Impact of Bariatric Surgery on Post-Transplant Outcomes in Solid Organ Recipients: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Study Group Definitions
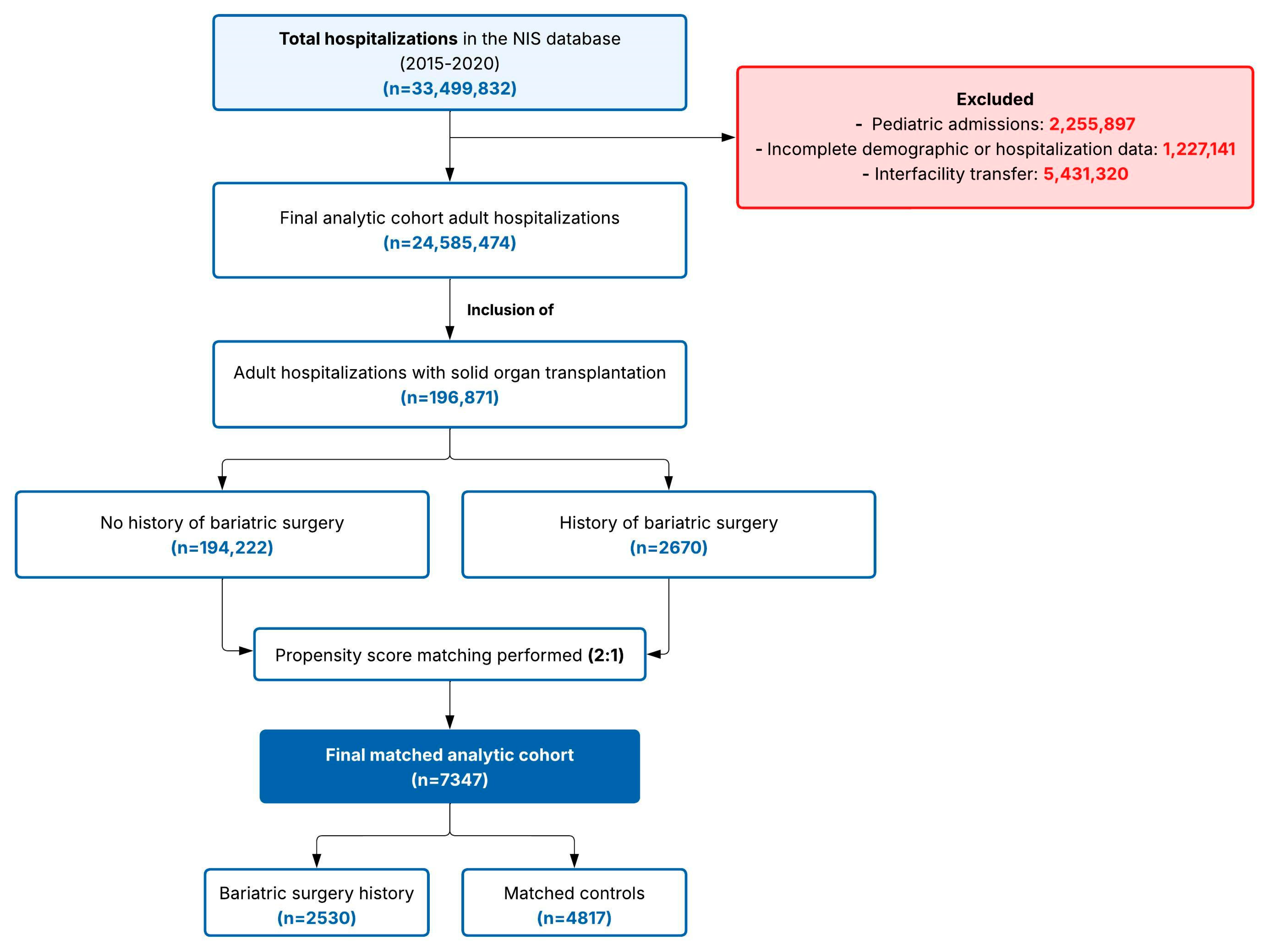
2.3. Inclusion and Exclusion Criteria
2.4. Covariates
2.5. Outcomes
2.6. Propensity Score Matching
2.7. Statistical Analysis
2.8. Ethical Considerations
3. Results
3.1. Study Population and Propensity Score Matching
3.2. Baseline Characteristics of the Matched Cohort
3.3. Comorbidity Comparison
3.4. Hospitalization Outcomes
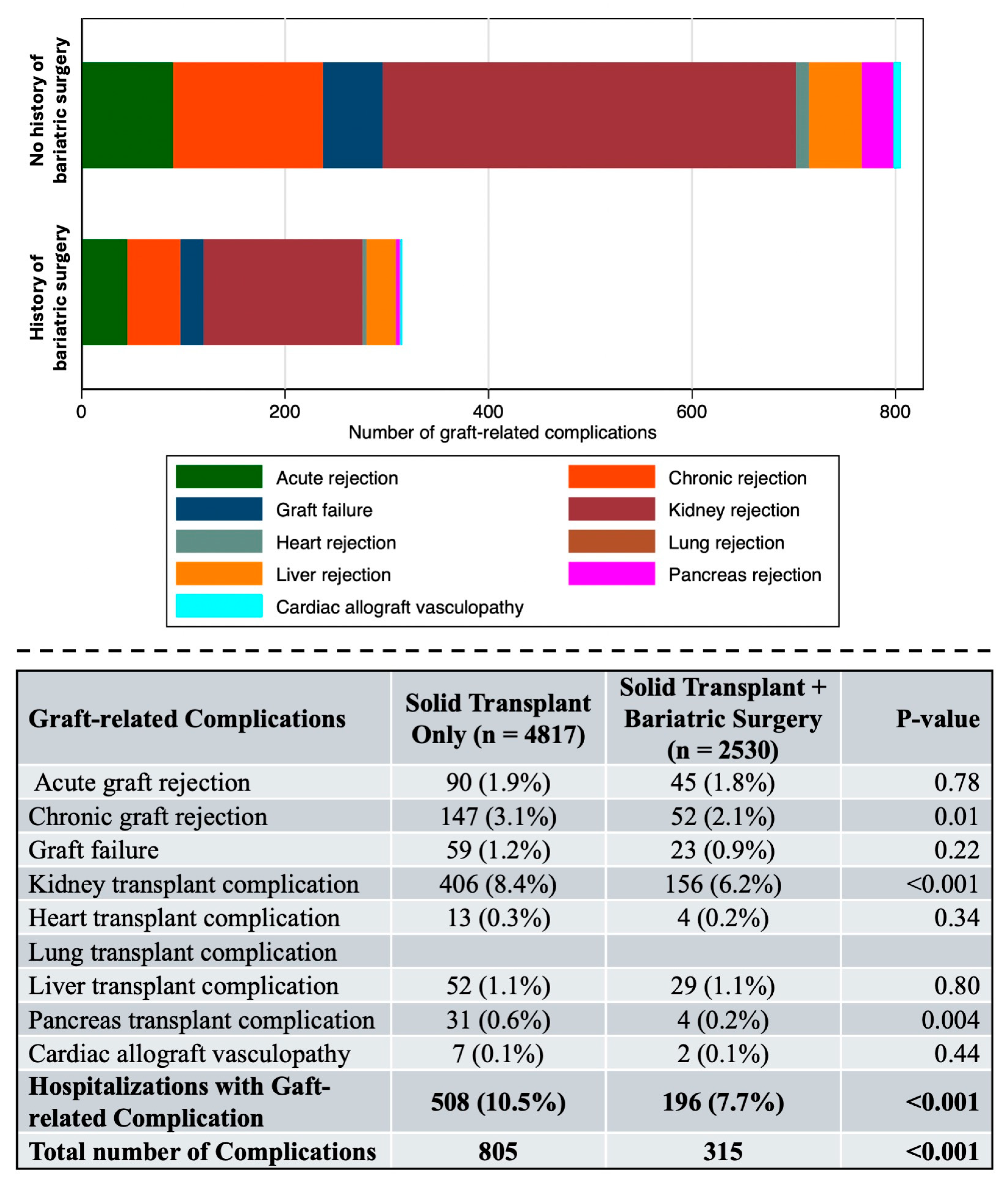
3.5. Graft-Related Complications
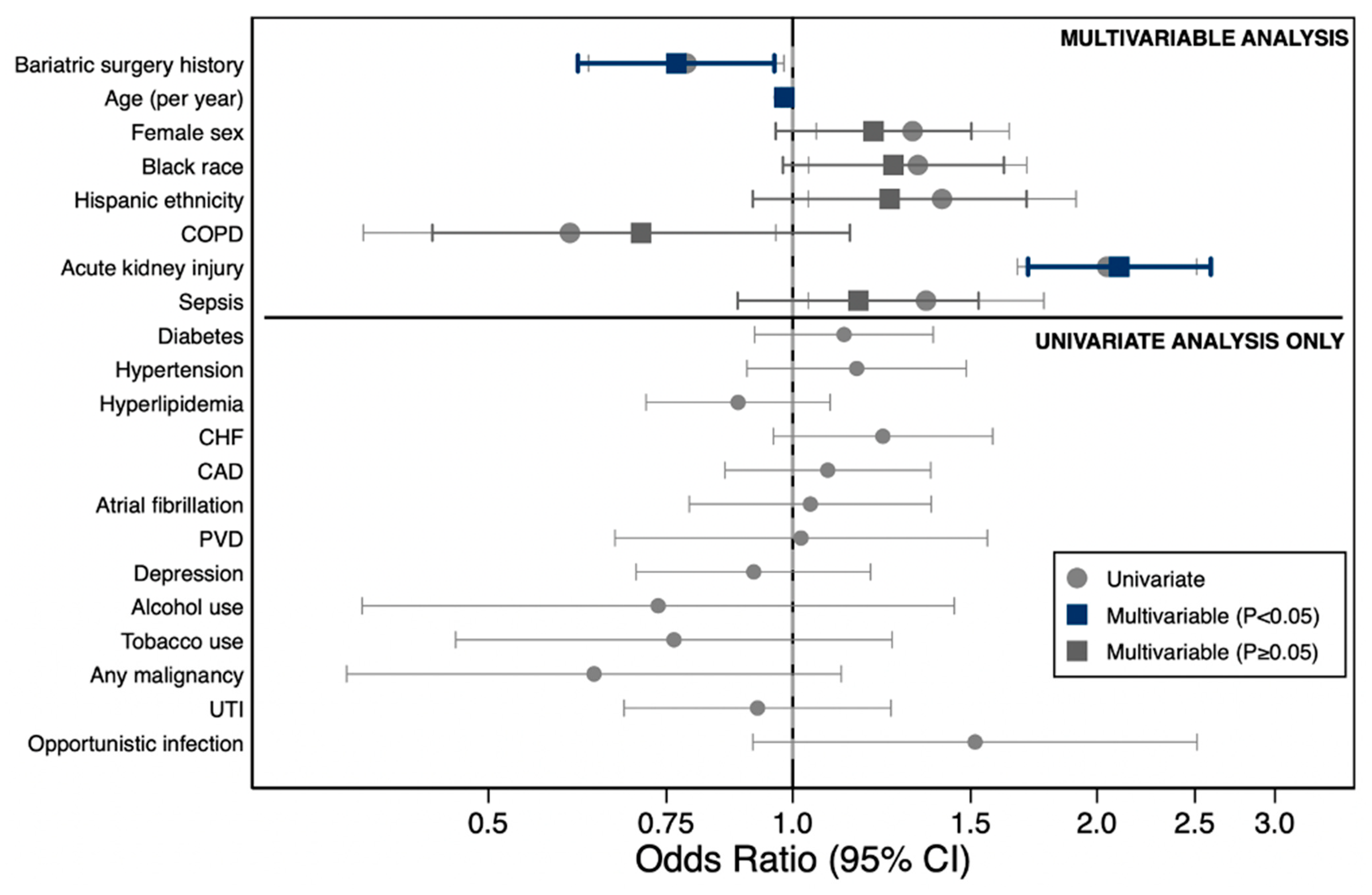
3.6. Predictors of Graft-Related Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHRQ | Agency for Healthcare Research and Quality |
| AUC | area under the concentration–time curve |
| BMI | body mass index |
| CCI | Charlson Comorbidity Index |
| CI | confidence interval |
| CM | clinical modification |
| COPD | chronic obstructive pulmonary disease |
| HCUP | Healthcare Cost and Utilization Project |
| ICD-10-CM | International Classification of Diseases, Tenth Revision, Clinical Modification |
| ICD-10-PCS | International Classification of Diseases, Tenth Revision, Procedure Coding System |
| KT | kidney transplantation |
| LOS | length of stay |
| LVEF | left ventricular ejection fraction |
| NIS | Nationwide Inpatient Sample |
| OR | odds ratio |
| PCS | Procedure Coding System |
| RYGB | Roux-en-Y gastric bypass |
| SD | standard deviation |
| SG | sleeve gastrectomy |
| SMD | standardized mean difference |
| US | United States |
| WTP | willingness to pay |
References
- GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar]
- Ghanem, O.M.; Pita, A.; Nazzal, M.; Johnson, S.; Diwan, T.; Obeid, N.R.; Croome, K.P.; Lim, R.; Quintini, C.; Whitson, B.A.; et al. Obesity, organ failure, and transplantation: A review of the role of metabolic and bariatric surgery in transplant candidates and recipients. Surg. Endosc. 2024, 38, 4138–4151. [Google Scholar] [CrossRef]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose tissue and insulin resistance in obese. Biomed. Pharmacother. 2021, 137, 111315. [Google Scholar] [CrossRef]
