Multicentre Retrospective Cohort Study on Current Practices in Treatment of Patients Presenting with Non-A Non-B Aortic Dissection and Factors Predicting the Need for Intervention and Mortality
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Endpoints
- Demographics (age, gender, ethnicity); cardiovascular risk factors (diabetes, hypertension, obesity, smoking status, recreational drug use).
- Coexisting morbidities (renal, cardiac, cerebrovascular, pulmonary, peripheral arteries diseases and congenital aortic syndromes).
- Clinical presentation at the acute onset.
- Selected treatment strategies and complications encountered.
- In-hospital mortality (death during the first hospitalization).
2.3. Statistical Analysis
3. Results
3.1. Baseline Data and Management Strategies
- -
- Urgent operations were performed in seven (18.4%) cases as reported above;
- -
- Ten (26.3%) patients required surgery within 15 days (mean, 13 days; range, 0–30 days) for recurrent symptoms or uncontrolled hypertension with or without imaging evidence of proximal extension of the AD (7) or end-organ ischemia (1).
- -
- Two (5.3%) patients were operated upon within two months (27 and 43 days after the initial diagnosis, respectively) for recurrent pain and proximal extension at the CTA.
- -
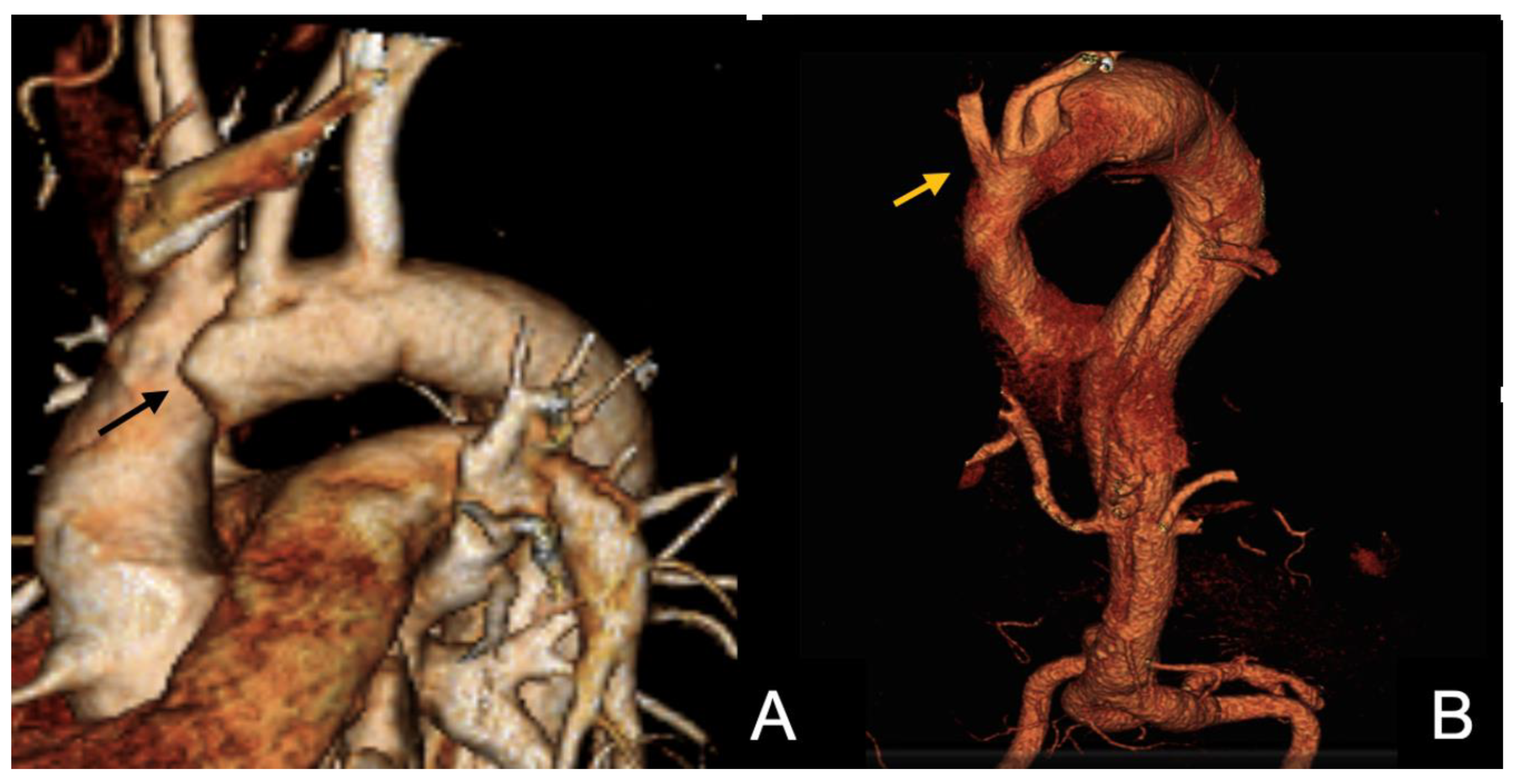
- Finally, two patients died from aortic rupture and cardiac tamponade one and two days after the acute onset, respectively, while waiting for surgery. In those cases, dissection originated from zones 3 and 2, respectively, and extended to the iliofemoral vessels; aortic diameter at the entry tear site was 35 mm in both cases, with a dilated non-dissected ascending aorta (maximal diameter 46 mm) being reported in one case (Figure 1).
3.2. Clinical Results and Factors Associated with Mortality and Need of Intervention
- a.
- In interventionally treated patients, aortic-related reinterventions during follow-up included two emergent operations (one TEVAR performed 4 days after FET for a DTA rupture, and one ascending aorta repair for retrograde extension of the dissection 8 days after a hybrid repair, as detailed above); three planned TEVAR procedures were completed for residual dissection with large communication within the lumens (one month after FET in two cases; three months after FET in one case).
