Intraoperative Suction-Assisted Kyphoplasty for Immediate Removal of Posterior PMMA Extravasation in Decompressed Vertebral Compression Fractures
Abstract
1. Introduction
2. Materials and Methods
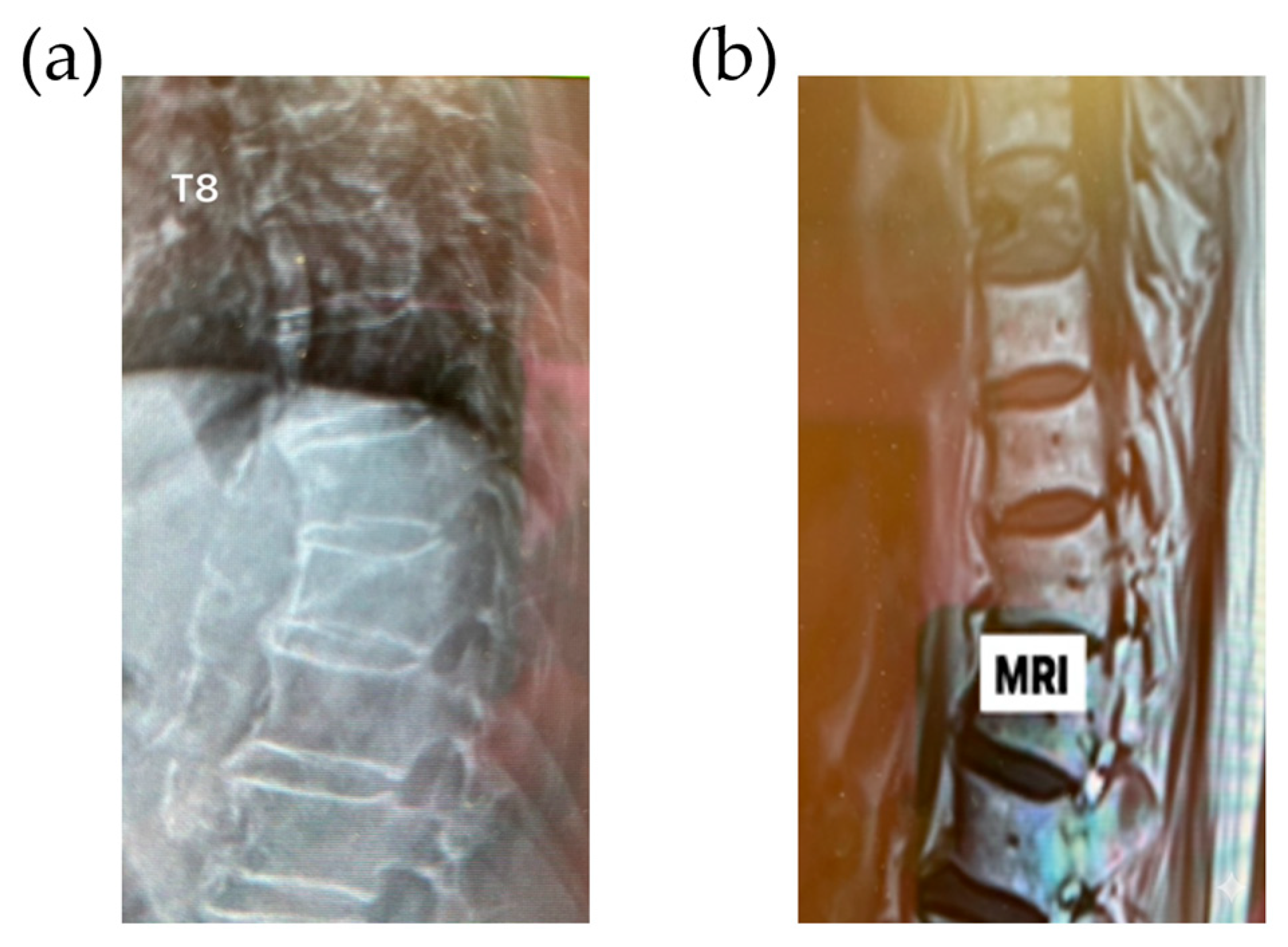
2.1. Patient History and Evaluation
2.2. Surgical Technique
- Left pedicle (Injection Portal): Primarily used for cement injection, aided by differential pressure to facilitate controlled delivery.