- Pierpont, Y.N.; Dinh, T.P.; Salas, R.E.; Johnson, E.L.; Wright, T.G.; Robson, M.C.; Payne, W.G. Obesity and surgical wound healing: A current review. ISRN Obes. 2014, 2014, 638936. [Google Scholar] [CrossRef]
- Schuette, H.B.; Durkin, W.M.; Passias, B.J.; DeGenova, D.; Bertolini, C.; Myers, P.; Taylor, B.C. The Effect of Obesity on Operative Time and Postoperative Complications for Peritrochanteric Femur Fractures. Cureus 2020, 12, e11720. [Google Scholar] [CrossRef]
- Hall, J.I. Obesity—A reluctance to treat? Obes. Facts 2010, 3, 79–80. [Google Scholar] [CrossRef] [PubMed]
- Phelan, S.M.; Burgess, D.J.; Yeazel, M.W.; Hellerstedt, W.L.; Griffin, J.M.; van Ryn, M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes. Rev. 2015, 16, 319–326. [Google Scholar] [CrossRef]
- Gill, J.S.; Lan, J.; Dong, J.; Rose, C.; Hendren, E.; Johnston, O.; Gill, J. The survival benefit of kidney transplantation in obese patients. Am. J. Transplant. 2013, 13, 2083–2090. [Google Scholar] [CrossRef]
- Freitas, W.R., Jr.; Oliveira, L.V.F.; Perez, E.A.; Ilias, E.J.; Lottenberg, C.P.; Silva, A.S.; Urbano, J.J.; Oliveira, M.C., Jr.; Vieira, R.P.; Ribeiro-Alves, M.; et al. Systemic inflammation in severe obese patients undergoing surgery for obesity and weight-related diseases. Obes. Surg. 2018, 28, 1931–1942. [Google Scholar] [CrossRef] [PubMed]
- Larson, E.L.; Ellias, S.D.; Blezek, D.J.; Klug, J.; Hartman, R.P.; Ziller, N.F.; Bamlet, H.; Mao, S.A.; Perry, D.K.; Nimma, I.R.; et al. Simultaneous liver transplant and sleeve gastrectomy provides durable weight loss, improves metabolic syndrome and reduces allograft steatosis. J. Hepatol. 2025, 83, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Puttarajappa, C.M.; Smith, K.J.; Ahmed, B.H.; Bernardi, K.; Lavenburg, L.-M.; Hoffman, W.; Molinari, M. Economic evaluation of weight loss and transplantation strategies for kidney transplant candidates with obesity. Am. J. Transplant. 2024, 24, 2212–2224. [Google Scholar] [CrossRef] [PubMed]
