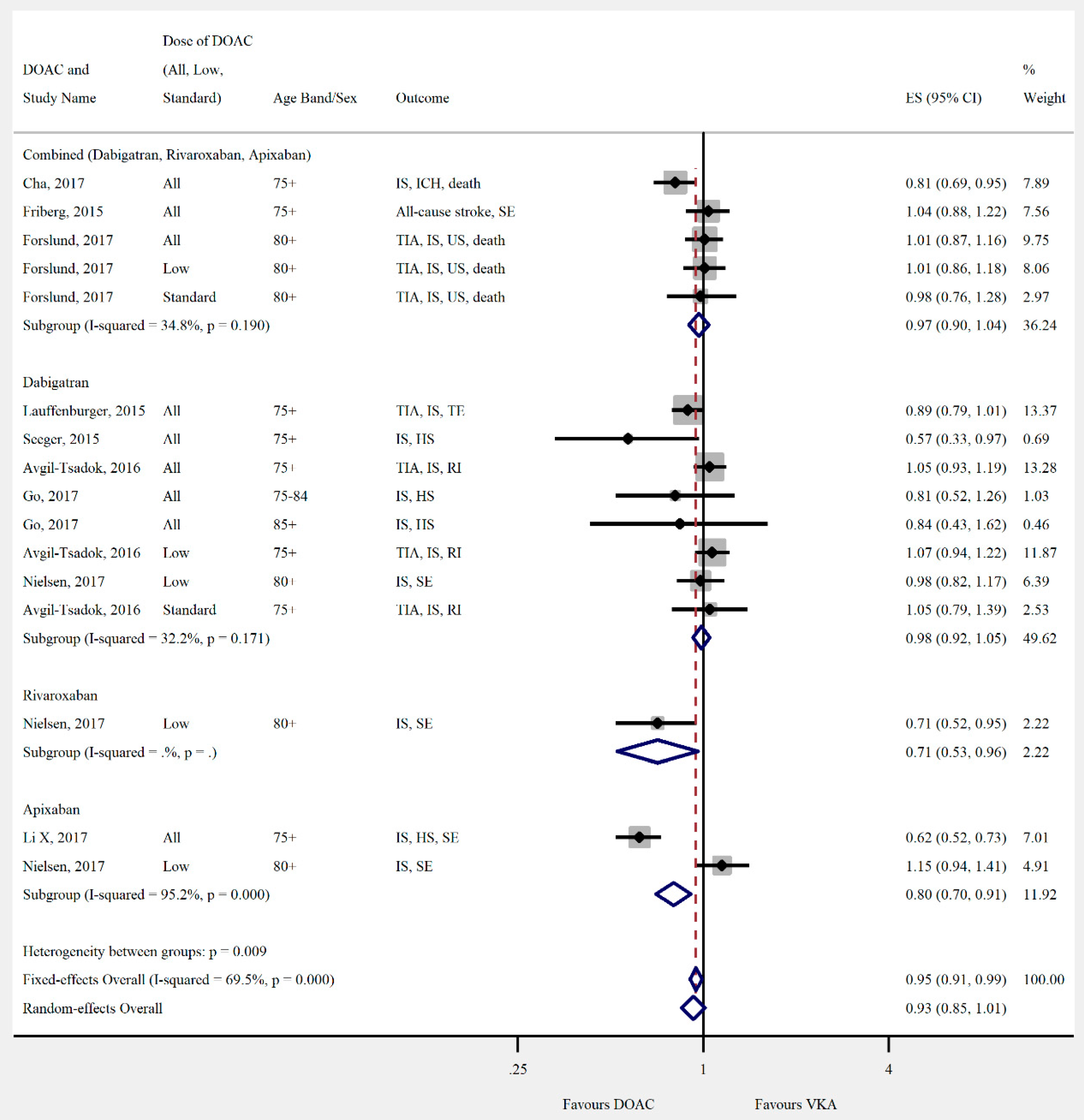
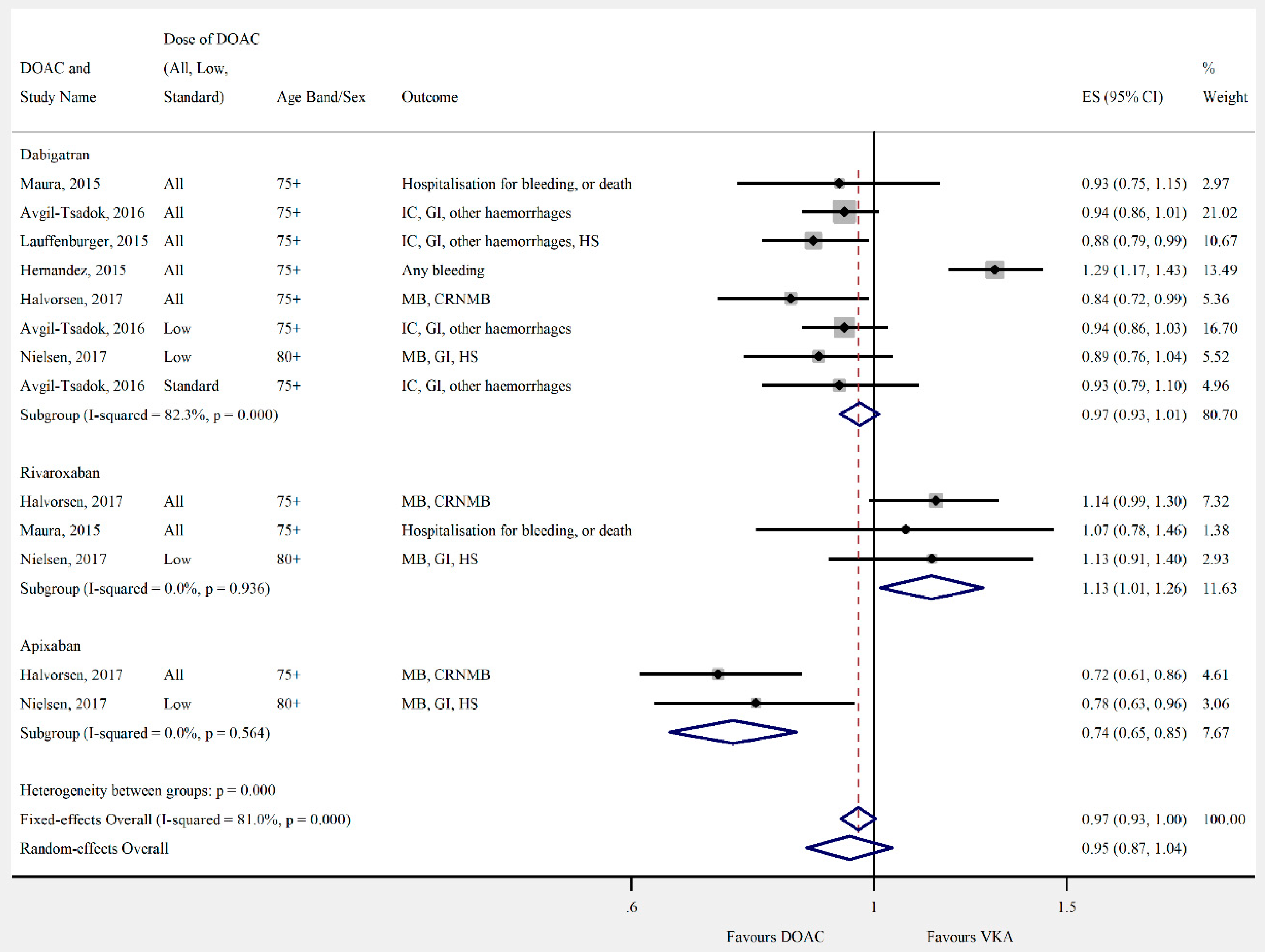
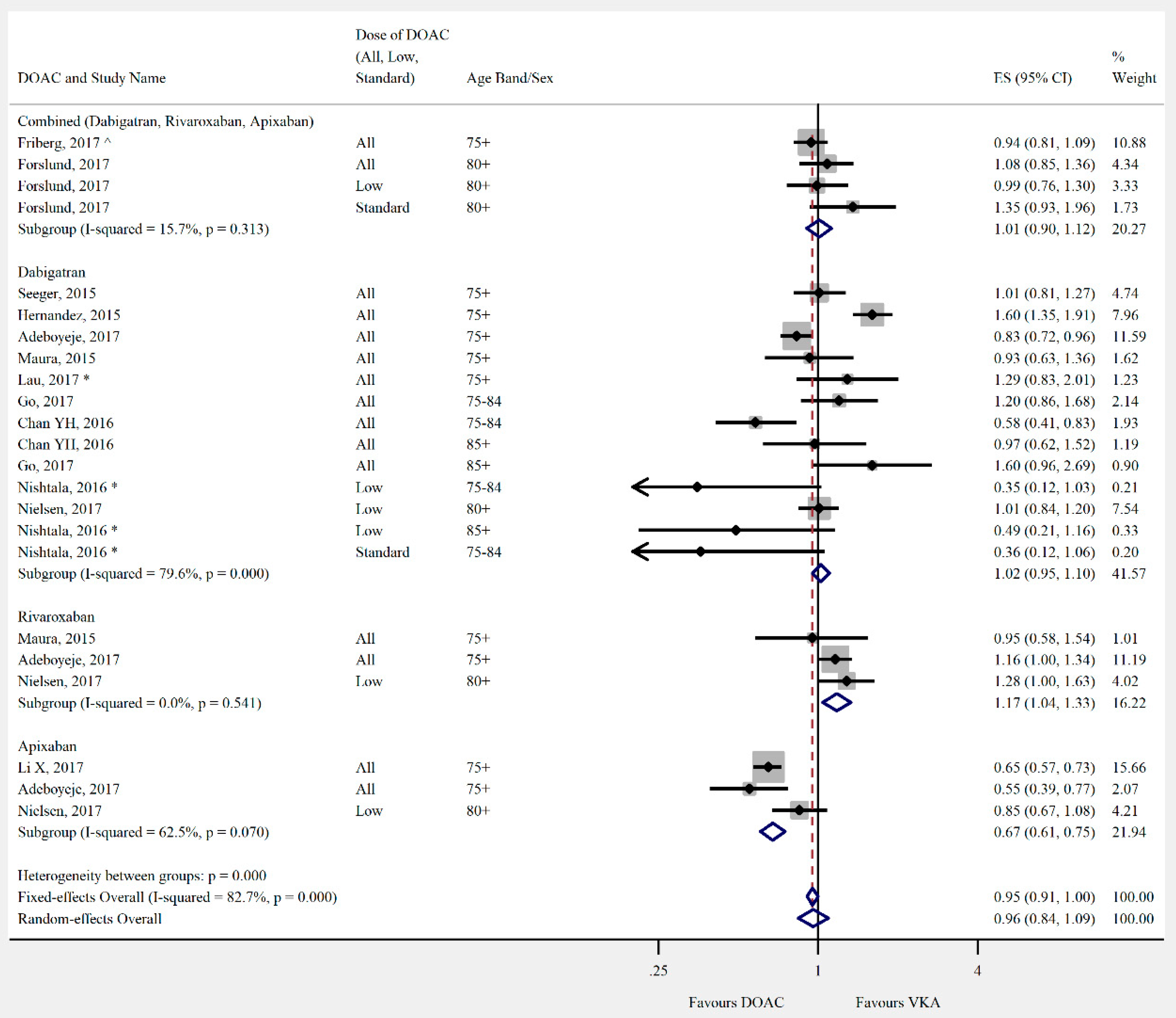
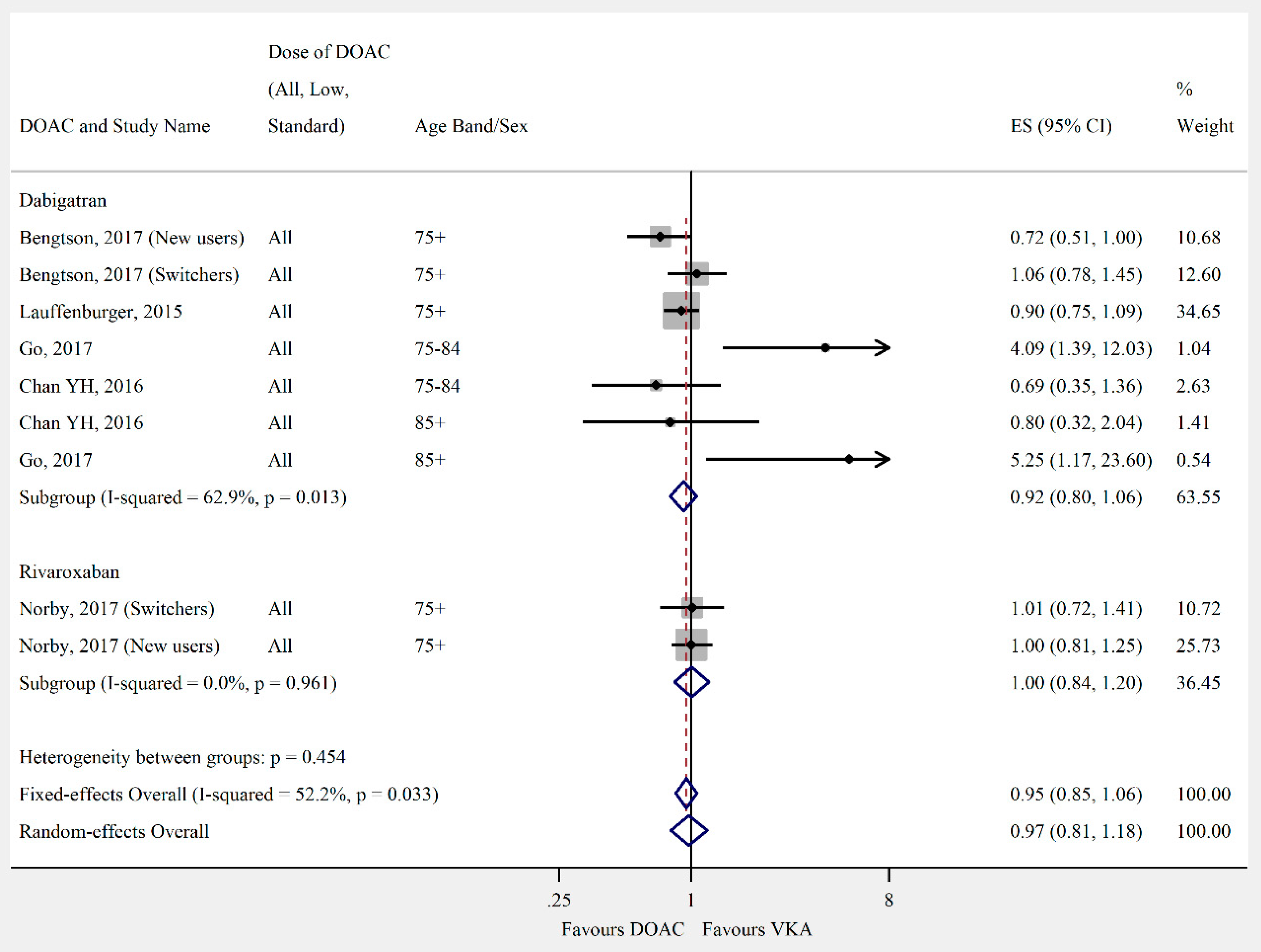
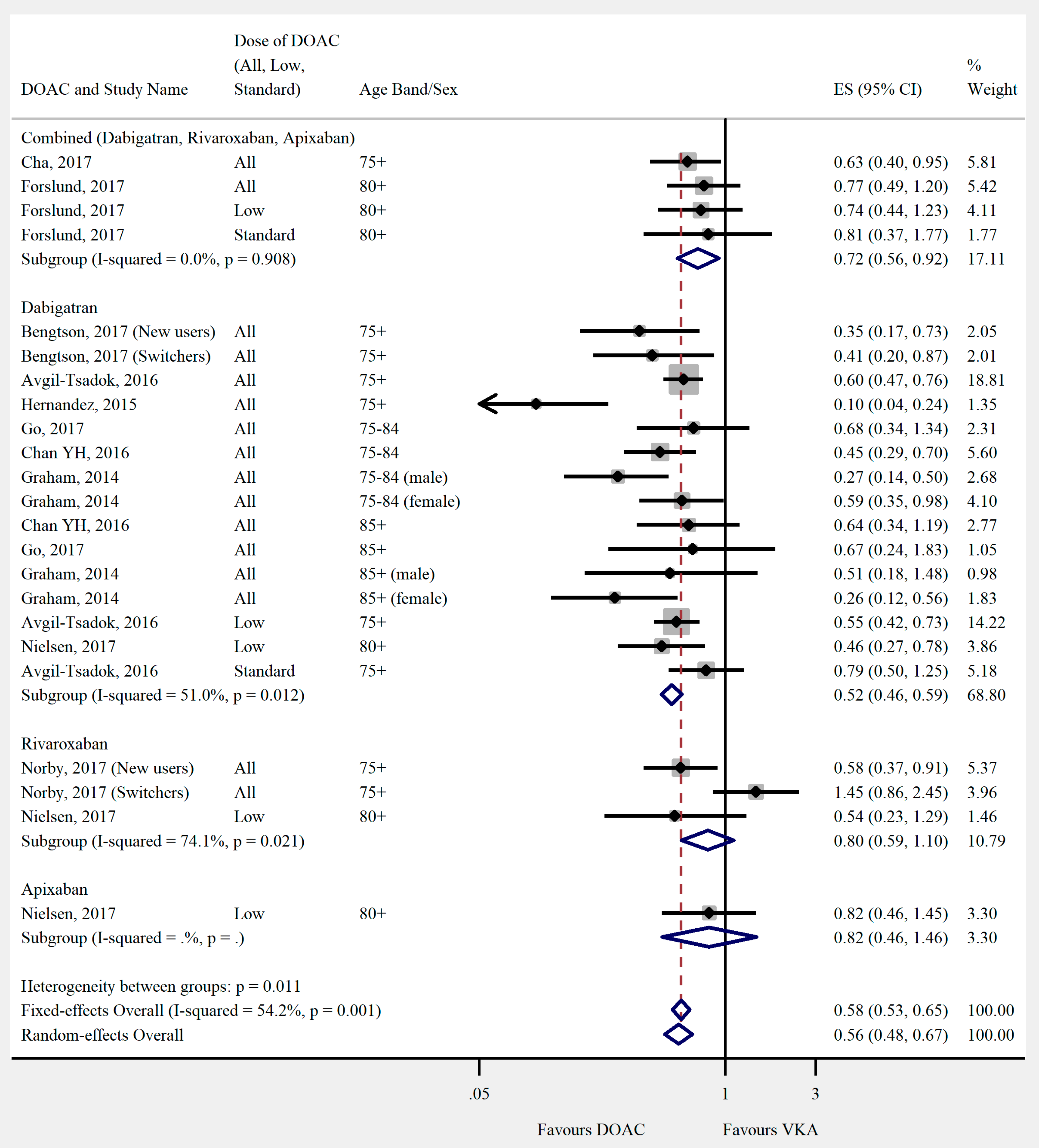
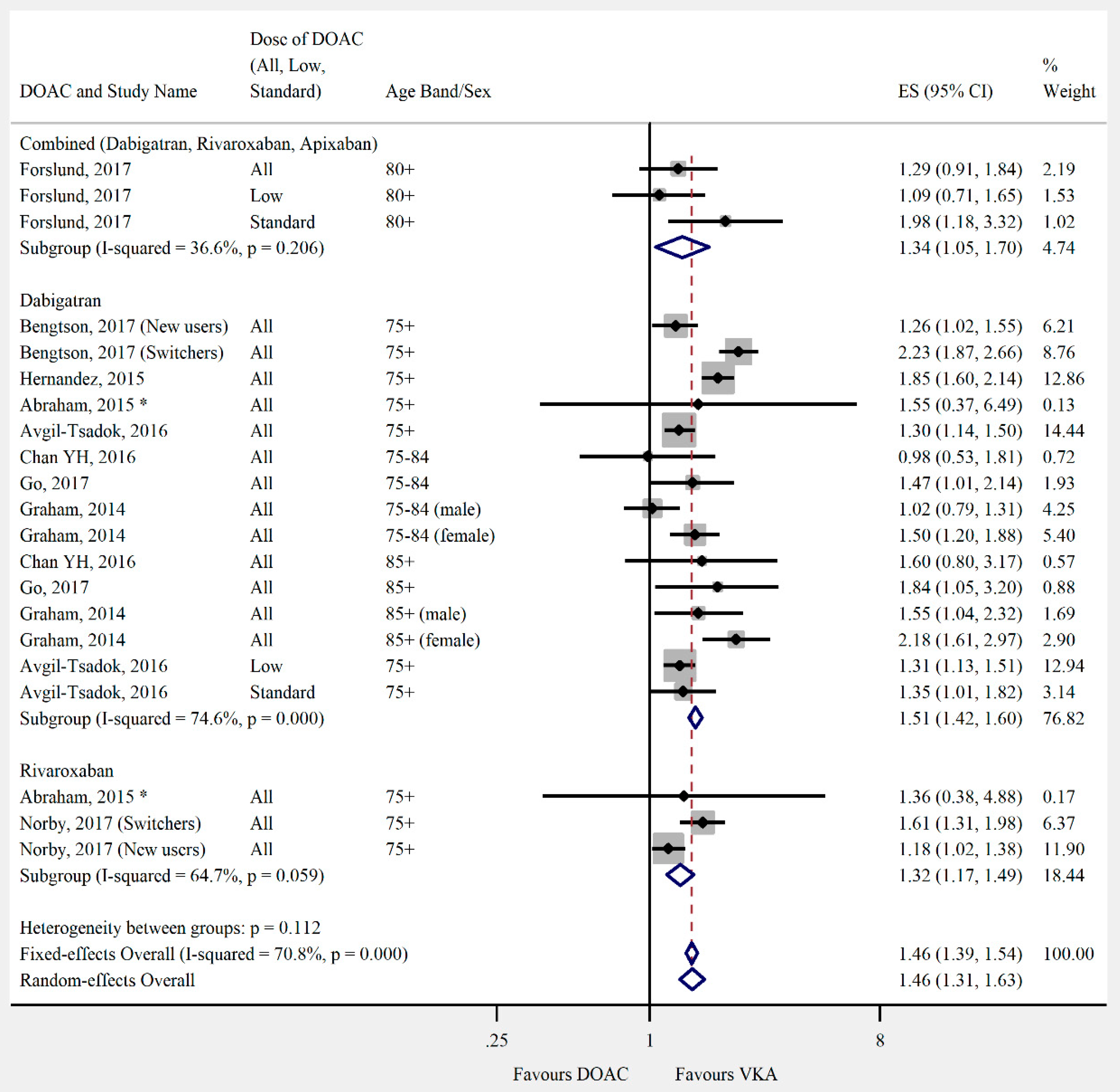
3.4. Outcomes
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategy
- Rivaroxaban (MeSH and ti,ab) OR Xarelto.ti,ab OR Apixaban.ti,ab OR Eliquis.ti,ab OR Dabigatran (MeSH and ti,ab) OR Pradaxa.ti,ab OR Edoxaban.ti,ab OR Lixiana.ti,ab OR Savaysa.ti,ab OR Factor Xa Inhibitors (Pharmacological Action) OR Antithrombins (Pharmacological Action) OR “New oral