- Right pedicle (Venting Portal): Connected to continuous aspiration via a vacuum pump (DF-650, Doctor’s Friend Medical Instrument, Taichung, Taiwan) during the initial filling phase.
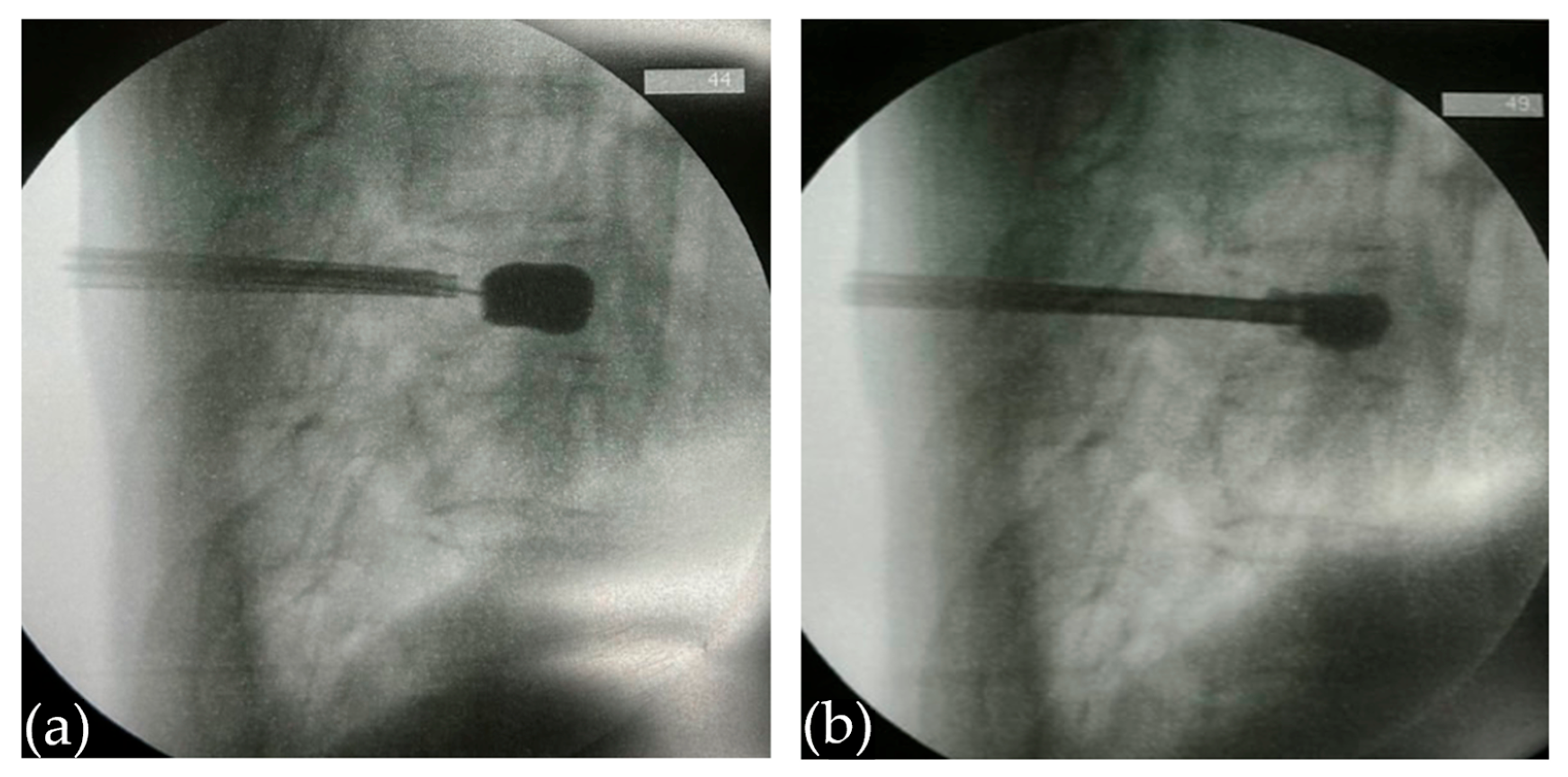
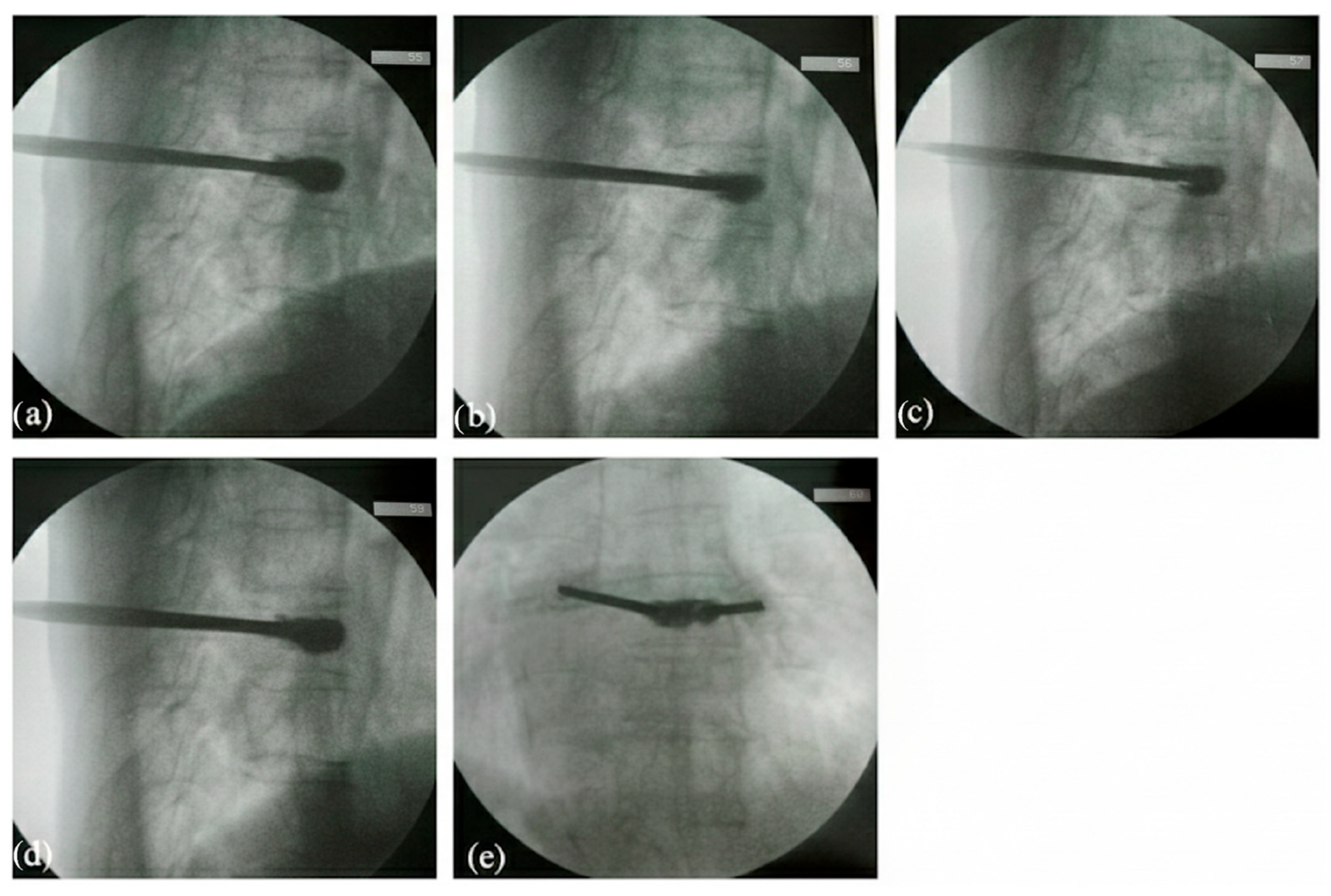
2.2.1. Creation of a Vertebral Cavity
2.2.2. Cement Preparation and Initial Injection
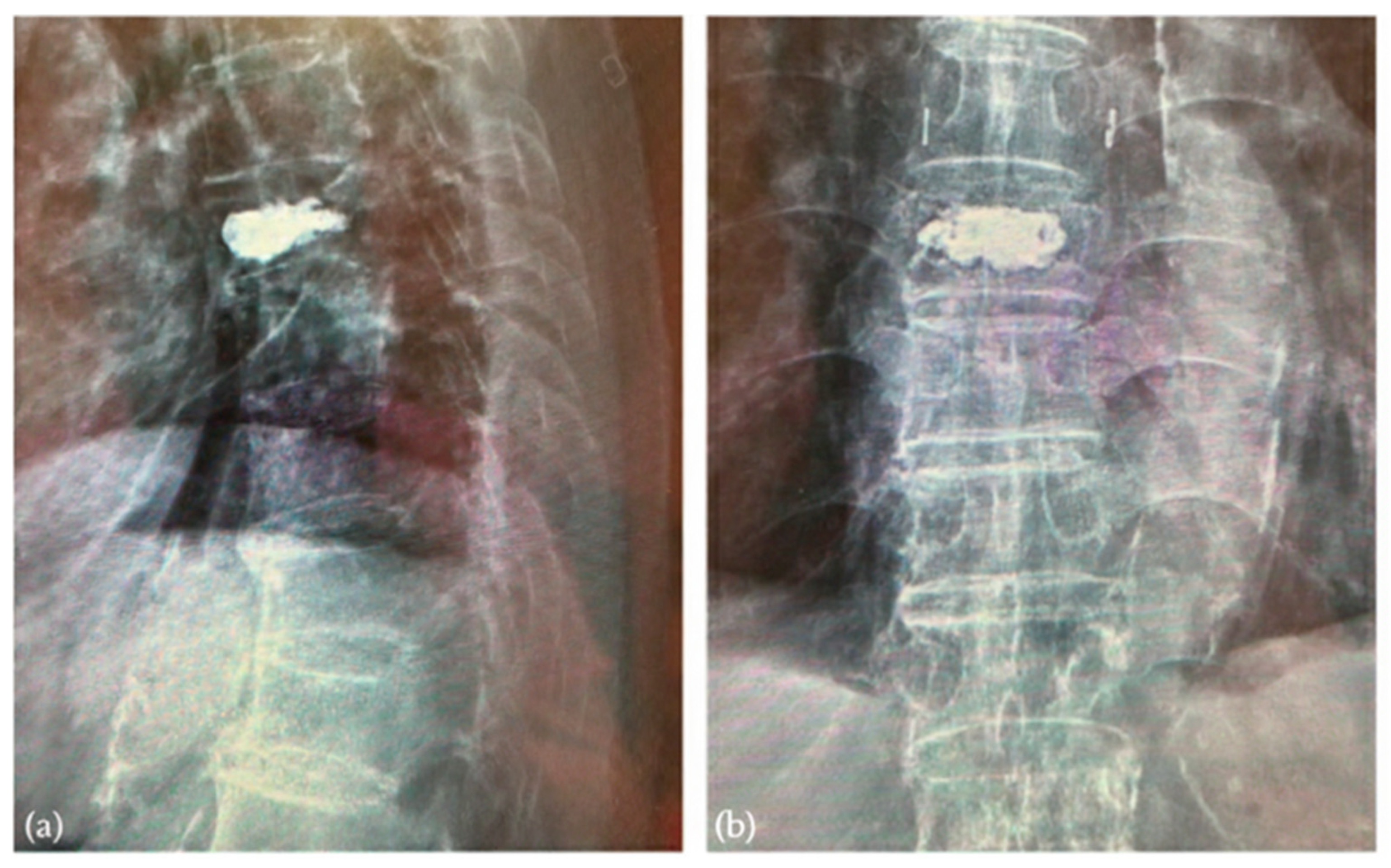
3. Results
3.1. Surveillance of Cement Leakage
3.2. Decompression Maneuver
3.3. Postoperative Clinical and Radiographic Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gao, H.; Huang, J.; Wei, Q.; He, C. Advances in animal models for studying bone fracture healing. Bioengineering 2023, 10, 201. [Google Scholar] [CrossRef]
- Albrecht, A.P.; Kistler-Fischbacher, M.; De Godoi Rezende Costa Molino, C.; Armbrecht, G.; Freystaetter, G.; Theiler, R.; Kressig, R.W.; Da Silva, J.A.; Rizzoli, R.; Wanner, G.A. Prevalence and incidence of osteoporotic vertebral fractures in community-dwelling European older adults: An observational analysis of the DO-HEALTH trial. Osteoporos. Int. 2025, 36, 1077–1088. [Google Scholar] [CrossRef] [PubMed]
- Kakoullis, L.; Sampsonas, F.; Karamouzos, V.; Kyriakou, G.; Parperis, K.; Papachristodoulou, E.; Christophi, C.; Lykouras, D.; Kalogeropoulou, C.; Daoussis, D. The impact of osteoporosis and vertebral compression fractures on mortality and association with pulmonary function in COPD: A meta-analysis. Jt. Bone Spine 2022, 89, 105249. [Google Scholar] [CrossRef]
- Lyons, K.J.; Majumdar, S.R.; Ezekowitz, J.A. The unrecognized burden of osteoporosis-related vertebral fractures in patients with heart failure. Circ. Heart Fail. 2011, 4, 419–424. [Google Scholar] [CrossRef]
