Early Changes in Volumetric Body Composition Parameters Predict Survival Outcomes in Patients with Metastatic Renal Cell Carcinoma Treated with Targeted Therapy
Abstract
:1. Introduction
2. Materials and Methods
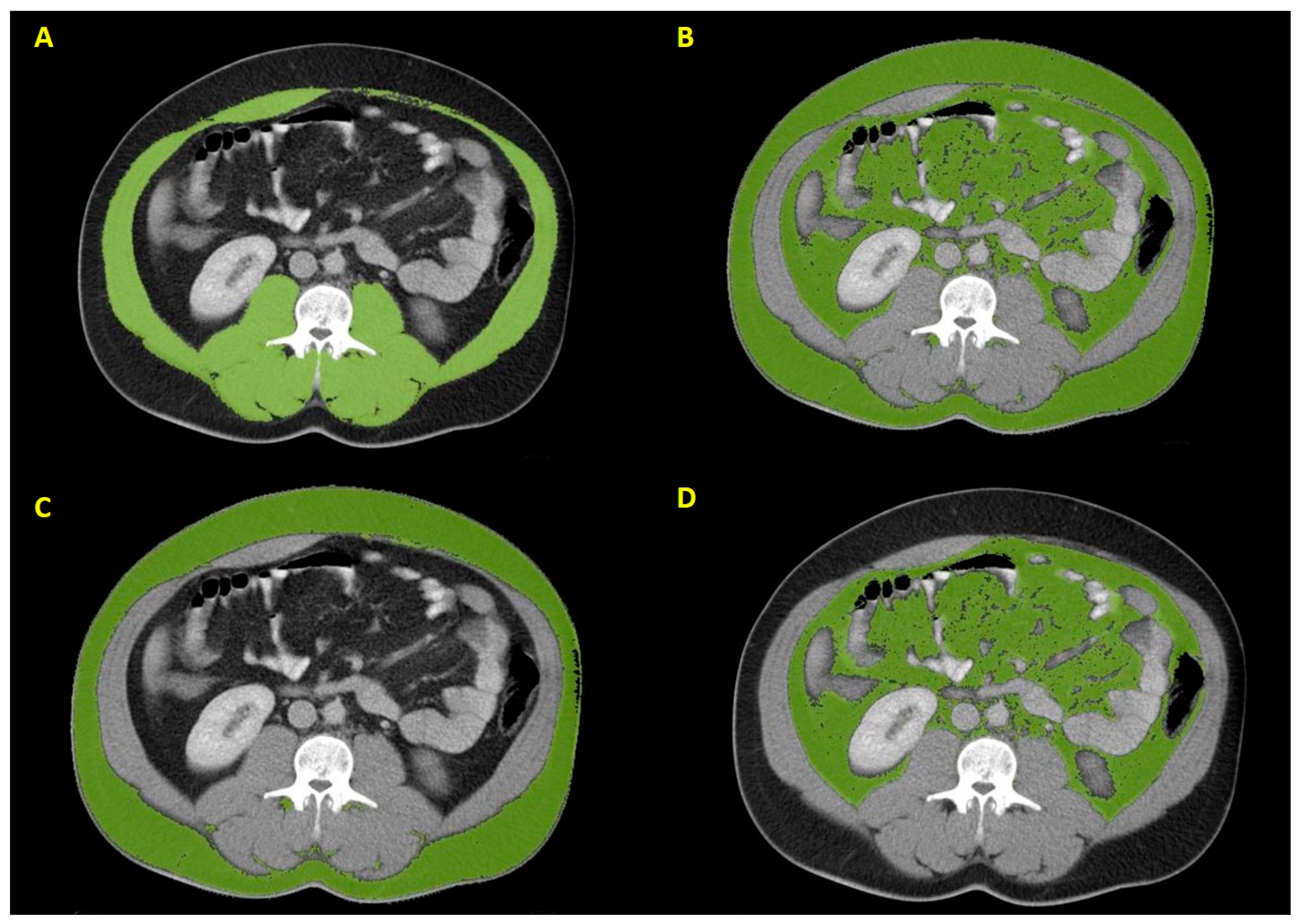
2.1. Imaging Analysis
2.2. Statistical Analysis
3. Results
3.1. Baseline Patient Characteristics
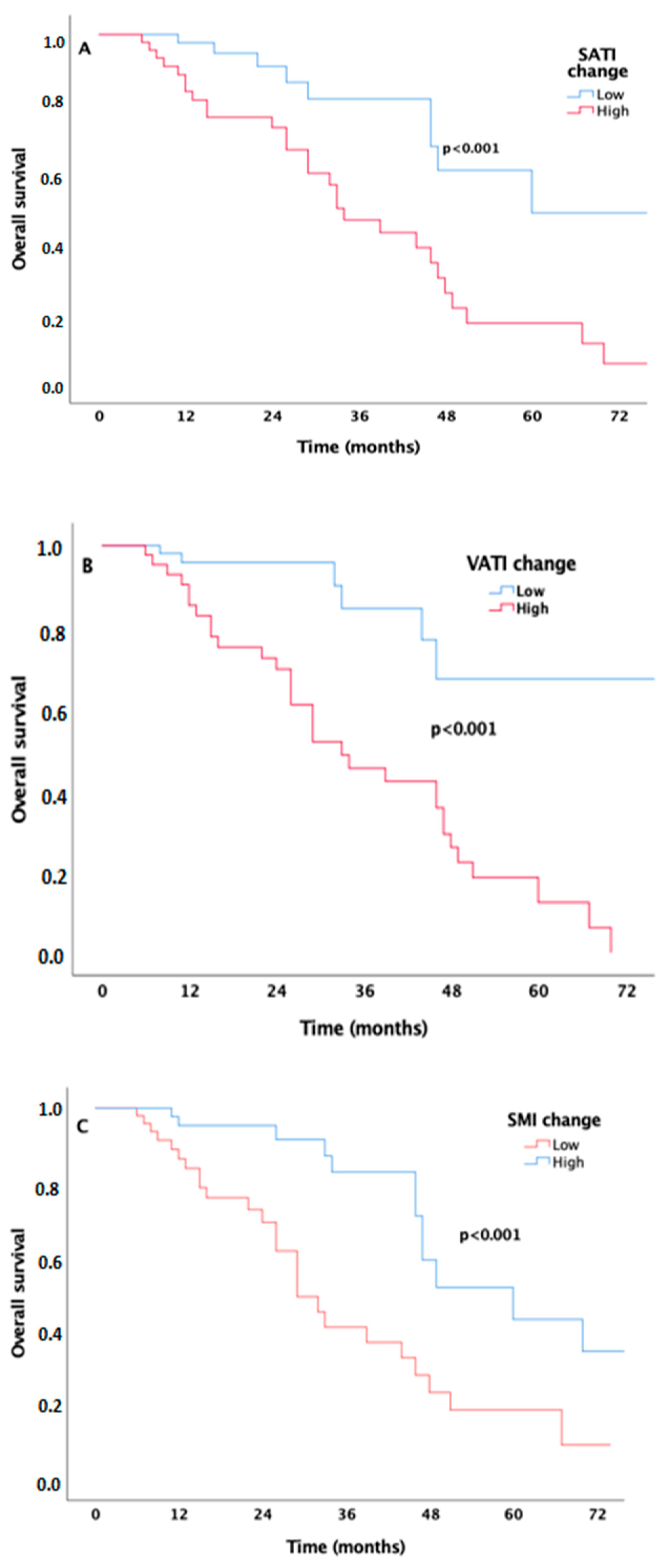
3.2. The Effect of Body Composition Parameters on Survival Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BSA | Body surface area |
| BMI | Body mass index |
| CI | Confidence interval |
| CT | Computerized tomography |
| HR | Hazard ratio |
| ICI | Immune checkpoint inhibitor |
| IMDC | International Metastatic Renal Cell Carcinoma Database Consortium |
| mRCC | Metastatic renal cell carcinoma |
| OS | Overall survival |
| PFS | Progression-free survival |
| RCC | Renal cell carcinoma |
| ROC | Receiver operating characteristic |
| SATI | Subcutaneous adipose tissue index |
| SFA | Subcutaneous fat area |
| SMI | Skeletal muscle index |
| VEGF | Vascular endothelial growth factor |
| VATI | Visceral adipose tissue index |
| VFA | Visceral fat area |
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. CA Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Capitanio, U.; Montorsi, F. Renal cancer. Lancet 2016, 387, 894–906. [Google Scholar] [CrossRef] [PubMed]
- Ivanyi, P.; Fröhlich, T.; Grünwald, V.; Zschäbitz, S.; Bedke, J.; Doehn, C. The Treatment of Metastatic Renal Cell Carcinoma. Dtsch. Arztebl. Int. 2024, 121, 576–586. [Google Scholar] [CrossRef]
- Heng, D.Y.; Xie, W.; Regan, M.M.; Warren, M.A.; Golshayan, A.R.; Sahi, C.; Eigl, B.J.; Ruether, J.D.; Cheng, T.; North, S.; et al. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor–targeted agents: Results from a large, multicenter study. J. Clin. Oncol. 2009, 27, 5794–5799. [Google Scholar] [CrossRef]
- Klinghoffer, Z.; Yang, B.; Kapoor, A.; Pinthus, J.H. Obesity and renal cell carcinoma: Epidemiology, underlying mechanisms and management considerations. Expert Rev. Anticancer Ther. 2009, 9, 975–987. [Google Scholar] [CrossRef]
