Long-Term Outcomes of Cementless Versus Hybrid Cemented Total Knee Arthroplasty: A Minimum 10-Year Follow-Up
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgical Procedure
2.2. Study Parameters
2.3. Data Analyses
3. Results
3.1. Evaluable Cases and Demographic Comparison of Final Cohorts
3.2. Revisions
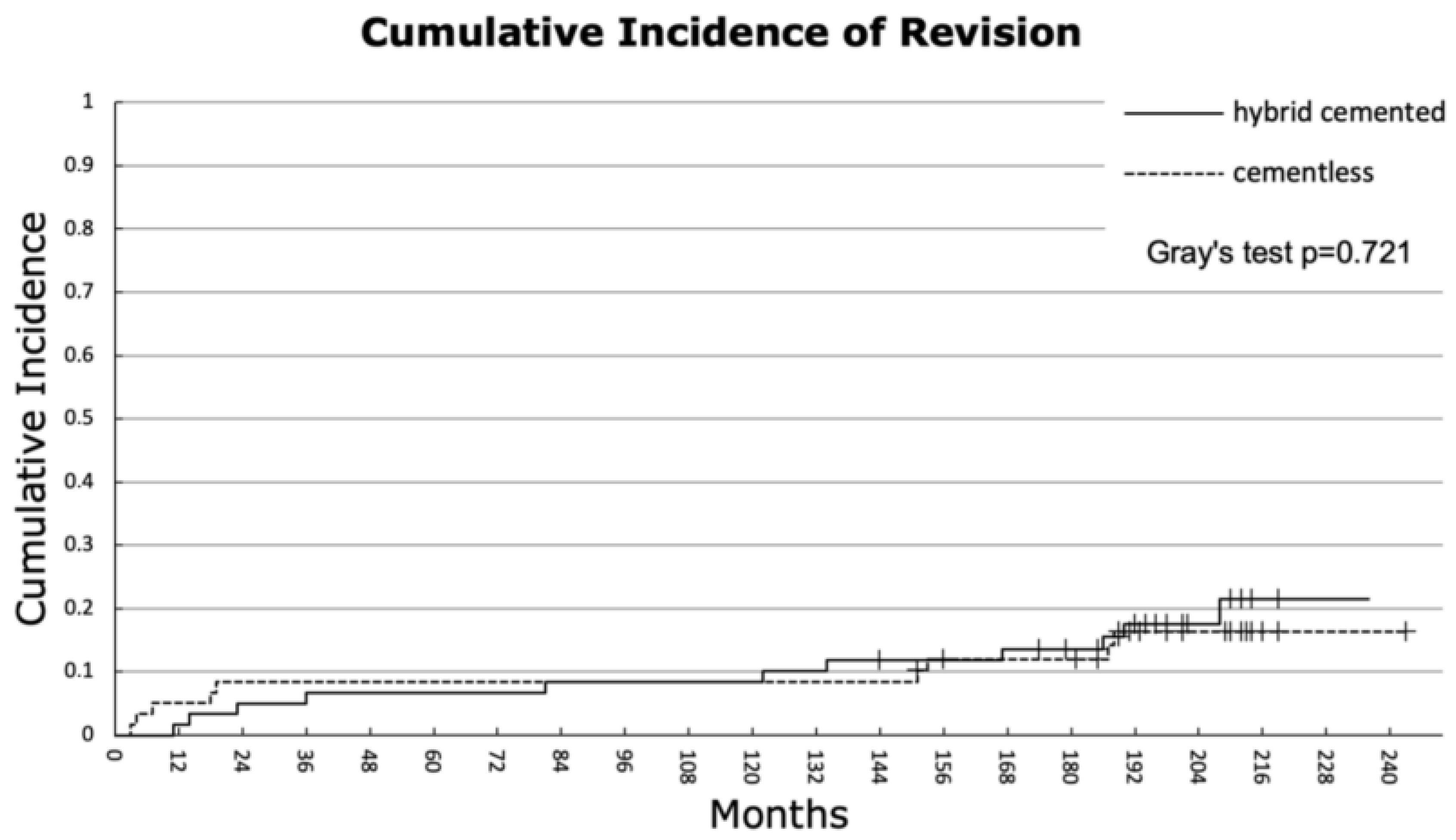
3.3. Cumulative Incidence and Competing Risk Analysis
3.4. Clinical Outcomes
3.5. Radiological Outcomes
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TKA | Total knee arthroplasty |
| KSS | Knee Society Score |
| BMI | Body Mass Index |
| IQR | Interquartile range |
| PE | Polyethylene |
| PJI | Periprosthetic joint infection |
| RCT | Randomized controlled trial |
| SD | Standard deviation |
References
- Shichman, I.; Roof, M.; Askew, N.; Nherera, L.; Rozell, J.C.; Seyler, T.M.; Schwarzkopf, R. Projections and Epidemiology of Primary Hip and Knee Arthroplasty in Medicare Patients to 2040–2060. JB JS Open Access 2023, 8, e22. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.; Ong, K.; Zhao, K.; Kelly, M.; Bozic, K.J. Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. Clin. Orthop. Relat. Res. 2009, 467, 2606–2612. [Google Scholar] [CrossRef]
- Julin, J.; Jämsen, E.; Puolakka, T.; Konttinen, Y.T.; Moilanen, T. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthop. 2010, 81, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Polizzotti, G.; Lamberti, A.; Mancino, F.; Baldini, A. New Horizons of Cementless Total Knee Arthroplasty. J. Clin. Med. 2023, 13, 233. [Google Scholar] [CrossRef]
- Duffy, G.P.; Berry, D.J.; Rand, J.A. Cement versus cementless fixation in total knee arthroplasty. Clin. Orthop. Relat. Res. 1998, 356, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.A.; Lyon, J.H.; Jacobs, J.J.; Barden, R.M.; Berkson, E.M.; Sheinkop, M.B.; Rosenberg, A.G.; Galante, J.O. Problems with cementless total knee arthroplasty at 11 years followup. Clin. Orthop. Relat. Res. 2001, 392, 196–207. [Google Scholar] [CrossRef]
- Hu, B.; Chen, Y.; Zhu, H.; Wu, H.; Yan, S. Cementless Porous Tantalum Monoblock Tibia vs Cemented Modular Tibia in Primary Total Knee Arthroplasty: A Meta-Analysis. J. Arthroplast. 2017, 32, 666–674. [Google Scholar] [CrossRef]