- Alpantaki, K.; Dohm, M.; Korovessis, P.; Hadjipavlou, A.G. Surgical options for osteoporotic vertebral compression fractures complicated with spinal deformity and neurologic deficit. Injury 2018, 49, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Yang, D.; Zhuo, C.; Zhou, Z.; Aleem, H.B.; Huang, L.; Chen, H. Comparative analysis of percutaneous vertebroplasty and kyphoplasty in the treatment of Stage III Kummell’s disease without neurological symptoms: A retrospective study. J. Orthop. Surg. Res. 2024, 19, 515. [Google Scholar] [CrossRef]
- Deng, R.-Y.; Zhan, P. Clinical Effectiveness of Percutaneous Vertebroplasty in Elderly Patients with Osteoporotic Lumbar Vertebral Fractures: A Retrospective Study. Curr. Probl. Surg. 2025, 69, 101820. [Google Scholar] [CrossRef] [PubMed]
- Alvi, M.A.; Zreik, J.; Yolcu, Y.U.; Goyal, A.; Kim, D.K.; Kallmes, D.F.; Freedman, B.A.; Bydon, M. Comparison of costs and postoperative outcomes between vertebroplasty and kyphoplasty for osteoporotic vertebral compression fractures: Analysis from a state-level outpatient database. World Neurosurg. 2020, 141, e801–e814. [Google Scholar] [CrossRef]
- Encalada, S.; Hunt, C.; Duszynski, B.; Salmasi, V.; Scholten, P.; Zhao, Z.; Rappard, G.; Rivers, W.E.; Vu, T.-N.; Lobel, S. The effectiveness of balloon kyphoplasty compared to conservative treatment for osteoporotic vertebral compression fractures: A systematic review and meta-analysis. Interv. Pain Med. 2025, 4, 100569. [Google Scholar] [CrossRef]
- Daher, M.; Kreichati, G.; Kharrat, K.; Sebaaly, A. Vertebroplasty versus kyphoplasty in the treatment of osteoporotic vertebral compression fractures: A meta-analysis. World Neurosurg. 2023, 171, 65–71. [Google Scholar] [CrossRef]
- You, Z.; Wu, K.; Jiang, Y.; Chen, J. Effect of vertebral kyphoplasty versus vertebroplasty on pain and indicators of imaging parameters of the injured vertebrae in patients with osteoporotic vertebral compression fractures: A meta-analysis. J. Orthop. Surg. Res. 2025, 20, 199. [Google Scholar] [CrossRef]