- b.
- In the medically treated group, two patients needed an aortic procedure during the follow-up: one of them underwent open thoracoabdominal aneurysm repair two years after the initial diagnosis; the other needed an axillo–femoral bypass to treat claudication following FL thrombosis and true lumen stenosis one month after initial diagnosis.
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- von Segesser, L.K.; Killer, I.; Ziswiler, M.; Linka, A.; Ritter, M.; Jenni, R.; Baumann, P.C.; Turina, M.I. Dissection of the descending thoracic aorta extending into the ascending aorta. A therapeutic challenge. J. Thorac. Cardiovasc. Surg. 1994, 108, 755–761. [Google Scholar] [CrossRef]
- Lombardi, J.V.; Hughes, G.C.; Appoo, J.J.; Bavaria, J.E.; Beck, A.W.; Cambria, R.P.; Charlton-Ouw, K.; Eslami, M.H.; Kim, K.M.; Leshnower, B.G.; et al. Society for Vascular Surgery (SVS) and Society of Thoracic Surgeons (STS) reporting standards for type B aortic dissections. J. Vasc. Surg. 2020, 7, 723–747. [Google Scholar] [CrossRef]
- Sievers, H.H.; Rylski, B.; Czerny, M.; Baier, A.L.M.; Kreibich, M.; Siepe, M.; Beyersdorf, F. Aortic dissection reconsidered: Type, entry site, malperfusion classification adding clarity and enabling outcome prediction. Interact. Cardiovasc. Thorac. Surg. 2020, 30, 451–457. [Google Scholar] [CrossRef]
- Hiratzka, L.F.; Bakris, G.L.; Beckman, J.A.; Bersin, R.M.; Carr, V.F.; Casey, D.E., Jr.; Eagle, K.A.; Hermann, L.K.; Isselbacher, E.M.; Kazerooni, E.A.; et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: Executive summary. Catheter. Cardiovasc. Interv. 2010, 76, E43–E86. [Google Scholar]
- Borghese, O.; Pisani, A.; Mastracci, T.M. Challenges in diagnosis of Non-A Non-B Acute Aortic Dissection. Ann. Vasc. Surg. 2024, 108, 201–218. [Google Scholar] [CrossRef]
- Czerny, M.; Schmidli, J.; Adler, S.; van den Berg, J.C.; Bertoglio, L.; Carrel, T.; Chiesa, R.; Clough, R.E.; Eberle, B.; EACTS/ESVS scientific document group; et al. Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: An expert consensus document of the European Association for Cardio-Thoracic surgery (EACTS) and the European Society for Vascular Surgery (ESVS). Eur. J. Cardiothorac. Surg. 2019, 55, 133–162. [Google Scholar]