- Calle, E.E.; Kaaks, R. Overweight, obesity and cancer: Epidemiological evidence and proposed mechanisms. Nat. Rev. Cancer. 2004, 4, 579–591. [Google Scholar] [CrossRef]
- Donat, S.M.; Salzhauer, E.W.; Mitra, N.; Yanke, B.V.; Snyder, M.E.; Russo, P. Impact of Body Mass Index on Survival of Patients With Surgically Treated Renal Cell Carcinoma. J. Urol. 2006, 175, 46–52. [Google Scholar] [CrossRef]
- Hakimi, A.A.; Furberg, H.; Zabor, E.C.; Jacobsen, A.; Schultz, N.; Ciriello, G.; Mikklineni, N.; Fiegoli, B.; Kim, P.H.; Voss, M.H.; et al. An Epidemiologic and Genomic Investigation Into the Obesity Paradox in Renal Cell Carcinoma. JNCI J. Natl. Cancer Inst. 2013, 105, 1862–1870. [Google Scholar] [CrossRef] [PubMed]
- Steffens, S.; Grünwald, V.; Ringe, K.I.; Seidel, C.; Eggers, H.; Schrader, M.; Wacker, F.; Kuczyk, M.A.; Schrader, A.J. Does Obesity Influence the Prognosis of Metastatic Renal Cell Carcinoma in Patients Treated with Vascular Endothelial Growth Factor–Targeted Therapy? Oncologist 2011, 16, 1565–1571. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Horwich, T.B.; Oreopoulos, A.; Kovesdy, C.P.; Younessi, H.; Anker, S.D.; Morley, J.E. Risk factor paradox in wasting diseases. Curr. Opin. Clin. Nutr. Metab. Care. 2007, 10, 433–442. [Google Scholar] [CrossRef]
- Gu, W.; Wu, J.; Liu, X.; Zhang, H.; Shi, G.; Zhu, Y.; Ye, D. Early skeletal muscle loss during target therapy is a prognostic biomarker in metastatic renal cell carcinoma patients. Sci. Rep. 2017, 7, 7587. [Google Scholar] [CrossRef]
- Harimoto, N.; Shirabe, K.; Yamashita, Y.I.; Ikegami, T.; Yoshizumi, T.; Soejima, Y.; Ikeda, T.; Maehara, Y.; Nishie, A.; Yamanaka, T. Sarcopenia as a predictor of prognosis in patients following hepatectomy for hepatocellular carcinoma. Br. J. Surg. 2013, 100, 1523–1530. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, Y.; Baba, Y.; Sakamoto, Y.; Ohuchi, M.; Tokunaga, R.; Kurashige, J.; Hiyoshi, Y.; Iwagami, S.; Yoshida, N.; Yoshida, M.; et al. Sarcopenia is a Negative Prognostic Factor After Curative Resection of Colorectal Cancer. Ann. Surg. Oncol. 2015, 22, 2663–2668. [Google Scholar] [CrossRef]
