Abstract
Background: Intravitreal injections of vascular endothelial growth factor (VEGF) inhibitors are standard for diabetic macular edema (DME), yet a gap exists between clinical guidelines and actual practices. This study aimed to investigate the extent of deviation between physician-planned and actually performed treatment regimens. Methods: The PACIFIC study (NCT04847895) was a prospective, multicenter, non-interventional study conducted in Germany, the Netherlands, and Switzerland. A total of 910 patients with DME receiving ranibizumab were enrolled. Physicians documented the intended treatment regimen at baseline, and actual treatment patterns were retrospectively derived from the timing of visits and injections over a 24-month observation period. Results: Although most physicians initially planned fixed or pro re nata (PRN) regimens, 77% of pretreated and 73% of treatment-naïve patients ultimately followed a monitor and extend strategy. Treatment discontinuation was frequent (58.8% and 59.4%, respectively), and injection frequencies remained below recommended levels, although central retinal thickness improved over time. Conclusions: The study highlights a consistent and clinically relevant discrepancy between planned and actual treatment delivery in DME care, underscoring the need for better adherence to guideline-informed strategies in routine practice.
1. Introduction
Intravitreal injections of vascular endothelial growth factor (VEGF) inhibitors, such as ranibizumab, represent the standard of care for diabetic macular edema (DME). Various clinical trials have demonstrated the efficacy and safety of ranibizumab in treating DME [1,2,3,4]. In addition, researchers have published several studies demonstrating the effectiveness of ranibizumab in treating DME in a real-world setting. However, these studies have methodological limitations; for instance, previous studies did not compare the initially planned treatment regimen to the one actually performed [5,6,7,8]. In particular, the number of treatments was low in previous retrospective cohorts. According to the observational study design, there were several possible explanations: either only a few injections were initially agreed upon, a conscious or unconscious decision was made against further injections, or early withdrawal from longer follow-up distorted the figures.
Since clinicians often observe continuous but slow improvement under initial treatment and macular fluid needs time to decline [9], guidelines recommend intensive treatment, e.g., providing an initial series of injections, followed by further injections as needed (“pro re nata”) until maximum visual acuity is achieved (German guidelines [10]). Retina specialists consider the condition to be stable when the patient’s visual acuity remains unchanged and/or no signs of disease activity are detected during consecutive monthly tests. They monitor these parameters by assessing best corrected visual acuity (BCVA) and using optical coherence tomography (OCT) [11]. The initial intensity has been shown to be important for later outcomes [12,13,14]. After the first 6 months, a “treat and extend” regimen might be an excellent alternative to the “pro re nata” regimen, particularly if only one eye is affected [10].
The poorer outcome of crossover groups with late treatment started proved the impact on therapy outcomes [15]. Visual acuity at the start of therapy is an important prognostic factor for the level of visual acuity that can be reached by treatment [16,17,18,19,20,21]. Clearly, relatively good visual acuity at baseline limits “room for improvement” in terms of gains in letters. However, despite lower relative gains in letters, better absolute visual acuity can be achieved in these patients, and high visual acuity can be maintained in comparison to starting treatment with low visual acuity. Thus, the aim should be to diagnose DME as early as possible and initiate treatment immediately [22].
At the time of planning the PACIFIC study, no data regarding the efficacy of different treatment regimens used in routine clinical practice had been available. Thus, the PACIFIC study was conducted to determine the utilization and effectiveness of these various treatment regimens in routine clinical practice and their dependence on the application of different treatment regimens.
2. Materials and Methods
2.1. Study Design
The PACIFIC study was an observational, multicenter, open-label, single-arm study of patients with DME in Germany, the Netherlands, and Switzerland who were treated with ranibizumab.
Patient enrollment started in June 2015 and ended in March 2019. A minimum of one follow-up visit per year was required to maintain patient participation in the study over the prospective observational period of 24 months. This was a non-interventional study (NIS) in which no therapy, diagnostic/therapeutic procedure, or visit schedule was imposed.
2.2. Subjects
Patients could be included in the study if they were being treated with ranibizumab for any approved indication and gave written informed consent. Treatment-naïve (untreated) and pretreated patients were included. Pretreatment was defined as prior treatment with ranibizumab, other anti-VEGF drugs, intravitreal corticosteroids, photodynamic therapy, or laser coagulation before the start of the PACIFIC study (baseline). A total of 185 sites participated in the PACIFIC study, with 4948 patients in the safety evaluation set (SES) and 4932 patients in the full analysis set (FAS) for all indications. Of these, 913 patients in the SES cohort and 910 patients in the FAS had DME and were the subject of the present evaluation.
2.3. Statistical Methods
In the present analysis, descriptive summary statistics were calculated for the data from all the DME patients. Patient characteristics were documented at baseline. Variables such as details of ranibizumab injections and planned treatment regimens, BCVA examinations, OCT examinations, and adverse events (AEs) were documented at each visit. Diseases from medical history and AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA) version 24.0. For variables with predictive validity, appropriate strata were created. Statistics were calculated using the SAS software version 9.4 (SAS Institute, Cary, NC, USA). All safety-relevant analyses were performed for the SES, and all analyses relevant for utilization and effectiveness were performed for the FAS. Analyses were performed according to a predefined analysis plan.
The intended treatment regimens were documented by the treating physicians. The actual treatment regimens used were derived from the documented time points. Treatment regimens were defined as follows: “fixed” scheme, with regular intervals between follow-up visits and reinjection at every visit; “pro re nata”, with regular intervals between follow-up visits and reinjection as needed; “treat and extend”, with intervals between follow-up visits extended step by step and reinjection at every visit; and “monitor and extend”, with variable intervals between follow-up visits and reinjection as needed.
3. Results
3.1. Participants
A total of 913 patients with DME (in the SES) were enrolled in the PACIFIC study, and 910 patients were included in the FAS. Among those, 458 patients had previously received treatment, and 452 patients were treatment naïve. Most patients were from Germany (423 pretreated, 433 naïve), and few were from the Netherlands (19 pretreated, 0 naïve) or Switzerland (16 pretreated, 19 naïve). Among patients from Germany, the vast majority had public health insurance (92.0% of pretreated patients, 93.3% of treatment-naïve patients).
Demographics and baseline disease characteristics are shown in Table 1. Slightly more patients in the PACIFIC study were male, and the mean age was approximately 66 years for both pretreated and treatment-naïve patients. The mean baseline HbA1c value was approximately 52 mmol/mol for pretreated patients and 49 mmol/mol for treatment-naïve patients. The mean baseline BCVA, measured as early treatment diabetic retinopathy study (ETDRS) letters, was 66.3 of the ETDRS letters for pretreated patients compared to 64.1 of the ETDRS letters for treatment-naïve patients. Most patients had a baseline OCT examination, with a mean central retinal thickness of 330.0 µm for pretreated patients and 352.8 µm for treatment-naïve patients. The documented fundus lesions did not differ between the naïve and pretreated study participants (Appendix A, Table A1).

Table 1.
Demographics and baseline disease characteristics of patients with DME stratified by pretreatment status (FAS).
3.2. Treatments
Pretreated patients received a mean (±SD) number of 5.8 ± 2.9 injections (n = 266) of ranibizumab for the study eye in the first year (among those patients with documentation for at least the first year) and 10.6 ± 5.4 injections (n = 55) in two years (among those patients with documentation for at least two years). Treatment-naïve patients with DME received 6.4 ± 2.8 injections (n = 264) in the first year and 9.2 ± 4.5 injections (n = 52) in two years.
In the first 6 months, the pretreated patients had a mean (±SD) of 3.5 ± 1.6 injections. In the first 6 months, treatment-naïve patients had a mean (±SD) of 4.1 ± 1.5 injections.
The median time between the baseline BCVA examination and the first ranibizumab injection was 6 days (mean ± SD: 12.6 ± 17.1 days; n = 386) for pretreated patients with DME and 5 days (mean ± SD: 10.7 ± 15.1 days; n = 408) for treatment-naïve patients. The median time between subsequent study eye injections was 44.4 days (mean ± SD: 50.8 ± 23.1 days; n = 398) in pretreated patients and 39.2 days (mean ± SD: 45.1 ± 19.9 days; n = 432) in treatment-naïve patients.
The course of concomitant laser treatments over the observational period for treatment-naïve patients is shown in Figure 1. Concomitant laser treatments for pretreated patients are provided in Appendix A, Figure A1, and a cumulative depiction of treatment-naïve and pretreated patients is provided in Appendix A, Figure A2. Most patients who received concomitant laser treatments had at least one laser treatment within the first 6 months. In total, 9.0% of the pretreated patients and 15.1% of the treatment-naïve patients received concomitant laser treatments during the observational period.