anticoagulant$”.ti,ab OR “Novel oral anticoagulant$”.ti,ab OR “direct oral anticoagulant$”.ti,ab OR (NOAC or NOACS).ti,ab OR (DOAC or DOACS).ti,ab OR oral adj2 anticoagulant$.ti,ab)
- (Warfarin (MeSH and ti,ab) OR exp Coumarins (MeSH) OR Coumarin*.ti,ab OR Acenocoumarol (MeSH and ti,ab) OR Fluindione.ti,ab OR Phenindione (MeSH and ti,ab))
- (exp Atrial fibrillation (MeSH and free text) OR exp atrial flutter (MeSH and free text) OR exp stroke (MeSH and ti,ab) OR ((atrial or atrium or auricular) adj3 fibrillat*).ti,ab OR heart fibrillat*.ti,ab OR ((atrial or atrium) adj3 (tachycardi$ or arrythmi$)).ti,ab OR (atrial adj3 tachyarrhythmi$).ti,ab OR ((atrial or auricular) adj3 flutter$).ti,ab).
- Rivaroxaban (Emtree and ti,ab) OR Xarelto.ti,ab OR dabigatran (Emtree and ti,ab) OR dabigatran etexilate (Emtree) OR Pradaxa.ti,ab OR apixaban (Emtree and ti,ab) OR Eliquis.ti,ab OR edoxaban (Emtree and ti,ab) OR Lixiana.ti,ab OR Savaysa.ti,ab OR thrombin inhibitor (Emtree) OR exp blood clotting factor 10A inhibitor (Emtree) OR “direct oral anticoagulant$”.ti,ab OR “novel oral anticoagulant$”.ti,ab OR “new oral anticoagulant$”.ti,ab OR (NOAC or NOACS).ti,ab OR (DOAC or DOACS).ti,ab OR oral adj2 anticoagulant$.ti,ab
- Warfarin (Emtree and ti,ab) OR antivitamin k (Emtree) OR fluindione (Emtree and ti,ab) OR acenocoumarol (Emtree and ti,ab) OR phenindione (Emtree and ti,ab) OR exp coumarin anticoagulant (Emtree)
- Exp Cerebrovascular accident (Emtree) OR stroke.ti,ab OR exp atrial fibrillation (Emtree or ti,ab) OR atrial flutter.ti,ab OR heart atrium flutter.ti,ab ((atrial or atrium or auricular) adj3 fibrillat*).ti,ab OR heart fibrillat*.ti,ab OR ((atrial or atrium) adj3 (tachycardi$ or arrythmi$)).ti,ab OR (atrial adj3 tachyarrhythmi$).ti,ab OR ((atrial or auricular) adj3 flutter$).ti,ab
Appendix B. Modified Newcastle–Ottawa Scale
- 1.