- Cerny, J.; Soukup, J.; Petrosian, K.; Loukotova, L.; Novotny, T. Efficacy and complication rates of percutaneous vertebroplasty and kyphoplasty in the treatment of vertebral compression fractures: A retrospective analysis of 280 patients. J. Clin. Med. 2024, 13, 1495. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhou, Z.; Lu, G.; Ye, L.; Lao, A.; Ouyang, S.; Song, Z.; Zhang, Z. Risk factors for cement leakage after percutaneous vertebral augmentation for osteoporotic vertebral compression fractures: A meta-analysis. Int. J. Surg. 2025, 111, 1231–1243. [Google Scholar] [CrossRef] [PubMed]
- Sheen, S.; Hasan, P.; Sun, X.; Wang, J.; Tatsui, C.; Nouri, K.; Javed, S. Retrospective Analysis of Cement Extravasation Rates in Vertebroplasty, Kyphoplasty, and Bone Tumor Radiofrequency Ablation. J. Clin. Med. 2025, 14, 2908. [Google Scholar] [CrossRef]
- Yang, F.; Liu, Z.; Li, P.; Zhu, Q.; He, Q.; Liang, Y.; Zhang, B. Analysis of Potential Risk Factors for Cement Leakage into Paraspinal Veins after Vertebroplasty for Acute Osteoporotic Vertebral Fractures Based on a 3D Reconstruction Technique: A Retrospective Matched Case–Control Study. Orthop. Surg. 2023, 15, 3209–3222. [Google Scholar] [CrossRef]
- Baek, I.-H.; Park, H.-Y.; Kim, K.-W.; Jang, T.-Y.; Lee, J.-S. Paraplegia due to intradural cement leakage after vertebroplasty: A case report and literature review. BMC Musculoskelet. Disord. 2021, 22, 741. [Google Scholar] [CrossRef]
- Mao, Z.; Xiong, Z.-H.; Li, J.-F. Thoracic spinal cord injury and paraplegia caused by intradural cement leakage after percutaneous kyphoplasty: A case report. World J. Clin. Cases 2024, 12, 1837. [Google Scholar] [CrossRef]
- Cui, Y.; Pan, Y.; Lin, Y.; Mi, C.; Wang, B.; Shi, X. Risk factors for predicting cement leakage in percutaneous vertebroplasty for spinal metastases. J. Orthop. Sci. 2022, 27, 79–83. [Google Scholar] [CrossRef]
