Emerging Oculomic Signatures: Linking Thickness of Entire Retinal Layers with Plasma Biomarkers in Preclinical Alzheimer’s Disease
Abstract
1. Introduction
2. Methods
2.1. Study Cohort
2.2. Retinal Layer Segmentation and Analysis
2.3. Plasma Biomarker Assay Methods
2.4. Statistical Analysis
3. Results
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chatterjee, P.; Pedrini, S.; Stoops, E.; Goozee, K.; Villemagne, V.L.; Asih, P.R.; Verberk, I.M.W.; Dave, P.; Taddei, K.; Sohrabi, H.R.; et al. Plasma glial fibrillary acidic protein is elevated in cognitively normal older adults at risk of Alzheimer’s disease. Transl. Psychiatry 2021, 11, 27. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Preische, O.; Schultz, S.A.; Apel, A.; Kuhle, J.; Kaeser, S.A.; Barro, C.; Gräber, S.; Kuder-Buletta, E.; Lafougere, C.; Laske, C.; et al. Long-term course of neurofilament light chain in blood across the Alzheimer’s disease continuum. Alzheimers Res. Ther. 2021, 13, 66. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Palmqvist, S.; Stomrud, E.; Cullen, N.; Janelidze, S.; Manuilova, E.; Jethwa, A.; Bittner, T.; Eichenlaub, U.; Suridjan, I.; Kollmorgen, G.; et al. An accurate fully automated panel of plasma biomarkers for Alzheimer’s disease. Alzheimers Dement. 2023, 19, 1204–1215. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ashton, N.J.; Brum, W.S.; Di Molfetta, G.; Benedet, A.L.; Arslan, B.; Jonaitis, E.; Langhough, R.E.; Cody, K.; Wilson, R.; Carlsson, C.M.; et al. Diagnostic Accuracy of a Plasma Phosphorylated Tau 217 Immunoassay for Alzheimer Disease Pathology. JAMA Neurol. 2024, 81, 255–263. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jang, H.; Shin, D.; Yoo, H.; Zetterberg, H.; Blennow, K.; Gonzalez-Ortiz, F.; Ashton, N.J.; Day, T.A.; Lee, E.H.; Yun, J.; et al. Differential roles of Alzheimer’s disease plasma biomarkers in stepwise biomarker-guided diagnostics. Alzheimers Dement. 2025, 21, e14526. [Google Scholar] [CrossRef]
- Stocker, H.; Beyer, L.; Perna, L.; Rujescu, D.; Holleczek, B.; Beyreuther, K.; Stockmann, J.; Schöttker, B.; Gerwert, K.; Brenner, H. Association of plasma biomarkers, p-tau181, glial fibrillary acidic protein, and neurofilament light, with intermediate and long-term clinical Alzheimer’s disease risk: Results from a prospective cohort followed over 17 years. Alzheimers Dement. 2022, 19, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, E.; Wilkinson, T.; Coughlan, G.; Mirza, S.; Baril, A.; Ramirez, J.; Binns, M.A.; Black, S.E.; Borrie, M.; Dilliott, A.A.; et al. Association of plasma biomarkers with cognition, cognitive decline, and daily function across and within neurodegenerative diseases: Results from the Ontario Neurodegenerative Disease Research Initiative. Alzheimers Dement. 2023, 20, 1753–1770. [Google Scholar] [CrossRef]