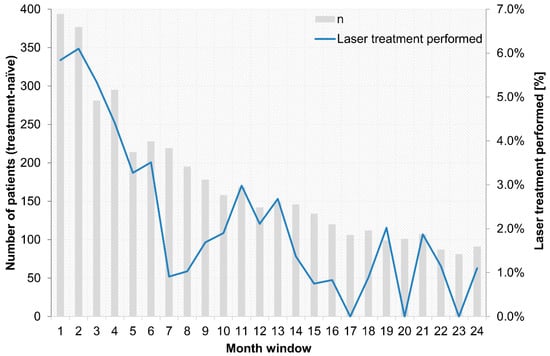
Figure 1.
Concomitant laser treatment over the 24-month observational period for treatment-naïve patients.
The pretreated patients remained in the documented study treatment for a median follow-up of 442 days, i.e., approximately 14.5 months, and treatment-naïve patients for a median of 453 days, i.e., approximately 15 months. Premature discontinuation of the study was documented for 258 of the 439 pretreated patients (58.8%) and for 252 of the 424 treatment-naïve patients (59.4%). The percentage of patients who prematurely discontinued the study was slightly greater among patients with renal insufficiency (68.0% of 25 pretreated patients, 88.9% of 18 treatment-naïve patients) and among patients with HbA1c >9% (66.7% of 21 pretreated patients, 68.4% of 19 treatment-naïve patients).
3.3. Treatment Regimens
The intended treatment regimens, as documented at baseline, as well as the actually performed treatment regimens in the last month, based on statistical derivation from temporal patterns of visits and injections, are shown in Figure 2. At baseline, a “fixed” scheme and “pro re nata” were the most commonly used treatment regimens. For pretreated patients, “pro re nata” was slightly more frequent (41% “pro re nata”, 34% “fixed”), while for treatment-naïve patients, a “fixed” scheme was more frequent (46% “fixed”, 35% “pro re nata”). However, overall, the treatment regimen used was “monitor and extend” for the majority of patients (77% of pretreated patients and 73% of treatment-naïve patients). The time-dependent trends in treatment regimens over 24 months are shown in Appendix A, Figure A3 and Figure A4 for pretreated and treatment-naïve patients, respectively.
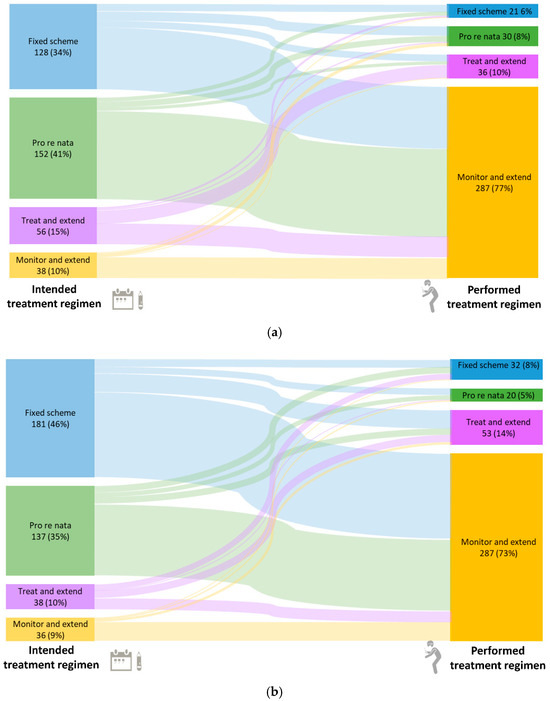
Figure 2.
Intended treatment regimens at baseline and actual treatment regimens in the last month for pretreated (a) and treatment-naïve (b) patients. Percentages are based on non-missing observations. In total, 443 pretreated patients had observations in the last month. Information on the treatment regimen was missing for 26 patients, and for 43 patients, the intended treatment regimen was changed during the study; therefore, these patients are not included in this figure. Of the 443 naïve patients with observations in the last month, 16 patients were missing information, and the intended treatment regimen was changed for 35 patients.
3.4. Visual Acuity
At the end of the observational period (month 24), the mean (±SD) BCVA was logMAR 0.270 ± 0.274 or 71.5 ± 13.7 of ETDRS letters (n = 71) for pretreated patients and logMAR 0.353 ± 0.330 or 67.3 ± 16.5 of ETDRS letters (n = 76) for treatment-naïve patients. Compared to the baseline BCVA, the BCVA of the study eye improved during each month of the study. The changes from baseline for pretreated and treatment-naïve patients are shown in Figure 3.
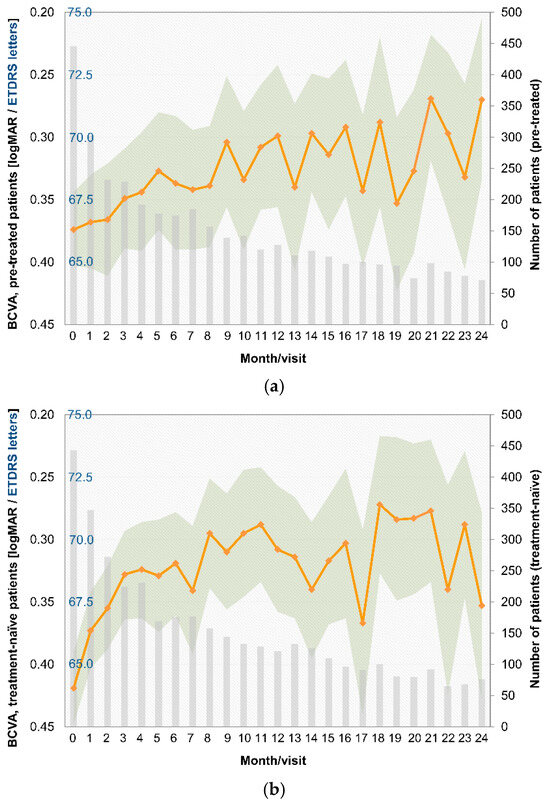
Figure 3.
BCVA by month, logMAR, and ETDRS values for pretreated (a) and treatment-naïve patients (b).
Pretreated patients received a total mean (±SD) number of 9.2 ± 5.2 OCT examinations of the study eye (n = 55), and treatment-naïve patients received 8.6 ± 5.7 OCT examinations (n = 52, among patients with documentation for at least two years). Decreases in the central retinal thickness of the study eye were observed at all visits compared to baseline. The course of central retinal thickness by study month is provided in Appendix A, Figure A5 for pretreated patients and in Appendix A, Figure A6 for treatment-naïve patients.
3.5. Adverse Events
Among pretreated patients, 41.2% (of 459 patients in the SES) experienced AEs. Severe AEs (SAEs) were reported for 27.7%, and serious adverse drug reactions (SADRs) were reported for 6.1%. The most frequently reported AEs were diabetic retinal edema (5.0%), cystoid macular edema (4.6%), retinal edema (4.1%), and concomitant disease aggravation (4.1%). Of a total of 551 AEs, 33.6% had mild intensity, 40.1% had moderate intensity, and 16.3% had severe intensity. The incidence of AEs was greater among pretreated patients with an HbA1c >9% (66.7% of 21 patients).
Among treatment-naïve patients, 33.5% (of 454 patients in the SES) experienced AEs. SAEs were reported for 22.5%, and SADRs were reported for 5.3%. The most frequently reported AEs were diabetic retinal edema (5.1%), cystoid macular edema (4.0%), concomitant aggravated disease (3.3%), and reduced visual acuity (3.1%). Of a total of 438 AEs, 33.3% had mild intensity, 40.2% had moderate intensity, and 16.9% had severe intensity.