- Iannelli, A.; Bulsei, J.; Debs, T.; Tran, A.; Lazzati, A.; Gugenheim, J.; Anty, R.; Petrucciani, N.; Fontas, E. Clinical and economic impact of previous bariatric surgery on liver transplantation: A nationwide, population-based retrospective study. Obes. Surg. 2022, 32, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Cucchiari, D.; Podestà, M.A.; Ponticelli, C. Pathophysiology of rejection in kidney transplantation. Expert Rev. Clin. Immunol. 2024, 20, 1471–1481. [Google Scholar] [CrossRef]
- Cohen, J.B.; Lim, M.A.; Tewksbury, C.M.; Torres-Landa, S.; Trofe-Clark, J.; Abt, P.L.; Williams, N.N.; Dumon, K.R.; Goral, S. Bariatric surgery before and after kidney transplantation: Long-term weight loss and allograft outcomes. Surg. Obes. Relat. Dis. 2019, 15, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Jung, A.D.; Dhar, V.K.; Tadros, J.S.; Schauer, D.P.; Smith, E.P.; Hanseman, D.J.; Cuffy, M.C.; Alloway, R.R.; Shields, A.R.; et al. Laparoscopic sleeve gastrectomy improves renal transplant candidacy and posttransplant outcomes in morbidly obese patients. Am. J. Transplant. 2018, 18, 410–416. [Google Scholar] [CrossRef]
- Quante, M.; Iske, J.; Uehara, H.; Minami, K.; Nian, Y.; Maenosono, R.; Matsunaga, T.; Liu, Y.; Azuma, H.; Perkins, D.; et al. Taurodeoxycholic acid and valine reverse obesity-associated augmented alloimmune responses and prolong allograft survival. Am. J. Transplant. 2022, 22, 402–413. [Google Scholar] [CrossRef]
- Fagenson, A.M.; Mazzei, M.; Swaszek, L.; Edwards, M.A. Is bariatric procedure type associated with morbidity in transplant patients? J. Surg. Res. 2022, 273, 172–180. [Google Scholar] [CrossRef]
- Zevallos, A.; Cornejo, J.; Sarmiento, J.; Shojaeian, F.; Mokhtari-Esbuie, F.; Adrales, G.; Li, C.; Sebastian, R. Outcomes of Sleeve Gastrectomy in Patients with Organ Transplant-Related Immunosuppression. J. Surg. Res. 2024, 300, 253–262. [Google Scholar] [CrossRef]
- Yemini, R.; Nesher, E.; Winkler, J.; Carmeli, I.; Azran, C.; Ben David, M.; Mor, E.; Keidar, A. Bariatric surgery in solid organ transplant patients: Long-term follow-up results of outcome, safety, and effect on immunosuppression. Am. J. Transplant. 2018, 18, 2772–2780. [Google Scholar] [CrossRef]