- Assfaw, A.D.; Schindler, S.E.; Morris, J.C. Advances in blood biomarkers for Alzheimer’s disease (AD): A review. Kaohsiung J. Med. Sci. 2024, 40, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Chan, V.T.T.; Sun, Z.; Tang, S.; Chen, L.J.; Wong, A.; Tham, C.C.; Wong, T.Y.; Chen, C.; Ikram, M.K.; Whitson, H.E.; et al. Spectral-domain OCT measurements in preclinical Alzheimer’s disease. Ophthalmology 2019, 126, 497–510. [Google Scholar] [CrossRef] [PubMed]
- Asanad, S.; Fantini, M.; Sultan, W.; Nassisi, M.; Felix, C.M.; Wu, J.; Karanjia, R.; Ross-Cisneros, F.N.; Sagare, A.P.; Zlokovic, B.V.; et al. Retinal nerve fiber layer thickness predicts CSF amyloid/tau before cognitive decline. PLoS ONE 2020, 15, e0232785, Correction in PLoS ONE 2020, 15, e0236379. https://doi.org/10.1371/journal.pone.0236379. [Google Scholar]
- Santos, C.Y.; Johnson, L.N.; Sinoff, S.E.; Festa, E.K.; Heindel, W.C.; Snyder, P.J. Change in retinal structural anatomy during the preclinical stage of Alzheimer’s disease. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2018, 10, 196–209. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- López-de-Eguileta, A.; López-García, S.; Lage, C.; Pozueta, A.; García-Martínez, M.; Kazimierczak, M.; Bravo, M.; Irure, J.; López-Hoyos, M.; Muñoz-Cacho, P.; et al. The retinal ganglion cell layer reflects neurodegenerative changes in cognitively unimpaired individuals. Alzheimers Res. Ther. 2022, 14, 57. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harrington, M.G.; Chiang, J.; Pogoda, J.M.; Gomez, M.; Thomas, K.; Marion, S.D.; Miller, K.J.; Siddarth, P.; Yi, X.; Zhou, F.; et al. The Alzheimer’s Disease Fluid Biomarker Study: Design and baseline cohort. Alzheimers Dement. 2013, 9, 743–751. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gorelick, P.B.; Scuteri, A.; Black, S.E.; DeCarli, C.; Greenberg, S.M.; Iadecola, C.; Launer, L.J.; Laurent, S.; Lopez, O.L.; Nyenhuis, D.; et al. Vascular contributions to cognitive impairment and dementia. Stroke 2011, 42, 2672–2713. [Google Scholar] [CrossRef]
- Iadecola, C. The pathobiology of vascular dementia. Neuron 2013, 80, 844–866. [Google Scholar] [CrossRef]