4. Discussion
The PACIFIC study provides real-life data on therapy with ranibizumab in local routine clinical practice. It is noteworthy that this study was initiated before the latest publication of the German guidelines [10], which recommended treatment initiation by six monthly intravitreal injections of a VEGF inhibitor. Although the corresponding study data should be carefully interpreted due to certain limitations (selection bias, loss of documentation), five important observations can be made as conclusions about everyday treatment:
- (1)
- Over the last few years, a learning curve has been recognized, which is reflected in key parameters. The median treatment delay was 6 days for pretreated patients and 5 days for treatment-naïve patients in this study. This is notably shorter than in the preceding OCEAN study (conducted between 2011 and 2016), which reported a median treatment delay of approximately 21 days for DME patients [23]. This finding indicates an increased awareness of the importance of early treatment among ophthalmologists in recent years. Success and long-term preservation of visual function depend largely on the function at the start of treatment [24,25];
- (2)
- The intended treatment pattern showed notable differences compared to the actually performed regimen. At baseline, a “fixed” scheme and “pro re nata” were the most commonly used treatment regimens. This would have been in accordance with the DOG guidelines, which recommend a “fixed” scheme for the first 6 months, followed by “pro re nata” treatment [10]. However, in reality, these regimens were only performed for a small percentage of patients. This finding indicates that undertreatment is still an issue for DME patients [26]. Over the course of the observational period, a shift toward a “monitor and extend” regimen was observed based on the statistical derivation. It is possible that due to the study’s defined query and temporal limits, the data led to an interpretation of the study as a “monitor and extend” regimen in many cases, even if not intended by the physician. It seems important to look for unconscious influences and other relevant factors [27]. In the future, attention should be given to realistic agreements to improve the quality of educational discussions and provide informed consent;
- (3)
- Concomitant laser treatment has much less significance than described in clinical studies. Approximately 41–64% of treatment-naïve DME patients (DRCR.net Protocol T from 2012 to 2014) received at least one laser treatment over 2 years, and 23% of pretreated patients and 15% of treatment-naïve patients among the PACIFIC participants underwent concomitant laser treatment. However, it remains unclear whether this difference is ultimately due to the non-interventional nature of the study or to the basic philosophy of a less aggressive combined approach in Europe vs. the USA [28]. Presumably, both influences are likely to play a role if the decision to use a focal-grid laser in addition to anti-VEGF drugs does not follow a systematic algorithm. Although the stability of the achieved visual acuity gain is more relevant for retreatment than retinal morphology is, given the proportions of persistent fluid in DME [11], the strategy may not always be effective because of unclear expectations and perceived non-response. Although combined laser treatment did not show a general benefit in studies, there is indirect evidence for the benefits of targeted supplementary laser treatment over time [29];
- (4)
- The trend toward low treatment numbers was similar between naïve and pretreated patients. Pretreated patients in the PACIFIC study received a mean of 10.6 injections, and treatment-naïve patients received 9.2 injections (among those patients with documentation for at least two years). Thus, patients received notably more injections than in the previous observational OCEAN study (5.5 injections) [30], but still fewer injections than in clinical trials [31,32];
- (5)
- Treatment discontinuation is still a relevant problem in this treatment indication [33]. Aggravated general conditions often cause patients to discontinue treatment. In the PACIFIC study, patients with very high HbA1c values (>9%) were more likely to be discontinued prematurely and experience more AEs. There were no major outliers in terms of insurance or race, but the analyzed cohort was quite homogeneous and of Central European ancestry [34].
The efficacy of the treatment was assessed in representative cohorts. However, by providing real-life data on DME therapy, observational insights from routine clinical practice may lead to a better understanding of the status quo and challenges in patient health care in real-life settings [35,36].
Earlier studies were unable to reveal the considerable deviations between original planning and actual implementation because the planning perspective was not recorded. Specifically, the findings raise the question of whether and to what extent practitioners are aware of the pathways to undertreatment and treatment discontinuation. Overt or hidden resistance, if not the justified and clearly articulated will of the patient, can be relevant. This makes it all the more important that the opportunities for better information—including the relevance of the necessary adherence—are utilized in the future [37].
5. Conclusions
In summary, compared with those of previous studies, the present study showed a slight improvement in the real-world treatment of DME patients with regard to treatment delay and the number of injections given during the first year of treatment. However, the current local recommendations [10], suggesting intensive treatment (e.g., comprising six monthly injections followed by further injections based on specific reinjection criteria), were not achieved.
Although regimens clearly define the sequence of control of morphological parameters, fixed re-treatment and determination of the interval for the ‘treat and extend‘ regime, the actual observed behavior after appropriate planning corresponded to completely different patterns. Various factors may contribute to the lack of regular re-treatment while extending, and patients interrupting or terminating the strategy despite the need for intensive treatment.
Deviations in the execution of the plans definitely occur. The search for the reasons and causes can help to improve the treatment of DME in different healthcare settings.
Author Contributions
C.H., M.I., B.M. and F.Z. designed the study. C.H. and B.M. developed the methodology. All the authors were involved in the formal analysis and investigation. C.H., M.I. and F.Z. wrote the main manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Novartis Pharma GmbH, Germany.
Institutional Review Board Statement
This study was conducted in accordance with relevant guidelines and with the ethical principles of the Declaration of Helsinki. The study was approved by the ethics committee responsible for the study site of the principal investigator (Ethik-Kommission der Bayerischen Landesärztekammer, Ethics Approval Number 15024 and date of approval 15 May 2015), as well as by local ethics committees in the Netherlands (METC [Medisch Ethische Toetsings Commissie] Brabant and CGR [Codecommissie Geneesmiddelen Reclame]) and in Switzerland (EKNZ [Ethikkommission Nordwest- und Zentralschweiz]).
Informed Consent Statement
Every patient was informed by the treating physician about the key objectives as well as the type and scope of the documentation. Eligible patients could only be included in the study after providing written informed consent or, if incapable of doing so, after such consent had been provided by a legally acceptable representative of the patient.
Data Availability Statement
Patients provided signed informed consent for the publication of their data.
Acknowledgments
We want to thank all participating patients of the PACIFIC study.
Conflicts of Interest
Christos Haritoglou received honoraria as a speaker from Novartis, Bayer, and Allergan/AbbVie. Matthias Iwersen and Bettina Müller are employees of Novartis Pharma GmbH, Germany. Erik Beeke received a grant from Novartis. Hüsnü Berk declares no conflicts of interest outside the study participation fees. Matthias Grüb received grants from Novartis and Bayer and personal fees from Novartis. Katrin Lorenz received honoraria from Ethikkommission der Landesärztekammer Rheinland-Pfalz and Novartis Pharma GmbH, travel grants from Novartis Pharma GmbH, and participated in the following clinical trials/grants: Aerie, Allergan, Amgen, Bayer, Chengdu Kanghong Biotechnology Co., Hexal, Hoya, iStar, Iveric Bio, Janssen Cilag, Implandata, Lumithera, Microoptx, Mylan, Novartis, Ophtea limited, Pfizer, Redwood, Roche, Sensimed, and Santen. Martin Scheffler declares no conflicts of interest outside the study participation fees. Focke Ziemssen received grants or personal fees from Acelyrin, Alimera, Allergan/Abbvie, Apellis, Bayer Healthcare, BDI, Biogen, Boehringer-Ingelheim, Clearside, CME Health, Ionis, Janssen, Kodiak, Novartis, NovoNordisk, MSD Sharp & Dohme, Oxurion, ODOS, Ophtea, Regeneron, Roche/Genentech, Sandoz, Sanofi, and Stada.
Abbreviations
The following abbreviations are used in this manuscript:
| DME | Diabetic Macular Edema |
| VEGF | Vascular Endothelial Growth Factor |
| OCT | Optical Coherence Tomography |
| BCVA | Best Corrected Visual Acuity |
| NIS | Non-Interventional Study |
| SES | Safety Evaluation Set |
| FAS | Full Analysis Set |
| AEs | Adverse Events |
| SAEs | Severe Adverse Events |
| SADRs | Serious Adverse Drug Reactions |
| MedDRA | Medical Dictionary for Regulatory Activities |
| DOG | Deutsche Ophthalmologische Gesellschaft (German Ophthalmological Society) |
Appendix A

Table A1.
Most common ophthalmological findings (>10%) of the study eye at baseline.
Table A1.
Most common ophthalmological findings (>10%) of the study eye at baseline.
| Ophthalmological Findings, n (%) a | Pre-Treated N = 458 | Treatment-Naïve N = 452 |
|---|---|---|
| Subretinal fluid with foveal involvement | 142 (31.00%) | 170 (37.61%) |
| Subretinal fluid without foveal involvement | 47 (10.26%) | 66 (14.60%) |
| Cystoid fluid inclusion with foveal involvement | 265 (57.86%) | 274 (60.62%) |
| Cystoid fluid inclusion without foveal involvement | 127 (27.73%) | 158 (34.96%) |
| Diffuse retinal thickening | 183 (39.96%) | 153 (33.85%) |
| Ischemic areas | 55 (12.01%) | 59 (13.05%) |
| Bleeding or punctate bleeding | 275 (60.04%) | 288 (63.72%) |
| Exudate | 155 (33.84%) | 158 (34.96%) |
| Intraretinal microvascular anomalies | 76 (16.59%) | 62 (13.72%) |
| Proliferative diabetic retinopathy | 63 (13.76%) | 74 (16.37%) |
| Cataract | 142 (31.00%) | 140 (30.97%) |
a Multiple responses permitted. N: number of patients in analysis set, n: number of non-missing observations.