- Carino, D.; Singh, M.; Molardi, A.; Agostinelli, A.; Goldoni, M.; Pacini, D.; Nicolini, F. Non-A non-B aortic dissection: A systematic review and meta-analysis. Eur. J. Cardiothorac. Surg. 2019, 55, 653–659. [Google Scholar] [CrossRef]
- Kreibich, M.; Siepe, M.; Berger, T.; Kondov, S.; Morlock, J.; Pingpoh, C.; Beyersdorf, F.; Rylski, B.; Czerny, M. The Frozen Elephant Trunk Technique for the Treatment of Type B and Type Non-ANon-B Aortic Dissection. Eur. J. Vasc. Endovasc. Surg. 2021, 6, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yang, F.; Chen, L.; Xie, E.; Su, S.; Liu, Y.; Geng, Q.; Fan, R.; Li, J.; Luo, J. Management and outcomes of non-A non-B aortic dissection. Eur. J. Vasc. Endovasc. Surg. 2022, 64, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Kosiorowska, M.; Berezowski, M.; Widenka, K.; Kreibich, M.; Beyersdorf, F.; Czerny, M.; Rylski, B. Non-A non-B acute aortic dissection with entry tear in the aortic arch. Interact. Cardiovasc. Thorac. Surg. 2022, 34, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Piao, H.; Wang, Y.; Li, B.; Zhu, Z.; Wang, T.; Liu, K. Early outcomes with a hybrid technique for repair of a non-A non-B aortic dissection. J. Thorac. Cardiovasc. Surg. 2022, 163, 1766–177412. [Google Scholar] [CrossRef]
- Ishimaru, S. Endografting of the aortic arch. J. Endovasc. Ther. 2004, 11, II62–II71. [Google Scholar] [CrossRef]
- Evangelista, A.; Isselbacher, E.M.; Bossone, E.; Gleason, T.G.; Eusanio, M.D.; Sechtem, U.; Ehrlich, M.P.; Trimarchi, S.; Braverman, A.C.; Myrmel, T.; et al. Insights from the international registry of acute aortic dissection: A 20-year experience of collaborative clinical research. Circulation 2018, 137, 1846–1860. [Google Scholar] [CrossRef]
- Urbanski, P.P.; Wagner, M. Acute non-A–non-B aortic dissection: Surgical or conservative approach? Eur. J. Cardiothorac. Surg. 2016, 49, 1249–1254. [Google Scholar] [CrossRef]
- Rylski, B.; Pérez, M.; Beyersdorf, F.; Reser, D.; Kari, F.A.; Siepe, M.; Czerny, M. Acute non-A non-B aortic dissection: Incidence, treatment and outcome. Eur. J. Cardiothorac. Surg. 2017, 52, 1111–1117. [Google Scholar] [CrossRef]
- Valentine, R.J.; Boll, J.M.; Hocking, K.M.; Curci, J.A.; Garrard, C.L.; Brophy, C.M.; Naslund, T.C. Aortic arch involvement worsens the prognosis of type B aortic dissections. J. Vasc. Surg. 2016, 64, 1212–1218. [Google Scholar] [CrossRef]
