Effect of Eyelid Opener on Wound Closure Time in Cataract Surgery
Abstract
:1. Introduction
2. Material and Methods
2.1. Ethics Statement
2.2. Subjects
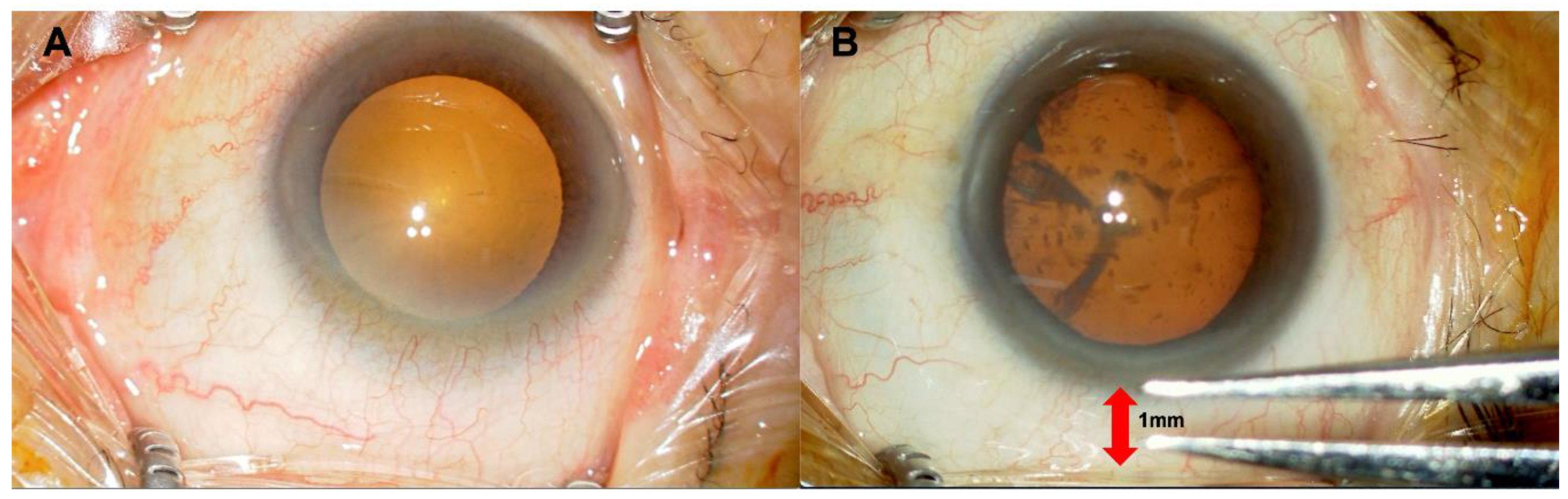
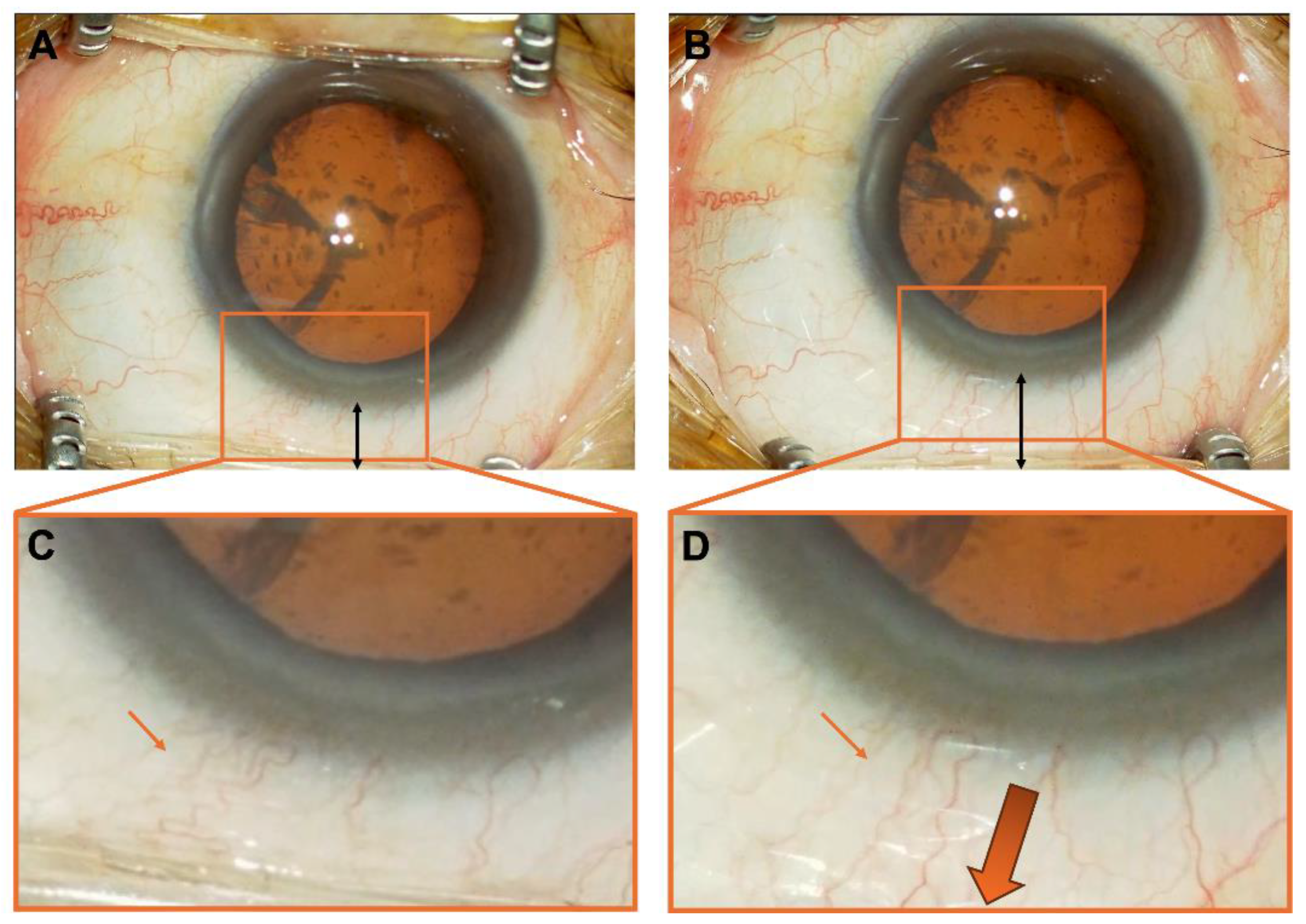
2.3. Surgical Methods
2.4. Comparison Between Groups: Full Eyelid Opening Group and 1-mm Eyelid Opening Group
2.5. Statistical Analysis
3. Results
3.1. Subjects Characteristics
3.2. Comparison of Postoperative Ocular Data
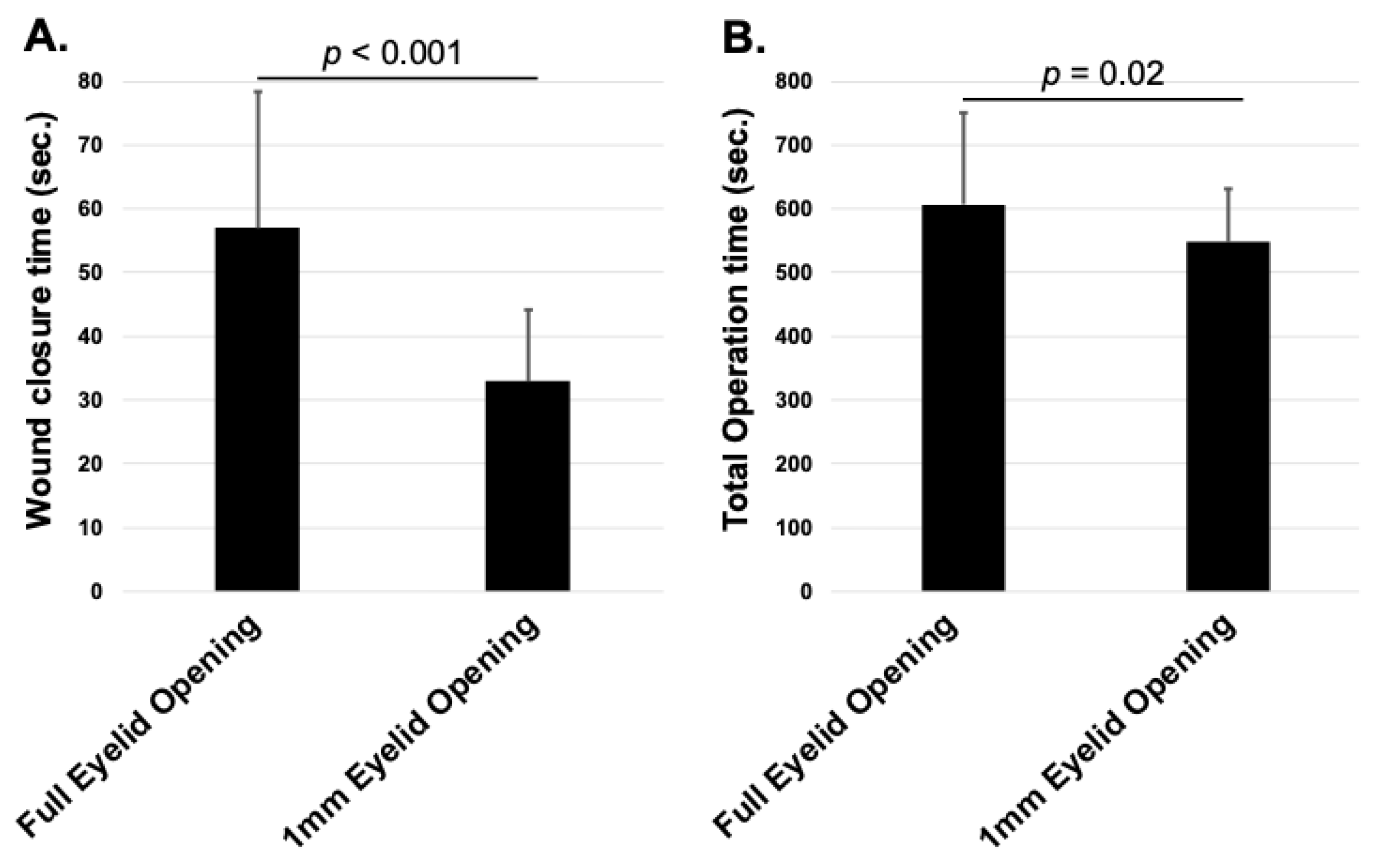
3.3. Comparison of Wound Closure and Total Operation Time
4. Discussion
4.1. Advantages
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, Y.C.; Wilkins, M.; Kim, T.; Malyugin, B.; Mehta, J.S. Cataracts. Lancet 2017, 390, 600–612. [Google Scholar] [CrossRef] [PubMed]
- Lindstrom, R. Thoughts on Cataract Surgery: 2015. Review of Ophthalmology. Published online: 9 March 2015. Available online: https://www.reviewofophthalmology.com/article/thoughts-on--cataract-surgery-2015 (accessed on 23 April 2025).
- Leaming, D.V. Practice styles and preferences of ASCRS members-survey 2001. J. Cataract Refract. Surg. 2002, 28, 1681–1688. [Google Scholar] [CrossRef] [PubMed]
- Seal, D.V.; Barry, P.; Gettinby, G.; Lees, F.; Peterson, M.; Revie, C.W.; Wilhelmus, K.R.; ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Case for a European multicenter study. J. Cataract Refract. Surg. 2006, 32, 396–406. [Google Scholar] [CrossRef] [PubMed]
- Cooper, B.A.; Holekamp, N.M.; Bohigian, G.; Thompson, P.A. Case-control study of endophthalmitis after cataract surgery comparing scleral tunnel and clear corneal wounds. Am. J. Ophthalmol. 2003, 136, 300–305. [Google Scholar] [CrossRef]