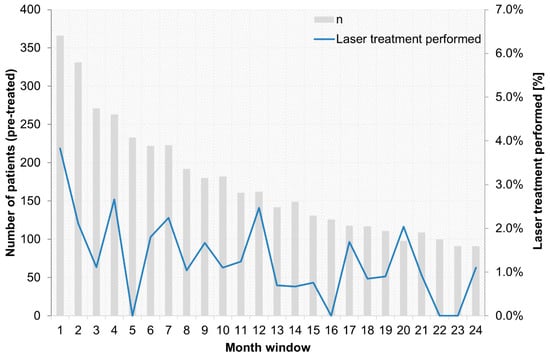
Figure A1.
Concomitant laser treatment over the 24-month observational period for pre-treated patients.
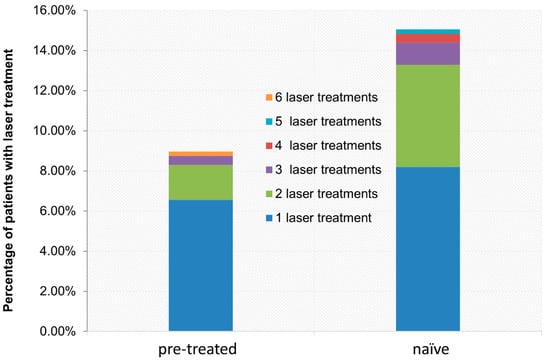
Figure A2.
Cumulative percentages of concomitant laser treatments for pre-treated and treatment-naïve patients.
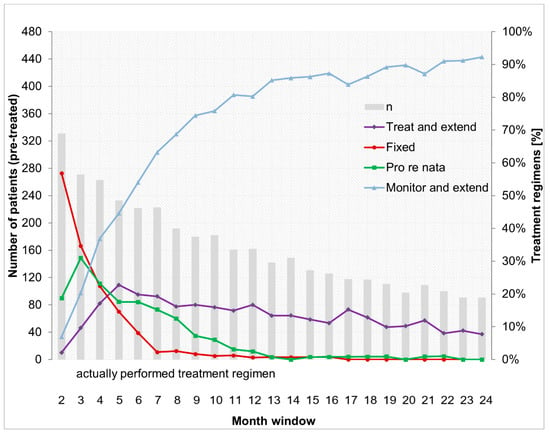
Figure A3.
Actually performed treatment regimens over the 24-month observational period for pre-treated patients.
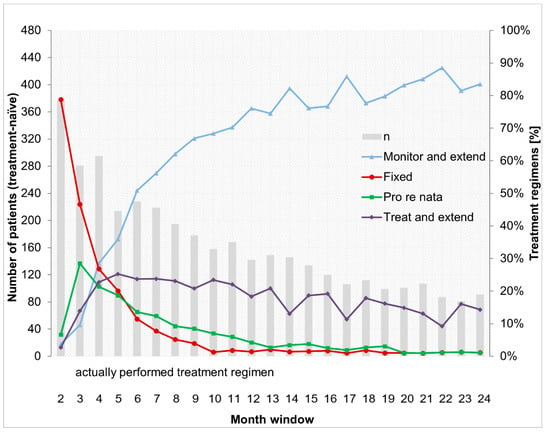
Figure A4.
Actually performed treatment regimens over the 24-month observational period for treatment-naïve patients.
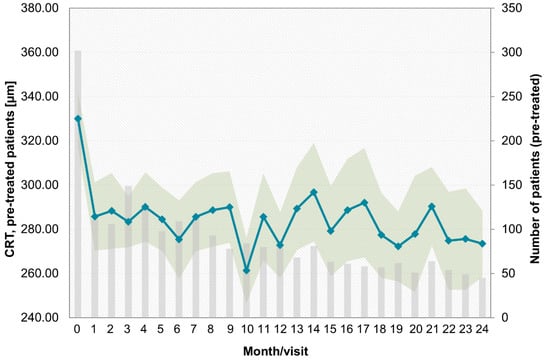
Figure A5.
Central retinal thickness (CRT) by month for pre-treated patients.
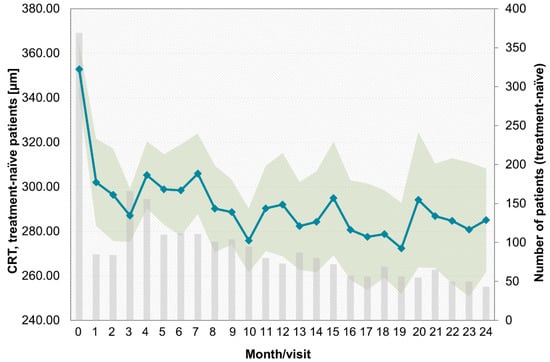
Figure A6.
Central retinal thickness (CRT) by month for treatment-naïve patients.
Appendix B

Table A2.
List of PACIFIC study investigators.
Table A2.
List of PACIFIC study investigators.
| PI | Center | Location |
|---|---|---|
| Christos Haritoglou | Gemeinschaftspraxis Profs. Haritoglou, Schultheiß, Klink | Munich |
| Martin Bechmann | Augenklinik Airport GmbH | Munich Airport |
| Daniela Erhard | Augenklinik Airport GmbH | Munich Airport |
| Shervin Mir Mohi Sefat | Augenklinik Airport GmbH | Munich Airport |
| Gabriele Kuba | Praxis Gabriele Kuba | Munich |
| Ines Lanzl | Institut Rund ums Auge, I. Lanzl & W. Reich | Prien/Chiemsee |
| Richard Wertheimer | Augenärzte im Arabellahaus, Richard Wertheimer, Katharina Wittmer | Munich |
| Udo Heuer | MEC Augenärzte, Udo Heuer | Hamburg |
| Angela Timm | Augenärztliche Gemeinschaftspraxis. M. Bayer, H. Schneider und A. Timm | Wismar |
| Bertram Machnik | Praxis Bertram Machnik | Hamburg |
| Peter Kaupke | Gemeinschaftspraxis Kaupke, Görges, Miebach und Ehrich | Hamburg |
| Semse Özmen | Augenarztpraxis Gemeinschaftspraxis Wedel | Wedel |
| Christine Onken | Augenarztpraxis Gemeinschaftspraxis Wedel | Wedel |
| Soheyl Asadi | Praxis Augenärzte am Weidenbaumsweg | Hamburg |
| Smbat Berger | Smbat Berger | Bremerhaven |
| Martin Winter | Praxis Martin Winter | Bremen |
| Martin Scheffler | Praxis Martin Scheffler | Rhauderfehn |
| Stephan Kilias | Gemeinschaftspraxis Kilias und Fetter | Hoppegarten |
| Janek Häntzschel | Gemeinschaftspraxis Häntzschel, Later | Pirna |
| Linda Later | Gemeinschaftspraxis Häntzschel, Later | Pirna |
| Marc Marré | Gemeinschaftspraxis Marc Marré | Dresden |
| Lada Matschke | Praxis Lada Matschke | Neubrandenburg |
| Kyra Lauritzen | Kyra Lauritzen | Buchholz i.d.N. |
| Bilal Chamat | Berlin Eye Clinic, Bilal Chamat, FEBO | Berlin |
| Stefan Heinrich | Praxis Stefan Heinrich | Berlin |
| Mehrinfar Ben | Gemeinschaftspraxis Dres. Pahlitzsch, Grüngreiff | Berlin |
| Kathleen Steinberg | Praxis Kathleen Steinberg | Berlin |
| Jochen Thieme | Jochen Thieme | Berlin |
| Mohammed O. Ramez | Praxis M. Osman Ramez | Buxtehude |
| Malek Moubid | Augenarztpraxis Malek Moubid | Buxtehude |
| Christoph Wehner | Praxis Christoph Wehner, Andreas Meyer-Rößler | Bremervörde |
| Mayk Steiner | Gemeinschaftspraxis Anke Steiner und Mayk Steiner | Dannenberg |
| Anke Steiner | Gemeinschaftspraxis Anke Steiner und Mayk Steiner | Dannenberg |
| Alper Bilgic | Alpha Vision Alper Bilgic, Ahmed Galal | Bremerhaven |
| Peter Ruokonen | Gemeinschaftspraxis Baecker und Ruokonen | Berlin |
| Anaelle Laurent | Augenklinik Berlin-Marzahn GmbH | Berlin |
| Sorin Draghici | Augenarztpraxis Draghici & Kontopoulos | Berlin |
| Theodoros Kontopoulos | Augenarztpraxis Draghici & Kontopoulos | Berlin |
| Mirjam Gross | Augenarztpraxis für Gross und Klein | Berlin |
| Thomas Kube | Praxis Thomas Kube | Bielefeld |
| Erik Beeke | Visual eins Ärztehaus-Praxis/Klinik | Osnabrück |
| Susanne Eller-Woywod | Augenärzte Goldmann, Dr.Engels, Dr.Grotheheide, Dr.Eller-Woywod | Gütersloh |
| Sabine Kaps | Sabine Kaps | Obernkirchen |
| Nikolai Holak | Nikolai Holak | Salzgitter |
| Ole Krüger | Augenärzte am Bankplatz Dres. Heinichen, Ahrens, Krüger | Braunschweig |
| T. Heinichen | Augenärzte am Bankplatz Dres. Heinichen, Ahrens, Krüger | Braunschweig |
| S. Heinichen | Augenärzte am Bankplatz Dres. Heinichen, Ahrens, Krüger | Braunschweig |
| M. Ahrens | Augenärzte am Bankplatz Dres. Heinichen, Ahrens, Krüger | Braunschweig |
| Annette Handstein | Praxis Annette Handstein | Paderborn |
| Sandra Festag | Sandra Festag | Petershagen |
| Christof Lenz | Christof Ulrich Lenz | Paderborn |
| Frank-Christian Nickel | Frank Nickel-Augenärztliche Gemeinschaftspraxis | Peine |
| Alexander Petzold | Augenzentrum am Johannisplatz, Alexander Petzold | Leipzig |
| Thomas Hammer | Praxis Thomas Hammer | Halle (Saale) |
| Gernot Duncker | Gernot Duncker-MVZ Augenheilkunde Mitteldeutschland GmbH | Halle (Saale) |
| Kerstin Hellmund | Praxis Kerstin Hellmund | Dresden |
| Matthias Müller-Holz | Überörtliche Gemeinschaftspraxis, Matthias Müller-Holz | Dresden |
| Tobias Riedel | Überörtliche Gemeinschaftspraxis, Matthias Müller-Holz | Dresden |
| Regina Matthes | Praxis Regina Matthes | Dresden |
| Nasser Al-Ashi | Oberlausitz Kliniken gGmbH, Nasser Al-Ashi | Bautzen |
| Jakub Chmielowski | Praxis Jakub Chmielowski | Plauen |
| Simo Murovski | Praxis Simo Murovski | Zschopau |
| Stephan Kretschmar | Praxis Stephan Kretschmar | Bautzen |
| Dirk Pohlmann | Augenzentrum Osthessen | Fulda |
| Houcem Ghribi | Houcem Ghribi | Gifhorn |
| Wolfram Lieschke | Praxis Wolfram Lieschke | Leipzig |
| Christian Ksinsik | Augenarztpraxis am Glacis | Torgau |
| Alain de Alba Castilla | Augenarztpraxis am Glacis | Torgau |
| Jorge Cantu Dibildox | Augenarztpraxis am Glacis | Torgau |
| Alexander Goldberg | Alexander Goldberg | Coswig |
| Alexander Stoll | Praxis Alexander Stoll | Chemnitz |