- Humięcka, M.; Sawicka, A.; Kędzierska, K.; Binda, A.; Jaworski, P.; Tarnowski, W.; Jankowski, P. Prevalence of nutrient deficiencies following bariatric surgery-long-term, prospective observation. Nutrients 2025, 17, 2599. [Google Scholar] [CrossRef]
- Obinwanne, K.M.; Fredrickson, K.A.; Mathiason, M.A.; Kallies, K.J.; Farnen, J.P.; Kothari, S.N. Incidence, treatment, and outcomes of iron deficiency after laparoscopic Roux-en-Y gastric bypass: A 10-year analysis. J. Am. Coll. Surg. 2014, 218, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Sarno, G.; Nappi, R.; Altieri, B.; Tirabassi, G.; Muscogiuri, E.; Salvio, G.; Paschou, S.A.; Ferrara, A.; Russo, E.; Vicedomini, D.; et al. Current evidence on vitamin D deficiency and kidney transplant: What’s new? Rev. Endocr. Metab. Disord. 2017, 18, 323–334. [Google Scholar] [CrossRef]
- Mirzakhani, M.; Mohammadkhani, S.; Hekmatirad, S.; Aghapour, S.; Gorjizadeh, N.; Shahbazi, M.; Mohammadnia-Afrouzi, M. The association between vitamin D and acute rejection in human kidney transplantation: A systematic review and meta-analysis study. Transpl. Immunol. 2021, 67, 101410. [Google Scholar] [CrossRef]
- Mechanick, J.I.; Apovian, C.; Brethauer, S.; Garvey, W.T.; Joffe, A.M.; Kim, J.; Kushner, R.F.; Lindquist, R.; Pessah-Pollack, R.; Seger, J.; et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures—2019 update: Cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg. Obes. Relat. Dis. 2020, 16, 175–247. [Google Scholar]
- Parrott, J.; Frank, L.; Rabena, R.; Craggs-Dino, L.; Isom, K.A.; Greiman, L. American Society for Metabolic and bariatric surgery integrated health nutritional guidelines for the surgical weight loss patient 2016 update: Micronutrients. Surg. Obes. Relat. Dis. 2017, 13, 727–741. [Google Scholar] [CrossRef] [PubMed]
- Sierra, L.; Aitharaju, V.; Prado, R.; Cymbal, M.; Chaterjee, A.; Khurana, A.; Patel, R.; Firkins, S.; Simons-Linares, R. In-Hospital Outcomes of Bariatric Surgery in People Living with HIV: A Nationwide Analysis. Obes. Surg. 2025, 35, 3111–3119. [Google Scholar] [CrossRef]