- Nagaki, Y.; Hayasaka, S.; Kadoi, C.; Matsumoto, M.; Yanagisawa, S.; Watanabe, K.; Watanabe, K.; Hayasaka, Y.; Ikeda, N.; Sato, S.; et al. Bacterial endophthalmitis after small-incision cataract surgery. effect of incision placement and intraocular lens type. J. Cataract Refract. Surg. 2003, 29, 20–26. [Google Scholar] [CrossRef]
- Ninomiya, Y.; Hirakata, A.; Hiraoka, T.; Kunita, D.; Inoue, M.; Oshitari, K.; Sugitani, A.; Futagami, S.; Miki, D.; Hida, T. Clinical features of endophthalmitis after cataract surgery evaluated by the presence of background factors. Nippon Ganka Gakkai Zasshi 2008, 112, 525–530. [Google Scholar]
- Althiabi, S.; Aljbreen, A.J.; Alshutily, A.; Althwiny, F.A. Postoperative endophthalmitis after cataract surgery: An update. Cureus 2022, 14, e22003. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cao, H.; Zhang, L.; Li, L.; Lo, S. Risk factors for acute endophthalmitis following cataract surgery: A systematic review and meta-analysis. PLoS ONE 2013, 8, e71731. [Google Scholar] [CrossRef]
- Matossian, C.; Makari, S.; Potvin, R. Cataract surgery and methods of wound closure: A review. Clin. Ophthalmol. 2015, 9, 921–928. [Google Scholar] [CrossRef]
- Chee, S.P.; Ti, S.E.; Lim, L.; Chan, A.S.Y.; Jap, A. Anterior segment optical coherence tomography evaluation of the integrity of clear corneal incisions: A comparison between 2.2-mm and 2.65-mm main incisions. Am. J. Ophthalmol. 2010, 149, 768–776.e1. [Google Scholar] [CrossRef]