| Agnes Ute Porstmann | Elbland Augenzentrum am Elblandklinikum-Agnes Ute Porstmann | Radebeul |
| Gregor Schwert | MVZ Beckum I-Röschinger, Grewe und Schwert | Beckum |
| Ulrich Thelen | Augenärzte Klosterstraße | Münster |
| Elisabeth Bator-Banasik | GP Elisabeth Bator-Banasik, Heidi Fischer | Ahaus |
| Farsad Fanihagh | Gemeinschaftspraxis Ch.-L. Kallmann und F. Fanihagh | Ratingen |
| Stephan Dunker | Praxis Stephan Dunker | Troisdorf |
| Maren Unger | Augenzentrum Brühl | Brühl |
| Frederik Wiegand | Gemeinschaftspraxis Radetzky, Jurek-Becker und Looke, Frederik Wiegand | Neuwied |
| Hendrik Fuchs | Belenus Augenzentrum Siegen Service GbR | Siegen |
| Hans-Ulrich Frank | Belenus Augenzentrum Siegen Service GbR | Siegen |
| Omar Mohamed Alnahrawy | Augencentrum Koblenz, M. Derse, C. Papoulis und Kollegen | Koblenz |
| Andreas Schmidt | Augenzentrum Andernach Andreas Schmidt, C. Schmidt-Dudziak | Andernach |
| Christian Abel | Praxis Christian Abel | Trier |
| Markus Strauß | Praxis Markus Strauß | Saarbrücken |
| Stefan Pfennigsdorf | Praxis Stefan Pfennigsdorf | Polch |
| Eduard Berenstein | Augencentrum Koblenz-Höhr-Grenzhausen Derse, Papoulis und Kollegen | Höhr-Grenzhausen |
| Tatyana Lazarova-Hristova | Praxis Fazil Peru | Frankfurt |
| Stefan Müller | Praxis Stefan Müller | Neustadt |
| Martin Rauber | Gemeinschaftspraxis Zuche und Rauber | Saarburg |
| Andreas Liermann | Andreas Liermann | Neustadt |
| Isolde Olivas | Praxis Isolde Olivas | Heddenheim |
| Martin Mundschenk | Praxis Martin Mundschenk | Worms |
| Gerber Tina | Praxis Tina Gerber | Mutterstadt |
| Viktor Gossmann | Praxis Viktor Gossmann | Ludwigshafen |
| Babak Mohammadi | Praxis Babak Mohammadi | Düsseldorf |
| Hakan Kaymak | Breyer, Kaymak und Klabe Augenchirurgie | Düsseldorf |
| Johannes Bohnen | LUMEDICO Johannes Bohnen | Düsseldorf |
| Matthias Grüb | Praxis Matthias Grüb | Breisach |
| Andrea Wißmann | Praxis Hartmut Karl König | Baden-Baden |
| Anita Lis-Kowalczyk | Praxis Anita Lis-Kowalczyk | Freudenstadt |
| Dirk Eberhardt | Gemeinschaftspraxis B. Entenmann und D. Eberhardt | Waldshut-Tiengen |
| Beatrix Entenmann | Gemeinschaftspraxis B. Entenmann und D. Eberhardt | Waldshut-Tiengen |
| David Schell | Praxis David Schell | Memmingen |
| Christian Scherer | Gemeinschaftspraxis Renata Scherer und Christian Scherer | Augsburg |
| Thilo Schimitzek | Augenklinik Kempten, Thilo Schimitzek | Kempten |
| Marianne Liedtke-Maier | Augen-Diagnostik-Zentrum Maier, Liedtke-Maier | Hösbach |
| Othmar Keller | Überörtliche BAG Othmar Keller, Susanne Müller | Herrsching |
| Jürgen Garus | Praxis Jürgen Garus | Pfaffenhofen an der Ilm |
| Uwe Schütz | GP Nikolaus Hillenbrand, Uwe Schütz | Ehingen |
| Christian Schäferhoff | Christian Schäferhoff | Esslingen |
| Barbara Fuchs-Koelwel | Barbara Fuchs-Koelwel | Regensburg |
| Klaus Königsreuther | Praxis Klaus Königsreuther | Eckental/Eschenau |
| Christoph Winkler v. Mohrenfels | Praxis Christoph Winkler v. Mohrenfels | Neutraubling |
| Magda Rau | Privatklinik Rau | Cham |
| Thomas Brandl | Praxis Thomas Brandl | Straubing |
| Georgios Siochos | Praxis Georgios Siochos | Karlsfeld |
| Janna Harder | Janna Harder | Munich |
| Stephan Eckert | Gemeinschaftspraxis Kemmerling und Eckert | Sindelfingen |
| Kamil Weinhold | Praxis Kamil Weinhold | Karlsruhe |
| Axel Hautzinger | Augenärzte Dres. Reichert und Hautzinger | Frankenthal |
| Ralph Maria Alles | Praxis Ralph Maria Alles | Saarlouis |
| Ralf Schmitt | Augen-Zentrum im Medizeum, Ralf Schmitt | Saarbrücken |
| Susanne Grewing | GP Ralf Grewing und Kollegen | Kaiserslautern |
| Michael Kusber | Michael Kusber | Bad Arolsen |
| Björn Feldner | Augenärztliches MVZ Friedländer Weg-Dres. Genée, Feldner und Kolck-Bölling | Göttingen |
| Stefan Kienzle | Praxis Kienzle, Lojewski und Nolte | Herzberg |
| Christian Gittner | Christian Gittner | Einbeck |
| Pia Kirchner | Gemeinschaftspraxis Schröder, Hoerauf, Pia Kirchner | Göttingen |
| Waldemar Jendritza | Praxis Dres. Jendritza | Ludwigshafen |
| Annette Brusis | Praxis Annette Brusis | Heppenheim |
| Harry Domack | Gemeinschaftspraxis Domack, Best und Schmidt | Schweinfurt |
| Peter Lang | Gemeinschaftspraxis H. Lang, P. Lang, K. Gottschalk | Nürnberg |
| Judith Becker | Überörtliche BAG Haupt, Spraul, Teuchert und Zorn | Ulm |
| Carolin Schwamberger | MVZ Augen Rombold, Niederdellmann und Kollegen | Friedberg |
| Martin Lambert | ÜöBAG Dankwart, Schmidl. Lambert, Schmidt | Rüsselsheim |
| Frank Koch | Goethe-Universität Frankfurt am Main-Augenklinik | Frankfurt |
| Svenja Deuchler | Goethe-Universität Frankfurt am Main-Augenklinik | Frankfurt |
| Ninel Kenikstul | Goethe-Universität Frankfurt am Main-Augenklinik | Frankfurt |
| Pankaj Singh | Goethe-Universität Frankfurt am Main-Augenklinik | Frankfurt |
| Katrin Lorenz | Universitätsmedizin der Johannes Gutenberg-Universität Mainz | Mainz |
| Anna Beck | Universitätsmedizin der Johannes Gutenberg-Universität Mainz | Mainz |
| Helmut Sachs | Städtisches Klinikum Dresden | Dresden |
| Merle Schrader | Carl von Ossietzky Universität Oldenburg | Oldenburg |
| Sabine Aisenbrey | Carl von Ossietzky Universität Oldenburg | Oldenburg |
| Guido Esper | Carl von Ossietzky Universität Oldenburg | Oldenburg |
| Menelaos Pipilis | Carl von Ossietzky Universität Oldenburg | Oldenburg |
| Roland Richter | Augenärzte am Brand 12-Dres. Müller-Richter-Coracas | Mainz |
| Gregor Eberlein | Klinikum Augsburg AöR-Klinik für Augenheilkunde | Augsburg |
| Arthur Mueller | Klinikum Augsburg AöR-Klinik für Augenheilkunde | Augsburg |
| Jürgen Pleines | ZG Zentrum Gesundheit GmbH | Leer |
| Dieter Hagedorn | ZG Zentrum Gesundheit GmbH | Leer |
| Klaas Heidemann | ZG Zentrum Gesundheit GmbH | Leer |
| Nikolaus Lohmann | ZG Zentrum Gesundheit GmbH | Leer |