- Steenackers, N.; Vanuytsel, T.; Augustijns, P.; Tack, J.; Mertens, A.; Lannoo, M.; Van der Schueren, B.; Matthys, C. Adaptations in gastrointestinal physiology after sleeve gastrectomy and Roux-en-Y gastric bypass. Lancet Gastroenterol. Hepatol. 2021, 6, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Angeles, P.C.; Robertsen, I.; Seeberg, L.T.; Krogstad, V.; Skattebu, J.; Sandbu, R.; Åsberg, A.; Hjelmesæth, J. The influence of bariatric surgery on oral drug bioavailability in patients with obesity: A systematic review. Obes. Rev. 2019, 20, 1299–1311. [Google Scholar] [CrossRef]
- Rogers, C.C.; Alloway, R.R.; Alexander, J.W.; Cardi, M.; Trofe, J.; Vinks, A.A. Pharmacokinetics of mycophenolic acid, tacrolimus and sirolimus after gastric bypass surgery in end-stage renal disease and transplant patients: A pilot study. Clin. Transplant. 2008, 22, 281–291. [Google Scholar] [CrossRef]
- Friedman, A.N.; Wolfe, B. Is Bariatric Surgery an Effective Treatment for Type II Diabetic Kidney Disease? Clin. J. Am. Soc. Nephrol. 2016, 11, 528–535. [Google Scholar] [CrossRef]
- Lee, Y.; Tian, C.; Lovrics, O.; Soon, M.S.; Doumouras, A.G.; Anvari, M.; Hong, D. Bariatric surgery before, during, and after liver transplantation: A systematic review and meta-analysis. Surg. Obes. Relat. Dis. 2020, 16, 1336–1347. [Google Scholar] [CrossRef] [PubMed]
- Esparham, A.; Mehri, A.; Hadian, H.; Taheri, M.; Moghadam, H.A.; Kalantari, A.; Fogli, M.J.; Khorgami, Z. The Effect of Bariatric Surgery on Patients with Heart Failure: A Systematic Review and Meta-analysis. Obes. Surg. 2023, 33, 4125–4136. [Google Scholar] [CrossRef] [PubMed]
| Before Propensity Score Matching | After Propensity Score Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Solid Transplant Only | Solid Transplant + Bariatric | p | SMD | Solid Transplant Only | Solid Transplant + Bariatric | p | SMD |
| n | 194,232 (98.6) | 2670 (1.4) | 4817 (65.6) | 2530 (34.4) | ||||
| Age, years, mean (SD) | 57.7 (15.4) | 55.6 (11.3) | <0.001 | −0.15 | 56.3 (13.9) | 55.6 (11.3) | 0.041 | −0.05 |
| Length of stay, days, mean (SD) | 6.2 (9.3) | 5.5 (6.3) | <0.001 | −0.09 | 5.3 (5.2) | 5.5 (6.3) | <0.001 | 0.11 |