- Coniglio, A.; Rava, A.; Fusini, F.; Colò, G.; Massè, A.; Girardo, M. Effectiveness and reliability of cannulated fenestrated screws augmented with polymethylmethacrylate cement in the surgical treatment of osteoporotic vertebral fractures. J. Craniovertebral Junction Spine 2021, 12, 33–37. [Google Scholar] [CrossRef]
- Chu, W.; Tsuei, Y.-C.; Liao, P.-H.; Lin, J.-H.; Chou, W.-H.; Chu, W.-C.; Young, S.-T. Decompressed percutaneous vertebroplasty: A secured bone cement delivery procedure for vertebral augmentation in osteoporotic compression fractures. Injury 2013, 44, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.-H.; Chou, W.-H.; Tsuei, Y.-C.; Chu, W.; Chu, W.-C. Assessment of cement leakage in decompressed percutaneous kyphoplasty. J. Clin. Med. 2024, 13, 345. [Google Scholar] [CrossRef]
- Lu, H.-T.; Lin, J.-Y.; Tsuei, Y.-C.; Hsu, Y.-F.; Chen, C.-Y.; Cheng, S.-H.; Chu, W.; Li, C.; Chu, W.-C. Impact of aspiration percutaneous vertebroplasty in reducing bone cement leakage and enhancing Distribution—An ex vivo study in goat vertebrae. Bioengineering 2023, 10, 795. [Google Scholar] [CrossRef]
- Lan, Y.; Chen, S.; Lan, G.; Li, C.; Wei, J. Global, regional, and national burden of fracture of vertebral column, 1990–2021: Analysis of data from the global burden of disease study 2021. Front. Public Health 2025, 13, 1573888. [Google Scholar] [CrossRef] [PubMed]
- Ciatti, C.; Asti, C.; Maniscalco, P.; Rinaldi, M.; Pirellas, G.; Caggiari, G.; Pisanu, F.; Sanna, A.; Doria, C. The Use of Polymethylmethacrylate Cement in Percutaneous Vertebroplasty Versus Conservative Management: How to Treat Osteoporotic Vertebral Compression Fractures. Medicina 2025, 61, 2004. [Google Scholar] [CrossRef]