- Representativeness of the Exposed Cohort
- a)
- Truly representative of the average atrial fibrillation patient in the community (2 point)
- b)
- Somewhat representative of the average atrial fibrillation patient in the community (1 point)
- c)
- Selected group of users e.g., hospital inpatients
- d)
- No description of the derivation of the cohort
- 2.
- Selection of the Non-Exposed Cohort
- a)
- Drawn from the same community as the exposed cohort (1 point)
- b)
- Drawn from a different source
- c)
- No description of the derivation of the non-exposed cohort
- 3.
- Ascertainment of Exposure
- a)
- Secure record (e.g., medical records)—describes how both the initial and ongoing exposure were measured (2 points)
- b)
- Secure record (e.g., medical records)—describes only how the initial exposure was measured (1 point)
- c)
- Structured interview (1 point)
- d)
- Written self-report
- e)
- No description
- 4.
- Demonstration that Outcome of Interest was not Present at Start of StudyIn the case of mortality studies, outcome of interest is still the presence of a disease/ incident, rather than death. That is to say that a statement of no history of disease or incident earns a star
- a)
- Yes (1 point)
- b)
- No
- 5.
- Comparability of Cohorts on the Basis of the Design or Analysis
- a)
- Study controls for age, sex, medication and comorbidities at baseline (1 point)
- b)
- Study controls for the above plus any additional factors (such as socioeconomic status, type of prescriber) (2 points)
- c)
- Limited or no attempt to control for differences in cohorts
- 6.
- Assessment of Outcome
- a)
- Independent or blind assessment stated in the paper, or confirmation of the outcome by reference to secure records (x-rays, medical records, etc.) (2 point)
- b)
- Record linkage (e.g., identified through ICD codes on database records) (1 point)
- c)
- Self-report (i.e., no reference to original medical records or x-rays to confirm the outcome)
- d)
- No description
- 7.
- Was Follow-Up Long Enough for Outcomes to Occur
- a)
- yes—for all primary outcomes (minimum follow-up of 3 months for bleeding outcomes, 1 year for effectiveness outcomes) (2 points)
- b)
- Yes—for some outcomes (1 point)
- c)
- No
- d)
- Length of follow-up not stated
- 8.
- Adequacy of Follow-Up of Cohorts
- a)
- Complete follow-up - all subjects accounted for (1 point)
- b)
- Subjects lost to follow-up unlikely to introduce bias - small number lost, follow-up, or description provided of those lost) (1 point)
- c)
- Follow-up rate <50% and no description of those lost
- d)
- No statement
References
- Zoni-Berisso, M.; Lercari, F.; Carazza, T.; Domenicucci, S. Epidemiology of atrial fibrillation: European perspective. Clin. Epidemiol. 2014, 6, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.N.; Abdelhafiz, A. Clinical and Economic Implications of AF Related Stroke. J. Atr. Fibrillat. 2016, 8, 1279. [Google Scholar]
- Hart, R.G.; Pearce, L.A.; Aguilar, M.I. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann. Intern. Med. 2007, 146, 857–867. [Google Scholar] [CrossRef] [PubMed]
- Mant, J.; Hobbs, F.D.; Fletcher, K.; Roalfe, A.; Fitzmaurice, D.; Lip, G.Y.; Murray, E. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): A randomised controlled trial. Lancet 2007, 370, 493–503. [Google Scholar] [CrossRef]
- Scowcroft, A.C.; Lee, S.; Mant, J. Thromboprophylaxis of elderly patients with AF in the UK: An analysis using the General Practice Research Database (GPRD) 2000-2009. Heart 2013, 99, 127–132. [Google Scholar] [CrossRef][Green Version]
- Loo, S.Y.; Dell’Aniello, S.; Huiart, L.; Renoux, C. Trends in the prescription of novel oral anticoagulants in UK primary care. Br. J. Clin. Pharmacol. 2017, 83, 2096–2106. [Google Scholar] [CrossRef]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.H.; Banerjee, A.; Boriani, G.; Chiang, C.E.; Fargo, R.; Freedman, B.; Lane, D.A.; Ruff, C.T.; Turakhia, M.; Werring, D.; et al. Antithrombotic Therapy for Atrial Fibrillation: CHEST Guideline and Expert Panel Report. Chest 2018, 154, 1121–1201. [Google Scholar] [CrossRef]
- Mitchell, A.; Watson, M.C.; Welsh, T.; McGrogan, A. Systematic Review and Meta-Analysis of Observational Studies Comparing Direct Oral Anticoagulants with Vitamin K Antagonists for Stroke Prevention and Major Bleeding in People Aged over 75 Years Old with Atrial Fibrillation. Available online: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018081696 (accessed on 22 April 2019).