| Total hospitalization charge, USD, mean (SD) | 90,716 (204,672) | 75,464 (139,219) | <0.001 | −0.09 | 70,722 (142,375) | 75,486 (140,059) | 0.17 | 0.03 |
| Sex | <0.001 | 0.43 | 0.20 | −0.03 | ||||
| Female | 113,606 (58.5) | 997 (37.3) | 1732 (36.0) | 948 (37.5) | ||||
| Male | 80,588 (41.5) | 1673 (62.7) | 3085 (64.0) | 1582 (62.5) | ||||
| Race/ethnicity | <0.001 | −0.13 | <0.001 | 0.09 | ||||
| White | 113,178 (60.3) | 1618 (63.0) | 3271 (67.9) | 1600 (63.2) | ||||
| Black | 35,260 (18.8) | 560 (21.8) | 885 (18.4) | 554 (21.9) | ||||
| Hispanic | 25,704 (13.7) | 293 (11.4) | 517 (10.7) | 285 (11.3) | ||||
| Asian | 6582 (3.5) | 26 (1.0) | 79 (1.6) | 24 (0.9) | ||||
| Native American | 1488 (0.8) | 12 (0.5) | 15 (0.3) | 10 (0.4) | ||||
| Other | 5557 (3.0) | 58 (2.3) | 50 (1.0) | 57 (2.3) | ||||
| Median household income quartile, USD | <0.001 | 0.09 | 0.504 | 0.04 | ||||
| 1–24,999 | 52,451 (27.4) | 595 (22.6) | 1175 (24.4) | 580 (22.9) | ||||
| 25,000–34,999 | 49,010 (25.6) | 709 (26.9) | 1295 (26.9) | 678 (26.8) | ||||
| 35,000–44,999 | 48,452 (25.3) | 713 (27.1) | 1264 (26.2) | 681 (26.9) | ||||
| 45,000 or more | 41,369 (21.6) | 614 (23.3) | 1083 (22.5) | 591 (23.4) | ||||
| Charlson Comorbidity Index, mean (SD) | 3.6 (2.0) | 3.3 (1.9) | <0.001 | −0.15 | 3.3 (1.8) | 3.3 (1.8) | 0.94 | <0.001 |
| Hospital region | <0.001 | −0.03 | <0.001 | 0.05 | ||||
| Northeast | 37,361 (19.2) | 437 (16.4) | 970 (20.1) | 427 (16.9) | ||||
| Midwest | 45,135 (23.2) | 783 (29.3) | 1196 (24.8) | 705 (27.9) | ||||
| South | 73,398 (37.8) | 981 (36.7) | 1839 (38.2) | 945 (37.4) | ||||
| West | 38,338 (19.7) | 469 (17.6) | 812 (16.9) | 453 (17.9) | ||||
| Organ type | ||||||||
| Kidney | 115,889 (59.7) | 1687 (63.2) | <0.001 | 0.07 | 2924 (60.7) | 1609 (63.6) | 0.16 | 0.06 |
| Heart | 16,929 (8.7) | 249 (9.3) | 0.27 | 0.02 | 383 (8.0) | 236 (9.3) | 0.40 | 0.05 |
| Lung | 10,851 (5.6) | 83 (3.1) | <0.001 | −0.12 | 274 (5.7) | 78 (3.1) | 0.06 | −0.13 |
| Liver | 51,794 (26.7) | 699 (26.2) | 0.58 | −0.01 | 1254 (26.0) | 657 (26.0) | 0.95 | 0 |
| Pancreas | 12,900 (6.6) | 110 (4.1) | <0.001 | −0.11 | 381 (7.9) | 105 (4.2) | <0.001 | −0.16 |