- Borghese, O.; Pisani, A.; Lopez-Marco, A.; Adams, B.; Oo, A.Y.; Kapil, V.; Mastracci, T. Aortic Outcomes After Implementation of a Treatment Strategy for Type B Aortico Dissection Involving the Aortic Arch. Ann. Vasc. Surg. 2025, 110, 373–38518. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.C.; Clough, R.E.; Taylor, P.R. Predicting aneurysmal dilatation after type B aortic dissection. Eur. J. Vasc. Endovasc. Surg. 2011, 42, 464–466. [Google Scholar] [CrossRef]
- Song, J.M.; Kim, S.D.; Kim, J.H.; Kim, M.J.; Kang, D.H.; Seo, J.B.; Lim, T.-H.; Lee, J.W.; Song, M.-G.; Song, J.-K. Long-term predictors of descending aorta aneurysmal change in patients with aortic dissection. J. Am. Coll. Cardiol. 2007, 50, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Shu, C.; Luo, M.Y.; Li, Q.M.; Li, M.; Wang, T.; He, H. Early results of left carotid chimney technique in endovascular repair of acute non-a-non-B aortic dissections. J. Endovasc. Ther. 2011, 18, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Shu, C.; Li, X.; Wang, T.; Li, M.; Li, Q.M.; Fang, K.; Wang, S. Endovascular aortic repair combined with chimney technique in the treatment of stanford type B aortic dissection involving aortic arch. Ann. Vasc. Surg. 2015, 29, 758–763. [Google Scholar] [CrossRef] [PubMed]
- Nauta, F.J.; Tolenaar, J.L.; Patel, H.J.; Appoo, J.J.; Tsai, T.T.; Desai, N.D.; Montgomery, D.G.; Mussa, F.F.; Upchurch, G.R.; Fattori, R.; et al. Impact of Retrograde Arch Extension in Acute Type B Aortic Dissection on Management and Outcomes. Ann. Thorac. Surg. 2016, 102, 2036–2043. [Google Scholar] [CrossRef] [PubMed]
| Baselines Data | Total = 38 n% |
|---|---|
| Sex | |
| Male | 26 (68.4) |
| Female | 12 (31.6) |
| Age, years (mean, SD) | 60.5 (SD 12.9) |
| Ethnicity | |
| Caucasian | 29 (76.3) |
| Asian | 4 (10.5) |
| Black | 5 (13.2) |
| Cardiovascular risk factors | |
| Hypertension | 35 (92.1) |
| Active Smoker | 8 (21.1) |
| Former smoker * | 3 (7.9) |
| Diabetes Mellitus | 2 (5.3) |
| Dyslipidaemia | 11 (28.9) |
| Comorbidities | |
| Prior Stroke/TIA † | 4 (10.5) |
| COPD ‡ | 2 (5.3) |
| CAD § | 2 (5.3) |
| CKD ‖ | 4 (10.5) |
| Arrythmia | 2 (5.3) |
| Marfan Syndrome | 1 (2.6) |
| Alcohol abuse | 1 (2.6) |
| Drug use | 2 (5.3) |
| Clinical presentation (one or more) | |