- Zhang, T.-Y.; Zhang, P.-X.; Xue, F.; Zhang, D.-Y.; Jiang, B.-G. Risk factors for cement leakage and nomogram for predicting the intradiscal cement leakage after the vertebra augmented surgery. BMC Musculoskelet. Disord. 2020, 21, 792. [Google Scholar] [CrossRef]
- Hou, J.-G.; Zhang, N.; Chen, G.-D. Factors affecting cement leakage in percutaneous vertebroplasty: A retrospective cohort study of 309 patients. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 3877–3886. [Google Scholar]
- Mao, Y.; Wu, W.; Zhang, J.; Ye, Z. Prediction model of adjacent vertebral compression fractures after percutaneous kyphoplasty: A retrospective study. BMJ Open 2023, 13, e064825. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Xu, S.; Chen, X.; Cui, L.; Wang, Y.; Yan, X.; Liu, Y. The impact of intravertebral cleft on cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: A case-control study. BMC Musculoskelet. Disord. 2021, 22, 805. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Cui, L.; Chen, X.; Liu, Y. Risk factors for cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: An analysis of 1456 vertebrae augmented by low-viscosity bone cement. Spine 2021, 46, 216–222. [Google Scholar] [CrossRef]
- Tan, L.; Wen, B.; Guo, Z.; Chen, Z. The effect of bone cement distribution on the outcome of percutaneous Vertebroplasty: A case cohort study. BMC Musculoskelet. Disord. 2020, 21, 541. [Google Scholar] [CrossRef]
- Zhou, C.; Liao, Y.; Huang, S.; Li, H.; Zhu, Z.; Zheng, L.; Wang, B.; Wang, Y. Effect of cement distribution type on clinical outcome after percutaneous vertebroplasty for osteoporotic vertebral compression fractures in the aging population. Front. Surg. 2022, 9, 975832. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Zhu, X.; Sun, X.; Shi, H.; Sun, L.; Ding, H. Bone cement distribution patterns in vertebral augmentation for osteoporotic vertebral compression fractures: A systematic review. J. Orthop. Surg. Res. 2025, 20, 568. [Google Scholar] [CrossRef] [PubMed]