- Mishra, Z.; Ganegoda, A.; Selicha, J.; Wang, Z.; Sadda, S.R.; Hu, Z. Automated Retinal Layer Segmentation Using Graph-based Algorithm Incorporating Deep-learning-derived Information. Sci. Rep. 2020, 10, 9541. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hu, Z.; Wu, X.; Hariri, A.; Sadda, S.R. Multiple layer segmentation and analysis in three-dimensional spectral-domain optical coherence tomography volume scans. J. Biomed. Opt. 2013, 18, 076006. [Google Scholar] [CrossRef] [PubMed]
- Mishra, Z.; Wang, Z.; Sadda, S.R.; Hu, Z. Automatic Segmentation in Multiple OCT Layers For Stargardt Disease Characterization via Deep Learning. Transl. Vis. Sci. Technol. 2021, 10, 24. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Garzone, D.; Finger, R.P.; Mauschitz, M.M.; Santos, M.L.S.; Breteler, M.M.B.; Aziz, N.A. Neurofilament light chain and retinal layers’ determinants and association: A population-based study. Ann. Clin. Transl. Neurol. 2022, 9, 564–569. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- García-Bermúdez, M.Y.; Vohra, R.; Freude, K.; Wijngaarden, P.v.; Martin, K.; Thomsen, M.S.; Aldana, B.I.; Kolko, M. Potential Retinal Biomarkers in Alzheimer’s Disease. Int. J. Mol. Sci. 2023, 24, 15834. [Google Scholar] [CrossRef]
- Linsenmeier, R.A.; Padnick-Silver, L. Metabolic dependence of photoreceptors on the choroid in the normal and detached retina. Investig. Ophthalmol. Vis. Sci. 2000, 41, 3117–3123. [Google Scholar] [PubMed]
- Palmqvist, S.; Insel, P.S.; Stomrud, E.; Janelidze, S.; Zetterberg, H.; Brix, B.; Eichenlaub, U.; Dage, J.L.; Chai, X.; Blennow, K.; et al. Cerebrospinal fluid and plasma biomarker trajectories with increasing amyloid deposition in Alzheimer’s disease. EMBO Mol. Med. 2019, 11, e11170. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Silva-Spínola, A.; Bernardes, C.; Lima, M.; Tábuas-Pereira, M.; Baldeiras, I.; Duro, D.; Tábuas-Pereira, M.; Santana, I.; Baldeiras, I. Blood biomarkers in mild cognitive impairment patients: Relationship between analytes and progression to Alzheimer’s disease dementia. Eur. J. Neurol. 2023, 30, 1565–1573. [Google Scholar] [CrossRef]
- Kim, B.J.; Grossman, M.; Aleman, T.S.; Song, D.; Cousins, K.A.; McMillan, C.T.; Saludades, A.; Yu, Y.; Lee, E.B.; Wolk, D.; et al. Retinal photoreceptor layer thickness has disease specificity and distinguishes predicted FTLD-Tau from biomarker-determined Alzheimer’s disease. Neurobiol. Aging 2023, 125, 74–82. [Google Scholar] [CrossRef]