- Vasavada, A.R.; Praveen, M.R.; Pandita, D.; Gajjar, D.U.; Vasavada, V.A.; Vasavada, V.A.; Raj, S.M.; Johar, K. Effect of stromal hydration of clear corneal incisions: Quantifying ingress of trypan blue into the anterior chamber after phacoemulsification. J. Cataract Refract. Surg. 2007, 33, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Fine, I.H.; Hoffman, R.S.; Packer, M. Profile of clear corneal cataract incisions demonstrated by ocular coherence tomography. J. Cataract Refract. Surg. 2007, 33, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Doeller, B.; Hirnschall, N.; Fichtenbaum, M.; Nguyen, P.M.; Varsits, R.; Findl, O. A randomized study of the impact of a corneal pre-cut during cataract surgery on wound architecture and corneal astigmatism. Ophthalmol. Ther. 2021, 10, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Bar-Sela, S.M.; Spierer, O.; Spierer, A. Suture-related complications after congenital cataract surgery: Vicryl versus mersilene sutures. J. Cataract Refract. Surg. 2007, 33, 301–304. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Mohammadi, M.; Naderan, M.; Pahlevani, R.; Jahanrad, A. Prevalence of corneal astigmatism before cataract surgery. Int. Ophthalmol. 2016, 36, 807–817. [Google Scholar] [CrossRef]
- Ferrer-Blasco, T.; Montés-Micó, R.; Peixoto-de-Matos, S.C.; González-Méijome, J.M.; Cerviño, A. Prevalence of corneal astigmatism before cataract surgery. J. Cataract Refract. Surg. 2009, 35, 70–75. [Google Scholar] [CrossRef]
- Marek, R.; Kluś, A.; Pawlik, R. Comparison of surgically induced astigmatism of temporal versus superior clear corneal incisions. Klin. Oczna 2006, 108, 392–396. [Google Scholar]
- Borasio, E.; Mehta, J.S.; Maurino, V. Surgically induced astigmatism after phacoemulsification in eyes with mild to moderate corneal astigmatism: Temporal versus on-axis clear corneal incisions. J. Cataract Refract. Surg. 2006, 32, 565–572. [Google Scholar] [CrossRef]