- Luo, A.-J.; Liao, J.-C.; Chen, L.-H.; Lai, P.-L. High viscosity bone cement vertebroplasty versus low viscosity bone cement vertebroplasty in the treatment of mid-high thoracic vertebral compression fractures. Spine J. 2022, 22, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Y.; Bao, C.; Yang, H.; Li, L.; Yan, L.; Kong, L.; Hao, D.; Wang, B. Biomechanical analysis of a novel bone cement bridging screw system combined with percutaneous vertebroplasty for treating Kummell’s disease. Front. Bioeng. Biotechnol. 2023, 11, 1077192. [Google Scholar] [CrossRef]
- Gao, Y.; Zheng, J.; Yao, K.; Wang, W.; Tan, G.; Xin, J.; Li, N.; Chen, Y. Construction of a nomogram to predict the probability of new vertebral compression fractures after vertebral augmentation of osteoporotic vertebral compression fractures: A retrospective study. Front. Med. 2024, 11, 1369984. [Google Scholar] [CrossRef]
- Zhang, Z.-F.; Liu, D.-H.; Wu, P.-Y.; Xie, C.-L.; Qin, F.-W.; Huang, H. Ultra-early injection of low-viscosity cement in vertebroplasty procedure for treating osteoporotic vertebral compression fractures: A retrospective cohort study. Int. J. Surg. 2018, 52, 35–39. [Google Scholar] [CrossRef]
- Wang, Q.; Sun, C.; Zhang, L.; Wang, L.; Ji, Q.; Min, N.; Yin, Z. High-versus low-viscosity cement vertebroplasty and kyphoplasty for osteoporotic vertebral compression fracture: A meta-analysis. Eur. Spine J. 2022, 31, 1122–1130. [Google Scholar] [CrossRef]
- Viola, R.; Aslan, S.; Al-Smadi, M.W.; Gati, A.; Szilágyi, K.; Foglar, V.; Viola, Á. Effect of Cold Saline Pre-Washing on Cement Leakage in Vertebroplasty: A Novel Approach. J. Clin. Med. 2025, 14, 2755. [Google Scholar] [CrossRef]
- Kochai, A.; Enercan, M.; Kahraman, S.; Ozturk, C.; Hamzaoglu, A. The effect of mechanical aspiration of the vertebral body on pulmonary arterial pressure before cement injection in the vertebroplasty procedure. J. Orthop. Surg. 2018, 26, 2309499018762608. [Google Scholar] [CrossRef]