- Antoun, S.; Baracos, V.E.; Birdsell, L.; Escudier, B.; Sawyer, M.B. Low body mass index and sarcopenia associated with dose-limiting toxicity of sorafenib in patients with renal cell carcinoma. Ann. Oncol. 2010, 21, 1594–1598. [Google Scholar] [CrossRef]
- Prado, C.M.; Lieffers, J.R.; McCargar, L.J.; Reiman, T.; Sawyer, M.B.; Martin, L.; Baracos, V.E. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 2008, 9, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Gu, W.; Zhu, Y.; Wang, H.; Zhang, H.; Shi, G.; Liu, X.; Ye, D. Prognostic Value of Components of Body Composition in Patients Treated with Targeted Therapy for Advanced Renal Cell Carcinoma: A Retrospective Case Series. PLoS ONE 2015, 10, e0118022. [Google Scholar] [CrossRef] [PubMed]
- Ladoire, S.; Bonnetain, F.; Gauthier, M.; Zanetta, S.; Petit, J.M.; Guiu, S.; Kermarrec, I.; Mourey, E.; Michel, F.; Krause, D.; et al. Visceral Fat Area as a New Independent Predictive Factor of Survival in Patients with Metastatic Renal Cell Carcinoma Treated with Antiangiogenic Agents. Oncologist 2011, 16, 71–81. [Google Scholar] [CrossRef]
- Antoun, S.; Lanoy, E.; Iacovelli, R.; Albiges-Sauvin, L.; Loriot, Y.; Merad-Taoufik, M.; Fizazi, K.; di Palma, M.; Baracos, V.E.; Escudier, B. Skeletal muscle density predicts prognosis in patients with metastatic renal cell carcinoma treated with targeted therapies. Cancer 2013, 119, 3377–3384. [Google Scholar] [CrossRef]
- Antoun, S.; Birdsell, L.; Sawyer, M.B.; Venner, P.; Escudier, B.; Baracos, V.E. Association of Skeletal Muscle Wasting With Treatment With Sorafenib in Patients With Advanced Renal Cell Carcinoma: Results From a Placebo-Controlled Study. J. Clin. Oncol. 2010, 28, 1054–1060. [Google Scholar] [CrossRef]
- Powles, T.; Albiges, L.; Staehler, M.; Bensalah, K.; Dabestani, S.; Giles, R.H.; Hofmann, F.; Hora, M.; Kuczyk, M.A.; Lam, T.B.; et al. Updated European Association of Urology Guidelines: Recommendations for the Treatment of First-line Metastatic Clear Cell Renal Cancer. Eur. Urol. 2018, 73, 311–315. [Google Scholar] [CrossRef]