- Khokhar, S.; Lohiya, P.; Murugiesan, V.; Panda, A. Corneal astigmatism correction with opposite clear corneal incisions or single clear corneal incision: Comparative analysis. J. Cataract Refract. Surg. 2006, 32, 1432–1437. [Google Scholar] [CrossRef]
- Shepherd, J.R. Induced astigmatism in small incision cataract surgery. J. Cataract Refract. Surg. 1989, 15, 85–88. [Google Scholar] [CrossRef]
- Hayashi, K.; Yoshida, M.; Hayashi, H. Postoperative corneal shape changes: Microincision versus small-incision coaxial cataract surgery. J. Cataract Refract. Surg. 2009, 35, 233–239. [Google Scholar] [CrossRef]
| Full Eyelid Opening Group (Mean ± SD) | 1 mm Eyelid Opening Group (Mean ± SD) | p Value | |
|---|---|---|---|
| Age | 71.6 ± 9.40 | 72.9 ± 7.30 | 0.904 |
| Right/left | 41/37 | 24/27 | 0.666 |
| Sex (male/female) | 43/35 | 21/30 | 0.171 |
| BCVA (logMAR) | −0.21 ± 0.37 | −0.16 ± 0.43 | 0.354 |
| Refractive error (diopter) | −1.90 ± 4.59 | −0.38 ± 2.95 | 0.266 |
| Axial length (mm) | 24.1 ± 3.09 | 24.2 ± 1.12 | 0.925 |
| Corneal endothelium (cells/mm2) | 2744 ± 263 | 2746 ± 251 | 0.747 |
| Full Eyelid Opening Group (Mean ± SD) | 95% CI | 1 mm Eyelid Opening Group (Mean ± SD) | 95% CI | p Value | |
|---|---|---|---|---|---|
| Postoperative day 2 BCVA (logMAR) | −0.09 ± 0.18 | −0.13–−0.049 | −0.08 ± 0.15 | −0.12–0.032 | 0.588 |
| Postoperative day 7 BCVA (logMAR) | −0.016 ± 0.12 | −0.044–0.012 | −0.002 ± 0.10 | −0.030–0.031 | 0.231 |
| Postoperative day 2 UCVA (logMAR) | −0.19 ± 0.15 | −0.24–−0.15 | −0.20 ± 0.24 | −0.28–0.12 | 0.881 |
| Postoperative day 7 UCVA (logMAR) | −0.11 ± 0.16 | −0.15–−0.066 | −0.10 ± 0.20 | −0.16–0.032 | 0.910 |