- Wu, S.C.-H.; Luo, A.-J.; Liao, J.-C. Cement augmentation for treatment of high to mid-thoracic osteoporotic compression fractures, high-viscosity cement percutaneous vertebroplasty versus balloon kyphoplasty. Sci. Rep. 2022, 12, 19404. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Tao, L.; Su, Q.; Zhang, X.; Wu, X. Warning line for preventing bone cement leakage in surgery involving percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Front. Surg. 2025, 12, 1530495. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Tsuei, Y.-C.; Lu, H.-T.; Hsu, Y.-F.; Cheng, S.-H.; Chu, W.; Chu, W.-C. Intraoperative Suction-Assisted Kyphoplasty for Immediate Removal of Posterior PMMA Extravasation in Decompressed Vertebral Compression Fractures. J. Clin. Med. 2026, 15, 481. https://doi.org/10.3390/jcm15020481
Tsuei Y-C, Lu H-T, Hsu Y-F, Cheng S-H, Chu W, Chu W-C. Intraoperative Suction-Assisted Kyphoplasty for Immediate Removal of Posterior PMMA Extravasation in Decompressed Vertebral Compression Fractures. Journal of Clinical Medicine. 2026; 15(2):481. https://doi.org/10.3390/jcm15020481
Chicago/Turabian StyleTsuei, Yu-Chuan, Hsin-Tzu Lu, Yung-Fu Hsu, Shih-Hao Cheng, William Chu, and Woei-Chyn Chu. 2026. "Intraoperative Suction-Assisted Kyphoplasty for Immediate Removal of Posterior PMMA Extravasation in Decompressed Vertebral Compression Fractures" Journal of Clinical Medicine 15, no. 2: 481. https://doi.org/10.3390/jcm15020481
APA StyleTsuei, Y.-C., Lu, H.-T., Hsu, Y.-F., Cheng, S.-H., Chu, W., & Chu, W.-C. (2026). Intraoperative Suction-Assisted Kyphoplasty for Immediate Removal of Posterior PMMA Extravasation in Decompressed Vertebral Compression Fractures. Journal of Clinical Medicine, 15(2), 481. https://doi.org/10.3390/jcm15020481