- Motzer, R.J.; Penkov, K.; Haanen, J.; Rini, B.; Albiges, L.; Campbell, M.T.; Venugopal, B.; Kollmannsberger, C.; Negrier, S.; Uemura, M.; et al. Avelumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Yip, S.M.; Heng, D.Y.C.; Tang, P.A. Review of the Interaction Between Body Composition and Clinical Outcomes in Metastatic Renal Cell Cancer Treated With Targeted Therapies. J. Kidney Cancer VHL 2016, 3, 12–22. [Google Scholar] [CrossRef] [PubMed]
- McManus, H.D.; Zhang, D.; Schwartz, F.R.; Wu, Y.; Infield, J.; Ho, E.; Armstrong, A.J.; George, D.J.; Kruse, D.; Gupta, R.T.; et al. Relationship Between Pretreatment Body Composition and Clinical Outcomes in Patients With Metastatic Renal Cell Carcinoma Receiving First-Line Ipilimumab Plus Nivolumab. Clin. Genitourin. Cancer 2023, 21, e429–e437.e2. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | All Patients (n = 108) | Female (n = 31) | Male (n = 77) |
|---|---|---|---|
| Age [median (IQR)] | 57 (51–64) | 56 (50–64) | 59 (52–64) |
| IMDC risk group [n (%)] | |||
| Favorable | 23 (21.3%) | 6 (19.4%) | 17 (22.1%) |
| İntermediate | 54 (50%) | 19 (61.2%) | 35 (45.4%) |
| Poor | 31 (28.7%) | 6 (19.4%) | 25 (32.5%) |
| Histology [n (%)] | |||
| Clear cell | 84 (77.8%) | 27(87%) | 57 (74%) |
| Non-clear cell | 24 (22.2%) | 4 (13%) | 20 (26%) |
| Metastatic sites [n (%)] | |||
| ≤2 | 88 (81.5%) | 24 (81.5%) | 64 (81.5%) |
| >2 | 20 (18.5%) | 7 (18.5%) | 13 (18.5%) |
| Fuhrman grade [n (%)] | |||
| I–II | 88 (81.5%) | 28 (90.3%) | 60 (77.9%) |
| III–IV | 20 (18.5%) | 3 (9.7%) | 17 (22.1%) |
| Treatment [n (%)] | |||
| Pazopanib | 64 (59.3%) | 17 (54.8%) | 47 (61%) |
| Sunitinib | 44 (40.7%) | 14 (45.2%) | 30 (39%) |
| Body Composition Variables | All Patients n = 108 | Female n = 31 (28.7%) | Men n = 77 (71.3%) | p-Value |
|---|---|---|---|---|
| Height, cm | 1.70 (1.64–1.75) | 1.61 (1.58–1.65) | 1.71 (1.69–1.75) | <0.001 |
| Weight, kg | 75 (69–82) | 70 (63–77) | 77 (70–83) | 0.004 |
| BMI (kg/m2) | 25.9 (3.89) | 26.7 (3.83) | 25.8 (3.93) | 0.541 |
| Baseline VATI, cm2/m2 | 45.7 (32.6–72.5) | 53.2 (33.4–80.1) | 44.2 (30.7–66.9) | 0.252 |