- Ravichandran, S.; Snyder, P.J.; Alber, J.; Murchison, C.F.; Chaby, L.E.; Jeromin, A.; Arthur, E. Association and multimodal model of retinal and blood-based biomarkers for detection of preclinical Alzheimer’s disease. Alzheimer’s Res. Ther. 2025, 17, 19. [Google Scholar] [CrossRef]
- Fernández-Albarral, J.A.; Salobrar-García, E.; Martínez-Páramo, R.; Ramírez, A.I.; de Hoz, R.; Ramírez, J.M.; Salazar, J.J. Retinal glial changes in Alzheimer’s disease—A review. J. Optom. 2019, 12, 198–207. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Blanks, J.C.; Schmidt, S.Y.; Torigoe, Y.; Porrello, K.V.; Hinton, D.R.; Blanks, R.H. Retinal pathology in Alzheimer’s disease. II. Regional neuron loss and glial changes in GCL. Neurobiol. Aging 1996, 17, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Nagai, N.; Mushiga, Y.; Ozawa, Y. Retinal Pigment Epithelial Abnormality and Choroidal Large Vascular Flow Imbalance Are Associated with Choriocapillaris Flow Deficits in Age-Related Macular Degeneration in Fellow Eyes. J Clin Med. 2023, 12, 1360. [Google Scholar] [CrossRef]
- Asanad, S.; Ross-Cisneros, F.N.; Barron, E.; Nassisi, M.; Sultan, W.; Karanjia, R.; Sadun, A.A. The retinal choroid as an oculovascular biomarker for Alzheimer’s dementia: A histopathological study in severe disease. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2019, 11, 775–783. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bellaver, B.; Povala, G.; Ferreira, P.C.L.; Ferrari-Souza, J.P.; Leffa, D.T.; Lussier, F.Z.; Benedet, A.L.; Ashton, N.J.; Triana-Baltzer, G.; Kolb, H.C.; et al. Astrocyte reactivity influences amyloid-β effects on tau pathology in preclinical Alzheimer’s disease. Nat. Med. 2023, 29, 1775–1781. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ashton, N.J.; Pascoal, T.A.; Karikari, T.K.; Benedet, A.L.; Lantero-Rodriguez, J.; Brinkmalm, G.; Snellman, A.; Schöll, M.; Troakes, C.; Hye, A.; et al. Plasma p-tau231: A new biomarker for incipient Alzheimer’s disease pathology. Acta Neuropathol. 2021, 141, 709–724. [Google Scholar]
- Thal, D.R.; Li, X.; Konstatoulea, K.; Gawor, K.; Wiedmer, A.; von Arnim, C.A.; Vandenberghe, R.; Carpentier, S.; Otto, M.; Schymkowitz, J.; et al. Basic Science and Pathogenesis. Alzheimers. Dement. 2025, 21, e102036. [Google Scholar] [CrossRef]