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. (Clin. Res. Ed.) 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Fisher, D. Two-stage individual participant data meta-analysis and generalized forest plots. Stata J. 2015, 15, 369–396. [Google Scholar] [CrossRef]
- Go, A.S.; Singer, D.E.; Toh, S.; Cheetham, T.C.; Reichman, M.E.; Graham, D.J.; Southworth, M.R.; Zhang, R.; Izem, R.; Goulding, M.R.; et al. Outcomes of Dabigatran and Warfarin for Atrial Fibrillation in Contemporary Practice A Retrospective Cohort Study. Ann. Intern. Med. 2017, 167, 845–854. [Google Scholar] [CrossRef]
- Cha, M.J.; Choi, E.K.; Han, K.D.; Lee, S.R.; Lim, W.H.; Oh, S.; Lip, G.Y.H. Effectiveness and Safety of Non-Vitamin K Antagonist Oral Anticoagulants in Asian Patients with Atrial Fibrillation. Stroke 2017, 48, 3040–3048. [Google Scholar] [CrossRef]
- Lau, W.C.Y.; Li, X.; Wong, I.C.K.; Man, K.K.C.; Lip, G.Y.H.; Leung, W.K.; Siu, C.W.; Chan, E.W. Bleeding-related hospital admissions and 30-day readmissions in patients with non-valvular atrial fibrillation treated with dabigatran versus warfarin. J. Thromb. Haemost. 2017, 15, 1923–1933. [Google Scholar] [CrossRef]
- Norby, F.L.; Bengtson, L.G.S.; Lutsey, P.L.; Chen, L.Y.; MacLehose, R.F.; Chamberlain, A.M.; Rapson, I.; Alonso, A. Comparative effectiveness of rivaroxaban versus warfarin or dabigatran for the treatment of patients with non-valvular atrial fibrillation. BMC Cardiovasc. Disord. 2017, 17, 238. [Google Scholar] [CrossRef]
- Adeboyeje, G.; Sylwestrzak, G.; Barron, J.J.; White, J.; Rosenberg, A.; Abarca, J.; Crawford, G.; Redberg, R. Major Bleeding Risk During Anticoagulation with Warfarin, Dabigatran, Apixaban, or Rivaroxaban in Patients with Nonvalvular Atrial Fibrillation. J. Manag. Care Spec. Pharm. 2017, 23, 968–978. [Google Scholar] [CrossRef]
- Bengtson, L.G.S.; Lutsey, P.L.; Chen, L.Y.; MacLehose, R.F.; Alonso, A. Comparative effectiveness of dabigatran and rivaroxaban versus warfarin for the treatment of non-valvular atrial fibrillation. J. Cardiol. 2017, 69, 868–876. [Google Scholar] [CrossRef]
- Nielsen, P.B.; Skjoth, F.; Sogaard, M.; Kjaeldgaard, J.N.; Lip, G.Y.H.; Larsen, T.B. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: Propensity weighted nationwide cohort study. Br. Med. J. 2017, 356, j510. [Google Scholar] [CrossRef]
- Forslund, T.; Wettermark, B.; Andersen, M.; Hjemdahl, P. Stroke and bleeding with non-vitamin K antagonist oral anticoagulant or warfarin treatment in patients with non-valvular atrial fibrillation: A population-based cohort study. Europace 2018, 20, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Halvorsen, S.; Ghanima, W.; Tvete, I.F.; Hoxmark, C.; Falck, P.; Solli, O.; Jonasson, C. A nationwide registry study to compare bleeding rates in patients with atrial fibrillation being prescribed oral anticoagulants. Eur. Heart J. Cardiovasc. Pharmacother. 2017, 3, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.H.; Huang, D.; Hai, J.J.; Li, W.-H.; Yin, L.-X.; Chan, E.W.; Wong, I.C.K.; Lau, C.-P.; Chiang, C.-E.; Zhu, J.; et al. Stroke prevention using dabigatran in elderly Chinese patients with atrial fibrillation. Heart Rhythm 2016, 13, 366–373. [Google Scholar] [CrossRef]
- Nishtala, P.S.; Gnjidic, D.; Jamieson, H.A.; Hanger, H.C.; Kaluarachchi, C.; Hilmer, S.N. ‘Real-world’ haemorrhagic rates for warfarin and dabigatran using population-level data in New Zealand. Int. J. Cardiol. 2016, 203, 746–752. [Google Scholar] [CrossRef]
- Avgil-Tsadok, M.; Jackevicius, C.A.; Essebag, V.; Eisenberg, M.J.; Rahme, E.; Behlouli, H.; Pilote, L. Dabigatran use in elderly patients with atrial fibrillation. Thromb. Haemost. 2016, 115, 152–160. [Google Scholar] [CrossRef]
- Kwon, C.H.; Kim, M.; Kim, J.; Nam, G.B.; Choi, K.J.; Kim, Y.H. Real-world comparison of non-vitamin K antagonist oral anticoagulants and warfarin in Asian octogenarian patients with atrial fibrillation. J. Geriatr. Cardiol. 2016, 13, 566–572. [Google Scholar] [PubMed]
- Seeger, J.D.; Bykov, K.; Bartels, D.B.; Huybrechts, K.; Zint, K.; Schneeweiss, S. Safety and effectiveness of dabigatran and warfarin in routine care of patients with atrial fibrillation. Thromb. Haemost. 2015, 114, 1277–1289. [Google Scholar] [PubMed]
- Maura, G.; Blotière, P.O.; Bouillon, K.; Billionnet, C.; Ricordeau, P.; Alla, F.; Zureik, M. Comparison of the Short-Term Risk of Bleeding and Arterial Thromboembolic Events in Nonvalvular Atrial Fibrillation Patients Newly Treated with Dabigatran or Rivaroxaban Versus Vitamin K Antagonists A French Nationwide Propensity-Matched Cohort Study. Circulation 2015, 132, 1252–1260. [Google Scholar] [CrossRef] [PubMed]
- Abraham, N.S.; Singh, S.; Alexander, G.C.; Heien, H.; Haas, L.R.; Crown, W.; Shah, N.D. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: Population based cohort study. Br. Med. J. 2015, 350, h1857. [Google Scholar] [CrossRef]
- Lauffenburger, J.C.; Farley, J.F.; Gehi, A.K.; Rhoney, D.H.; Brookhart, M.A.; Fang, G. Effectiveness and safety of dabigatran and warfarin in real-world US patients with non-valvular atrial fibrillation: A retrospective cohort study. J. Am. Heart Assoc. 2015, 4, e001798. [Google Scholar] [CrossRef]
- Hernandez, I.; Baik, S.H.; Piñera, A.; Zhang, Y. Risk of Bleeding with Dabigatran in Atrial Fibrillation. JAMA Intern. Med. 2015, 175, 18–24. [Google Scholar] [CrossRef]
- Friberg, L.; Oldgren, J. Efficacy and safety of non-Vitamin K antagonist oral anticoagulants compared with warfarin in patients with atrial fibrillation. Open Heart 2017, 4, e000682. [Google Scholar] [CrossRef]
- Li, X.; Deitelzweig, S.; Keshishian, A.; Hamilton, M.; Horblyuk, R.; Gupta, K.; Luo, X.; Mardekian, J.; Friend, K.; Nadkarni, A.; et al. Effectiveness and safety of apixaban versus warfarin in non-valvular atrial fibrillation patients in “real-world” clinical practice: A propensity-matched analysis of 76,940 patients. Thromb. Haemost. 2017, 117, 1072–1082. [Google Scholar] [PubMed]
- Chan, Y.H.; Yen, K.C.; See, L.C.; Chang, S.-H.; Wu, L.-S.; Lee, H.-F.; Tu, H.-T.; Yeh, Y.-H.; Kuo, C.-T. Cardiovascular, Bleeding, and Mortality Risks of Dabigatran in Asians with Nonvalvular Atrial Fibrillation. Stroke 2016, 47, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.J.; Reichman, M.E.; Wernecke, M.; Zhang, R.; Southworth, M.-R.; Levenson, M.; Sheu, T.-C.; Mott, K.; Goulding, M.-R.; Houstoun, M.; et al. Cardiovascular, Bleeding, and Mortality Risks in Elderly Medicare Patients Treated with Dabigatran or Warfarin for Non-Valvular Atrial Fibrillation. Circulation 2015, 131, 157–164. [Google Scholar] [CrossRef]