- Nam, D.; Bhowmik-Stoker, M.; Mahoney, O.M.; Dunbar, M.J.; Barrack, R.L. Mid-Term Performance of the First Mass-Produced Three-Dimensional Printed Cementless Tibia in the United States as Reported in the American Joint Replacement Registry. J. Arthroplast. 2023, 38, 85–89. [Google Scholar] [CrossRef]
- Hannon, C.P.; Salih, R.; Barrack, R.L.; Nunley, R.M. Cementless Versus Cemented Total Knee Arthroplasty: Concise Midterm Results of a Prospective Randomized Controlled Trial. J. Bone Jt. Surg. 2023, 105, 1430–1434. [Google Scholar] [CrossRef]
- van der Lelij, T.J.N.; Marang-van de Mheen, P.J.; Kaptein, B.L.; Toksvig-Larsen, S.; Nelissen, R.G.H.H. Continued Stabilization of a Cementless 3D-Printed Total Knee Arthroplasty: Five-Year Results of a Randomized Controlled Trial Using Radiostereometric Analysis. J. Bone Jt. Surg. Am. 2023, 105, 1686–1694. [Google Scholar] [CrossRef] [PubMed]
- Lass, R.; Kubista, B.; Holinka, J.; Pfeiffer, M.; Schuller, S.; Stenicka, S.; Windhager, R.; Giurea, A. Comparison of cementless and hybrid cemented total knee arthroplasty. Orthopedics 2013, 36, e420–e427. [Google Scholar] [CrossRef]
- Ewald, F.C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin. Orthop. Relat. Res. 1989, 248, 9–12. [Google Scholar] [CrossRef]
- Kumar, N.; Yadav, C.; Raj, R.; Anand, S. How to Interpret Postoperative X-rays after Total Knee Arthroplasty. Orthop. Surg. 2014, 6, 179–186. [Google Scholar] [CrossRef]
- Maradit Kremers, H.; Devick, K.L.; Larson, D.R.; Lewallen, D.G.; Berry, D.J.; Crowson, C.S. Competing Risk Analysis: What Does It Mean and When Do We Need It in Orthopedics Research? J. Arthroplast. 2021, 36, 3362–3366. [Google Scholar] [CrossRef] [PubMed]
- Hegde, V.; Stambough, J.B.; Levine, B.R.; Springer, B.D. Highlights of the 2022 American Joint Replacement Registry Annual Report. Arthroplast 2023, 21, 101137. [Google Scholar] [CrossRef] [PubMed]
- Asokan, A.; Plastow, R.; Kayani, B.; Radhakrishnan, G.T.; Magan, A.A.; Haddad, F.S. Cementless knee arthroplasty: A review of recent performance. Bone Jt. Open 2021, 2, 48–57. [Google Scholar] [CrossRef]
- Zhou, K.; Yu, H.; Li, J.; Wang, H.; Zhou, Z.; Pei, F. No difference in implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in primary total knee arthroplasty: A systematic review and meta-analysis. Int. J. Surg. 2018, 53, 312–319. [Google Scholar] [CrossRef]