| Comorbidity | No Bariatric Surgery (n = 4817) | Bariatric Surgery (n = 2530) | p Value | SMD |
|---|---|---|---|---|
| Coronary artery disease | 1217 (25.3) | 527 (20.8) | <0.001 | −0.11 |
| Congestive heart failure | 924 (19.2) | 400 (15.8) | <0.001 | −0.09 |
| Peripheral vascular disease | 305 (6.3) | 135 (5.3) | 0.09 | −0.04 |
| Chronic obstructive pulmonary disease | 397 (8.2) | 162 (6.4) | 0.01 | −0.07 |
| Chronic kidney disease | 2651 (55.0) | 1335 (52.8) | 0.06 | −0.05 |
| Liver disease | 166 (3.4) | 94 (3.7) | 0.55 | 0.01 |
| Diabetes mellitus | 2339 (48.6) | 1262 (49.9) | 0.28 | 0.03 |
| Obesity | 1402 (29.1) | 733 (29.0) | 0.10 | 0.01 |
| Hypertension | 3738 (77.6) | 1906 (75.3) | 0.03 | −0.05 |
| Hyperlipidemia | 1959 (40.7) | 987 (39.0) | 0.17 | −0.03 |
| Atrial fibrillation | 765 (15.9) | 391 (15.5) | 0.63 | −0.01 |
| Depression | 801 (16.6) | 578 (22.8) | <0.001 | 0.16 |
| Alcohol use disorder | 103 (2.1) | 120 (4.7) | <0.001 | 0.14 |
| Tobacco use | 275 (5.7) | 130 (5.1) | 0.31 | −0.03 |
| Steroid use | 733 (15.2) | 443 (17.5) | 0.07 | 0.1 |
| Any malignancy | 253 (5.3) | 114 (4.5) | 0.16 | −0.03 |
| Acute kidney injury | 1543 (32.0) | 822 (32.5) | 0.69 | 0.01 |
| Urinary tract infection | 653 (13.6) | 343 (13.6) | 1.00 | <0.001 |
| Sepsis | 695 (14.4) | 316 (12.5) | 0.02 | −0.06 |
| Opportunistic infection | 131 (2.7) | 87 (3.4) | 0.08 | 0.04 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Variable | OR (95% CI) | p Value | OR (95% CI) | p Value |
| Bariatric surgery history | 0.78 (0.62–0.98) | 0.01 | 0.77 (0.61–0.96) | 0.02 |
| Age (per year) | 0.98 (0.97–0.99) | <0.001 | 0.98 (0.97–0.99) | <0.001 |
| Female sex | 1.31 (1.05–1.64) | 0.015 | 1.20 (0.96–1.50) | 0.11 |
| Race/ethnicity | ||||
| White | Reference | Reference | ||
| Black | 1.33 (1.04–1.70) | 0.02 | 1.26 (0.98–1.62) | 0.074 |
| Hispanic | 1.41 (1.04–1.91) | 0.03 | 1.25 (0.91–1.70) | 0.165 |
| Asian | 1.20 (0.52–2.77) | 0.66 | — | — |
| Other | 0.76 (0.28–2.07) | 0.59 | — | — |
| Diabetes mellitus | 1.12 (0.92–1.38) | 0.26 | — | — |
| Hypertension | 1.16 (0.90–1.48) | 0.25 | — | — |
| Hyperlipidemia | 0.88 (0.72–1.09) | 0.25 | — | — |