- Hartling, L.; Milne, A.; Hamm, M.P.; VanderMeer, B.; Ansari, M.; Tsertsvadze, A.; Dryden, D.M. Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers. J. Clin. Epidemiol. 2013, 66, 982–993. [Google Scholar] [CrossRef]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef] [PubMed]
- Hylek, E.M.; Al-Khalidi, H.R.; Ansell, J.; Bahit, M.C.; Ezekowitz, J.A.; Geraldes, M.; Golitsyn, S.; Hermosillo, A.G.; Mohan, P.; Lewis, B.S.; et al. Apixaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus Warfarin in Nonvalvular Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef]
- Giugliano, R.P.; Ruff, C.T.; Braunwald, E.; Murphy, S.A.; Wiviott, S.D.; Halperin, J.L.; Waldo, A.L.; Ezekowitz, M.D.; Weitz, J.I.; Špinar, J.; et al. Edoxaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2013, 369, 2093–2104. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.D.; Heizer, G.; Aronson, R.; Vora, A.N.; Massaro, T.; Mehran, R.; Goodman, S.G.; Windecker, S.; Darius, H.; Li, J.; et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N. Engl. J. Med. 2019, 380, 1509–1524. [Google Scholar] [CrossRef]
- López-López, J.A.; Sterne, J.A.C.; Thom, H.H.Z.; Higgins, J.P.T.; Hingorani, A.D.; Okoli, G.N.; A Davies, P.; Bodalia, P.N.; A Bryden, P.; Welton, N.J.; et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: Systematic review, network meta-analysis, and cost effectiveness analysis. Br. Med. J. 2017, 359, j5058. [Google Scholar] [CrossRef]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Hoffman, E.B.; Deenadayalu, N.; Ezekowitz, M.D.; Camm, A.J.; I Weitz, J.; Lewis, B.S.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet 2014, 383, 955–962. [Google Scholar] [CrossRef]
- Ntaios, G.; Papavasileiou, V.; Diener, H.C.; Makaritsis, K.; Michel, P. Nonvitamin-K-antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and previous stroke or transient ischemic attack: An updated systematic review and meta-analysis of randomized controlled trials. Int. J. Stroke 2017, 12, 589–596. [Google Scholar] [CrossRef]
- Makam, R.C.P.; Hoaglin, D.C.; McManus, D.D.; Wang, V.; Gore, J.M.; Spencer, F.A.; Pradhan, R.; Tran, H.; Yu, H.; Goldberg, R.J. Efficacy and safety of direct oral anticoagulants approved for cardiovascular indications: Systematic review and meta-analysis. PLoS ONE 2018, 13, e0197583. [Google Scholar] [CrossRef]
- Cohen, D. Dabigatran: How the drug company withheld important analyses. Br. Med. J. 2014, 349, g4670. [Google Scholar] [CrossRef]
- Cohen, D. Rivaroxaban: Can we trust the evidence? Br. Med. J. 2016, 352, i575. [Google Scholar] [CrossRef]
- Eikelboom, J.W.; Wallentin, L.; Connolly, S.J.; Ezekowitz, M.; Healey, J.-S.; Oldgren, J.; Yang, S.; Alings, M.; Kaatz, S.; Hohnloser, S.-H.; et al. Risk of Bleeding With 2 Doses of Dabigatran Compared With Warfarin in Older and Younger Patients With Atrial Fibrillation: An analysis of the randomized evaluation of long-term anticoagulant therapy(RE-LY) trial. Circulation 2011, 123, 2363–2372. [Google Scholar] [CrossRef]
- Halperin, J.L.; Hankey, G.J.; Wojdyla, D.M.; Piccini, J.-P.; Lokhnygina, Y.; Patel, M.-R.; Breithardt, G.; Singer, D.-E.; Becker, R.-C.; Hacke, W.; et al. Efficacy and Safety of Rivaroxaban Compared with Warfarin Among Elderly Patients With Nonvalvular Atrial Fibrillation in the Rivaroxaban Once Daily, Oral, Direct Factor Xa Inhibition Compared With Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF). Circulation 2014, 130, 138–146. [Google Scholar]
- Kato, E.T.; Giugliano, R.P.; Ruff, C.T.; Koretsune, Y.; Yamashita, T.; Kiss, R.G.; Nordio, F.; Murphy, S.A.; Kimura, T.; Jin, J.; et al. Efficacy and Safety of Edoxaban in Elderly Patients with Atrial Fibrillation in the ENGAGE AF-TIMI 48 Trial. J. Am. Heart Assoc. 2016, 5, e003432. [Google Scholar] [CrossRef]
- Sharma, M.; Cornelius, V.R.; Patel, J.P.; Davies, J.G.; Molokhia, M. Efficacy and Harms of Direct Oral Anticoagulants in the Elderly for Stroke Prevention in Atrial Fibrillation and Secondary Prevention of Venous Thromboembolism. Circulation 2015, 132, 194–204. [Google Scholar] [CrossRef]
- Kim, I.S.; Kim, H.J.; Kim, T.H.; Uhm, J.-S.; Joung, B.; Lee, M.-H.; Pak, H.-N. Non-vitamin K antagonist oral anticoagulants have better efficacy and equivalent safety compared to warfarin in elderly patients with atrial fibrillation: A systematic review and meta-analysis. J. Cardiol. 2018, 72, 105–112. [Google Scholar] [CrossRef]
- Bai, Y.; Guo, S.D.; Deng, H.; Shantsila, A.; Fauchier, L.; Ma, C.-S.; Lip, G.Y. Effectiveness and safety of oral anticoagulants in older patients with atrial fibrillation: A systematic review and meta-regression analysis. Age Ageing 2018, 47, 9–17. [Google Scholar] [CrossRef]
- Almutairi, A.R.; Zhou, L.; Gellad, W.F.; Lee, J.K.; Slack, M.K.; Martin, J.R.; Lo-Ciganic, W.-H. Effectiveness and Safety of Non-vitamin K Antagonist Oral Anticoagulants for Atrial Fibrillation and Venous Thromboembolism: A Systematic Review and Meta-analyses. Clin. Ther. 2017, 39, 1456–1478. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Deng, H.; Shantsila, A.; Lip, G.Y. Rivaroxaban Versus Dabigatran or Warfarin in Real-World Studies of Stroke Prevention in Atrial Fibrillation: Systematic Review and Meta-Analysis. Stroke 2017, 48, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Shen, A.Y.; Yao, J.F.; Brar, S.S.; Jorgensen, M.B.; Chen, W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J. Am. Coll. Cardiol. 2007, 50, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.L.; Chiang, C.E. Optimal International Normalized Ratio for Atrial Fibrillation in Asians and Japanese. Circ. J. 2013, 77, 2242–2243. [Google Scholar] [CrossRef] [PubMed]

| Score per Modified NOS Domain | Total | Comments | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author, Year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| Lau, 2017 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 0 | 11 | |
| Halvorsen, 2017 | 2 | 1 | 2 | 0 | 2 | 1 | 2 | 0 | 10 | No demonstration that outcome was not present at start of study. |