| Uncontrolled hypertension | 24 (63.2) |
| Chest/back pain | 32 (84.2) |
| Abdominal pain | 2 (5.3) |
| Neurological symptoms | 3 (7.9) |
| Shortness of breath | 1 (2.6) |
| Syncope | 2 (5.3) |
| Malperfusion | 4 (10.5) |
| Anatomical Data | Total = 38 n% |
|---|---|
| Primary entry tear at presentation | |
| Zone 1 | 7 (18.4) |
| Zone 2 | 17 (44.7) |
| Zone 3 | 13 (34.2) |
| Zone 4 | 1 (2.6) |
| Involvement of collateral branches | |
| Brachiocephalic artery | 1 (2.6) |
| Left common carotid | 3 (7.9) |
| Left subclavian artery | 2 (5.3) |
| Coeliac trunk | 6 (15.8) |
| Superior mesenteric artery | 8 (21.1) |
| Right renal artery | 6 (15.8) |
| Left renal artery | 18 (47.4) |
| Inferior mesenteric artery | 11 (28.9) |
| Mean Aortic Diameter (mm) at initial presentation | (median, IRQ) |
| Zone 0 | 37 (7) |
| Zone 1 | 36 (7) |
| Zone 2 | 34.5 (6) |
| Zone 3 | 35 (11) |
| Zone 4 | 35 (11) |
| Zone 5 | 30.5 (7) |
| Zone 6 | 27 (8) |
| Zone 7 | 24.5 (6) |
| Management Strategy | Total = 38 (100) N (%) |
|---|---|
| Treatment during the first 24 h | |
| BMT * | 31 (81.6) |
| Surgery | 7 (18.4) |
| Indication for surgical treatment during the first 24 h (one or more) | Total = 13 |
| Risks of impending aortic rupture/retrograde extension to the aortic root | 6 (17.8) |
| Hemodynamic instability/persistent pain in the setting of low blood pressure | 6 (17.8) |
| Clinical/laboratory signs of end organ malperfusion | 1 (2.6) |
| Timing to Surgery after BMT * in days (mean, range) | 13 (0–30) |
| Indication for surgical treatment after BMT *(one or more) | |
| Recurrent symptoms | 2 (5.3) |
| Unfavourable anatomic evolution at the serial CTA † (rupture, proximal/distal extension of the dissection, aortic growth) | 12 (38.7) |
| Clinical/laboratory signs of visceral/lower limb malperfusion | 2 (5.3) |
| In-Hospital and Follow-Up Clinical Outcomes | |
|---|---|
| Total = 38 (100%) N (%) | |
| 30-day mortality | 5 (13.2) |
| Medically treated complications | |
| Stroke/TIA * | 3 (7.9) |
| Myocardial infarction | - |
| Spinal cord ischemia † | 1 (2.6) |
| Pulmonary infection | 11 (28.9) |
| Bowel ischaemia ‡ | - |
| Renal failure § | 5 (13.5) |
| Complications requiring surgical treatment | 8 (21.1) |
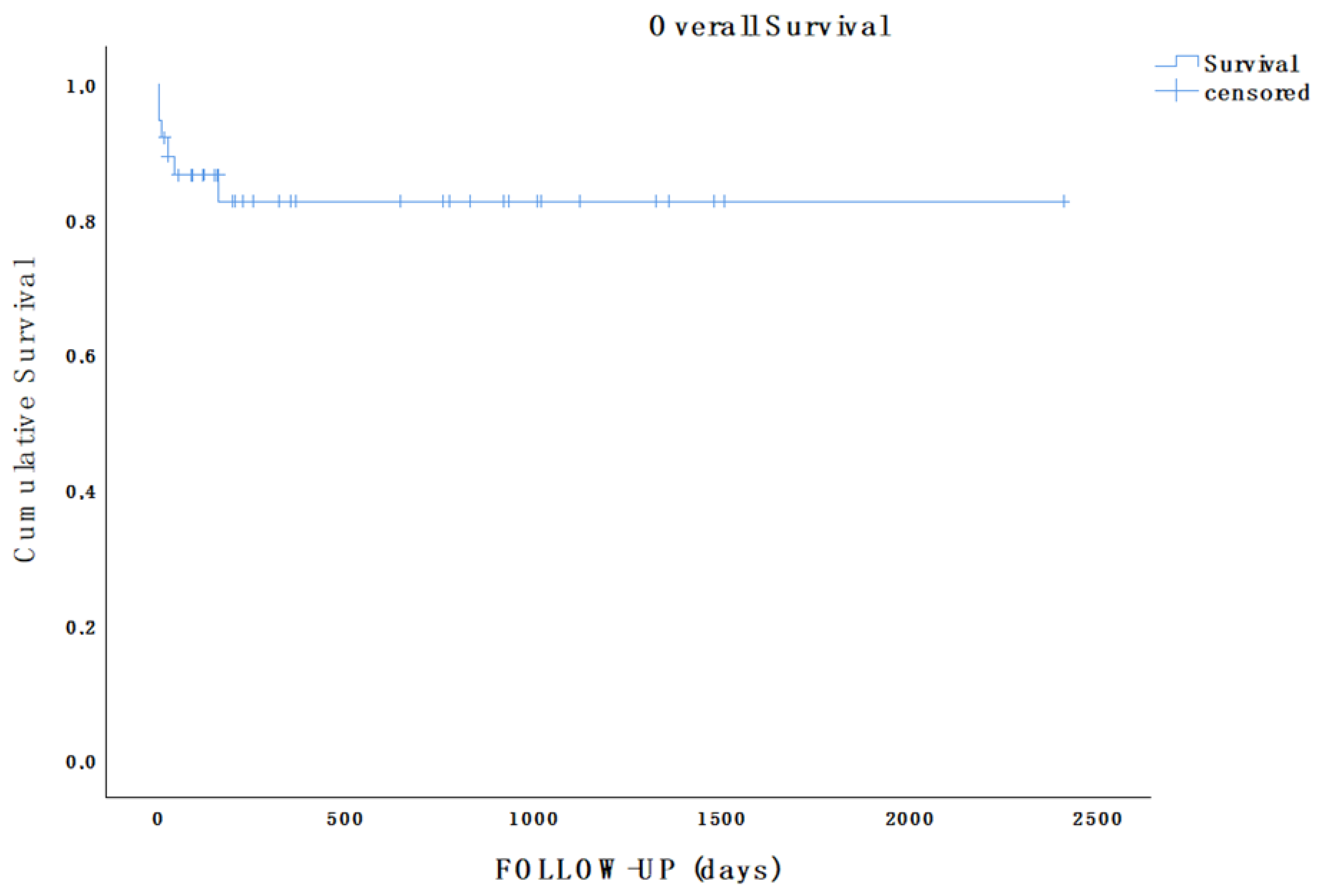
| Survival rate during follow-up | 32 (84.1) |