- Kim, Y.H.; Park, J.W.; Lim, H.M.; Park, E.S. Cementless and cemented total knee arthroplasty in patients younger than fifty five years. Which is better? Int. Orthop. 2014, 38, 297–303. [Google Scholar] [CrossRef]
- Kim, Y.-H.; Park, J.-W.; Jang, Y.-S. The 22 to 25-Year Survival of Cemented and Cementless Total Knee Arthroplasty in Young Patients. J. Arthroplast. 2021, 36, 566–572. [Google Scholar] [CrossRef]
- Gibon, E.; Lewallen, D.G.; Larson, D.R.; Stuart, M.J.; Pagnano, M.W.; Abdel, M.P.; John, N. Insall Award: Randomized Clinical Trial of Cementless Versus Cemented Tibial Components: Durable and Reliable at a Mean 10-Years Follow-Up. J. Arthroplast. 2023, 38, S14–S20. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.R.; Yang, J.H. Unsatisfactory clinical outcomes of second-generation mobile bearing floating platform total knee arthroplasty: Comparing outcomes with fixed bearing after five years minimum. Int. Orthop. 2018, 42, 2583–2589. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-M.; Seo, J.-G.; Lim, S.-J.; Lim, H.-T.; Cho, C.-H.; Moon, Y.-W. Clinical performance and survivorship of navigated floating platform mobile-bearing total knee arthroplasty: A minimum 10-year follow-up. Int. J. Med. Robot. Comput. Assist. Surg. 2017, 13, e1833. [Google Scholar] [CrossRef]
- Lee, D.-H.; Lee, D.-K.; Shin, Y.-S.; Han, S.-B. Mid-term outcomes of floating platform mobile-bearing total knee arthroplasty under navigational guidance with a minimum 4-year follow-up. J. Arthroplast. 2013, 28, 1801–1815. [Google Scholar] [CrossRef]
- Prasad, A.K.; Tan, J.H.S.; Bedair, H.S.; Dawson-Bowling, S.; Hanna, S.A. Cemented vs. cementless fixation in primary total knee arthroplasty: A systematic review and meta-analysis. EFORT Open Rev. 2020, 5, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Costales, T.G.; Chapman, D.M.; Dalury, D.F. The Natural History of Radiolucencies Following Uncemented Total Knee Arthroplasty at 9 Years. J. Arthroplast. 2020, 35, 127–131. [Google Scholar] [CrossRef]
- Iosifidis, M.; Iliopoulos, E.; Neofytou, D.; Sakorafas, N.; Andreou, D.; Alvanos, D.; Kyriakidis, A. The Rotaglide mobile-bearing total knee arthroplasty: No difference between cemented and hybrid implantation. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1843–1848. [Google Scholar] [CrossRef]



| Demographic Data | All Patients n = 120 | Cementless n = 60 | Hybrid Cemented n = 60 | p-Value |