| Li X, 2017 | 2 | 1 | 2 | 0 | 2 | 1 | 2 | 0 | 10 | No demonstration that outcome was not present at start of study. |
| Maura, 2015 | 2 | 1 | 1 | 0 | 2 | 1 | 2 | 1 | 10 | Intention to treat approach stated so exposure assumed to continue from index date until censored. No demonstration that outcome was not present at start of study. |
| Friberg, 2017 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 9 | Exposure monitoring after initial fill date not stated. No demonstration that outcome was not present at start of study. |
| Hernandez, 2015 | 1 | 1 | 2 | 0 | 2 | 1 | 2 | 0 | 9 | Used a 5% sample of Medicare patients, so unclear how representative of US population as a whole. No demonstration that outcome was not present at start of study. |
| Chan YH, 2016 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 8 | Exposure monitoring after initial fill date not stated. No demonstration that outcome was not present at start of study. |
| Forslund, 2017 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 8 | No demonstration that outcome was not present at start of study. |
| Lauffenburger, 2015 | 1 | 1 | 1 | 0 | 2 | 1 | 2 | 0 | 8 | Commercially insured population may not be truly representative of average US population. Exposure monitoring after initial fill date not stated. No demonstration that outcome was not present at start of study |
| Nielsen, 2017 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 8 | Exposure monitoring after initial fill date not stated. No demonstration that outcome was not present at start of study. |
| Nishtala, 2016 | 1 | 1 | 2 | 0 | 2 | 1 | 1 | 0 | 8 | Only includes patients with a hospital admission in the 5 years prior to study entry, so potentially represents sicker patients than in the average population. No demonstration that outcome was not present at start of study. |
| Norby, 2017 | 1 | 1 | 1 | 0 | 2 | 1 | 2 | 0 | 8 | Exposure monitoring after initial fill date not stated. No demonstration that outcome was not present at start of study. |
| Seeger, 2015 | 1 | 1 | 2 | 0 | 2 | 1 | 1 | 0 | 8 | Predominantly commercially insured patients only, so may not be truly representative of average US population. No demonstration that outcome was not present at start of study. |
| Abraham, 2015 | 1 | 1 | 2 | 0 | 2 | 1 | 0 | 0 | 7 | Does not include Medicare patients, so may not represent older population well. Length of follow-up not stated, so unclear if long enough for outcomes to occur. No demonstration that outcome was not present at start of study. |
| Adeboyeje, 2017 | 1 | 1 | 2 | 0 | 2 | 1 | 0 | 0 | 7 | Commercially insured patients only, so may not be truly representative of average US population. No demonstration that outcome was not present at start of study. |
| Avgil-Tsadok, 2016 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 7 | Only represents patients diagnosed with AF as inpatients, so may not be truly representative. No demonstration that outcome was not present at start of study. |
| Bengtson, 2017 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 7 | Exposure monitoring after initial fill date not stated. No demonstration that outcome was not present at start of study. |
| Cha, 2017 | 2 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 7 | Intention to treat approach stated, so exposure assumed to continue from index date until censored. Propensity score used in analysis to adjust for confounders. However, it seems to include CHADS2-VASC2 score as the only variable. |
| Go, 2017 | 1 | 1 | 2 | 0 | 2 | 1 | 0 | 0 | 7 | Predominantly privately insured population, so may not represent average US population. |
| Graham, 2014 | 1 | 1 | 2 | 0 | 2 | 1 | 0 | 0 | 7 | Included only Medicare patients, so may not represent average US population. Follow-up duration not explicitly stated. However, sensitivity analysis for different lengths of follow-up did not affect results. |
| Kwon, 2016 | 0 | 1 | 1 | 0 | 0 | 2 | 1 | 0 | 5 | Data from one hospital only. No description of how exposure was measured. Limited attempts to control for confounding. No demonstration that outcome was not present at start of study. |
| Chan PH, 2016 | 0 | 1 | 0 | 0 | 0 | 1 | 2 | 0 | 4 | Data from one hospital only. No description of how exposure was measured. Limited attempts to control for confounding. |
| Modified Newcastle–Ottawa scale (NOS) domains: | ||||||||||
| Selection 1. Representativeness of the exposed cohort 2. Selection of the non-exposed cohort 3. Ascertainment of exposure 4. Demonstration that outcome of interest was not present at start of study | Comparability 5. Comparability of cohorts on the basis of the design or analysis | Outcome 6. Assessment of outcome 7. Was follow-up long enough for outcomes to occur 8. Adequacy of follow-up of cohorts | ||||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitchell, A.; Watson, M.C.; Welsh, T.; McGrogan, A. Effectiveness and Safety of Direct Oral Anticoagulants versus Vitamin K Antagonists for People Aged 75 Years and over with Atrial Fibrillation: A Systematic Review and Meta-Analyses of Observational Studies. J. Clin. Med. 2019, 8, 554. https://doi.org/10.3390/jcm8040554
Mitchell A, Watson MC, Welsh T, McGrogan A. Effectiveness and Safety of Direct Oral Anticoagulants versus Vitamin K Antagonists for People Aged 75 Years and over with Atrial Fibrillation: A Systematic Review and Meta-Analyses of Observational Studies. Journal of Clinical Medicine. 2019; 8(4):554. https://doi.org/10.3390/jcm8040554
Chicago/Turabian StyleMitchell, Anneka, Margaret C. Watson, Tomas Welsh, and Anita McGrogan. 2019. "Effectiveness and Safety of Direct Oral Anticoagulants versus Vitamin K Antagonists for People Aged 75 Years and over with Atrial Fibrillation: A Systematic Review and Meta-Analyses of Observational Studies" Journal of Clinical Medicine 8, no. 4: 554. https://doi.org/10.3390/jcm8040554
APA StyleMitchell, A., Watson, M. C., Welsh, T., & McGrogan, A. (2019). Effectiveness and Safety of Direct Oral Anticoagulants versus Vitamin K Antagonists for People Aged 75 Years and over with Atrial Fibrillation: A Systematic Review and Meta-Analyses of Observational Studies. Journal of Clinical Medicine, 8(4), 554. https://doi.org/10.3390/jcm8040554