| Aortic-related reintervention | 7 (19.4) |
| Length of stay (median, IQR) | |
| ICU ‖ stay | 9 (20) |
| Hospital stay | 18 (25) |
| Follow-up in days/months (mean, range) | 16.9 (2–80.2) |
| Outcomes Comparison Between Interventionally and Conservatively Treated Groups | |||
|---|---|---|---|
| Outcomes | Need for Surgery After BMT | ||
| NO | YES | p | |
| 30-day mortality | - | 4 (30.8) | 0.023 |
| Complication | |||
| Stroke/TIA * | 1 (5.6) | 2 (15.4) | 0.558 |
| Myocardial infarction | - | - | - |
| Spinal cord ischemia † | - | - | - |
| Pulmonary infection | - | 6 (46.2) | 0.002 |
| Bowel ischaemia ‡ | - | - | - |
| Renal failure § | 1 (5.6) | 3 (25.0) | 0.274 |
| Aortic-related intervention during follow-up | 3 (16.7) | 2 (18.2) | 0.917 |
| Thrombosis FL | 9 (52.9) | 9 (81.8) | 0.226 |
| Death during follow-up | - | 1 (8.3) | 0.400 |
| Length of stay (mean, range) | |||
| ICU ‖ | 8 (1–30) | 29 (2–59) | 0.010 |
| Hospital Stay | 13 (6–45) | 38 (2–54) | 0.012 |
| Follow-up (mean, range) | 630.4 (18–2406) | 445.5 (2–1359) | 0.415 |
| Need for surgery after BMT | |||
| NO (total = 18) | YES (total = 13) | p | |
| Female | 6 (33.3) | 5 (38.5) | 0.768 |
| Age (mean, SD) | 57.6 (11.4) | 66.1 (12.5) | 0.059 |
| Ethnicity | |||
| Caucasian | 13 (72.2) | 11 (84.6) | |
| Asian | 2 (11.1) | 1 (7.7) | |
| Black | 3 (16.7) | 1 (7.7) | |
| Hypertension | 15 (83.3) | 13 (100) | 0.245 |
| Dyslipidaemia | 5 (27.8) | 5 (38.5) | 0.530 |
| COPD | 1 (5.6) | 1 (7.7) | 0.811 |
| Prior stroke/TIA * | 2 (11.1) | 2 (15.4) | 0.726 |
| Diabetes mellitus type II | - | 1 (7.7) | 0.419 |
| CAD | 2 (11.1) | - | 0.497 |
| Chronic kidney failure (GFR < 30 mL/min/1.73 m2) | 1 (5.6) | 2 (15.4) | 0.558 |
| Atrial fibrillation | - | 1 (7.7) | 0.419 |
| Aortic diameter (median, IQR) | |||
| Zone 0 | 36.5 (9) | 37 (5) | 0.146 |
| Zone 1 | 34 (7) | 37 (3) | 0.043 |
| Zone 2 | 32.5 (7) | 36 (6) | 0.044 |
| Zone 3 | 35 (8) | 37 (10) | 0.472 |
| Zone 4 | 34.5 (12) | 35 (15) | 0.366 |
| Zone 5 | 30 (10) | 31 (5) | 0.448 |
| Zone 6 | 24.5 (7) | 28 (8) | 0.126 |
| Zone 7 | 22.5 (8) | 25 (4) | 0.431 |
| Factors Associated with Increased Risk of Mortality | ||||
|---|---|---|---|---|
| Univariable analysis | Multivariable analysis | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Male | 4.000 (0.571–28.011) | 0.301 | 7.658 (0.291–201.431) | 0.222 |