| First VATI, cm2/m2 | 47.7 (30.2–71.5) | 40.7 (30.6–75.8) | 48 (30–67.9) | 0.911 |
| ΔVATI, cm2/m2 | −2.3 (−8.1–6.2) | −3.5 (−8.8–3.6) | −1 (−7.7–7.2) | 0.310 |
| Baseline SATI, cm2/m2 | 54.5 (39.6–77.9) | 76.2 (64.8–114.3) | 47.5 (34–68.7) | <0.001 |
| First SATI, cm2/m2 | 60.3 (39.7–77.6) | 75.4 (60.5–112.6) | 54.2 (31.6–71.5) | <0.001 |
| ΔSATI, cm2/m2 | −0.64 (−6.8–7.7) | −5.9 (−9.9–6.5) | 2 (−5.13–7.8) | 0.018 |
| Baseline SMI, cm2/m2 | 49.2 (41.7–55.3) | 43.5 (39.5–49.9) | 51.8 (42.8–58.6) | 0.004 |
| First SMI, cm2/m2 | 46.9 (39.2–54.5) | 44 (36.3–49.9) | 47.5 (40.5–55.35) | 0.082 |
| ΔSMI, cm2/m2 | −1.6 (−5.2–0.5) | −0.85 (−2.9–1.3) | −2.24 (−6.7–[−0.07]) | 0.067 |
| PFS | OS | |||
|---|---|---|---|---|
| Characteristic | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| Age, years | 1 (0.98–1.03) | 0.464 | 1 (0.96–1.03) | 0.937 |
| Gender (Male vs. Female) | 1.41 (0.91–2.18) | 0.121 | 1.63 (0.74–3.58) | 0.223 |
| IMDC risk group | <0.001 | 0.001 | ||
| Favorable | 1 (reference) | 1 (reference) | ||
| İntermediate | 1.66 (0.98–2.82) | 0.06 | 2.59 (1.19–5.66) | 0.016 |
| Poor | 6.95 (3.55–13.59) | <0.001 | 8.91 (2.95–26.92) | <0.001 |
| Tumor grade (III–IV vs. I–II) | 1.02 (0.63–1.65) | 0.913 | 1.3 (0.63–2.69) | 0.476 |
| Histology (non-clear vs. clear) | 0.85 (0.49–1.45) | 0.553 | 1.33 (0.62–2.83) | 0.453 |
| Metastasis region site (III–IV vs. I–II) | 1.09 (0.65–1.81) | 0.737 | 0.43 (0.10–1.82) | 0.256 |
| BMI | 0.95 (0.9–1) | 0.223 | 0.94 (0.84–1.04) | 0.245 |
| Baseline VATI | 0.99 (0.98–1) | 0.251 | 0.99 (0.98–1) | 0.185 |
| ΔVATI (high value vs. low value) | 0.65 (0.43–0.99) | 0.049 | 4.7 (1.82–12.15) | 0.001 |
| Baseline SATI | 1 (0.99–1) | 0.945 | 0.99 (0.98–1) | 0.168 |
| ΔSATI (high value vs. low value) | 0.61 (0.40–0.94) | 0.028 | 3.61 (1.70–7.66) | 0.001 |
| Baseline SMI | 0.97 (0.96–0.99) | 0.011 | 1.01 (0.98–1.04) | 0.345 |
| ΔSMI (low value vs. high value) | 1.5 (0.98–2.29) | 0.056 | 3.29 (1.64–6.61) | 0.001 |
| PFS | OS | |||
|---|---|---|---|---|