| Congestive heart failure | 1.23 (0.96–1.58) | 0.11 | — | — |
| Coronary artery disease | 1.08 (0.86–1.37) | 0.51 | — | — |
| COPD | 0.60 (0.38–0.96) | 0.03 | 0.71 (0.44–1.14) | 0.154 |
| Atrial fibrillation | 1.04 (0.79–1.37) | 0.78 | — | — |
| Peripheral vascular disease | 1.02 (0.67–1.56) | 0.93 | — | — |
| Depression | 0.91 (0.70–1.19) | 0.51 | — | — |
| Alcohol use disorder | 0.74 (0.37–1.45) | 0.37 | — | — |
| Tobacco use | 0.76 (0.46–1.25) | 0.29 | — | — |
| Acute kidney injury | 2.05 (1.67–2.51) | <0.001 | 2.10 (1.71–2.59) | <0.001 |
| Any malignancy | 0.64 (0.36–1.12) | 0.12 | — | — |
| Urinary tract infection | 0.92 (0.68–1.25) | 0.61 | — | — |
| Sepsis | 1.35 (1.04–1.77) | 0.03 | 1.16 (0.88–1.53) | 0.287 |
| Opportunistic infection | 1.51 (0.91–2.51) | 0.11 | — | — |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Sierra, L.; Bahierathan, K.; Abad, M.O.; Khurana, A.; Chatterjee, A.; Patel, R.; Firkins, S.; Simons-Linares, R. Impact of Bariatric Surgery on Post-Transplant Outcomes in Solid Organ Recipients: A Retrospective Cohort Study. J. Clin. Med. 2026, 15, 954. https://doi.org/10.3390/jcm15030954
Sierra L, Bahierathan K, Abad MO, Khurana A, Chatterjee A, Patel R, Firkins S, Simons-Linares R. Impact of Bariatric Surgery on Post-Transplant Outcomes in Solid Organ Recipients: A Retrospective Cohort Study. Journal of Clinical Medicine. 2026; 15(3):954. https://doi.org/10.3390/jcm15030954
Chicago/Turabian StyleSierra, Leandro, Kanisha Bahierathan, Maria Ortega Abad, Akash Khurana, Arjun Chatterjee, Roma Patel, Stephen Firkins, and Roberto Simons-Linares. 2026. "Impact of Bariatric Surgery on Post-Transplant Outcomes in Solid Organ Recipients: A Retrospective Cohort Study" Journal of Clinical Medicine 15, no. 3: 954. https://doi.org/10.3390/jcm15030954
APA StyleSierra, L., Bahierathan, K., Abad, M. O., Khurana, A., Chatterjee, A., Patel, R., Firkins, S., & Simons-Linares, R. (2026). Impact of Bariatric Surgery on Post-Transplant Outcomes in Solid Organ Recipients: A Retrospective Cohort Study. Journal of Clinical Medicine, 15(3), 954. https://doi.org/10.3390/jcm15030954