- den Haan, J.; Morrema, T.H.; Verbraak, F.D.; de Boer, J.F.; Scheltens, P.; Rozemuller, A.J.; Bergen, A.A.; Bouwman, F.H.; Hoozemans, J.J. Amyloid-beta and phosphorylated tau in post-mortem Alzheimer’s disease retinas. Acta Neuropathol. Commun. 2018, 6, 147. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Cunefare, D.; Wang, C.; Guymer, R.H.; Li, S.; Farsiu, S. Automatic segmentation of nine retinal layer boundaries in OCT images of non-exudative AMD patients using deep learning and graph search. Biomed. Opt. Express 2017, 8, 2732–2744. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Carass, A.; Liu, Y.; Jedynak, B.M.; Solomon, S.D.; Saidha, S.; Calabresi, P.A.; Prince, J.L. Fully convolutional boundary regression for OCT layer segmentation. Biomed. Opt. Express 2019, 10, 364–377. [Google Scholar]
- Marques, I.P.; Alves, D.; Santos, T.; Mendes, L.; Lobo, C.; Santos, A.R.; Durbin, M.; Cunha-Vaz, J. Graph-based deep learning for automated retinal layer segmentation in OCT. Investig Ophthalmol. Vis. Sci. 2020, 61, 20. [Google Scholar] [CrossRef] [PubMed]
- Cullen, N.C.; Leuzy, A.; Janelidze, S.; Palmqvist, S.; Svenningsson, A.L.; Stomrud, E.; Dage, J.L.; Mattsson-Carlgren, N.; Hansson, O. Plasma biomarkers of Alzheimer’s disease improve prediction of cognitive decline in cognitively unimpaired elderly populations. Nat. Commun. 2021, 12, 3555. [Google Scholar] [CrossRef]
- Mattsson-Carlgren, N.; Salvadó, G.; Ashton, N.J.; Tideman, P.; Stomrud, E.; Zetterberg, H.; Ossenkoppele, R.; Betthauser, T.J.; Cody, K.A.; Jonaitis, E.M.; et al. Prediction of Longitudinal Cognitive Decline in Preclinical Alzheimer Disease Using Plasma Biomarkers. JAMA Neurol. 2023, 80, 360–369. [Google Scholar] [CrossRef]
| Characteristic | N | Mean ± SD | Percent | Notes |
|---|---|---|---|---|
| Total number of subjects | 11 | |||
| Total number of eyes | 20 | |||
| Age (years) | 11 | 74.9 ± 10.4 | ||
| Females | 9 | 82% | ||
| ApoE ε 3/3 | 9 | 82% | ||
| ApoE ε 3/4 | 2 | 18% | ||
| Plasma Aβ42/40 ratio | 11 | 0.05 ± 0.01 | <0.10 = increased risk of AD | |
| NFL | 11 | 178,722.20 ± 88,823.43 | ||
| GFAP | 11 | 59,253.03 ± 23,691.11 | ||
| ptau217 | 11 | 7689.32 ± 2955.07 | ||
| ptau181 | 11 | 2928.47± 2346.68 | ||
| Mini-Mental Status Exam score | 11 | 26.0 ± 0.9 | ≥24 = normal cognition | |
| Best-corrected visual acuity | 20 | 20/25 ± 2.2 |
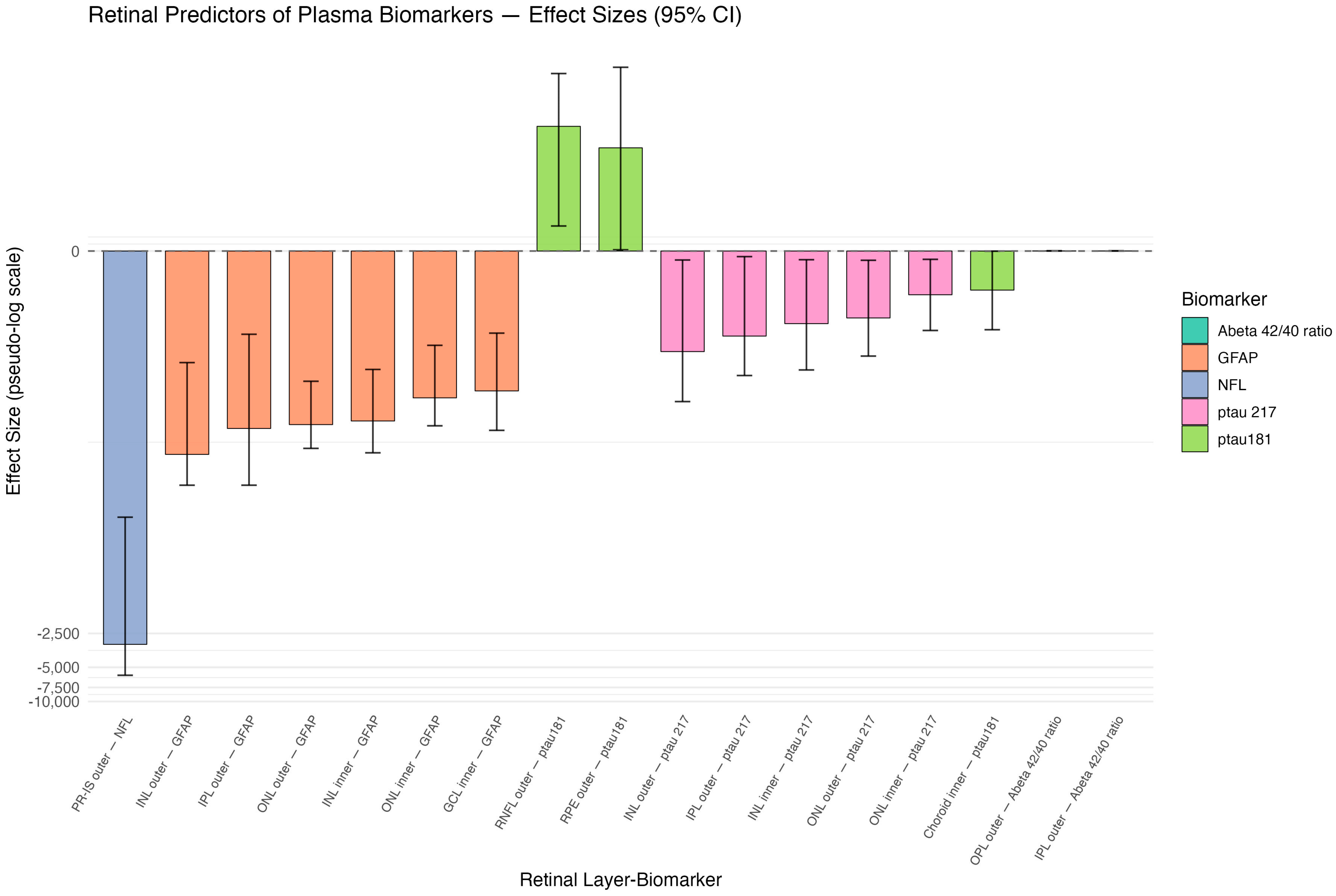
| Predictor | Outcome | Estimate (95% CI) | Natural Log Estimate | CI Width | Direction | Significance |
|---|---|---|---|---|---|---|
| PR-IS outer ring | NfL | −3126.8 (−5849.4, −231.8) | −8.0 | 5617.6 | Negative | Yes |
| INL outer ring | GFAP | −64.1 (−120.4, −9.7) | −4.2 | 110.7 | Negative | Yes |
| IPL outer ring | GFAP | −37.7 (−120.4, −5.3) | −3.6 | 115.1 | Negative | Yes |