| Matthias Meyer | ZG Zentrum Gesundheit GmbH | Leer |
| Nakisa Amiri | ZG Zentrum Gesundheit GmbH | Leer |
| Michael Witteborn | ZG Zentrum Gesundheit GmbH | Leer |
| Hansgeorg Albrechtr | ZG Zentrum Gesundheit GmbH | Leer |
| Claudia Lanzrath | Berufsausübungsgemeinschaft Zentrum Gesundheit Oldenburg GbR | Oldenburg |
| Daniela Fromm | Berufsausübungsgemeinschaft Zentrum Gesundheit Oldenburg GbR | Oldenburg |
| Ramin Khoramnia | Universitäts-Augenklinik Heidelberg | Heidelberg |
| Gerd Auffarth | Universitäts-Augenklinik Heidelberg | Heidelberg |
| Dirk Sandner | GWT-TUD GmbH Sandner | Dresden |
| Matthe Egbert | GWT-TUD GmbH Sandner | Dresden |
| Hüsnü Berk | St. Elisabeth Krankenhaus Köln-Hohenlind Berk | Cologne |
| V. Romanou-Papadopoulou | MVZ der Klinik Dardenne GmbH, Vassiliki Romanou-Papadopoulou | Bonn-Bad Godesberg |
| Hans-Wilhelm Große | MVZ der Klinik Dardenne GmbH, Vassiliki Romanou-Papadopoulou | Bonn-Bad Godesberg |
| Jasmin Bartling | MVZ der Klinik Dardenne GmbH, Vassiliki Romanou-Papadopoulou | Bonn-Bad Godesberg |
| Helmut Höh | Dietrich-Bonhoeffer-Klinikum | Neubrandenburg |
| Mathias Schwanengel | Dietrich-Bonhoeffer-Klinikum | Neubrandenburg |
| Salvatore Grisanti | Universitätsklinikum Schleswig-Holstein-Klinik für Augenheilkunde | Lübeck |
| Martin Rudolf | Universitätsklinikum Schleswig-Holstein-Klinik für Augenheilkunde | Lübeck |
| Matthias Lüke | Universitätsklinikum Schleswig-Holstein-Klinik für Augenheilkunde | Lübeck |
| Mahdy Ranjbar | Universitätsklinikum Schleswig-Holstein-Klinik für Augenheilkunde | Lübeck |
| Laurenz Sonnentag | Universitätsklinikum Schleswig-Holstein-Klinik für Augenheilkunde | Lübeck |
| Thomas Ach | Universitätsklinikum Würzburg Thomas Ach | Würzburg |
| Jost Hillenkamp | Universitätsklinikum Würzburg Thomas Ach | Würzburg |
| Kerstin Stange | Augenarztpraxis Stange und Langner | Borna |
| Andrea Langner | Augenarztpraxis Stange und Langner | Borna |
| Ulrich Schaudig | Asklepios Kliniken Hamburg GmbH-Asklepios Klinik Barmbek | Hamburg |
| Kais Al-Samir | Asklepios Kliniken Hamburg GmbH-Asklepios Klinik Barmbek | Hamburg |
| Birthe Stemplewitz | Asklepios Kliniken Hamburg GmbH-Asklepios Klinik Barmbek | Hamburg |
| Katinka Westermann-Lammers | Asklepios Kliniken Hamburg GmbH-Asklepios Klinik Barmbek | Hamburg |
| Gelareh Winter | Asklepios Kliniken Hamburg GmbH-Asklepios Klinik Barmbek | Hamburg |
| Peter Großkopf | Augenzentrum Hochrhein | Bad Säckingen |
| Gudrun Papadopoulos | Augenzentrum Hochrhein | Bad Säckingen |
| Sebastian Tudor | Augenzentrum Hochrhein | Bad Säckingen |
| Olga Sartorius | Praxis Olga Sartorius | Erkrath |
| Focke Ziemssen Focke | Universitäts-Augenklinik Tübingen, Focke Ziemssen | Tübingen |
| Véronique Kitiratschky | Ortenau Klinikum Offenburg-Gengenbach-St. Josefsklinik | Offenburg |
| Amin Gamael | MVZ der Universitätsmedizin Rostock | Rostock |
| Joachim Schmidt | Lichtblick MVZ Moers GmbH | Moers |
| Roland Koch | Lichtblick MVZ Moers GmbH | Moers |
| Stefanie Schmickler | Augen-Zentrum-Nordwest (MVZ) | Ahaus |
| Olaf Cartsburg | Augen-Zentrum-Nordwest (MVZ) | Ahaus |
| Jens Schrecker Jens | Rudolf Virchow Klinikum Glauchau gGmbH | Glauchau |
| Ute Jüst | Rudolf Virchow Klinikum Glauchau gGmbH | Glauchau |
| Chris P. Lohmann | Klinikum rechts der Isar-Augenklinik und Poliklinik | Munich |
| Georg Spital | Augenärzte am St. Franziskus-Hospital | Münster |
| Frederike Hochhaus | Frederike Hochhaus | Bockhorn |
| Berthold Seitz | Universität des Saarlandes | Homburg/Saar |
| Karl-Heinz Emmerich | Klinikum Darmstadt GmbH | Darmstadt-Eberstadt |
| Andreas Krieb | Klinikum Darmstadt GmbH | Darmstadt-Eberstadt |
| Monica Lang | Klinikum Darmstadt GmbH | Darmstadt-Eberstadt |
| Ralf Ungerechts | Klinikum Darmstadt GmbH | Darmstadt-Eberstadt |
| Christoph Ehlken | Universitätsklinikum Schleswig-Holstein, Campus Kiel | Kiel |
| Claus von der Burchard | Universitätsklinikum Schleswig-Holstein, Campus Kiel | Kiel |
| Anna-Maria Kirsch | Universitätsklinikum Schleswig-Holstein, Campus Kiel | Kiel |
| Ayman Barouni | Ayman Barouni | Hückelhoven |
| Andrea Wißmann | Praxis Kristin Schubert | Ettlingen |
| Lena Goldammer | Praxis Lena Goldammer | Celle |
| Ralf-H. Gerl | Überörtliche BAG Gerl Raesfeld | Raesfeld |
| Matthias Gerl | Augenklinik Ahaus GmbH & Co. KG | Ahaus |
| Ralf-H. Gerl | Überörtliche BAG Gerl und Kollegen in Rheine | Rheine |
| Pascal Hasler | Universitätsspital Basel Augenklinik | Basel |
| Patrik Kloos | Augenklinik Wil | Wil |
| Marcel Menke | Kantonsspital Aarau Augenklinik | Aarau |
| Ioannis Petropoulos | Centre Ophtalmologique de Rive | Geneva |
| Veronika Vaclavik | Hôpital Cantonal de Fribourg Ophtalmologie | Fribourg |
| Gabriele Thumann | Hôpitaux Universitaires Genève | Geneva |
| Fabrizio Branca | Augenzentrum Bahnhof Basel | Basel |
| Ralf Kiel | Centre neuchâtelois d’ophtalmologie | Neuchatel |
| Pascal Imesch | Imesch AG | Muri |
| Daniel Barthelmes | UniversitätsSpital Zürich Augenklinik | Zürich |
| R.J. Wouters | Oogcentrum Noordholland | Heerhugowaard |
| L.J. Noordzij | Maasstad Ziekenhuis | Rotterdam |
| Janneke van Lith | St. Elisabeth Ziekenhuis | Tilburg |
| V.P.T. Hoppenreijs | Deventer Ziekenhuis | Deventer |
| Mrs. M. Smeets | Jeroen Bosch Ziekenhuis | ‘s-Hertogenbosch |
| Vicky Boeyden | Ziekenhuis ZorgSaam Zeeuws Vlaanderen | Terneuzen |
| Thorsten Stolwijk | StolMed Oogklinieken | Bergen op Zoom |
| J.P. Martinez Ciriano | Oogziekenhuis Rotterdam | Rotterdam |
References
- Comyn, O.; Sivaprasad, S.; Peto, T.; Neveu, M.M.; Holder, G.E.; Xing, W.; Bunce, C.V.; Patel, P.J.; Egan, C.A.; Bainbridge, J.W.; et al. A randomized trial to assess functional and structural effects of ranibizumab versus laser in diabetic macular edema (the LUCIDATE study). Am. J. Ophthalmol. 2014, 157, 960–970. [Google Scholar] [CrossRef] [PubMed]