| Characteristic | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| ΔSMI (low value vs. high value) | 2.66 (1.30–5.45) | 0.007 | ||
| ΔVATI (high value vs. low value) | 5.10 (1.90–13.69) | 0.001 | ||
| Baseline SMI | 0.98 (0.96–0.99) | 0.026 | ||
| IMDC risk group | <0.001 | 0.001 | ||
| Favorable | 1 (reference) | 1 (reference) | ||
| İntermediate | 1.74 (1.02–2.97) | 0.040 | 2.38 (1.06–5.34) | 0.057 |
| Poor | 6.84 (3.48–13.47) | <0.001 | 9.58 (2.86–32.0) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aktepe, O.H.; Erdemir, A.G.; Caliskan Yildirim, E.; Demirciler, E.; Ulasli, T.; Guven, D.C.; Onur, M.R.; Unek, I.T.; Semiz, H.S.; Erman, M.; et al. Early Changes in Volumetric Body Composition Parameters Predict Survival Outcomes in Patients with Metastatic Renal Cell Carcinoma Treated with Targeted Therapy. J. Clin. Med. 2025, 14, 3140. https://doi.org/10.3390/jcm14093140
Aktepe OH, Erdemir AG, Caliskan Yildirim E, Demirciler E, Ulasli T, Guven DC, Onur MR, Unek IT, Semiz HS, Erman M, et al. Early Changes in Volumetric Body Composition Parameters Predict Survival Outcomes in Patients with Metastatic Renal Cell Carcinoma Treated with Targeted Therapy. Journal of Clinical Medicine. 2025; 14(9):3140. https://doi.org/10.3390/jcm14093140
Chicago/Turabian StyleAktepe, Oktay Halit, Ahmet Gurkan Erdemir, Eda Caliskan Yildirim, Erkut Demirciler, Tugce Ulasli, Deniz Can Guven, Mehmet Ruhi Onur, Ilkay Tugba Unek, Huseyin Salih Semiz, Mustafa Erman, and et al. 2025. "Early Changes in Volumetric Body Composition Parameters Predict Survival Outcomes in Patients with Metastatic Renal Cell Carcinoma Treated with Targeted Therapy" Journal of Clinical Medicine 14, no. 9: 3140. https://doi.org/10.3390/jcm14093140
APA StyleAktepe, O. H., Erdemir, A. G., Caliskan Yildirim, E., Demirciler, E., Ulasli, T., Guven, D. C., Onur, M. R., Unek, I. T., Semiz, H. S., Erman, M., & Yalcin, S. (2025). Early Changes in Volumetric Body Composition Parameters Predict Survival Outcomes in Patients with Metastatic Renal Cell Carcinoma Treated with Targeted Therapy. Journal of Clinical Medicine, 14(9), 3140. https://doi.org/10.3390/jcm14093140