|---|---|---|---|---|
| Mean patient age, years (range) | 66.93 (33 to 90) | 65.72 (43 to 85) | 68.13 (35 to 90) | 0.189 * |
| Female patients, n (%) | 81 (67.50) | 35 (58.33) | 46 (76.67) | 0.032 †§ |
| Mean BMI kg/m2 (range) | 30.28 (19 to 51) | 30.03 (19 to 44) | 30.53 (23 to 51) | 0.615 * |
| L–R knees | 56:64 | 29:31 | 27:33 | 0.714 † |
| Operative time, minutes (range) | 130.71 (80 to 200) | 125.7 (80 to 175) | 135.7 (95 to 200) | 0.017 *§ |
| Primary diagnosis, n (%) | ||||
| Idiopathic arthritis | 106 (88.3) | 52 (86.7) | 54 (90.0) | 0.570 † |
| Posttraumatic arthritis | 6 (5) | 5 (8.3) | 1 (1.7) | 0.094 † |
| Rheumatoid arthritis | 4 (3.3) | 2 (3.3) | 2 (3.3) | 1.000 † |
| Avascular necrosis | 1 (0.8) | 1 (1.7) | 0 (0) | 0.331 † |
| Unicondylar knee arthroplasty | 3 (2.5) | 0 (0) | 3 (5) | 0.079 † |
| Demographic Data | All Patients n = 59 | Cementless n = 29 | Hybrid Cemented n = 30 | p-Value |
|---|---|---|---|---|
| Mean patient age, years (range) | 62.8 (35 to 78) | 61.8 (49 to 77.5) | 63.8 (35 to 78) | 0.234 a |
| Female patients, n (%) | 46 (78%) | 23 (79.41%) | 23 (76.7%) | 0.807 † |
| Mean BMI kg/m2 (range) | 30.3 (19 to 46) | 30 (19 to 37) | 30.5 (23 to 46) | 0.915 a |
| L–R knees | 26:33 | 12:17 | 14:16 | 0.683 † |
| Operative time, minutes (range) | 130.3 (80 to 190) | 125.4 (80 to 175) | 135.0 (98 to 190) | 0.162 a |
| Primary diagnosis, n (%) | ||||
| Idiopathic arthritis | 54 (91.6) | 28 (96.5) | 26 (86.7) | 0.353 † |
| Posttraumatic arthritis | 1 (1.7) | 0 (0) | 1 (3.3) | 1.000 † |
| Rheumatoid arthritis | 3 (5) | 1 (3.5) | 2 (6.7) | 1.000 † |
| Avascular necrosis | 0 (0) | 0 (0) | 0 (0) | - |
| Unicondylar knee arthroplasty | 1 (1.7) | 0 (0) | 1 (3.3) | 1.000 † |
| Reasons for Revision | All Patients (n = 120) | Cementless (n = 60) | Hybrid Cemented (n = 60) | p-Value |
|---|---|---|---|---|
| Polyethylene failure, n (%) | 7 (35) | 3 (15) | 4 (20) | 0.761 a |
| Aseptic loosening, n (%) | 6 (30) | 3 (15) | 3 (15) | 0.967 a |
| PJI, n (%) | 3 (15) | 0 (0) | 3 (15) | 0.087 a |
| Limited mobility, n (%) | 4 (15) | 3 (15) | 1 (5) | 0.299 a |
| Total, n (%) | 20 (100) | 9 (45) | 11 (55) | 0.721 a |
| Time to Revision | ||||
| Polyethylene failure, months (median, IQR) | 176.5 (151.5 to 187.7) | 152 (151.0 to 161.5) | 186 (167.0 to 190.0) | 0.761 a |