- Massin, P.; Bandello, F.; Garweg, J.G.; Hansen, L.L.; Harding, S.P.; Larsen, M.; Mitchell, P.; Sharp, D.; Wolf-Schnurrbusch, U.E.K.; Gekkieva, M.; et al. Safety and efficacy of ranibizumab in diabetic macular edema (RESOLVE Study): A 12-month, randomized, controlled, double-masked, multicenter phase II study. Diabetes Care 2010, 33, 2399–2405. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Brown, D.M.; Marcus, D.M.; Boyer, D.S.; Patel, S.; Feiner, L.; Gibson, A.; Sy, J.; Rundle, A.C.; Hopkins, J.J.; et al. Ranibizumab for diabetic macular edema: Results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012, 119, 789–801. [Google Scholar] [CrossRef]
- Ishibashi, T.; Li, X.; Koh, A.; Lai, T.Y.; Lee, F.L.; Lee, W.K.; Ma, Z.; Ohji, M.; Tan, N.; Cha, S.B.; et al. The REVEAL Study: Ranibizumab Monotherapy or Combined with Laser versus Laser Monotherapy in Asian Patients with Diabetic Macular Edema. Ophthalmology 2015, 122, 1402–1415. [Google Scholar] [CrossRef] [PubMed]
- Kodjikian, L.; Lecleire-Collet, A.; Dot, C.; Le Lez, M.; Baillif, S.; Erginay, A.; Souied, E.; Fourmaux, E.; Gain, P.; Ponthieux, A. ETOILE: Real-World Evidence of 24 Months of Ranibizumab 0.5 mg in Patients with Visual Impairment Due to Diabetic Macular Edema. Clin. Ophthalmol. 2021, 15, 2307–2315. [Google Scholar] [CrossRef]
- Sakamoto, T.; Shimura, M.; Kitano, S.; Ohji, M.; Ogura, Y.; Yamashita, H.; Suzaki, M.; Mori, K.; Ohashi, Y.; Yap, P.S.; et al. Impact on visual acuity and psychological outcomes of ranibizumab and subsequent treatment for diabetic macular edema in Japan (MERCURY). Graefes Arch. Clin. Exp. Ophthalmol. 2022, 260, 477–487. [Google Scholar] [CrossRef]
- Van Aken, E.; Favreau, M.; Ramboer, E.; Denhaerynck, K.; MacDonald, K.; Abraham, I.; Brié, H. Real-World Outcomes in Patients with Diabetic Macular Edema Treated Long Term with Ranibizumab (VISION Study). Clin. Ophthalmol. 2020, 14, 4173–4185. [Google Scholar] [CrossRef]
- Mitchell, P.; Sheidow, T.G.; Farah, M.E.; Mahmood, S.; Minnella, A.M.; Eter, N.; Eldem, B.; Al-Dhibi, H.; Macfadden, W.; Parikh, S.; et al. Effectiveness and safety of ranibizumab 0.5 mg in treatment-naïve patients with diabetic macular edema: Results from the real-world global LUMINOUS study. PLoS ONE 2020, 15, e0233595. [Google Scholar] [CrossRef]
- Michl, M.; Fabianska, M.; Seeböck, P.; Sadeghipour, A.; Haj Najeeb, B.; Bogunovic, H.; Schmidt-Erfurth, U.M.; Gerendas, B.S. Automated quantification of macular fluid in retinal diseases and their response to anti-VEGF therapy. Br. J. Ophthalmol. 2022, 106, 113–120. [Google Scholar]
- German Society of Ophthalmology (DOG); German Retina Society (RG); Professional Association of Ophthalmologists in Germany (BVA). Statement of the German Ophthalmological Society, the German Retina Society, and the Professional Association of Ophthalmologists in Germany on treatment of diabetic macular edema. Ophthalmologe 2021, 118 (Suppl. S1), 40–67. [CrossRef]
- Kalur, A.; Iyer, A.I.; Muste, J.C.; Talcott, K.E.; Singh, R.P. Impact of retinal fluid in patients with diabetic macular edema treated with anti-VEGF in routine clinical practice. Can. J. Ophthalmol. 2023, 58, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.A.; Glassman, A.R.; Ayala, A.R.; Jampol, L.M.; Bressler, N.M.; Bressler, S.B.; Brucker, A.J.; Ferris, F.L.; Hampton, G.R.; Jhaveri, C.; et al. Aflibercept, Bevacizumab, or Ranibizumab for Diabetic Macular Edema: Two-Year Results from a Comparative Effectiveness Randomized Clinical Trial. Ophthalmology 2016, 123, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Elman, M.J.; Ayala, A.; Bressler, N.M.; Browning, D.; Flaxel, C.J.; Glassman, A.R.; Jampol, L.M.; Stone, T.W.; Diabetic Retinopathy Clinical Research Network. Intravitreal Ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: 5-year randomized trial results. Ophthalmology 2015, 122, 375–381. [Google Scholar] [CrossRef]
- Ziemssen, F.; Schlottman, P.G.; Lim, J.I.; Agostini, H.; Lang, G.E.; Bandello, F. Initiation of intravitreal aflibercept injection treatment in patients with diabetic macular edema: A review of VIVID-DME and VISTA-DME data. Int. J. Retin. Vitr. 2016, 2, 16. [Google Scholar] [CrossRef]
- Mitchell, P.; Bandello, F.; Schmidt-Erfurth, U.; Lang, G.E.; Massin, P.; Schlingemann, R.O.; Sutter, F.; Simader, C.; Burian, G.; Gerstner, O.; et al. The RESTORE study: Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 2011, 118, 615–625. [Google Scholar] [CrossRef]
- Brown, D.M.; Schmidt-Erfurth, U.; Do, D.V.; Holz, F.G.; Boyer, D.S.; Midena, E.; Heier, J.S.; Terasaki, H.; Kaiser, P.K.; Marcus, D.M.; et al. Intravitreal Aflibercept for Diabetic Macular Edema: 100-Week Results From the VISTA and VIVID Studies. Ophthalmology 2015, 122, 2044–2052. [Google Scholar] [CrossRef] [PubMed]
- Boyer, D.S.; Yoon, Y.H.; Belfort, R., Jr.; Bandello, F.; Maturi, R.K.; Augustin, A.J.; Li, X.Y.; Cui, H.; Hashad, Y.; Whitcup, S.M.; et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology 2014, 121, 1904–1914. [Google Scholar] [CrossRef]
- Heng, L.Z.; Sivaprasad, S.; Crosby-Nwaobi, R.; Saihan, Z.; Karampelas, M.; Bunce, C.; Peto, T.; Hykin, P.G. A prospective randomized controlled clinical trial comparing a combination of repeated intravitreal Ozurdex and macular laser therapy versus macular laser only in center-involving diabetic macular edema (OZLASE study). Br. J. Ophthalmol. 2016, 100, 802–807. [Google Scholar] [CrossRef]
- Brown, D.M.; Nguyen, Q.D.; Marcus, D.M.; Boyer, D.S.; Patel, S.; Feiner, L.; Schlottmann, P.G.; Rundle, A.C.; Zhang, J.; Rubio, R.G.; et al. Long-term outcomes of ranibizumab therapy for diabetic macular edema: The 36-month results from two phase III trials: RISE and RIDE. Ophthalmology 2013, 120, 2013–2022. [Google Scholar] [CrossRef]