| ONL outer ring | GFAP | −34.8 (−56.7, −14.3) | −3.5 | 42.4 | Negative | Yes |
| INL inner ring | GFAP | −32.3 (−62.1, −11.2) | −3.5 | 50.9 | Negative | Yes |
| ONL inner ring | GFAP | −20.1 (−35.7, −6.7) | −3.0 | 29.0 | Negative | Yes |
| GCL inner ring | GFAP | −17.4 (−39.2, −5.2) | −2.9 | 34.0 | Negative | Yes |
| RNFL outer ring | p-tau181 | 12.7 (1.1, 37.7) | 2.5 | 36.6 | Positive | Yes |
| RPE cell layer outer ring | p-tau181 | 8.1 (0, 42.9) | 2.1 | 42.9 | Positive | No |
| INL outer ring | p-tau217 | −7.7 (−21.7, −0.4) | −2.0 | 21.3 | Negative | Yes |
| IPL outer ring | p-tau217 | −5.5 (−12.7, −0.2) | −1.7 | 12.5 | Negative | Yes |
| INL inner ring | p-tau217 | −4.2 (−11.3, −0.4) | −1.4 | 10.9 | Negative | Yes |
| ONL outer ring | p-tau217 | −3.7 (−8.5, −0.4) | −1.3 | 8.1 | Negative | Yes |
| ONL inner ring | p-tau217 | −2.1 (−4.9, −0.3) | −0.7 | 4.6 | Negative | Yes |
| Choroid inner ring | p-tau181 | −1.8 (−4.8, 0) | −0.6 | 4.8 | Negative | No |
| OPL outer ring | Aβ42/40 ratio | 0 (0, 0) | 0.0 | 0.0 | Positive | No |
| IPL outer ring | Aβ42/40 ratio | 0 (0, 0) | 0.0 | 0.0 | Positive | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Abboud, I.; Xu, E.; Xu, S.; Alhasany, A.; Wang, Z.; Wu, X.; Astraea, N.; Jiang, F.; Hu, Z.J.; Chan, J.W. Emerging Oculomic Signatures: Linking Thickness of Entire Retinal Layers with Plasma Biomarkers in Preclinical Alzheimer’s Disease. J. Clin. Med. 2026, 15, 275. https://doi.org/10.3390/jcm15010275
Abboud I, Xu E, Xu S, Alhasany A, Wang Z, Wu X, Astraea N, Jiang F, Hu ZJ, Chan JW. Emerging Oculomic Signatures: Linking Thickness of Entire Retinal Layers with Plasma Biomarkers in Preclinical Alzheimer’s Disease. Journal of Clinical Medicine. 2026; 15(1):275. https://doi.org/10.3390/jcm15010275
Chicago/Turabian StyleAbboud, Ibrahim, Emily Xu, Sophia Xu, Aya Alhasany, Ziyuan Wang, Xiaomeng Wu, Natalie Astraea, Fei Jiang, Zhihong Jewel Hu, and Jane W. Chan. 2026. "Emerging Oculomic Signatures: Linking Thickness of Entire Retinal Layers with Plasma Biomarkers in Preclinical Alzheimer’s Disease" Journal of Clinical Medicine 15, no. 1: 275. https://doi.org/10.3390/jcm15010275
APA StyleAbboud, I., Xu, E., Xu, S., Alhasany, A., Wang, Z., Wu, X., Astraea, N., Jiang, F., Hu, Z. J., & Chan, J. W. (2026). Emerging Oculomic Signatures: Linking Thickness of Entire Retinal Layers with Plasma Biomarkers in Preclinical Alzheimer’s Disease. Journal of Clinical Medicine, 15(1), 275. https://doi.org/10.3390/jcm15010275