| Hypertension | 1.167 (1.019–1.336) | 1.000 | ||
| Smoking | - | 1.000 | ||
| Diabetes | - | 1.000 | ||
| Dyslipidaemia | 1.778 (0.254–12.449) | 0.559 | 4.445 (0.115–171.213) | 0.423 |
| Stroke/TIA | 2.500 (0.207–30.215) | 0.459 | ||
| COPD | - | 1.000 | ||
| CAD | - | 1.000 | ||
| Renal failure | - | 1.000 | ||
| Arrythmia | - | 1.000 | ||
| Marfan Syndrome | ||||
| Alcohol abuse | - | 1.000 | ||
| Drug use | - | 1.000 | ||
| Previous aortic surgery | - | 1.000 | ||
| Entry tear | ||||
| Zone 1 | - | 1.000 | ||
| Zone 2 | 6.154 (0.617–61.371) | 0.152 | ||
| Zone 3 | 0.438 (0.044–4.378) | 0.643 | ||
| Zone 4 | - | 1.000 | ||
| Proximal extent of the AD | 0.339 (0.034–3.376) | 0.630 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Borghese, O.; Lopez-Pena, G.; Saratzis, A.; Vainas, T.; Lopes, A.; Maurel, B.; Mastracci, T. Multicentre Retrospective Cohort Study on Current Practices in Treatment of Patients Presenting with Non-A Non-B Aortic Dissection and Factors Predicting the Need for Intervention and Mortality. J. Clin. Med. 2026, 15, 211. https://doi.org/10.3390/jcm15010211
Borghese O, Lopez-Pena G, Saratzis A, Vainas T, Lopes A, Maurel B, Mastracci T. Multicentre Retrospective Cohort Study on Current Practices in Treatment of Patients Presenting with Non-A Non-B Aortic Dissection and Factors Predicting the Need for Intervention and Mortality. Journal of Clinical Medicine. 2026; 15(1):211. https://doi.org/10.3390/jcm15010211
Chicago/Turabian StyleBorghese, Ottavia, Gabriel Lopez-Pena, Athanasios Saratzis, Tryfon Vainas, Alice Lopes, Blandine Maurel, and Tara Mastracci. 2026. "Multicentre Retrospective Cohort Study on Current Practices in Treatment of Patients Presenting with Non-A Non-B Aortic Dissection and Factors Predicting the Need for Intervention and Mortality" Journal of Clinical Medicine 15, no. 1: 211. https://doi.org/10.3390/jcm15010211
APA StyleBorghese, O., Lopez-Pena, G., Saratzis, A., Vainas, T., Lopes, A., Maurel, B., & Mastracci, T. (2026). Multicentre Retrospective Cohort Study on Current Practices in Treatment of Patients Presenting with Non-A Non-B Aortic Dissection and Factors Predicting the Need for Intervention and Mortality. Journal of Clinical Medicine, 15(1), 211. https://doi.org/10.3390/jcm15010211