- Sophie, R.; Lu, N.; Campochiaro, P.A. Predictors of Functional and Anatomic Outcomes in Patients with Diabetic Macular Edema Treated with Ranibizumab. Ophthalmology 2015, 122, 1395–1401. [Google Scholar] [CrossRef]
- Lang, G.E.; Berta, A.; Eldem, B.M.; Simader, C.; Sharp, D.; Holz, F.G.; Sutter, F.; Gerstner, O.; Mitchell, P.; RESTORE Extension Study Group. Two-year safety and efficacy of ranibizumab 0.5 mg in diabetic macular edema: Interim analysis of the RESTORE extension study. Ophthalmology 2013, 120, 2004–2012. [Google Scholar] [CrossRef]
- Lim, J.I.; Kim, S.J.; Bailey, S.T.; Kovach, J.L.; Vemulakonda, G.A.; Ying, G.S.; Flaxel, C.J.; American Academy of Ophthalmology Preferred Practice Pattern Retina/Vitreous Committee. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology 2025, 132, P75–P162. [Google Scholar] [CrossRef] [PubMed]
- Ziemssen, F.; Bertelmann, T.; Hufenbach, U.; Scheffler, M.; Liakopoulos, S.; Schmitz-Valckenberg, S.; OCEAN study group. Delayed treatment initiation of more than 2 weeks. Relevance for possible gain of visual acuity after anti-VEGF therapy under real life conditions (interim analysis of the prospective OCEAN study). Ophthalmologe 2016, 113, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Dugel, P.U.; Hillenkamp, J.; Sivaprasad, S.; Vögeler, J.; Mousseau, M.; Wenzel, A.; Margaron, P.; Hashmonay, R.; Massin, P. Baseline visual acuity strongly predicts visual acuity gain in patients with diabetic macular edema following anti-vascular endothelial growth factor treatment across trials. Clin. Ophthalmol. 2016, 10, 1103–1110. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.A.; Glassman, A.R.; Ayala, A.R.; Jampol, L.M.; Aiello, L.P.; Antoszyk, A.N.; Arnold-Bush, B.; Baker, C.W.; Bressler, N.M.; Browning, D.J.; et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N. Engl. J. Med. 2015, 372, 1193–1203. [Google Scholar] [CrossRef]
- Singh, R.P.; Tabano, D.; Kuo, B.L.; LaPrise, A.; Leng, T.; Kim, E.; Hatfield, M.; Garmo, V. How intravitreal anti-vascular endothelial growth factor initial dosing impacts patient outcomes in diabetic macular oedema. BMC Ophthalmol. 2024, 24, 552. [Google Scholar] [CrossRef]
- Li, S.; Pan, J.; Xu, Y.; Dai, Z.; Fang, Q. Exploring the factors influencing the timely intravitreal anti-VEGF treatment in patients with diabetic macular edema: A qualitative interview study using the COM-B model. BMC Health Serv. Res. 2025, 25, 302. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Cao, Y.; Cao, X.; Wang, L.; Zhang, X.; Zhang, Z.; Zai, X.; Yan, Z. Anti-VEGF monotherapy versus anti-VEGF therapy combined with laser or intravitreal glucocorticoid therapy for diabetic macular edema: A Bayesian network meta-analysis. Diabetes Obes. Metab. 2025, 27, 2679–2689. [Google Scholar] [CrossRef]
- Ziemssen, F.; Cruess, A.; Dunger-Baldauf, C.; Margaron, P.; Snow, H.; Strain, W.D. Ranibizumab in diabetic macular edema–a benefit–risk analysis of ranibizumab 0.5 mg PRN versus laser treatment. Eur. Endocrinol. 2017, 13, 91. [Google Scholar]
- Ziemssen, F.; Wachtlin, J.; Kuehlewein, L.; Gamulescu, M.A.; Bertelmann, T.; Feucht, N.; Voegeler, J.; Koch, M.; Liakopoulos, S.; Schmitz-Valckenberg, S.; et al. Intravitreal Ranibizumab Therapy for Diabetic Macular Edema in Routine Practice: Two-Year Real-Life Data from a Noninterventional, Multicenter Study in Germany. Diabetes Ther. Res. Treat. Educ. Diabetes Relat. Disord. 2018, 9, 2271–2289. [Google Scholar] [CrossRef]
- Wells, J.A.; Glassman, A.R.; Jampol, L.M.; Aiello, L.P.; Antoszyk, A.N.; Baker, C.W.; Bressler, N.M.; Browning, D.J.; Connor, C.G.; Elman, M.J.; et al. Association of baseline visual acuity and retinal thickness with 1-Year efficacy of aflibercept, bevacizumab, and ranibizumab for diabetic macular edema. JAMA Ophthalmol. 2016, 134, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.F.; Wykoff, C.C.; Clark, W.L.; Bruce, B.B.; Boyer, D.S.; Brown, D.M.; TREX-DME Study Group. Randomized trial of treat and extend ranibizumab with and without navigated laser for diabetic macular edema: TREX-DME 1 year outcomes. Ophthalmology 2017, 124, 74–81. [Google Scholar] [PubMed]
- Peto, T.; Akerele, T.; Sagkriotis, A.; Zappacosta, S.; Clemens, A.; Chakravarthy, U. Treatment patterns and persistence rates with anti-vascular endothelial growth factor treatment for diabetic macular edema in the UK: A real-world study. Diabet. Med. 2022, 39, e14746. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, N.A.; Greenlee, T.E.; Iyer, A.I.; Conti, T.F.; Chen, A.X.; Singh, R.P. Racial, Ethnic, and Insurance-Based Disparities Upon Initiation of Anti-Vascular Endothelial Growth Factor Therapy for Diabetic Macular Edema in the US. Ophthalmology 2021, 128, 1438–1447. [Google Scholar] [CrossRef] [PubMed]
- Cantrell, R.A.; Lum, F.; Chia, Y.; Morse, L.S.; Rich, W.L.; Salman, C.A.; Willis, J.R. Treatment Patterns for Diabetic Macular Edema: An Intelligent Research in Sight (IRIS®) Registry Analysis. Ophthalmology 2020, 127, 427–429. [Google Scholar] [CrossRef] [PubMed]
- Kuo, B.L.; Tabano, D.; Garmo, V.; Kim, E.; Leng, T.; Hatfield, M.; LaPrise, A.; Singh, R.P. Long-term Treatment Patterns for Diabetic Macular Edema: Up to 6-Year Follow-up in the IRIS® Registry. Ophthalmol. Retina 2024, 8, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Ziemssen, F.; Sylvanowicz, M.; Amoaku, W.M.; Aslam, T.; Eldem, B.; Finger, R.P.; Gale, R.P.; Kodjikian, L.; Korobelnik, J.F.; Xiaofeng, L.; et al. Improving Clinical Management of Diabetic Macular Edema: Insights from a Global Survey of Patients, Healthcare Providers, and Clinic Staff. Ophthalmol. Ther. 2025, 14, 229–246. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).