| Intraocular pressure on postoperative day 1 (mmHg) | 15.7 ± 4.50 | 14.7–16.7 | 15.1 ± 3.28 | 14.0–15.9 | 0.652 |
| Intraocular pressure on postoperative day 2 (mmHg) | 13.7 ± 3.41 | 13.0–14.5 | 13.8 ± 2.81 | 12.9–14.4 | 0.915 |
| Anterior chamber protein measurement day 2 | 17.7 ± 9.75 | 15.4–20.0 | 17.6 ± 6.82 | 15.3–19.3 | 0.904 |
| Anterior chamber protein measurement day 7 | 13.3 ± 6.49 | 11.7–14.8 | 12.8 ± 5.95 | 10.9–14.6 | 0.354 |
| Postoperative day 7 corneal endothelium (cells/mm2) | 2770 ± 301 | 2700–2838 | 2686 ± 284 | 2605–2767 | 0.095 |
| Postoperative corneal endothelial reduction (cells/mm2) | −25.5 ± 279 | −89.3–38.3 | 53.9 ± 168 | −0.29–121 | 0.158 |
| Total operation time (second) | 606.9 ± 144 | 574–640 | 547.5 ± 83.1 | 523–571 | 0.02 |
| Wound closing time (second) | 57.0 ± 21.3 | 52.1–61.9 | 32.9 ± 11.2 | 31.7–38.2 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakono, T.; Mihara, N.; Sakamoto, T.; Terasaki, H. Effect of Eyelid Opener on Wound Closure Time in Cataract Surgery. J. Clin. Med. 2025, 14, 3163. https://doi.org/10.3390/jcm14093163
Sakono T, Mihara N, Sakamoto T, Terasaki H. Effect of Eyelid Opener on Wound Closure Time in Cataract Surgery. Journal of Clinical Medicine. 2025; 14(9):3163. https://doi.org/10.3390/jcm14093163
Chicago/Turabian StyleSakono, Takato, Naohisa Mihara, Taiji Sakamoto, and Hiroto Terasaki. 2025. "Effect of Eyelid Opener on Wound Closure Time in Cataract Surgery" Journal of Clinical Medicine 14, no. 9: 3163. https://doi.org/10.3390/jcm14093163
APA StyleSakono, T., Mihara, N., Sakamoto, T., & Terasaki, H. (2025). Effect of Eyelid Opener on Wound Closure Time in Cataract Surgery. Journal of Clinical Medicine, 14(9), 3163. https://doi.org/10.3390/jcm14093163