| Aseptic loosening, months (median, IQR) | 18.0 (8.5 to 79.0) | 10.5 (3 to 60.5) | 25 (14.0 to 57.5) | 0.967 a |
| PJI, months (median, IQR) | 46.0 (11 to 94.2) | 0 (0 to 0) | 46 (11.0 to 94.2) | 0.087 a |
| Limited mobility, months (median, IQR) | 7.0 (4.0 to 19.0) | 5.5 (4.0 to 10.0) | 23 (23.0 to 23.0) | 0.299 a |
| Overall time to revision (median, IQR) | 81.0 (14.0 to 167.0) | 18.5 (4.7 to 152.5) | 101.5 (20.7 to 171.7) | 0.721 a |
| KSS Outcome (Range) | Cementless (n = 24) | Hybrid Cemented (n = 22) | p-Value |
|---|---|---|---|
| Mean clinical score | |||
| Preoperative | 54.10 (10 to 95) | 45.40 (0 to 100) | 0.011 *§ |
| 5-year follow-up | 93.05 (55 to 100) | 89.17 (45 to 100) | 0.109 * |
| 10-year follow-up | 89.25 (65 to 100) | 88.18 (58 to 99) | 0.736 * |
| Mean functional score | |||
| Preoperative | 42.45 (0 to 69) | 46.10 (10 to 77) | 0.180 * |
| 5-year follow-up | 91.69 (64 to 100) | 90.52 (63 to 100) | 0.492 * |
| 10-year follow-up | 80.42 (30 to 100) | 80.00 (30 to 100) | 0.948 * |
| Mean total score | |||
| Preoperative | 96.52 (0 to 153) | 91.52 (44 to 142) | 0.291 * |
| 5-year follow-up | 184.75 (144 to 200) | 179.68 (113 to 200) | 0.146 * |
| 10-year follow-up | 168.63 (104 to 197) | 168.18 (93 to 199) | 0.480 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabitsch, L.; Vertesich, K.; Giurea, A.; Windhager, R.; Lass, R. Long-Term Outcomes of Cementless Versus Hybrid Cemented Total Knee Arthroplasty: A Minimum 10-Year Follow-Up. J. Clin. Med. 2025, 14, 3134. https://doi.org/10.3390/jcm14093134
Rabitsch L, Vertesich K, Giurea A, Windhager R, Lass R. Long-Term Outcomes of Cementless Versus Hybrid Cemented Total Knee Arthroplasty: A Minimum 10-Year Follow-Up. Journal of Clinical Medicine. 2025; 14(9):3134. https://doi.org/10.3390/jcm14093134
Chicago/Turabian StyleRabitsch, Lukas, Klemens Vertesich, Alexander Giurea, Reinhard Windhager, and Richard Lass. 2025. "Long-Term Outcomes of Cementless Versus Hybrid Cemented Total Knee Arthroplasty: A Minimum 10-Year Follow-Up" Journal of Clinical Medicine 14, no. 9: 3134. https://doi.org/10.3390/jcm14093134
APA StyleRabitsch, L., Vertesich, K., Giurea, A., Windhager, R., & Lass, R. (2025). Long-Term Outcomes of Cementless Versus Hybrid Cemented Total Knee Arthroplasty: A Minimum 10-Year Follow-Up. Journal of Clinical Medicine, 14(9), 3134. https://doi.org/10.3390/jcm14093134







